Back to Journals » Journal of Healthcare Leadership » Volume 15
Fostering Excellence in Obstetrical Surgery
Authors Wilson RD
Received 9 August 2023
Accepted for publication 13 November 2023
Published 27 November 2023 Volume 2023:15 Pages 355—373
DOI https://doi.org/10.2147/JHL.S404498
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Dr Pavani Rangachari
R Douglas Wilson
Department of Obstetrics and Gynecology, Cumming School of Medicine University of Calgary, Calgary, Alberta, Canada
Correspondence: R Douglas Wilson, Department of Obstetrics and Gynecology, Cumming School of Medicine University of Calgary, Alberta, Canada, Tel +1 403-470-7229, Email [email protected]
Introduction: This obstetric surgery review is directed toward the common obstetrical surgeries (caesarean delivery, VBAC/TOLAC, operative vaginal delivery, placenta accreta spectrum) with evidence for quality and safety to allow for obstetrical outcome excellence.
Materials and Methods: This focused scoping review has used a structured process for article identification and inclusion for each of the focused surgeries.
Results: The review results provide an obstetrical surgery (OS) overview for caesarean delivery, vaginal birth after caesarean delivery and/or trial of labor after caesarean delivery, operative vaginal delivery, placenta accreta spectrum; considerations for quality and safety variance due to non-clinical human factors; quality improvement (QI) tools; OS QI implementation cohorts; implementation considering certain barriers and solutions.
Conclusion: Administrative health care systems and obstetrical surgery care providers cannot afford, not to consider and implement, certain evidenced-based “bottom-up/top-down” processes for quality and safety, as the patients will demand the quality and the safety, but the lawyers should not have to enforce it.
Keywords: obstetrical safety, obstetrical quality, obstetrical morbidity, caesarean delivery, vaginal birth after caesarean delivery, trial of labor after caesarean delivery, operative vaginal delivery, placenta accreta spectrum, implementation process
Introduction
Why is obstetrical surgery important for reproductive health morbidity care in 2023? What are the systems (primary/secondary) and clinical factors that create morbidity for pregnant people? What evidenced-based management tools and implemented processes can be considered or used to provide enhanced safety and quality for obstetrical surgery?
The rates of caesarean delivery (CD) and the associated accreta spectrum disorder have increased steadily over the past 3 decades, while the clinical use of operative vaginal delivery and vaginal birth after CD – trial of labor after caesarean (VBAC /TOLAC) have decreased. The impact of obstetrical surgery on a person’s reproductive outcomes and future options is important. The clinical management of the first pregnancy (>20 weeks of gestation) and the utilized delivery method will have a significant impact on future reproductive choices. Clinical delivery training, maternity care pathways/systems, and hospital -birthing resources will influence the complexity of counselling, informed consent, and shared decision- making.1–8
This health care leadership commentary is directed toward the common obstetrical surgeries (caesarean delivery, VBAC/TOLAC, operative vaginal delivery, placenta accreta spectrum) and the available quality and safety evidence to allow for enhanced obstetrical practice outcomes.
Methods
This structured (scoping) prevention and quality improvement review has utilized the peer-reviewed and grey literature to evaluate clinical outcomes for caesarean delivery, operative vaginal delivery, and TOLAC/VBAC with the associated benefit and risk/morbidity including diagnosis and management for placenta accreta spectrum. Evidenced-based human resource, clinical, and system approaches were identified to be used for enhanced quality and safety with the listed obstetric surgeries. Key search terms were included using pregnancy, delivery, morbidity, adverse events, labor and delivery complications, quality improvement, patient safety, audit, measurement, caesarean delivery, operative vaginal delivery, placenta accreta spectrum, vaginal birth after CD (VBAC), trial of labor after caesarean (TOLAC).
Results
Counselling Overview for the Four Obstetrical Surgery Options
Table 1 summarizes the obstetrical surgeries with the clinical benefit and risk counselling topics.1–8
 |
Table 1 Obstetrical Surgeries Benefit and Risk Considerations1–8 |
Caesarean delivery (CD) (2021–2022) was the most common inpatient hospital surgery in Canada. The CD rates have continued to increase in Canada, from 18.7% (1997) to 28.2% (2016), representing a 50.8% increase. In the United States (2021), 32.1% of live births were by CDs, the rate of primary CDs (no previous CD) was 22.3 per 100 live births to women while the rate of vaginal births after a previous caesarean (VBAC) was 14.2 per 100 live births. These increasing CD rates for North American are, in concert, with global comparisons, as the rates in many countries have increased by 40% between 2000 and 2015. Some common explanations provided for these observed CD increases are attributed to pregnant persons having their first birth at a later age, increased pregnant person obesity, increased use of fertility treatments, clinical convenience for both physicians and patients, and more pregnant people are making the choice to have a CD, with expectations of smaller family size.1,2 Classification of CD clinical factors is important as it allows for an understanding and comparison of different classification rates and audit results (Table 2).9–12
 |
Table 2 Robson Caesarean Delivery (CD) Classification: International Comparisons9–12 |
Trial of labor after caesarean delivery (TOLAC) and vaginal delivery after caesarean delivery (VBAC)3,4 are similar terms for the option of waiting for the onset of spontaneous labor and the opportunity for a possible vaginal delivery, following a previous CD delivery. Important counselling issues are related to the indication for the previous caesarean delivery, the patient motivation for a vaginal delivery, the limited opportunity for oxytocin use in labor and the 1% risk for uterine rupture during labor, with maternal and neonatal morbidity and possible neonatal mortality. The optimal technique for uterine closure has not been established. Table 313–30 summarizes present evidence for uterine closure techniques related to minimizing the risk of uterine rupture during labor and/or a uterine scar defect with blastocyst implantation. A reasonable surgical approach would consider a double-layered continuous unlocked - monofilament suture with a decidual exclusion for uterine closure, following the use of routine pre-operative antibiotic prophylaxis. This suggestion for uterine closure is based on the evidence for better wound healing and an outcome of increased residual myometrial thickness (RMT), thereby providing improved quality and safety for maternal outcomes, regardless of increased OR time or cost-effectiveness factors.
 |
Table 3 Uterine Closure Detail |
Operative vaginal delivery (OVD)5,6 refers to the use of delivery forceps or vacuum devices, in the second stage of labour, to facilitate a vaginal birth when the fetal position and descent is appropriate for the delivery technique. Clinical factors, associated with the use of OVD, are a prolonged or arrested fetal descent or possible findings associated with imminent fetal risk or with pregnant person exhaustion or where a pregnant person co-morbidity contraindicates pushing to assist the vaginal delivery. The choice of forceps (and type) or a vacuum device is based on many factors such as the amount of caput or moulding on the fetal head, fetal gestational age, fetal presentation (position-station), fetal response to the pregnant person pushing efforts, pregnant person access to epidural anesthesia, operator-provider experience, and operator-patient informed consent preference based on the likelihood of OVD success.
Placenta accreta spectrum (PAS) disorders,7,8 first reported in 1927, is becoming more common and is evolving into one of the most significant iatrogenic pregnancy complications requiring team-based obstetrical surgical expertise. The PAS incidence has increased from 1 in 2510 women (1994) to the present range of 1 in 272 −403 women (2016). PAS contributes to 30% of the maternal mortality rate, especially if no antenatal diagnosis has been identified.31
Non-Clinical Human Factors (Culture and Insight for SMM, Equity, and Trauma Informed Care) Impacts Obstetrical Surgery
The domains reported for patient-centered care (PCCW) include fostering a relationship, exchanging information, addressing emotions, managing uncertainty, making decisions, and enabling self management. While the information exchange domain is more commonly identified, a theoretical rapid review found that little research has been done to establish what constitutes PCCW, or how to implement or measure PCCW despite the advocacy to improve women’s health with emphasis on PCC and the worldwide recognition in women’s health disparities.32
The components for quality of care have identified the clinical areas of equity, safety, patient-centered care, timeliness/accessibility, effectiveness/appropriateness, and efficiency. This obstetrical surgery review will only focus on the first three components as these reflect on the team-based culture and attitude for obstetrical surgery rather than the other components for procedural skill, although important.
