Back to Journals » Integrated Pharmacy Research and Practice » Volume 11
Evaluation of Potential Drug Interactions with AiDKlinik® in a Random Population Sample
Authors Schmidberger J , Kloth C, Müller M, Kratzer W, Klaus J
Received 9 December 2021
Accepted for publication 16 February 2022
Published 12 March 2022 Volume 2022:11 Pages 61—69
DOI https://doi.org/10.2147/IPRP.S351938
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Professor Jonathan Ling
Julian Schmidberger,1 Christopher Kloth,2 Martin Müller,1 Wolfgang Kratzer,1 Jochen Klaus1
1Department of Internal Medicine I, University Hospital Ulm, Ulm, Baden-Württemberg, Germany; 2Department of Diagnostic and Interventional Radiology, University Hospital Ulm, Ulm, Baden-Württemberg, Germany
Correspondence: Wolfgang Kratzer, Department of Internal Medicine I, University Hospital Ulm, Albert-EInstein-Allee 23, Ulm, 89081, Germany, Tel +49 731 500 44730, Fax +49 731 500 44705, Email [email protected]
Purpose: Undesirable drug interactions are frequent, they endanger the success of therapy, and they lead to adverse drug reactions. The present study aimed to evaluate statistically potentially drug interactions in a locally circumscribed, random sample population.
Patients and Methods: In a random sample population of 264 patients taking medications, we performed analyses with the drug information system AiDKlinik®. Statistical analysis was performed using SAS version 9.4.
Results: Statistically potentially drug interactions were recorded in 82/264 (31.1%) subjects, including 39/82 (47.56%) men, and 43/82 (52.43%) women (χ2= 0.081; p = 0.776). The average number of potential possible interactions detected per person was 1.60 ± 1.21. The regression model with the variables age, body-mass-index and number of long-term-medications shows a significant association between the number of long-term medications taken and the number of moderately severe and severe reactions to drug interactions (F(3.239) = 28.67, p < 0.0001; (t(239) 8.28; p < 0.0001)). After backward elimination, the regression model showed a significant interaction with the number of long-term medications (t (240) = 8.73, p < 0.0001) and body-mass-index (t (240) = 2.02, p = 0.0442). In descriptive analysis, the highest percentages of potential drug interactions occurred in 42/82 (51.22%) subjects with body mass indices (BMIs) > 25 kg/m2 and in 28/82 (34.15%) subjects aged 61– 70 years.
Conclusion: Number of long-term medications use, age, and obesity may lead to increased drug–drug interactions in a random population sample.
Keywords: long-term medications, drug interactions, random sample population, prevalence, age- and gender-specific frequency
Introduction
The number of prescribed drugs increases in proportion to age.1 Because these drugs are predominantly for treating chronic and long-term diseases, they generally must be taken throughout life.2 On average, patients over 65 years old take about five drugs concurrently, and those over 75 take about six drugs concurrently.3 The risk of adverse drug reactions is high when multiple drugs are taken in combination. Drug interactions can occur in any age group, but they are more common as age increases, because the interactions are related to the number of drugs, what increases with age.4 Adverse drug reactions were associated with hospitalisation rates up to 5%,5,6 an increased frequency of emergency room visits,7 a financial burden on the healthcare system,8,9 and mortality rates up to 0.5%.5 Drug–drug interactions are a subset of conditions that lead to adverse drug reactions, where the action of one drug interferes with that of another drug.10 Drug interactions can lead to drug unsuitability or inadequacy, particularly as patients grow older.11,12
Moreover, to a minor extent, self-medication with non-prescription or off-prescription medicines can contribute to these interactions.13 Pharmaceutical manufacturers have implemented reporting systems to detect and counter this problem; thus, in-house databases are operated and maintained by drug companies.9 However, those data might not be freely accessible. Thus, procuring information about relevant drug reactions - and ensuring completeness - presents a challenge for the healthcare system.14 Previous studies on drug–drug interactions have focused on specific individual drugs, classes of drugs, or pre-selected hospitalised patient groups.
The present single-centre study aimed to analyse potential drug interactions in a random, non-pre-selected population cohort, based on prospectively acquired and retrospectively evaluated data. Epidemiological characteristics that might contribute to drug interactions, such as age, gender, body weight, and potential self-medication drugs, were of particular interest.
