Back to Journals » Clinical, Cosmetic and Investigational Dentistry » Volume 15
Health Effects of Oral Contraceptives on Periodontal Disease and Gingivitis: A Cross-Sectional Questionnaire-Based Study Among Saudi Women in Jeddah
Authors AlGhamdi SA, Altowairqi K, Altowairqi YG, Alkharobi H, Alfayez E, Mansouri R, Aljahdali B, Badahdah A , Alqarni NM, Qumusan GS, Alrafiah A
Received 16 August 2023
Accepted for publication 13 October 2023
Published 20 October 2023 Volume 2023:15 Pages 237—244
DOI https://doi.org/10.2147/CCIDE.S431814
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Professor Christopher E. Okunseri
Samar Abdullah AlGhamdi,1 Khaled Altowairqi,1 Yazan Ghazi Altowairqi,1 Hanaa Alkharobi,1 Eman Alfayez,1 Rowaina Mansouri,1 Bushra Aljahdali,2 Arwa Badahdah,2 Naif Mari Alqarni,3 Ghadah Sidqi Qumusan,3 Aziza Alrafiah4
1Department of Oral Biology, Faculty of Dentistry, King Abdulaziz University, Jeddah, Saudi Arabia; 2Department of Periodontology, Faculty of Dentistry, King Abdulaziz University, Jeddah, Saudi Arabia; 3AlRuhaily Medical Center, General Dentistry, Jeddah, Saudi Arabia; 4Department of Medical Laboratory Sciences, Faculty of Applied Medical Sciences, King Abdulaziz University, Jeddah, Saudi Arabia
Correspondence: Aziza Alrafiah, Department of Medical Laboratory Sciences, Faculty of Applied Medical Sciences, King Abdulaziz University, Jeddah, Saudi Arabia, Email [email protected]
Background: Sex hormones strongly influence the health and ailment of the oral cavity. For instance, a woman’s oral health is influenced by her menstrual cycle, menopause, pregnancy, and usage of oral contraceptives. The use of various therapeutic medication results in intraoral alterations. Oral contraceptive pills (OCPs) are among the drugs that produce intraoral alterations. The study’s objective was to evaluate attitudes and oral health conditions of Saudi women’s utilizing OCPs in Jeddah, Saudi Arabia.
Methods: A cross-sectional questionnaire-based study was conducted among Saudi women in Jeddah, Saudi Arabia. The self-administered questionnaire was made and sent to women to evaluate the attitude and oral health condition of women utilizing OCPs. The women using OCPs were asked to self-administer 17 questions to evaluate attitudes and oral health conditions. The questionnaire had multiple-choice questions and was consisted of four sections.
Results: The number of participants who used contraceptives was 125 (35.9%) women; of them, only 94 (75.2%) used oral contraceptives. The duration of using oral contraceptives mainly was 1– 5 years (39.4%), then > 5 years (34.0%), and < 1 year (26.6%). Of the 94 women, 34 (36.2%) had gingival diseases, 23 (24.5%) treated their gums; and 13 (13.8%) cleaned their gums at a dental clinic regularly. Times of teeth brushing per day were one time in 32 women (34%), twice in 47 women (50.0%), and three times in 15 (16.0%). Of the 94 women, 4 (4.3%) were smoking, 24 (25.5%) took medication other than OCPs, and 16 (17.02%) had chronic diseases. Common oral complications noticed by participants were gum bleeding after brushing (51.6%), dental caries (25.5%), and oral ulcers (10.6%).
Conclusion: Females on OCPs had a high rate of gingival bleeding, dental caries, and oral ulcers. OCPs users had poor periodontal and gingival health. Establishing an oral hygiene program was necessary to treat gingival and periodontal inflammation that exacerbated by OCPs.