The variation in safety surveillance outcomes for the obstetrical surgery suggests that there are quality and equity variations in the care, especially when the populations have been risk adjusted.33 These areas could be considered as clinical targets for prevention.34–36 Socio-economic disadvantage has been associated with post-partum re-admission and could be an important quality obstetrical surgery indicator for improvement or prevention, based on the severe maternal and adverse outcomes surveillance in obstetrical care.37
Eight steps have been proposed for use in narrowing disparities and inequity across the maternal care gap: enhance communications; address implicit bias; implement a disparities dashboard; perform enhanced maternal mortality and severe maternal morbidity reviews; standardize care on labor and delivery; promote a culture of equity; develop new models of care across the care continuum; and engage key stakeholders.38,39
Surveillance and audit for severe maternal morbidity (SMM) is required to achieve safety and quality. SMM is defined as an unintended outcome(s) during the process of labor and delivery that may result in significant short-term or long-term consequences to a woman’s health. ACOG and SMFM have recommended two screening criteria for SMM identification: 1) transfusion of 4 or more units of blood and 2) admission of a pregnant or postpartum woman to an ICU. Investigators have demonstrated that these two simple criteria have a high sensitivity and specificity for identifying women with severe morbidity and a high positive predictive value (0.85). Centers may choose to incorporate additional screening criteria to identify additional maternal elements for detailed review.40,41 A short list of SMM causes and their potential preventability are summarized (Table 4).40,41
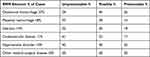 |
Table 4 Most Common Causes for Severe Maternal Morbidity (SMM): Opportunity to Alter Outcome Was Identified in 62% of Cases (Strong in 20% and Possible in 42%)40,41 |
Patient centered care/trauma-based feelings are very likely to have an impact on obstetrical surgery and should be considered. The CDC highlights the significant prevalence of patient-related trauma. It has been reported that one in four children experiences some sort of maltreatment (physical, sexual, or emotional abuse). One in four women have experienced domestic violence, while one in five women and one in 71 men have experienced rape at some point in their lives (12% of these women and 30% of these men were younger than 10 years old when they were raped). These statistics indicate that a very large number of people have experienced serious trauma at some point in their lives.42
It is important for health care providers to understand that commonly used medical exams, by definition, can feel invasive to the pregnant person. The medical care process often involves asking sensitive questions, examines intimate body parts, and sometimes delivers uncomfortable/painful treatments. An understanding of these six principles will help to guide a trauma-informed approach by maternity or all health care providers to create an environment with safety; peer-support; trustworthiness and transparency; collaboration and mutuality; empowerment and choice; and recognition of any potential cultural, historical and gender issues.42
The informed consent process for obstetrical surgery requires that there is knowledge, with the adoption of a trauma-informed approach required by the team/provider so there is constant attention, caring awareness, sensitivity, and possibly a cultural change at an organizational level.42
Obstetrical Surgery Services Options or Tools for Quality and Safety Considerations
The opportunity for obstetrical surgery improvement or prevention of adverse outcome requires a preventive approach as well as the identification of morbidity associated outcomes with the potential use of obstetrical surgery. Obstetrical surgery is a team-based process. Change implementation via the system, knowledge, or behavioral factors provides added complexity to an identified clinical improvement process.
Prevention requires preconception and/or antenatal knowledge transfer processes.
Pre-conception reproductive education to understand the personal maternal pregnancy risk estimate should be encouraged, given that maternity risk issues related to maternal comorbidities are increasing in prevalence. The person, planning a pregnancy, requires a better understanding and recognition of the maternal and pregnancy-related conditions before they become pregnant. The obstetrical risk conditions can change quickly from the common mild-to-moderate morbidity outcomes to SMM outcomes with potential long-term health implications, limiting an appropriate informed consent understanding. The possibility of pregnancy triage with change in maternity care, to the most appropriate level of maternity provider and delivery location, may be required and these potential risk needs to be understood and considered by the pregnant person. The morbidity risks for pregnant people have increased, multi-disciplinary collaborative processes may be required and understanding and acceptance from patients, providers, and health care systems is needed. A risk evaluation tool is available for early discussion with the non-pregnant or pregnant person related to possible clinical morbidity (mortality) factors. This counselling tool allows for a patient-provider review and recognition (informed consent) of the possible leading causes of maternal morbidity risk: pre-conception risks (maternal age >45 years; pre-existing cardiac or hypertensive conditions) and pregnancy-obstetrical risks (gestational hypertension, preeclampsia, or eclampsia; caesarean delivery, whether preterm or term; operative vaginal delivery; maternal sepsis; placenta accreta spectrum; antepartum or postpartum hemorrhage).43
Fetal-based morbidity (aneuploidy, genetic inheritance, congenital anomalies (malformation, deformation, disruptive-teratogenic impact)) requires protocol-guideline-based counselling by the provider to allow patient understanding and choice.44
The antenatal surveillance and perinatal data sources are commonly available as administrative healthcare requirements for many provinces, states, and countries collect this data. The Alberta Perinatal Health Program (APHP Alberta Canada) audits key perinatal – neonatal performance indicators to promote maternal health, positive birth outcomes and healthy infancy. These indicators are provided to the healthcare provider, with a view to enhance practitioner knowledge and skills, to promote evidence informed clinical practice through quality assurance, and to facilitate the collection and analysis of perinatal data for continued surveillance. The Peri-Link data repository is used to inform and evaluate programs and provides provincial leadership through partners and stakeholders.45
The three key APHP program activities identified are: the collection and validation of provincial perinatal data, the analysis and interpretation of data for those providing perinatal services, and support for perinatal research.45
APHP facilitates perinatal health research by offering epidemiology support and providing data from the Peri-Link data repository. These quality assurance activities are undertaken with a view for continual improvement of the provided health care or services (evaluating identified patient safety concerns; reviewing reported maternity associated adverse events). An additional goal for this surveillance is to provide a method of communication for QI recommendations to appropriate and accountable individual(s). The outcomes of these quality assurance activities would include:45
- The identification of preventable factors and system issues.
- Identified gaps in knowledge and clinical service delivery.
- Recommendations for quality improvements.
- Collection, analysis, and reporting of aggregate data with perinatal and maternal mortality.
- Review, revise, and/or develop perinatal forms and audit tools to support/promote the optimal perinatal practice.
With a quality surveillance program and an identified perinatal concern, a useful quality improvement approach is to “Plan, Do, Study, Act”.46 The Plan-Do-Study-Act (PDSA) method is a process to test the identified clinical care change that has been implemented to modify the identified problem /gap. The PDSA cycle evaluates a clinical care change – by planning it, trying it, observing results/outcomes, and acting on what is learned or identified. PDSA is a scientific method, used for action-oriented learning and change. The purpose is to learn as quickly as possible, whether and how an intervention or clinical care change works in a particular setting, allowing adjustments to be made to increase the chances of delivering and sustaining the desired improvement, or to stop the unsuccessful intervention and try something else. Planning is the foundation, as this step ensures that the whole clinical team is aligned, knows their responsibilities, and is clear in the purpose of the PDSA from the start.46
The four PDSA cycle approaches are:
- Plan: identifying a goal or purpose, formulating an intervention or clinical care change, defining success with a measurable outcome, and implementing the chosen plan/process appropriate plan into action.
- Do: identified components or the clinical care elements of the process or pathway are implemented.