Materials and Methods
Study Cohort
In 2002, the Echinococcus multilocularis and Internal Diseases in Leutkirch (EMIL)-I study recruited 4000 randomly selected subjects that resided in the urban district of Leutkirch, Germany. The 2429 subjects that participated in the study formed the original EMIL-I population. In 2013, 484 subjects from the EMIL-I study took part in the EMIL-II study. Drug interaction data were collected as part of the EMIL-II study. Participation in the study was voluntary, and all patients/parents or legal guardians provided written consent to participate. The study was carried out in accordance with the guidelines of the Declaration of Helsinki, and it was approved by the local Ethics Committee by the University of Ulm (No: 10/15).
Inclusion and Exclusion Criteria
For the present study, we sent questionnaires to the 484 subjects of the EMIL-II study, and 342 replied (response rate, 70.66%). Of the 342 questionnaires returned, we excluded 78, due to missing or incomplete medical information, no reported use of medication, or outlier values for age, weight, or BMI. In the final analysis, 264 questionnaires were evaluated (Figure 1).
 |
Figure 1 Flow chart of subjects selected for inclusion into the study. |
Evaluation Parameters
We collected data on personal details, including height, weight, weight loss, occupation, physical activity (regularity and duration), alcohol, coffee consumption, and nicotine consumption. We recorded any previous diseases, and we categorised subjective health assessments (very good, good, moderate, poor, very poor). The drugs reported were recorded in a table, keyed to the time of day each was taken, the class of medication, the formulation, and the dosage. We also recorded whether each drug was used as a self-medication and/or whether it was prescribed by a physician. In the case of self-medication, the subject was asked to state the reason for using a non-prescribed medication (eg, lack of time, convenience, previous experience, recommendation).
Statistical Analysis
We performed statistical analyses with SAS Version 9.4 (North American SAS Institute, Cary, North Carolina). We evaluated absolute and relative frequencies. Differences in frequency distributions were calculated with the Chi-Square and Exact-Fisher-Test statistics. Normal distributions were ascertained with the Shapiro–Wilk test. We performed multiple linear regression analyses to identify influencing factors. All tests were two-sided. The level of significance was set as α=0.05. Accordingly, p-values <0.05 were considered significant.
AiDKlinik® Drug Information System
Drug interactions in the sample population were determined with the drug information system, AiDKlinik® (Dosing GmbH, Heidelberg).15 AiDKlinik® is a scientifically tested, comprehensive drug information system (Clinical Decision Support System) that can be used to tailor drug dosage for individual patients. Thus, it aids in avoiding medication errors, and it significantly improves the safety of drug treatment. AiDKlinik® implements the evidence-based knowledge databases of the Department of Clinical Pharmacology and Pharmacoepidemiology of the University Hospital Heidelberg. This is updated monthly and supports users in their decision-making. Only clinically relevant entries are stored in the database to avoid over-alerting as much as possible. AiDKlinik® is registered as a medical device with version 4.0.0 and carries the CE mark. We used algorithms provided in AiDKlinik® to analyse information about the medication formulations and dosages recorded by patients in the EMIL-II study.15 AiDKlinik® offers a catalogue of all ready-to-use drugs available on the German market. When information about dosage was missing or imprecise, we used the standard dosages quoted in the German list of pharmaceuticals, which are approved in Germany and throughout Europe (Red List).
Results
Patient Cohort
The analyses included data from 264 subjects, including 129/264 (48.86%) males and 135/264 (51.13%) females. The mean age of the cohort was 62.90 ± 10.45 years. The ages of subjects at questionnaire completion were: under 40 years (n=8, 3.03%), between 40 and 50 years (n =24, 9.09%), and 51–60 years (n=65, 24.62%). Furthermore, 90 subjects (34.09%) were between 61 and 70 years and 77 subjects (29.17%) were over 70 years. The mean BMI was 29.35 ± 5.22 kg/m2; 43 (16.29%) subjects had BMIs under 20; 126 (47.73%) subjects had BMIs of 20–25; and 95 (35.98%) subjects had BMIs over 25 kg/m2 (Table 1 and Figure 2). Of 264 patients who reported medication use, 153/264 (57.95%) reported taking antihypertensives. Another 116/264 (43.94%) reported taking thyroid medications. The portion of analgesics taken was 73/264 (27.65%), and the portion of antidiabetic drugs taken was 31/264 (11.74%).
 |
Table 1 Characteristics of the Analysed Study Population (n=264) |
 |
Figure 2 Gender distribution in the different age groups. |
Non-Prescription and as Needed Medication
Self-Medication
Of the 264 patients, 67/129 (51.94%) men and 98/135 (72.59%) women reported that they used non-prescription or off-prescription drugs for self-medication. Here, the average number of medications taken was 3.95 ± 2.59 (range 1–14). Table 2 shows a significant difference in self-medication frequencies between men and women (67/129 vs 98/135; χ2=12.007; p=0.0005).
 |
Table 2 Drug Interactions in Germany (n=264) in a Random Sample Population Stratified by Gender and Non-Prescription and as Needed Medications |
Medication as Needed
A total of 78/264 (29.55%) subjects - 32/78 (41.0%) men and 46/78 (59.0%) women - reported taking medication as needed. In the study population, the average number of medications taken on demand was 1.45 ± 0.88 (range 1–6). We found no significant gender-specific differences in taking medications as-needed (97/129 vs 89/135; χ2=2.722; p=0.099, Table 2).