Keywords: oral contraceptives, oral cavity, attitude, women
Introduction
In addition to being used to prevent conception, hormonal contraceptives can also be used for family planning, regulating menstruation, reducing the risk of ovarian cysts, etc.1 Among the hormonal methods of contraception, there are several birth control methods available, including pills, patches, implants, injections, intravaginal delivery, and intrauterine delivery. Oral contraceptive pills typically contain two synthetic hormones, progestins and estrogens, which work by selectively inhibiting anterior pituitary secretion of follicle-stimulating hormone (FSH) and luteinizing hormone (LH), which prevent the ovary from releasing ovum and encourages contraception.1 Current OCPs contain low progestin (1.5mg/day) and estrogens (0.05mg/day). OCPs are commonly used by women. Women on oral contraceptives are about 50 million worldwide, so several systemic and oral side effects have occurred.2 The systemic side effects include cardiovascular and thromboembolic problems, nausea, vomiting, breast heaviness, and irregular menstruation.3
Oral cavity health is essential for general health, authenticated by the statement that the oral cavity is considered a “window” through which external microorganisms interact with the host.4 The oral cavity is a target organ for side effects caused by medications. Sex hormones affect periodontal disease pathogenesis5,6 as hormonal variation influences the physiology of the oral cavity.7 Estrogen and progesterone play a role in physiological changes in women at their live stages. Estrogens can affect the synthesis and maintenance of fibrous collagen and cytodifferentiation of stratified squamous epithelium.8,9 Progesterone affects the periodontium directly and may be crucial in coupling bone growth and resorption.10 When hormones are combined, they affect many different tissues and could impact someone’s health. The oral alterations that are most frequently reported while using OCPs include gingivitis, papillae irritation, gingival pregnancy-type epulis, erythema of gingiva, mucosal coloration, gingival bleeding, and inflammation.3 Due to lacking of the knowledge and awareness about the detrimental effects of OCPs on oral health status, most of these alterations go unreported by OCPs users.11
This research aimed to investigate the impact of OCPs usage on oral cavity health status, including dental caries, oral ulcers, and gingival bleeding after brushing.
Materials and Methods
Participants
The cross-sectional questionnaire-based study was conducted among Saudi women in Jeddah, Saudi Arabia. The Raosoft software package was utilized for sample size estimation, and a single proportion method was used. Assuming that 50% of Saudi women used contraceptives, the sample size was 150 patients at a % error margin and 95% confidence interval.12 Saudi women of 18 years or older, having positive history of OCPs usage and who accept to participate were included in this research. Excluded from the study were non-Saudi women and women who did not use oral contraceptives. A total of 384 women participated in this research; 125 women used contraceptives. Only 94 participants used oral contraceptives and were included in this study. Our study complies with the Declaration of Helsinki. Following a thorough description of the study’s purpose in Arabic to all women, informed consent was obtained. The data collection duration was seven months, from June 2022 to December 2022.
The study was designed with correspondence to the codes of the guidelines for Ethical Conduct in the Care and Use of female patient experimental conduct and handling were authorized via the Ethics division within the Ethics Committee of Dental Research-Faculty of Dentistry at King Abdul Aziz University, ethical approval number (043–02-23), followed in King Abdulaziz Dental Hospital, KAU, Jeddah, Saudi Arabia. All participants accepted to fill the consent form and to enrolled in the study.
The questionnaire was available in English and Arabic. The questionnaire’s reliability examination revealed a Cronbach full-scale alpha score of 78%, validity, solid internal consistency, and split-half reliability. The questionnaire was created in Google form, and respondents were sent the questionnaire via e-mail and WhatsApp.
Survey Questionnaire
In this study, women using OCPs were asked to self-administer 17 questions to evaluate attitudes and oral health conditions. The questionnaire had multiple-choice questions. The questionnaire consisted of four sections. The first section records sociodemographic data as women’s age, education, usage of contraceptives, and types of the used contraceptives. The second section assesses risk factors for oral diseases such as duration of oral contraceptive usage, smoking, medications used other than OCPs, and presence of chronic diseases. The third section is designed to assess attitudes about gingival health as the presence of gingival diseases and treatment of these diseases at dental clinics regularly. The fourth section is designed to assess oral health in women using OCPs as an increased rate of dental caries, oral ulcers, and gingival bleeding after brushing.
Statistics Analysis
Data were imported into Excel. IBM SPSS statistics version 22 (IBM Corp., 2013) was used to analyze it—Armonk, NY: IBM Corp. Descriptive quantitative data, such as frequency and percentage, were used to analyze the responses.
Results
The study sample of participants who answered the questionnaire was consisted of 348 married women. The women were classified according to age as following: 36–50 years old (n=63, 67.0%), 26–35 years old (n= 26, 27.7%), and 18–25 years old (n=5, 5.3%) (Figure 1). Most of the participants were in higher education and employee (n= 39, 41.5%), then university (n=36, 38.3%), secondary school (n=11, 11.7%), and uneducated (unschooled) (n= 8, 8.5%) (Figure 2).