- Study: monitoring/measuring outcomes to test the validity of the change for signs of progress and success, or problems and areas for improvement. Short-cycles changes, coupled with analysis of test results, are helpful so the team can learn from these clinical changes, before the PDSA activities are used more broadly.
- Act: closing the cycle, integrating the knowledge generated by the entire process, which can be used to adjust the goal, change methods, or even reformulate an intervention or improvement initiative altogether.
An implemented checklist QI approach has advantages of simplicity and repetition as any clinical care team may forget important care elements leading to clinical care mistakes.47 The team can serially follow a defined checklist, complete the identified elements, and adapt the list to your own circumstances and psychology. The checklist helps the team to be specific and allows the team to delegate tasks and responsibility.
The WHO Surgical Safety Checklist (SSC) considers nineteen items focused into three “time-based phases” of a surgical procedure: sign-in (before induction of anesthesia, while the patient is still conscious); time-out (with the surgeon present, before skin incision); and sign-out, based on the Joint Commission’s Universal Protocol. The SSC has been shown to reduce complications and mortality by >30%. The WHO Checklist is simple, can be completed in under 2 minutes, improves patient safety and inter-discipline communication, and prevents ‘avoidable complications by emphasising current safety procedures.47
Enhanced recovery after surgery (ERAS) is a protocol program that uses measurable clinical care elements in an operative pathway to provide surgical and patient quality and safety, audit, and comparison. ERAS is a patient-centered system that uses evidence-based pathways that have been developed and implemented by a multidisciplinary team to improve the surgical and facility culture and to reduce the patient’s surgical stress response, optimize their physiologic function, and facilitate recovery. There are three main ERAS pillars: evidence-based perioperative care process elements, multi-modal and multi-professional teamwork, and continuous clinical element audit using the pre-, intra-, and post-operative clinical elements/tasks to minimize the variance in care (benefit; risk).18,19,48–51
The Enhanced Recovery after Surgery – Caesarean Delivery (ERAS-CD) elements and recommendations (Parts 1–3) separate the surgical delivery process into a “focused” pathway with the pre-operative section (Part 1) starting at 30–60 minutes before skin incision, for both scheduled and unscheduled caesarean deliveries, but including a potential longer “optimized” pathway that manages the antenatal education and maternal comorbidities. The intraoperative section (Part 2) focuses on the time immediately prior to beginning the surgery including prophylactic antibiotics, through the caesarean surgery, to the immediate newborn care. The postoperative section (Part 3) focuses on the time from the completion of caesarean delivery until maternal discharge.18,19,48,49
The clinical maternity care has complex pathways, with increasing risk management factors that are related to obstetric comorbid medical, genetic, surgical, and lifestyle factors. Consideration for the prospective and quality assessment/improvement research, evaluation, audit, and collaboration is required for enhancement of the maternal and fetal health outcomes, quality, and safety.18,19,48,49
Understanding the caesarean delivery (CD) rate is complex as there are many factors that contribute to the overall CD rate.50,51 The Robson’s system is a classification system for caesarean deliveries, using 10 clinical groups, based on five parameters: obstetric history (parity and previous caesarean delivery), onset of labour (spontaneous, induced, or caesarean delivery before the onset of labour), fetal presentation or lie (cephalic, breech, or transverse), number of neonates, and gestational age (preterm or term). The ten Robson categories (Table 2) are mutually exclusive, totally inclusive, and can be applied prospectively, with each pregnant person that is admitted for delivery can be classified immediately, using a few variables that are generally routinely recorded.9–12,50,51 The Robson classification system helps with institution-specific monitoring and auditing but offers a standardised comparison method that can be used between institutions, countries, and timepoints.50
The Robson classification system (Table 2) has had some modifications to the original Robson groups.9–12,51 The modification has added a subclassification to categories 5–10 for pregnant people that have had a caesarean delivery but defines when, after spontaneous onset of labour, after induction of labour, or before the onset of labour:
5. Previous caesarean section, singleton, cephalic, ≥37 weeks’ gestation (5a; 5b; 5c).
6. All nulliparous with a single breech (6a; 6b; 6c).
7. All multiparous with a single breech (including previous caesarean section) (7a; 7b; 7c).
8. All multiple pregnancies (including previous caesarean section) (8a, 8b, 8c).
9. All women with a single pregnancy in transverse or oblique lie (including those with previous caesarean section) (9a; 9b; 9c).
10. All singleton, cephalic, <37 weeks’ gestation pregnancies (including previous caesarean section) (10a; 10b; 10c).
There are limitations when using the Modified Robson Criteria:51
- The classification does not allow the analysis of caesarean delivery by demand and indicated caesarean delivery for specific conditions (placenta previa).
- The classification does not account for: pre-existing medical, surgical, or fetal disease; indications for and methods used for induction of labour; and degrees of prematurity, all of which may influence the rate of caesarean delivery.
- Group 5 includes 2 clinically different groups: (1) those who planned or needed a repeat caesarean delivery, and (2) those who attempted VBAC and required caesarean delivery.
- Additional clinical factors that are not available for comparison are: maternal age; maternal BMI; specific gestational age at delivery; fetal vertex position (anterior; posterior); and birth weight.51
The American College of Surgeons National Surgical Quality Improvement Program (ACS NSQIP) is a nationally validated, risk-adjusted, outcomes-based approach to measure and improve the quality of surgical care. It employs a prospective, peer-controlled, validated database to quantify 30-day, risk-adjusted surgical outcomes, which provide a valid comparison of outcomes among all providers and hospitals in the program. ACS NSQIP utilizes the data that is:52,53
- From the patient’s medical record/chart (not from insurance claims)
- Risk-adjusted outcomes
- Case mix-adjusted outcomes (increased bench-making accuracy)
- Based on 30-day patient outcomes following the surgical exposure
ACS NSQIP has the appropriate tools, reports, analysis, and support to collect data and implement quality improvement initiatives:52,53
- Benchmarking (hospital-specific reports; comparative local and national data).
- Periodic reports and collaborative meetings are used to review and interpret data (performance information to guide surgical decision-making, identify areas for improvement that with the greatest return and highest impact).
- Access to and the use of validated practices tools (evidence-based guidelines, case studies).
- NSQIP software.
- Delivery site audits.