Drug Interactions
No drug interactions were detected in 182/264 (68.94%) subjects. Potential drug interactions were identified in 82/264 (31.06%) subjects, including 39/82 (47.56%) men and 43/82 (52.43%) women (χ2=0.081; p=0.776). In this group, 72 (87.80%) subjects had 1–2 drug interactions, 8 (9.76%) subjects had 3–4 drug interactions, and two (2.44%) subjects had more than five interactions. The average number of detected drug interactions per person was 1.60 ± 1.21 (Table 1).
Factors Associated with Drug Interactions
The regression model with the included variables age, body-mass-index and number of long-term-medications shows a significant association between the number of long-term medications taken and the number of moderately severe and severe reactions to drug interactions (F(3.239)=28.67, p<0.0001; (t(239) 8.28; p<0.0001)). After backward elimination, the regression model showed a significant interaction with the number of long-term medications (t (240)=8.73, p<0.0001) and body-mass-index (t (240)=2.02, p=0.0442). The highest percentages of potential drug interactions occurred in 42/82 (51.22%) subjects with body mass indices (BMIs) >25 kg/m2 (Figure 3) and in 28/82 (34.15%) subjects aged 61–70 years (Table 3).
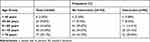 |
Table 3 Drug Interactions in a Random Sample Population in Germany (n=264), Stratified by Age |
 |
Figure 3 Percentage of detected drug interactions, stratified by gender and body mass index. |
Intensity of the Detected Interactions
According to the definitions of drug intensity given in the drug information system, we found that a mild interaction was present in 22/264 (8.33%) subjects, an inconsistent interaction occurred in 21/264 (7.95%) subjects, and a moderately severe to severe interaction occurred in 53/264 (20.08%) subjects (Figure 4).
 |
Figure 4 Percentage of severe and moderately severe drug interactions by number of interactions. |
Discussion
This comparative study analysed potential drug interactions in a random, non-pre-selected population cohort. We considered epidemiological aspects, including age group, gender, and aspects of self-medication. In our population, there was no significant gender predominance in the recorded drug interactions. Number of long-term medications use, age, and obesity may lead to increased drug–drug interactions in a random population sample. Our population had a relatively high average age (62.90 years) compared to the average age of the German population (44.25 years in 2015). This could be explained by the rural location of the patient cohort and the associated aging population.
The current literature on gender predominance for drug interactions has remained inconclusive. Cruciol-Souza et al reported that women were at increased risk of adverse drug interactions compared to men.16 On the other hand, the studies of Nobili et al and Hosia-Randell et al showed no gender predominance for the occurrence of drug interactions.17,18
Our average number of potential interactions per person was below the average of 3 incidences per person reported previously in the German population.6 However, previous studies that focused on older patients reported a frequency similar (1.5 incidences/person) to our results.19 Recent studies have confirmed our finding of a correlation between the number of drugs taken and the number of adverse drug interactions observed.16,17,20
A Jamaican study from 2015 reported a far higher incidence of drug–drug interactions. They found that 49.8% (n=1402/2814) of subjects showed potential drug–drug interactions.21 In contrast, a lower number of incidences occurred in a 2016 study, during a 5-year documentation period, where drug–drug interactions were recorded in 12.3% of subjects in the 5th year of documentation.22 Another study conducted by the King Saud University (2015) showed that at least one drug–drug interaction, regardless of severity, occurred in 91.6% of subjects. These drug–drug interactions were rated severe in 86.3% of cases and moderately severe in 84.5% of cases. The numbers of drug–drug interactions per person were 1–2 in 72.8% of subjects, 3–5 in 14.5% of subjects, and >6 in 4.4% of subjects. A total of 5109 drug–drug interactions were recorded, and of those, 45% were rated severe and 55% were rated moderately severe.23
However, in our population, by the software we use, potential drug interactions were considered mild in 8.3% of subjects and moderately severe or severe in approximately 20.08% of subjects. The discrepancy between our findings and those of Murtaza et al could be explained by the fact that their population consisted of patients hospitalised for cardiological disorders; i.e., subjects whose state of health were far worse than the health of our subjects.23 The study by Naples et al was also undertaken in a general population cohort; thus, the population was comparable to that in our study; however, their overall number of drug–drug interactions was somewhat lower than ours.22
We found a significant increase in drug interactions with increasing BMI and the number of long-term medications. Various explanations for this are conceivable. For example, patients with a low BMI are generally in a better state of health than those with high BMI. So, if obese patients have more drugs than non-obese the BMI is associated with the number of drugs interactions. Additionally, drug interactions were previously shown to be partially related to the level of education.2 Presumably, a better education would provide a better understanding of issues concerning health and diet. Thus, both a low BMI and a high education level could imply a better overall state of health, and hence, more efficient drug metabolism. In particular, recent studies have shown that larger drug doses were needed for subjects with larger body weights.24 Indeed, drug storage and metabolism in fat cells must be considered in subjects with high BMIs.