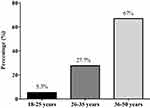 |
Figure 1 Age groups of participants (n= 94). |
 |
Figure 2 Education levels of participants (n= 94). |
Table 1 shows the risk factors that affect the gum. The duration of using oral contraceptives mainly was 1–5 years (39.4%), then more than five years (34.0%), and less than one year (26.6%). Of the 94 women, 4 (4.3%) were smoking. 24 (25.5%) were women who took medication other than oral contraceptives. 16 (17.02%) were women who had chronic diseases; of them, 5 (31.3%) had diabetic mellitus, and 11 (68.7%) had other chronic diseases.
 |
Table 1 Risk Factors of Participants That Affect Oral Health (N= 94) |
Table 2 shows the attitude of women about their oral health. Of the 94 women, 34 (36.2%) had gingival diseases, 23 (24.5%) treated their gums; and 13 (13.8%) cleaned their gums at dental clinics regularly. Times of brushing the teeth per day were one time in 32 women (34%), twice in 47 women (50.0%), and three times in 15 women (16.0%).
 |
Table 2 Attitude Towards Their Gingival Health (N= 94) |
Table 3 shows patients’ oral health after using oral contraceptives. 48 women (51.1%) had gingival bleeding after brushing; 24 women (25.5%) had an increased rate of dental caries; and 10 women (10.6%) had oral ulcers.
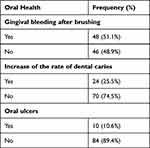 |
Table 3 Oral Health After Using Oral Contraceptive (N= 94) |
Discussion
Gingival hypertrophy is linked to OCPs users in females. To maintain proper oral hygiene, assessing attitudes about OCPs and their impact on oral health is crucial. In this cross-sectional questionnaire-based study, Saudi women participants using OCPs in a wide age range (18–50 years) were assessed for attitude and oral health status. A valid and reliable questionnaire was utilized. During menstruation, pregnancy, and menopause, increased gingival probing depth, gingival inflammation, and bleeding on probing may notice as these changes are related to physiological hormonal imbalances.13
In this study, the duration of OCPs usage was mostly 1–5 years (39.4%) where 4.3% of women were smokers, 25.5% of women took medication other than OCPs, and 17.02% had chronic diseases.
The attitude of women in this study towards their oral health was not good, as 36.2% had gingival diseases, 24.5% treated their gums, and 13.8% cleaned their gums at dental clinics regularly. Times of brushing the teeth per day were one time only in 34%, twice in 50.0%, and three times per day in 16.0% of the participants.
In this study, complications developed during usage of OCPs were mostly gingival bleeding after brushing (51.6%), increased rate of dental caries (25.5%), and oral ulcers (10.6%). In this respect, Lindhe and Björn was the first who identified the association between OCPs usage and gingival disease in 1967.14 Tilakaratne et al looked for any gingival alterations in 39 women who never used hormonal contraceptives (control), and a matched group of 32 women used hormonal contraceptives for less than 2 years, and 17 women used OCPs for 2–4 years. They found that contraceptive products containing estrogen and progesterone were linked to an increase in gingivitis prevalence. Attachment loss was noticeably higher when hormonal contraceptives were used for a more extended period than controls.14 Kardalkar et al reported that 49% of women had gingival disturbances during OCPs usage including swelling, bleeding of the gingiva, and 42% had gingival bleeding in the last six months.15
Gingival inflammation and crevicular exudate are the most typical oral symptoms of elevated ovarian hormone levels. Gingival tissue has androgen, estrogen, and progestin receptors that let periodontal tissues target gynecological hormones.16 These hormones operate as growth factors near microbial colonies in the crevicular fluid where they are found. Thus, aggravating plaque-associated gingivitis.15
Sex hormones can control how tissues, especially periodontal tissues,5,6 respond to inflammation. According to studies, the lamina propria, gingival keratinocytes, and gingival fibroblasts found in the periodontal ligament all have receptors for sex hormones, including estrogen and progesterone.17 Therefore, periodontal tissue can be indirectly modulated by steroid hormones. In addition to encouraging an increase in tissue glycogen production and lowering keratinization of gingival epithelium, which reduces the epithelial barrier, estrogen can control collagen metabolism8,9 and angiogenesis. Moreover, it alters cell proliferation by reducing leukocyte formation in the bone marrow and increasing phagocytosis. Progesterone causes blood vessels to dilate, subsequently increasing endothelial permeability and altering how periodontal ligament fibroblasts produce collagen. It also inhibits collagen and non-collagen protein synthesis, lowers folate levels, and promotes an unbalanced tissue repair process.18 Progesterone hormone increases vascular permeability and prostaglandin production.19