American College of Surgeons’ National Surgical Quality Improvement Program (NSQIP) has not been used directly for obstetrical surgery to date, but the successful implementation, in pregnant people with non-obstetrical surgical treatment, would support the obstetrical use. Annually, about 1 in 500 US individuals have a non-obstetric surgery while pregnant, most commonly appendectomy and cholecystectomy. Accurate risk assessment of non-obstetric surgery during pregnancy requires data but non-obstetric surgery during pregnancy and related complications are rare events. A study evaluated whether reproductive-aged pregnant people have a higher risk of major 30-day postoperative complications after non-obstetric surgery compared with their non-pregnant counterparts. The conclusion was that pregnant people are generally not at higher risk of major postoperative complications after non-obstetric surgery compared to their non-pregnant peers of reproductive age. It was reported that there was an increased need for blood transfusion in pregnancy and pregnancy complications were found to be increased for the less common surgical procedures such as colorectal and hernia surgeries. This study focused on maternal complications by pregnancy status, and not on pregnancy outcomes, as pregnancy outcomes are not available in NSQIP. The lack of pregnancy outcome data highlights the need for new NSQIP data additions and clinical vigilance related to any surgery during pregnancy. Continued prospective collection of surgical outcomes among pregnant women is required.52
Primary umbilical hernia repair account for 175,000 general surgery cases annually in the United States. An increased intra-abdominal pressure is a known risk factor for the development of primary umbilical hernias. Unlike groin hernias, primary umbilical hernias are far more common in women and this observation may be, at least partially related, to pregnant periods with increased intra-abdominal pressure. Review of the ACS-NSQIP database found that the incidence of umbilical hernia repair during pregnancy is very low, but for pregnant people who required an unscheduled repair, the majority had a bowel incarceration with strangulation. When the acute symptoms develop, umbilical hernias can be repaired with minimal 30-day morbidity to the mother. Additional studies are needed to determine the long-term recurrence rate of umbilical hernia repairs performed in pregnant patients and to better understand the effects of surgical intervention on the fetus.53
Perinatal Outcomes Following a Quality and Safety Implementation
In Caesarean Delivery/Obstetrical Surgery
The REDUCED Trial was based on the clinical assumption that reducing CD in nulliparous women would reduce the overall CD rate. The study aim was to assess whether adoption of a new guideline for diagnosing non-progressing labor would reduce the CD rate. This was a cluster randomized trial with the primary outcome being the rate of CD in nulliparous women with vertex presentation in labor at term. The secondary outcomes included spontaneous vaginal birth and maternal and neonatal safety. Data source was the APHP database. The outcome was that the CD rates in nulliparous women were not reduced following new guidelines for the diagnosis of nonprogressive labor. Spontaneous vaginal delivery was increased in the intervention group. The intervention was found to be safe.54,55
A retrospective study based in a tertiary obstetrical care hospital in India assessed the frequency and indications of CD using the Robson classification. From a cohort of 10,282 births, the overall CD rate was 35.2%. The study identified that group 5 with 11% (multiparous women with previous lower segment CD), group 2 with 8.6% (nulliparous women with labor induced or pre-labor CD), and group 4 with 5.5% (multiparous women without previous CD were induced or taken for pre-labor CD). The process to reduce CD identified that increasing use of VBAC is required, performing effective pelvic exams, and encourage the use of external fetal versions (breech to vertex).56
Country comparison of CD rates within the Robson classification allows insight into the areas of difference to identify innovation and/or educational correction. While the Robson classification has become a global standard for comparing and monitoring caesarean delivery (CD) rates across populations and over time; however, it does not account important maternal, fetal, and obstetric factors known to impact CD rates. The CD rate in Sweden was stable at 17.0% from 2004 to 2016 (p for trend = 0.10), while the CD rate increased in BC from 29.4% to 33.9% (p for trend <0.001). Differences in CD rates between Sweden and BC varied by Robson group.57
- Group 1 (nullipara with a term, single, cephalic fetus with spontaneous labor), the CD rate was 8.1% in Sweden and 20.4% in BC (rate ratio [RR] for BC versus Sweden = 2.52, 95% confidence interval [CI] 2.49 to 2.56, p < 0.001).
- Group 2 (nullipara, single, cephalic fetus, term gestation with induction of labor or pre-labor CD), the rate of CD was 37.3% in Sweden and 45.9% in BC (RR = 1.23, 95% CI 1.22 to 1.25, p < 0.001).
The effect of adjustment between countries varied by Robson group from having no effect in some groups to explaining up to 61% of the variation in CDs in others. Adjustment for maternal, fetal, and obstetric practice factors explained a substantial fraction of the temporal change in CD rates among some Robson groups in Canada but had little impact on temporal changes in CD rates among Robson groups in Sweden. Comprehensive and accurate perinatal data collection beyond the Robson criteria is necessary to ensure policies regarding CD rates are suitably evidence informed and prioritized.57
In VBAC/TOLAC
Factors and barriers to TOLAC/ VBAC choice indicated that the majority were systematic and interpersonal. These barriers varied across levels of influence and included restrictive clinical guidelines, provider reluctance, geographic disparities, and midwifery scopes of practice.58
A multi-faceted intervention including audits, feedback to health professionals, and implementation of best practice did not affect VBAC rates or maternal and neonatal morbidity. Recommendations indicated the need for decision-making processes and risk management tools specifically for TOLAC /VBAC.59
Hospital factors associated with maternal and neonatal outcomes of deliveries to patients with a previous CD (ecological study) identified that adverse maternal and neonatal outcomes showed no clear pattern of decreasing SMMM and SNMM with increasing tiers of service and hospital volume. Continued review and surveillance is recommended to monitor the rates of maternal and neonatal outcomes.60
Decision aid and educational/ motivational guideline implementations have shown a significant reduction in practice variation without an increase in CD or complications and increased VBAC rates and neonatal well-being, respectively.61,62
In Operative Vaginal Delivery
In Canada, rates of trauma following OVD are higher than previously reported, irrespective of region, levels of obstetric care and volume of OVD among hospitals. From a cohort of greater than 1.3 million deliveries, forceps were used in 2.9% and vacuums were used in 8.4%. For forceps, maternal trauma was 25.3% (24.8–25.7) and neonatal trauma was 9.6% (8.6–10.6) per 1000 LB. For vacuum, maternal trauma rate was 13.2% (13.0–13.4) and neonatal trauma was 9.6% (9.0–10.2) per 1000 LB. Adjusted analysis maintained the higher trauma rate for regions but not hospital levels.63
The use of intrapartum ultrasound verses routine assessment prior to instrumental vaginal delivery found that ultrasound was associated with a lower rate incorrect evaluation of fetal head position and station but with no improvement in maternal and neonatal outcomes.64
The rates of obstetric anal sphincter injury (OASI), associated with OVD and vaginal delivery, initiated the development of OASI – Care Bundles (4 practices: antenatal discussion, manual perineal protection, mediolateral episiotomy, systematic examination after vaginal birth). Post implementation outcomes found reduced OASI rates but identified barriers and enablers to implementation with four themes impacting OASI-CB adoption (method of implementation; opportunities for use; responsiveness to change; perceptions of “what women want”).65
In Placenta Accreta Spectrum
A primary management process requires an antenatal diagnosis of PAS as identification of PAS is needed to optimize maternal outcomes and arrange the delivery at level III or IV maternal care facility. Imaging by ultrasound and magnetic resonance imaging (MRI) development enable the antenatal diagnosis of PAS. Although ultrasonographic features of PAS may be seen as early as the first trimester; most women are not diagnosed during their 2nd or 3rd trimesters.7,66–68
Ultrasound is the primary imaging tool for the assessment of PAS. MRI serves as a complementary imaging technique to assist with the depth and extent of the myo-invasion into the uterus. This source provides a consensus statement and a pictorial review of the seven major MRI features for use in diagnosis and management.69
A panel of FIGO experts has consensually proposed a new classification and guidelines criteria for the pathologic diagnosis of PAS diseases:70–75
Placenta Accreta Spectrum (PAS) Grades (1–3).
- PAS Grade 1: Non-invasive morbidly adherent placenta (placenta accreta): Myometrial sections display a clear and complete placental–myometrial boundary and uniform myometrial thickness without thinning.
- PAS Grade 2: Superficial invasion of the placenta (placenta increta): Myometrial sections display an irregular placental–myometrial interface without the outer myometrium (with conservation of at least 25% of the wall thickness relative to the detached myometrium).
- PAS Grade 3A: Deep invasion of the placenta: Myometrial sections display an irregular placenta–myometrial interface with involvement of the outer myometrium (with conservation of less than 25% of the wall thickness relative to the detached myometrium). The serosa is completely safe (A = Abnormal invasion).
Grade 3D: Deep invasion of the placenta with disturbance of the serosa (placenta percreta): grossly invasive placenta with disruption of the uterine serosa surface (D = Deep invasion).
Grade 3E: Deep invasion of the placenta with adherent extra uterine tissues and organs: placental invasion into nearby organs (commonly the bladder) or extra-uterine fibro adipose tissues, confirmed by microscopy (E = Extra uterine invasion).