According to recent studies, drugs taken in the context of self-medication were involved in up to 3.9–4.5% of all adverse drug interaction events, and aspirin was the most frequent culprit.13,25 In our cohort, drugs were taken for self-medication significantly more often among women than among men. In contrast, no significant sex differences were observed with drugs taken as-needed. This result was consistent with results from larger German cohort studies.2 Current recommendations advise that one should not take more than five medications at the same time.26
Our study had some limitations. First, the population that we studied had a relatively high average age (62.90 years) compared to the average age (44.25 years) of all inhabitants in Germany in 2015. Another limitation was that we collected data with a self-questionnaire in 2013. This might have led to missing potential drug interactions, due to the inability of subjects to recognise true drug interactions. We did not require any verification of drug interactions by the family doctor or a specialist. Another important limitation is that only the AiDKlinik® tool was used to identify adverse potential drug interactions. There are currently a number of other programs available on the market for the identification of drug interactions and for drug decision making (e.g. LexiInteract module, Micromedex, Epocrates, Drugs.com). In a possible further study, these programs could be evaluated among each other.
Conclusion
In summary, we showed that, in an unselected cohort of German adults the number of long-term medications use, age, and obesity may lead to increased potential drug–drug interactions in a random population sample.
Data Sharing Statement
The datasets used and analyzed during the current study are available from the corresponding author upon reasonable request.
Ethics Approval and Informed Consent
The study was carried out in accordance with the guidelines of the Declaration of Helsinki, and it was approved by the local Ethics Committee (No: 244/13). All data were analyzed anonymously.
Consent for Publication
All patients/parents or guardians gave their written informed consent for participation in the study.
Author Contributions
All authors contributed to data analysis, drafting or revising the article, have agreed on the journal to which the article will be submitted, gave final approval of the version to be published, and agree to be accountable for all aspects of the work.
Funding
The authors received no financial support for the research, authorship, and/or publication of this article.
Disclosure
The authors report no conflicts of interest in this work.
References
1. Lazarou J, Pomeranz BH, Corey PN. Incidence of adverse drug reactions in hospitalized patients: a meta-analysis of prospective studies. JAMA. 1998;279:1200–1205. doi:10.1001/jama.279.15.1200
2. Knopf H, Grams D. [Medication use of adults in Germany: results of the German health interview and examination survey for adults (DEGS1)]. Bundesgesundheitsblatt Gesundheitsforschung Gesundheitsschutz. 2013;56:868–877. German. doi:10.1007/s00103-013-1667-8
3. Cascorbi I. Drug interactions–principles, examples and clinical consequences. Dtsch Arztebl Int. 2012;109:546–555. doi:10.3238/arztebl.2012.0546
4. Mallet L, Spinewine A, Huang A. The challenge of managing drug interactions in elderly people. Lancet. 2007;370:185–191. doi:10.1016/S0140-6736(07)61092-7
5. Bouvy JC, De Bruin ML, Koopmanschap MA. Epidemiology of adverse drug reactions in Europe: a review of recent observational studies. Drug Saf. 2015;38:437–453. doi:10.1007/s40264-015-0281-0
6. Schneider KL, Kastenmüller K, Weckbecker K, et al. Potential drug-drug interactions in a cohort of elderly, polymedicated primary care patients on antithrombotic treatment. Drugs Aging. 2018;35:559–568. doi:10.1007/s40266-018-0550-6
7. Schurig AM, Böhme M, Just KS, et al. Adverse Drug Reactions (ADR) and emergencies. Dtsch Arztebl Int. 2018;115:251–258. doi:10.3238/arztebl.2018.0251