It has been hypothesized that the use female hormonal contraception affects the development of gingival and periodontal disease. The overall duration of ingestion and hormone dosage are the two potential determinants of how OCPs affect periodontal health.20 When exposed to nearby irritants, gingival tissues may overreact. OCPs may worsen a patient’s inflammatory state, resulting in erythema and greater susceptibility to gingival bleeding. Inflammation can take many forms, from minor swelling and erythema to severe inflammation accompanied by hyperplastic or hemorrhagic gingival tissues. According to available data, the pathogenesis of chronic gingivitis is heavily influenced by the presence of sex hormone metabolic products in the gingiva.20 Women who have used OCPs for a year had a 50% increase in gingival fluid volume, which changes in the microvasculature may cause increased gingival permeability and prostaglandin production.21 Researching the impact of OCPs, Brusca et al found that women who used oral contraceptives, particularly smokers, had a significant prevalence of severe periodontitis.22 Additionally, these women exhibited a more significant percentage of Candida sp.-positive cultures linked to P. gingivalis and P. intermedia.23 The number of Bacteroides species is 16 times higher in the OCPs user group than in the non-pregnant group.21 OCPs are found to induce an enlargement of the gingiva.2 The incidence of gingival overgrowth induced by OCPs is common and resolves by OCPs withdrawn.20 During OCPs ingestion, maintaining appropriate plaque management is crucial for gingival health.23 Meanwhile, studies based on large population samples revealed that current combined OCPs did not affect periodontal health, possibly due to their lower concentrations of estradiol and progesterone.23,24
Limitation of the Study
The main limitation is self-reported data, which is always subjected to bias. Additionally, factors like social standing may impact and change the outcomes. This study, however, firmly backs up the fact that women do not have a positive perspective on how OCPs affect their oral health. Also, this study included smokers, women who took medications other than OCPs, and women who had chronic diseases; all these may affect oral health. Dentists must collaborate more to better understand the impact of OCPs on dental health and the pathways that contribute to oral issues.
Conclusions
Gingival bleeding, dental caries, and mouth ulcers were common in women using oral contraceptives. The periodontal and gingival health of OCPs users was poor. The treatment of gingival and periodontal inflammation caused by OCPs must include the implementation of an oral hygiene program. Because OCPs have a negative impact on oral health, women should use alternative birth control methods. Because current studies lack clinical oral cavity examinations, it is required to perform questionnaire studies that include clinical oral cavity examinations to evaluate the condition of oral health and raise awareness and information about oral hygiene during oral contraceptives. While OCPs can affect women oral health, consulting with the dentist and physician can help managing any side effects that contraceptives cause. Maintaining a regular oral care routine is key to ensuring that mouth stays healthy and that women stay comfortable.
Ethical Approval and Patients Consent Form
The study was designed with correspondence to the codes of the guidelines for Ethical Conduct in the Care and Use of female patient experimental conduct and handling were authorized via the Ethics division within the Ethics Committee of Dental Research-Faculty of Dentistry at King Abdul Aziz University, ethical approval number (043-02-23), followed in King Abdulaziz Dental Hospital, KAU, Jeddah, Saudi Arabia. All participants accepted to fill the consent form and to enrolled in the study.
Acknowledgments
The authors thank all participants that filled in the questionnaire needed for the project.
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Funding
This research received no external funding.
Disclosure
The authors report no conflicts of interest in this work.
References
1. Colquitt CW, Martin TS. Contraceptive methods: a review of nonbarrier and barrier products. J Pharm Pract. 2017;30(1):130–135. doi:10.1177/0897190015585751
2. Reddy P, Jamadar S, Chaitanya BN. Effects of Oral contraceptives on the oral cavity. Indian J Dental Adv. 2013;5(3):1274–1277.
3. Leelakanok N, Methaneethorn J. A systematic review and meta-analysis of the adverse effects of levonorgestrel emergency oral contraceptive. Clin Drug Investig. 2020;40(5):395–420. doi:10.1007/s40261-020-00901-x
4. Kane SF. The effects of oral health on systemic health. Gen Dent. 2017;65(6):30–34.
5. Apoorva S, Suchetha A. Effect of sex hormones on the periodontium. Indian J Dental Sci. 2010;2(5):36–40.
6. Boyapati R, Cherukuri SA, Bodduru R, Kiranmaye A. Influence of Female Sex Hormones in Different Stages of Women on Periodontium. J Midlife Health. 2021;12(4):263–266.