A patient -safety bundle for PAS management includes betamethasone, gynecologic oncology intra-operative consult, pre-operative balloon catheters, cell salvage technology in the OR, vertical skin incision, fundal or high transverse hysterotomy. This study indicated greater compliance to the use of all components after the introduction of the protocol (0 vs 41%; p < 0.0001) but the maternal and post-operative outcomes were not significantly different between groups. Factors were considered such as limited number of cases, retrospective design, and single center. The authors indicated while the safety bundles are important, they may not be formulaic, nor should they be proposed as a mandatory approach.76–78
Another center’s multidisciplinary collaboration focus has been on providing best/better available practices across a range of aspects of surgical care, resulting in the Toronto PAS care bundles.79 Among the 105 consecutive patients identified, there were 26 in the initial period and 32 in the current period. With the implementation of all QI care bundles, median estimated surgical blood loss halved from 2000 mL in the initial period to 1000 mL in the current period, and fewer patients required allogenic blood transfusion (61.5% vs 25%). Patients in the current period demonstrated improved postoperative levels of hemoglobin compared to those in the initial period (101 g/L vs 89 g/L) and had a shorter median postoperative hospital stay (3 days vs 5 days):79
1. Standardized care bundle: building a robust core diagnostic and management team, routinely using both specialist ultrasound (by experienced perinatal sonologists) and magnetic resonance imaging (MRI) (by experienced perinatal radiologists) to aid in diagnostic accuracy and surgical planning, use of programmatic clinical care pathways (including electronic medical record order sets to force function), all-inclusive surgical briefings, following a uniform surgical approach to caesarean hysterectomy, with a focus on minimizing blood loss and complications, together with adherence to contemporary guidelines on enhanced recovery after surgery.
2. Patient blood management bundle: optimization of preoperative iron and hemoglobin, routine perioperative use of the antifibrinolytic tranexamic acid, routine use of intraoperative cell salvage to reduce the need for allogenic (donor) blood transfusion, active communication between the surgical and anesthesia teams before blood transfusion and occlusion of the internal iliac artery (IIA) with balloon tamponade or surgical ligation.
3. Comprehensive self-audit bundle: achieved through longitudinal postoperative follow-up, data collection, and monthly multidisciplinary team meetings to discuss past and future cases of PAS, identification of what is working well and actively seeking areas for improvement.
4. Research and knowledge translation bundle: through the implementation of a comprehensive database of PAS disorders facilitating all current and future studies in the study institution, leading the national development of guidelines for PAS disorders, along with an overarching aim to proactively collaborate nationally and internationally to improve care and outcomes for patients and their infants with this disorder.
Additional uterine scar/placental morbidity results from blastocyst implantation in the previous hysterotomy scar with a reported incidence of 1 per 1800—2226 of overall pregnancies. Anterior myometrial thickness at the implantation site and the gestational sac diameter were identified as independent risk factors for intraoperative hemorrhage during the treatment of the caesarean scar ectopic pregnancy. A new classification type I–III uses the myometrial thickness and sac/mass diameter to define the risk with a surgical recommendation.80
Discussion
The obstetric surgery results have focused on the evidence from four obstetrical surgery areas thereby providing support for the value of diagnosis, measurement, audit, and information sharing to enhance quality and safety for the pregnant person and neonatal obstetrical care. Health care knowledge transfer via guidelines or protocols and then the subsequent clinical implementation into the clinical care pathway is difficult. Clinical funding, multi-disciplinary human resource needs, clinical acceptance are required, at many administrative and clinical levels, for the change, and the subsequent proof of value or return on investment (ROI) are to be identified. Surveillance processes, implementation processes and the recognized implementation barriers are summarized (Tables 581,82 and 6).83 These opportunities and barriers require continued oversight and support throughout the perinatal care period. The implementation process choices that have been used and the priorities to increase success are summarized (Table 5). The three implementation themes/barriers are the personal factors, the level of change required evidence (increases the likelihood of success), and the external factors are important to understand for the PSDA cycle (Table 6).83 There are many additional obstetrical surgery factors which require support for ongoing obstetrical surgery excellence (Table 7).4,6,7,60,63,69,79,84–86
 |
Table 5 Potential Implementation Strategy Considerations |
 |
Table 6 Barriers, Interventions, and Strategies in Guideline Implementation83 |
 |
Table 7 Additional Evidenced-Based Quality Impact Areas |
Guidelines have shown to be an effective strategy for improving health outcomes and processes of care in medicine.87 In addition, the guidelines are useful in decreasing the clinical care gap between research and current practice with the goal to reduce inappropriate variability in practice [Fischer 85]. Development of practice guidelines does not necessarily guarantee health care provider adoption and adherence in practice.
Despite all the guidelines and knowledge translation efforts of the past 30 years, the healthcare delivery system continues to provide measures of underperformance.88 Care in-line with guidelines is at 60% as shown by large national empirical studies of multiple conditions in adults and children. Some care is found to have waste, duplication, or of low value in 30%, according to several authoritative sources, with considerable expenditure. Many studies have documented iatrogenic harm or adverse events in at least 10% of patients globally.89–91
Despite these benefits, the implementation of guidelines is both complex, varied, and needs health system support in human resources and fiscal areas.92–95 While the learning model is appealing, there is no guarantee. In healthcare, some processes are quickly accepted and embedded (laparoscopic techniques, day only surgery) while other processes have been slow in adoption (patient involvement in decision-making, various level 1 evidence). Where innovation will create options, the learning health systems will need to spread, principally through diffusion of innovation models and local adaptations. Presently, the learning health system model represents the best option for changing the “60/30/10” outcomes but new decisions are needed. Health care is investing in biomedical and technological advances that promise safer, affordable, more effective healthcare. Big C change is required but until that time the process needs to have provider accountability using fit-for-purpose, responsive, and evidence-based delivery models that are built to learn and to correspond, in size or degree, with the local complex health system view of healthcare.89
Conclusions
The four obstetrical surgery areas, caesarean delivery, vaginal birth after caesarean delivery/trial of labor after caesarean, operative vaginal delivery, and placenta accrete spectrum, have significant impact on quality, safety, and informed choice for maternal-fetal-neonatal outcomes. The understanding and recognition of the non-clinical patient factors of equity and trauma informed care and the clinical system culture is required at the beginning of the process. Use of surveillance, audit, and feedback systems for providers is required for the understanding, measurement, and implementation of clinical care improvement.
The original questions of “why, what, how” for excellence in obstetrical surgery are answered in this focused review but the recognition, process, and cost of clinical change are difficult. Surgeons are capable of change as shown with the implementation of checklists, protocol-based care, and measurement-audit-feedback processes. Implementation and understanding of the barriers to quality improvement and safety change requires provider engagement and health care system coordination.
Health care systems and obstetrical surgery care cannot afford, not to implement “bottom-up/top-down” processes for quality and safety, as patients will demand quality and safety but the lawyers should not have to enforce it.
Acknowledgment
No funding or AI was used in this work.
Disclosure
The author reports no conflicts of interest in this work.