8. Alagoz O, Durham D, Kasirajan K. Cost-effectiveness of one-time genetic testing to minimize lifetime adverse drug reactions. Pharmacogenomics J. 2016;16:29–36. doi:10.1038/tpj.2015.39
9. Meier F, Maas R, Sonst A, et al. Adverse drug events in patients admitted to an emergency Department: an analysis of direct costs. Pharmacoepidemiol Drug Saf. 2015;24:176–186. doi:10.1002/pds.3663
10. Roblek T, Vaupotic T, Mrhar A, et al. Drug-drug interaction software in clinical practice: a systematic review. Eur J Clin Pharmacol. 2015;71:131–142. doi:10.1007/s00228-014-1786-7
11. Holt S, Schmiedl S, Thürmann PA. Potentially inappropriate medications in the elderly: the PRISCUS list. Dtsch Arztebl Int. 2010;107:543–551. doi:10.3238/arztebl.2010.0543
12. Gosney M, Tallis R. Prescription of contraindicated and interacting drugs in elderly patients admitted to hospital. Lancet. 1984;324:564–567. doi:10.1016/S0140-6736(84)90775-X
13. Schmiedl S, Rottenkolber M, Hasford J, et al. Self-medication with over-the-counter and prescribed drugs causing adverse-drug-reaction-related hospital admissions: results of a prospective, long-term multi-centre study. Drug Saf. 2014;37:225–235. doi:10.1007/s40264-014-0141-3
14. Straubhaar B, Krähenbühl S, Schlienger RG. The prevalence of potential drug-drug interactions in patients with heart failure at hospital discharge. Drug Saf. 2006;29:79–90. doi:10.2165/00002018-200629010-00006
15. Martin P, Haefeli WE, Martin-Facklam M. A drug database model as a central element for computer-supported dose adjustment within a CPOE system. J Am Med Inform Assoc. 2004;11:427–432. doi:10.1197/jamia.M1296
16. Cruciol-Souza JM, Thomson JC. Prevalence of potential drug-drug interactions and its associated factors in a Brazilian teaching hospital. J Pharm Pharm Sci. 2006;9:427–433.
17. Nobili A, Pasina L, Tettamanti M, et al. Potentially severe drug interactions in elderly outpatients: results of an observational study of an administrative prescription database. J Clin Pharm Ther. 2009;34:377–386. doi:10.1111/j.1365-2710.2009.01021.x
18. Hosia-Randell HM, Muurinen SM, Pitkälä KH. Exposure to potentially inappropriate drugs and drug-drug interactions in elderly nursing home residents in Helsinki, Finland: a cross-sectional study. Drugs Aging. 2008;25:683–692. doi:10.2165/00002512-200825080-00005
19. Raschi E, Piccinni C, Signoretta V, et al. Clinically important drug-drug interactions in poly-treated elderly outpatients: a campaign to improve appropriateness in general practice. Br J Clin Pharmacol. 2015;80:1411–1420. doi:10.1111/bcp.12754
20. Johnell K, Klarin I. The relationship between number of drugs and potential drug-drug interactions in the elderly: a study of over 600,000 elderly patients from the Swedish prescribed drug register. Drug Saf. 2007;30:911–918. doi:10.2165/00002018-200730100-00009
21. Kennedy-Dixon TG, Gossell-Williams M, Hall J, et al. The prevalence of major potential drug-drug interactions at a university health centre pharmacy in Jamaica. Pharm Pract (Granada). 2015;13:601. doi:10.18549/PharmPract.2015.04.601
22. Naples JG, Marcum ZA, Perera S, et al. Impact of drug-drug and drug-disease interactions on gait speed in community-dwelling older adults. Drugs Aging. 2016;33:411–418. doi:10.1007/s40266-016-0373-2
23. Murtaza G, Khan MY, Azhar S, et al. Assessment of potential drug-drug interactions and its associated factors in the hospitalized cardiac patients. Saudi Pharm J. 2016;24:220–225. doi:10.1016/j.jsps.2015.03.009
24. Tellor KB, Nguyen SN, Bultas AC, et al. Evaluation of the impact of body mass index on warfarin requirements in hospitalized patients. Ther Adv Cardiovasc Dis. 2018;12:207–216. doi:10.1177/1753944718781295
25. Locquet M, Honvo G, Rabenda V, et al. Adverse health events related to self-medication practices among elderly: a systematic review. Drugs Aging. 2017;34:359–365. doi:10.1007/s40266-017-0445-y
26. Wiedemann G. Big Five – sind 5 Medikamente genug? [Big Five - Are 5 drugs enough?] Klinikarzt. 2018;47:385–387. German. doi:10.1055/a-0654-4493
 © 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