7. Bobetsis YA, Graziani F, Gürsoy M, Madianos PN. Periodontal disease and adverse pregnancy outcomes. Periodontology. 2000;83(1):154–174. doi:10.1111/prd.12294
8. Eleni M, Boura E, Tsalikis L, Konstantinides A. The influence of sex steroid hormones on gingival of women. Open Dent J. 2009;3:114–119. doi:10.2174/1874210600903010114
9. Chopra M, Dhawan P, Kaur H. Role of progesterone in oral health and Prosthodontic rehabilitation in Geriatric females. Eur Chem Bull. 2023;12(S3):6739–6745.
10. Mascarenhas P, Gapski R, Al‐Shammari K, Wang HL. Influence of sex hormones on the periodontium. J Clin Periodontol. 2003;30(8):671–681. doi:10.1034/j.1600-051X.2003.00055.x
11. Al-Mehdar AA, Al-Battah AM. Evaluation of hypoglycemic activity of Boswellia carterii and Cissus rotundifolia in streptozotocin/nicotinamide-induced diabetic rats. Yemeni J Med Sci. 2016;10(1):30–38. doi:10.20428/yjms.v10i1.959
12. Lsharif SS, Abu Saeed RI, Alskhairi RF, Almuwallad SA, Mandili FA, Shatla M. Knowledge, Attitude, and Practice of Contraception Use Among Childbearing Women in Makkah Region, Saudi Arabia. Cureus. 2023;15(2):e34848. doi:10.7759/cureus.34848
13. Antony M, Rajasekar A. Influence of Female Sex Hormones on Periodontium. J Coastal Life Med. 2022;10:677–681.
14. Lindhe J, Bjorn AL. Influence of hormonal contraceptives on the gingiva of women. J Periodontal Res. 1967;2(1):1–6. doi:10.1111/j.1600-0765.1967.tb01989.x
15. Kardalkar S, Bhayya H, Kardalkar S. Assessment of Knowledge, Attitude and Oral Health Status of the Women Using Oral Contraceptive Pills among Different Socioeconomic Status. Saudi J Oral Dental Res. 2019;4(1):25–30.
16. Prachi S, Jitender S, Rahul C, Jitendra K, Priyanka M, Disha S. Impact of oral contraceptives on periodontal health. Afr Health Sci. 2019;19(1):1795–1800. doi:10.4314/ahs.v19i1.56
17. Castro MML, Ferreira MKM, Prazeres IEE, et al. Is the use of contraceptives associated with periodontal diseases? A systematic review and meta-analyses. BMC Women’s Health. 2021;21(1):1–22. doi:10.1186/s12905-021-01180-0
18. Elzer ASM, Sassi K, Elkremi M, Ragab T, Alwarfely H. Self-reported gingivitis among pregnant women and nonpregnant women in the City of Derna, Libya: is there any difference? A cross-sectional survey. Libyan J Med Sci. 2019;3(3):83. doi:10.4103/LJMS.LJMS_61_18
19. Rausch‐Fan X, Ulm C, Jensen‐Jarolim E, et al. Interleukin‐1β–Induced Prostaglandin E2 Production by Human Gingival Fibroblasts Is Upregulated by Glycine. J Periodontol. 2005;76(7):1182–1188. doi:10.1902/jop.2005.76.7.1182
20. Domingues RS, Ferraz BF, Greghi SL, Rezende ML, Passanezi E, Sant’Ana AC. Influence of combined oral contraceptives on the periodontal condition. J Appl Oral Sci. 2012;20(2):253–259. doi:10.1590/S1678-77572012000200022
21. Güncü GN, Tözüm TF, Cağlayan F. Effects of endogenous sex hormones on the periodontium--review of literature. Aust Dent J. 2005;50(3):138–145. doi:10.1111/j.1834-7819.2005.tb00352.x
22. Brusca MI, Rosa A, Albaina O, Moragues MD, Verdugo F, Pontón J. The impact of oral contraceptives on women’s periodontal health and the subgingival occurrence of aggressive periodontopathogens and Candida species. J Periodontol. 2010;81(7):1010–1018. doi:10.1902/jop.2010.090575
23. Abdollahi M, Rahimi R, Radfar M. Current opinion on drug-induced oral reactions: a comprehensive review. J Contemp Dent Pract. 2008;9(3):1–15. doi:10.5005/jcdp-9-3-1
24. Tilakaratne A, Soory M, Ranasinghe AW, Corea SM, Ekanayake SL, de Silva M. Effects of hormonal contraceptives on the periodontium, in a population of rural Sri-Lankan women. J Clin Periodontol. 2000;27(10):753–757. doi:10.1034/j.1600-051x.2000.027010753.x
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