References
1. Betran AP, Ye J, Moller A-B, et al. Trends and projections of caesarean section rates: global and regional estimates. BMJ Global Health. 2021;6(6):e005671. doi:10.1136/bmjgh-2021-005671
2. Wu ML, Nichols PM, Cormick G, Betran AP, Gibbons L, Belizan JM. Global inequities in cesarean section deliveries and required resources persist. Eur J Obstet Gynecol. 2023;285:31–40. doi:10.1016/j.ejogrb.2023.03.036
3. Turner MJ. Delivery after a previous cesarean section reviewed. Int J Gynecol Obstet. 2023:1–6. doi:10.1002/ijgo.14854
4. Bruno AM, Allshouse AA, Metz TD. Trends in attempted and successful trial of labor after cesarean delivery in the United States From 2010 to 2020. Obstet Gynecol. 2023;141:173–175. doi:10.1097/AOG.0000000000004998
5. Operative vaginal birth. ACOG practice bulletin No. 219. American College of Obstetricians and Gynecologists. Obstet Gynecol. 2020;135:e149–59. doi:10.1097/AOG.0000000000003764
6. Panelli DM, Leonard SA, Joudi N, et al. Clinical and physician factors associated with failed operative vaginal delivery. Obstet Gynecol. 2023;141:1181–1189. doi:10.1097/AOG.0000000000005181
7. Maged AM, El-Mazny A, Kamal N, et al. Diagnostic accuracy of ultrasound in the diagnosis of placenta accreta spectrum: systematic review and meta-analysis. BMC Pregnancy Childbirth. 2023;23:354. doi:10.1186/s12884-023-05675-6
8. Abdel Wahab M, Cackovic M. Placenta accreta spectrum and postpartum hemorrhage. Clin Obstet Gynecol. 2023. doi:10.1097/GRF.0000000000000783
9. Campos MG, Franco-Sena AB, Rebelo F. Direct standardization method according to Robson classification for comparison of cesarean rates. BMC Pregnancy Childbirth. 2023;23:117. doi:10.1186/s12884-023-05416-9
10. Roberge S, Dubé E, Blouin S, Chaillet N. Reporting caesarean delivery in Quebec using the Robson classification system. J Obstet Gynaecol Can. 2017;39(3):152e156. doi:10.1016/j.jogc.2016.10.0102017
11. Quibel T, Rozenberg P, Bouyer C, Bouyer J. Variation between hospital caesarean delivery rates when Robson’s classification is considered: an observational study from a French perinatal network. PLoS One. 2021;16(8):e0251141. doi:10.1371/journal.pone.0251141
12. Glaxi P, Gourounti K, Vivilaki V, et al. Implementation of the Robson classification in Greece: a retrospective cross-sectional study. Healthcare. 2023;11:908. doi:10.3390/healthcare11060908
13. Saccone G, Angelis MC, Zizolfi B, et al. Monofilament vs multifilament suture for uterine closure at the time of cesarean delivery: a randomized clinical trial. Am J Obstet Gynecol. 2022;4:1005592. doi:10.1016/j.ajogmf.2022.100592
14. Khanuja K, Burd J, Ozcan P, Peleg D, Saccone G. Suture type for hysterotomy closure: a systematic review and meta-analysis of randomized controlled trials. Am J Obstet Gynecol. 2022;4:100726. doi:10.1016/j.ajogmf.2022.100726
15. Raischer HB, Massalha M, Iskander R, Izhaki I, Salim R. Knotless barbed versus conventional suture for closure of the uterine incision at cesarean delivery: a systematic review and meta-analysis. J Min Invasive Gynecol. 2022;29:832–839. doi:10.1016/j.jimg.2022.05.001
16. Agarwal S, D-Souza R, Ryu M, Maxwell C. Barbed vs conventional suture at cesarean delivery: a systematic review and meta-analysis. Acta Obstet Gynecol Scand. 2021;100:1010–1018. doi:10.1111/aogs.14080
17. Roberge S, Demers S, Berghella V, Chaillet N, Moore L, Bujold E. Impact of single- vs double-layer closure on adverse outcomes and uterine scar defect: a systematic review and meta-analysis. Am J Obstet Gynecol. 2014;211:453–460. doi:10.1016/j.ajog.2014.06.014
18. Fay E, Sultan P, Bollag L. Cesarean delivery. In: Nelson G, Ramirez PT, Dowdy SC, Wilson RD, Scott MJ, editors. The ERAS Society Handbook for Obstetrics and Gynecology. Academic Press; 2022. ISBN 978-0-323-91208-2; Surgical Techniques. 261.
19. Caughey AB, Stephen L, Wood SL, et al. Guidelines for intraoperative care in caesarean delivery: enhanced recovery after surgery society recommendations (Part 2). Amer J Obstet Gynecol. 2018. doi:10.1016/j.ajog.2018.08.006
20. Marchand GJ, Masoud A, Ruther S, et al. Effect of single- and double-layer cesarean section closure on residual myometrial thickness and isthmocele- A systematic review and meta-analysis. Turk J Obstet Gynecol. 2021;18:322–332. doi:10.4246/tjog.galenos.2021.71173
21. Qayam K, Kar I, Sofi J, Panneerselvam H. Single-verses double-layer uterine closure after cesarean section delivery: a systematic review and meta-analysis. Cureus. 2021;13(9):e18405. doi:10.7759/cureus.18405
22. Stegwee HB, Jordans IPM, van der Voet LF, et al. Uterine caesarean closure techniques affect ultrasound findings and maternal outcomes: a systematic review and meta-analysis. BJOG. 2018;125:1097–1108. doi:10.1111/1471-0528.15048
23. Di Spiezo Sardo A, Saccone G, McCurdy R, Bujold E, Bifulco G, Bergella V. Risk of Cesarean scar defect following single- vs double-layer uterine closure: systematic review and meta-analysis of randomized controlled trials. Ultrasound Obstet Gynecol. 2017;30:578–583. doi:10.1002/uog.17401
24. Huire JAF, Stegwee SI, van der Voet LF, de Groot CJM, Hehenkamp WJK, Brolmann HAM. Risk of Cesarean scar defect following single- vs double-layer uterine closure. Ultrasound Obstet Gynecol. 2017;50:662–668. doi:10.1002/uog.18893
25. Bubny-Winska J, Zimmer-Stelmach A, Pomorski M. Impact of selected risk factors on uterine healing after cesarean section in women with single-layer uterine closure: a prospective study using two- and three-dimensional transvaginal ultrasonography. Adv Clin Exp Med. 2022;31(1):41–48. doi:10.17219/acem/142519
26. Kalem Z, Kaya AE, Bakirarar B, Basbug A, Kalem MN. An optimal uterine closure technique for better scar healing and avoiding isthmocele in cesarean section: a randomized controlled trial. J Invest Surg. 2021;34(2):148–156. doi:10.1080/08941939.2019.1610530
27. Tahermanesh K, Mirgalobayat S, Aziz-Ahari A, et al. Babu and Magon uterine closure technique during cesarean section: a randomized double-blind trial. J Obstet Gynaecol Res. 2021;47(9):3186–3195. doi:10.1111/jog.14889
28. Madhavi BK. Letter to “Babu and Magon uterine closure technique during cesarean section: a randomized double-blind trial”. J Obstet Gynaecol Res. 2021;47(12):4504–4505. doi:10.1111/jog.15026
29. Elkhouly NI, Abdelaal NK, Solyman AE, Elkelani OA, Elbasueny BF, Elhalaby AF. A new technique for uterine incision closure at the time of caesarean section: does it make a difference? J Obstet Gynaecol. 2022;42(3):416–423. doi:10.1080/01443615.2021.1910636
30. Erkayiran U, Arslanca T. Comparative analysis of classical primary continuous and novel technique uterine suturing methods on uterine scar formation after caesarean section: a prospective clinical study. Gynekologia Polska. 2022;93(7):552–557. doi:10.5603/GP.a2022.002
31. Arakaza A, Zou L, Zhu J. Placenta accreta spectrum diagnosis challenges and controversies in current obstetrics: a review. Int J Women’s Health. 2023;15:635–654. doi:10.2147/IJWH.S395271
32. Ramlakhan J, Foster AM, Grace SL, et al. What constitutes patient-centred care for women: a theoretical rapid review. Int J Equity Health. 2019;18:182. doi:10.1186/s12939-019-1048-5
33. Meiman J, Grobman WA, Haas DM, et al. Association of neighbourhood socioeconomic disadvantage and postpartum readmission. Obstet Gynecol. 2023;141(5):967–970. doi:10.1097/AOG.0000000000005151
34. Kern-Goldberger AR, Srinivas SK. Editorial: variation as evidence of preventability. Obstet Gynecol. 2023;141(5):875–876. doi:10.1097/AOG.0000000000005162
35. Admon LK, Auty SG, Daw JR, et al. State variation in severe maternal morbidity among individuals with Medicaid insurance. Obstet Gynecol. 2023;141(5):877–885. doi:10.1097/AOG.0000000000005144
36. Druyan B, Platner M, Jamieson DJ, Boulet SL. Severe maternal morbidity and postpartum readmission through one year. Obstet Gynecol. 2023;141(5):949–955. doi:10.1097/AOG.0000000000005150
37. Howell EA, Brown H, Brumley J, et al. Reduction of peripartum racial and ethnic disparities: a conceptual framework and maternal safety consensus bundle. Obstet Gynecol. 2018;131(5):770–782. doi:10.1097/AOG.0000000000002475
38. Howell EA, Ahmed ZN. Eight steps for narrowing the maternal health disparity gap: step-by-step plan to reduce racial and ethnic disparities in care. Contemp Ob Gyn. 2019;64(1):30–36. doi:10.1001/jama.2018.1150
39. Howell EA, Brown H, Brumley J, et al. Reduction of peripartum racial and ethnic disparities: a conceptual framework and maternal safety consensus bundle. JOGNN. 2018;47:275–289. doi:10.1016/j.jogn.2018.03.004
40. Grechukkina O, Lipkind HS, Lundsberg LS, et al. Severe maternal morbidity review and preventability assessment in a large academic center. Obstet Gynecol. 2023;141(4):875–880. doi:10.1097/AOG.0000000000005116
41. Kilpatrick SK, Ecker JL, Callaghan WM. Severe maternal morbidity screening and review. Obstetric care consensus No. 5. American College of Obstetricians and Gynecologists. Obstet Gynecol. 2016;128:e54–60.
42. Harvard Health Publishing. Trauma-informed care: What it is, and why it’s important. Available from: https://www.health.harvard.edu/blog/trauma-informed-care-what-it-is-and-why-its-important-2018101613562.
43. Wilson RD. The real maternal risks in a pregnancy: a structured review to enhance maternal understanding and education. J Obstet Gynaecol Can. 2019. doi:10.1016/j.jogc.2019.12.005
44. Hui L, Ellis K, Mayen D, et al. Position statement from the International Society for Prenatal Diagnosis on the use of non-invasive prenatal testing for the detection of fetal chromosomal conditions in singleton pregnancies. Prenat Diagnosis. 2023;43:814–828. doi:10.1002/pd.6357
45. APHP. Quality & Innovation. Available from: https://www.albertahealthservices.ca/info/Page16940.aspx.
46. Crowl A, Sharma A, Sorge L, Sorensen T. Accelerating quality improvement within your organization: applying the Model for Improvement. J Am Pharm Assoc. 2015;55(4):e364–74. doi:10.1331/JAPhA.2015.15533
47. Schwendimann R, Blatter C, Lüthy M, et al. Adherence to the WHO surgical safety checklist: an observational study in a Swiss academic center. Patient Safe Surg. 2019;13:14. doi:10.1186/s13037-019-0194-4
48. Wilson RD, Caughey AB, Wood SL, et al. Guidelines for antenatal and preoperative care in cesarean delivery: enhanced recovery after surgery society recommendations (Part 1). Am J Obstet Gynecol. 2018;219:523.e1–523.e15. doi:10.1016/j.ajog.2018.09.015
49. Macones GA, Caughey AB, Wood SL, et al. Guidelines for postoperative care in cesarean delivery: enhanced Recovery After Surgery (ERAS) Society recommendations (part 3). Am J Obstet Gynecol. 2019;221:247.e1–9. doi:10.1016/j.ajog.2019.04.012
50. Vogel JP, Betrán AP, Vindevoghel N, et al. Use of the Robson classification to assess caesarean delivery in 21 countries: a secondary assessment of two WHO multi-country surveys. Lancet Global Health. 2015;3:e260–e270. doi:10.1016/S2214-109X(15)70094-X
51. Farine D, Shepherd D, Robson M, et al. Classification of Caesarean Sections in Canada: the Modified Robson Criteria. J Obstet Gynaecol Can. 2012;34(10):976–979. doi:10.1016/S1701-2163(16)35412-3
52. Abdelwahab M, Lynch CD, Schneider P, et al. Postoperative complications after non-obstetric surgery among pregnant patients in the National Surgical Quality Improvement Program, 2005-2012. Am J Surg. 2022;223(2):364–369. doi:10.1016/j.amjsurg.2021.04.002
53. Haskins IN, Rosen MJ, Prabhu AS, et al. Umbilical hernia repair in pregnant patients: review of the American College of Surgeons National Surgical Quality Improvement Program. Hernia. 2017;21:767–770. doi:10.1007/s10029-017-1633-8
54. Wood S, Skiffington J, Brant R, et al. The REDUCED Trial. A cluster randomized trial REDucing the Utilization of CEsarean Delivery for Dystocia. Am J Obstet Gynecol. 2022. doi:10.1016/j.ajog.2022.10.038
55. Lauterbach R, Justman N, Ginsberg Y, et al. The impact of extending the second stage of labor on repeat cesarean section and maternal and neonatal outcomes. Int J Gynecol Obstet. 2023;163:594–600. doi:10.1002/ijgo.14855
56. Janani L, Christina S, Akoijam BS, Nameirakpam D, Laiphrakpam RS. Analysis of cesarean section rates and its indications using robson’s classification at a tertiary care hospital, Manipur. Indian J Public Health. 2022;66(4):434–438. doi:10.4103/ijph.ijph_1928_21
57. Murraca GM, Joesp KS, Razaz N, Ladfors LV, Lisonkova S, Stephansson O. Crude and adjusted comparisons of cesarean delivery rates using the Robson classification: a population-based cohort study in Canada and Sweden, 2004 to 2016. PLoS Med. 2022;19:e1004077. doi:10.1371/journalpmed.1004077
58. Egan MB, Petrey J, Robertson P, Curmutte M, Jennings JAC. An exploration of barriers to access to trial of labor and vaginal birth after caesarean in the United States: a scoping review. J Perinat Med. 2023;51:981–991. doi:10.1515/jpm-2022-0364
59. Roberge S, Boutin A, Bujold E, Dube E, Blouin S, Chaillet N. Impact of audits and multifaceted intervention on vaginal birth after caesarean: secondary analysis of the QUARISMA trail. J Obstet Gynecol Can. 2019;41:608–615. doi:10.1016/j.jogc.2018.05.044
60. Joseph KS, Young CB, Muraca GM, et al. Hospital factors associated with maternal and neonatal outcomes of deliveries to patients with a previous caesarean delivery: an ecological study. CMAJ. 2023;195:E178–86. doi:10.1503/cmaj.220928
61. Koppes DM, van Hees MSF, Koenders VM, et al. Nationwide implementation of a decision aid on vaginal birth after cesarean: a before and after cohort study. J Perinat Med. 2021;49(7):783–790. doi:10.1515/jpm-2021-0007
62. Monari F, Menichini D, Bertucci E, Neri I, Perrone E, Facchinetti F. Implementation of Guidelines about women with previous cesarean section through educational/motivational interventions. Int J Gynecol Obstet. 2022;159:810–816. doi:10.1002/ijgo.14212
63. Muraca GM, Boutin A, Razaz N, et al. Maternal and neonatal trauma following operative vaginal delivery. CMAJ. 2022;194:E1–12. doi:10.1503/cmaj.210841
64. Mappa I, Tartaglia S, Maquina P, et al. Ultrasound vs routine care before instrumental vaginal delivery: a systematic review and meta-analysis. Acta Obstet Gynecol Scand. 2021;100:1941–1948. doi:10.1111/aogs.14236
65. Jurczuk M, Bidwell P, Gurol-Urganci I, et al. The OASI care bundle quality improvement project: lessons learned and future directions. Inter Urogynecol J. 2021;32:1989–1995. doi:10.1007/s00192-021-04786-y
66. ACOG. Placenta accreta spectrum. Obstetric Care Consensus No 7. Obstet Gynecol. 2018;132:e259–75. doi:10.1097/AOG.0000000000002983
67. Shimshinaz AA, Fox KA, Salmanian B, et al. Maternal morbidity in patients with morbidly adherent placenta treated with and without a standardized multidisciplinary approach. Am J Obstet Gynecol. 2015;212(2):218.e1–9. doi:10.1016/j.ajog.2014.08.019
68. Gatta LA, Boyd BK, Einerson BD, et al. Validation of a sonographic checklist for the detection of histologic placenta accreta spectrum. AJOGMF. 2023. doi:10.1016/j.ajogmf.2023.101017
69. Patel-Lippmann KK, Planz VB, Phillips CH, Ohlendorf JM, Zuckerwise LC, Moshiri M. Placenta accreta spectrum disorders: updates and pictorial review of the SAR-ESUR Joint Consensus Statement for MRI. Radiographics. 2023;43(5):e220090. doi:10.1148/rg.220090
70. Jauniaux E, Ayres-de-Campos D, Langhoff-Roos J, Fox KA, Collins S. FIGO classification for the clinical diagnosis of placenta accreta spectrum disorders. FIGO Placenta Accreta Diagnosis and Management Expert Consensus Panel. Int J Gynecol Obstet. 2019;146:20–24. doi:10.1002/ijgo.12661
71. Jauniaux E, Ayres-de-campos D. FIGO consensus guidelines on placenta accreta spectrum disorders: introduction. FIGO Placenta Accreta Diagnosis and Management Expert Consensus Panel. Int J Gynaecol Obstet. 2018;140(3):261–264. doi:10.1002/ijgo.12406
72. Jauniaux E, Chantraine F, Silver RM, Langhoff-Roos J. FIGO consensus guidelines on placenta accreta spectrum disorders: epidemiology. FIGO Placenta Accreta Diagnosis and Management Expert Consensus Panel. Int J Gynaecol Obstet. 2018;140(3):265–273. doi:10.1002/ijgo.12407
73. Sentilhes L, Kayem G, Chandraharan E, Palacios-Jaraquemada J, Jauniaux E. FIGO consensus guidelines on placenta accreta spectrum disorders: conservative management. FIGO Placenta Accreta Diagnosis and Management Expert Consensus Panel. Int J Gynaecol Obstet. 2018;140(3):291–298. doi:10.1002/ijgo.12410
74. Jauniaux E, Bhide A, Kennedy A, Woodward P, Hubinont C, Collins S. FIGO consensus guidelines on placenta accreta spectrum disorders: prenatal diagnosis and screening. FIGO Placenta Accreta Diagnosis and Management Expert Consensus Panel. Int J Gynaecol Obstet. 2018;140(3):274–280. doi:10.1002/ijgo.12408
75. Allen L, Jauniaux E, Hobson S, Papillon-Smith J, Belfort MA. FIGO consensus guidelines on placenta accreta spectrum disorders: nonconservative surgical management. FIGO placenta accreta diagnosis and management expert consensus panel. Int J Gynaecol Obstet. 2018;140(3):281–290. doi:10.1002/ijgo.12409
76. Quist-Nelson J, Crank A, Oliver EA, et al. The compliance with a patient-safety bundle for management of placental accreta spectrum. J Maternal Fetal Neonat Med. 2019;34:17,2880–2886. doi:10.1018/14767058.2019.1671349
77. Nieto-Calvache AJ, Palacios-Jaraquemada JM, Vergara-Galliadi LM, et al. All maternal deaths related to placenta accreta spectrum are preventable: a difficult-to-tell reality. Am J Obster Gynecol Glob Rep. 2021;1:100012. doi:10.1016/j.xagr.2021.100012
78. Nieto-Calvache AJ, Trevino PM, Garcia de laTorre JI. Gomz Priorities for improving care in the placenta accreta spectrum. Int J Gynecol Obstet. 2022;157:198–209. doi:10.1002/ijog.14011
79. Hobson SR, Kingdom JCP, Windrim RC, et al. Safer outcomes for placenta accreta spectrum disorders: a decade of quality improvement. Int J Gynecol Obstet. 2022;157:130–139. doi:10.1002/ijgo.13717
80. Ban Y, Shen J, Wang X, et al. Cesarean scar ectopic pregnancy clinical classification system with recommended surgical strategy. Obstet Gynecol. 2023;141(5):927–936. doi:10.1097/AOG.0000000000005113
81. Peters S, Sukumar K, Blanchard S, et al. Trends in guideline implementation: an updated scoping review. Implement Sci. 2022;17:50. doi:10.1186/s13012-022-01223-6
82. Powell BJ, Fernandez ME, Williams NJ, et al. Enhancing the impact of implementation strategies in healthcare: a research agenda. Front Public Health. 2019;7(3). doi:10.3389/fpubh.2019.0000
83. Fischer F, Lange K, Klose K, Greiner W, Kraemeret A. Barriers and strategies in guideline implementation—a scoping review. Healthcare. 2016;4:36. doi:10.3390/healthcare4030036
84. Vaajala M, Liukkonen R, Ponkilainen V, Kekki M, Mattila VM, Kuitunen I. The rates of vaginal births after cesarean section have increased during the last decades: a nationwide register-based cohort study in Finland. Arch Gynecol Obstet. 2023;308:157–162. doi:10.1007/s00404-023-07010-y]
85. Wen SW, Kramer MS. Uses of ecologic studies in the assessment of intended treatment effects. J Clin Epidemiol. 1999;52(1):7–12. doi:10.1016/s0895-4356(98)00136-x
86. Kane D, Wall E, Malone E, et al. A retrospective cohort study of the characteristics of unsuccessful operative vaginal deliveries. Eur J Obstet Gynecol Reprod Biol. 2023;26(285):159–163. doi:10.1016/j.ejogrb.2023.04.02
87. Gundersen L. The effect of clinical practice guidelines on variations in care. Ann Intern Med. 2000;133(4):317–318. doi:10.7326/0003-4819-133-4-200008150-00102
88. Braithwaite J, Glasziou P, Westbrook J. The three numbers you need to know about healthcare: the 60-30-10 challenge. BMC Med. 2020;18(1):102. doi:10.1186/s12916-020-0156
89. Braithwaite J. Changing how we think about healthcare improvement. BMJ. 2018;361:k2014. doi:10.1136/bmj.k2014
90. OECD. Tackling Wasteful Spending on Health. Paris: OECD Publishing; 2017.
91. National Academies of Sciences Engineering and Medicine, Health and Medicine Division, Board on Health Care Services, Board on Global Health, Committee on Improving the Quality of Health Care Globally. Crossing the Global Quality Chasm: Improving Health Care Worldwide. Washington DC: National Academies Press (US); 2018.
92. Cassidy CE, Harrison MB, Godfrey C, et al. Use and effects of implementation strategies for practice guidelines in nursing: a systematic review. Implementation Science. 2021;16:102. doi:10.1186/s13012-021-01165-5
93. Grol R. Successes and failures in the implementation of evidence-based guidelines for clinical practice. Med Care. 2001;39(8 Suppl 2):II46–54. doi:10.1097/00005650-200108002-00003
94. Rycroft-Malone J, Burton CR, Wilkinson J, et al. Collective action for implementation: a realist evaluation of organisational collaboration in healthcare. Implement Sci. 2016;11(1):17. doi:10.1186/s13012-016-0380-z
95. Sheldon TA, Cullum N, Dawson D, et al. What’s the evidence that NICE guidance has been implemented? Results from a national evaluation using time series analysis, audit of patients’ notes, and interviews. BMJ. 2004;329(7473):999. doi:10.1136/bmj.329.7473.999
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
