Back to Journals » Breast Cancer: Targets and Therapy » Volume 15
Efficacy and Safety of Radiotherapy Combined with Pyrotinib in the Treatment of HER2-Positive Breast Cancer with Brain Metastases
Authors Huang J , Zhu W, Duan Q, Zhu C, Shi X, Zhao H, Cai P , Li D
Received 16 September 2023
Accepted for publication 8 November 2023
Published 17 November 2023 Volume 2023:15 Pages 841—853
DOI https://doi.org/10.2147/BCTT.S440427
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Professor Harikrishna Nakshatri
Jie Huang,1,* Wenqiang Zhu,1,* Qiangzhi Duan,2,* Chaomang Zhu,1 Xueling Shi,1 Hongyu Zhao,1 Peng Cai,1 Duojie Li1
1Department of Radiotherapy, The First Affiliated Hospital of Bengbu Medical College, Bengbu, Anhui, 233000, People’s Republic of China; 2Department of Radiotherapy, The 2nd Affiliated Hospital of Bengbu Medical College, Bengbu, Anhui, 233000, People’s Republic of China
*These authors contributed equally to this work
Correspondence: Duojie Li, Department of Radiotherapy, The First Affiliated Hospital of Bengbu Medical College, Bengbu, Anhui, 233000, People’s Republic of China, Tel/Fax +86-139-5633-2626, Email [email protected]
Purpose: To explore the efficacy and safety of pyrotinib combined with different radiotherapy modes in human epidermal growth factor receptor 2 (HER2)-positive breast cancer (BC) patients with brain metastasis (BM).
Patients and Methods: This study is a retrospective analysis of patients diagnosed with BM who underwent treatment with pyrotinib between November 2018 and April 2023. A total of 66 patients were administered radiotherapy in conjunction with pyrotinib (Group A), while 26 patients received pyrotinib as a standalone treatment (Group B). Within Group A, 18 patients underwent conventional fractionated radiotherapy (2Gy/F), while 48 patients received hyperfractionated radiotherapy (HFRT) (≥ 3Gy/F). The primary endpoints were intracranial progression-free survival (IC-PFS) and overall survival (OS). The secondary endpoints were objective response rate (ORR) and clinical benefit rate (CBR).
Results: The ORR of Group A was 54.5% (36/66), while the ORR of Group B was 34.6% (9/26) (P= 0.047). The CBR of Group A was 89.4% (59/66) and that of Group B was 69.2% (18/26) (P= 0.041). The IC-PFS between Group A and Group B were 12 months and 8 months, respectively (P< 0.001), and the OS were 20 months and 16 months, respectively (P= 0.065). In Group A, the IC-PFS and OS between the conventional fractionation radiotherapy group and the HFRT group were 10 months and 12 months, respectively (P= 0.001) and 16 months and 24 months, respectively (P< 0.001). No serious adverse reactions were observed in Group A and Group B.
Conclusion: For HER2-positive BC patients with BM, it is recommended to adopt the treatment mode of HFRT combined with pyrotinib, which can improve the local control and survival of patients.
Keywords: breast cancer, human epidermal growth factor receptor type 2, brain metastasis, pyrotinib, radiation therapy, hyperfractionated radiotherapy
Introduction
Breast cancer (BC) has become one of the most common malignant tumors in global and is the major cause of cancer-related death in women.1 As a highly heterogeneous disease, BC has different prognoses with different molecular typing. Human epidermal growth factor receptor 2 (HER2)-positive BC accounts for 15%–20% of all BC, HER2-positive BC progresses faster, is prone to relapse and metastasis, and has shorter patient survival and poorer prognosis.2,3 According to the latest data, the incidence of brain metastasis (BM) in BC is second only to non-small cell lung cancer, accounting for 10%–16% of primary tumors.4,5 HER2 overexpression, hormone receptor negativity and multiple regional lymph node metastases are risk factors for BM, among which HER2 overexpression is the main risk factor. BM seriously affects the survival quality of patients and is one of the main causes of death in advanced BC patients. Studies have confirmed that 20% of BC patients die from BM.6–8 Along with improvement of technology, the survival time of BC patients is gradually prolonged, but the incidence of BM also steadily increasing,9,10 and poor treatment of BM is becoming the main reason of death in these patients.11,12
Brain radiotherapy is the most common and effective treatment for BM,13 and radiation therapy is usually used for unresectable BM, which includes whole-brain radiotherapy (WBRT), stereotactic radiotherapy (SRS) and hyperfractionated radiotherapy (HFRT).14 SRS such as gamma knife and X-knife, can be used for those with fewer metastases, while WBRT is preferred for patients with multiple BM.15 WBRT can cause a certain degree of cognitive adverse effects, including somnolence, fatigue, memory and learning disabilities, which reduces the quality of life of the patients.16 The results of SRS are not always satisfactory, especially in larger diameter BM. On the one hand, a single high-dose radiotherapy may increase the risk of acute and late central nervous system toxicities. On the other hand, there are limitations of tolerated doses in peripheral critical organs.17 HFRT is a viable alternative to SRS and is increasingly becoming the treatment of choice for BM, which can not only provide high-dose radiation therapy to obtain good local intracranial control, but also minimize the occurrence of toxic side effects of the central nervous system.18
Systemic therapy has the advantage of controlling both intracranial and extracranial metastatic lesions as opposed to local therapy, and HER2-targeted therapy has been shown to be effective in patients with HER2-positive BM. Currently, available HER2-targeted drugs can be categorized into small-molecule tyrosine kinase inhibitors (TKIs), monoclonal antibodies, and antibody-drug conjugates (ADCs). The efficacy of monoclonal antibodies (such as trastuzumab and pertuzumab) on BM is not ideal.19 The blood–brain barrier (BBB) provides considerable resistance to chemotherapeutic agents.20 Compared with monoclonal antibodies and ADCs, TKIs are more advantageous in penetrating the BBB, and TKIs have shown good efficacy in HER2-positive BC, especially in BCBM.21–24
To date, four epidermal growth factor receptor (EGFR)-TKIs have been approved (namely lapatinib, pyrotinib, neratinib and tucatinib), all of which have shown promising efficacy in the treatment of patients with BM.25 Pyrotinib, a small-molecule TKIs independently developed in China, is an irreversible and potent TKIs against HER1, HER2 and HER4. In patients with HER2-positive metastatic BC previously treated with trastuzumab, paclitaxel, and/or anthracyclines, pyrotinib plus capecitabine increased mPFS by 5.7 months compared with lapatinib in combination with capecitabine (12.5 months vs 6.8 months, P < 0.001), according to the PHOEBE study.26 PERMEATE, a single-arm, prospective, Phase II study showed that patients with BM that progressed after radiotherapy received pyrotinib combined with capecitabine, and the intracranial ORR was 42.1% and PFS was 5.6 months, while the intracranial ORR was 74.6% and PFS was 11.3 months in patients with BM that did not receive radiotherapy.27 Pyrotinib has been proven to be an effective and safe drug for tumor treatment, disease control, and controllable adverse reactions.28 Pyrotinib may offer physicians a new treatment option for patients with HER2-positive advanced BC especially those with BM. With the development of small molecule targeted agents, improvements in intracranial control may outweigh local treatments alone, including WBRT, SRS and surgery. Recently published data suggest that the addition of most types of targeted therapies is safe and does not increase radiotherapy toxicity.29–31
All of the above studies have shown the role of drugs and radiotherapy in HER2-positive BCBM, however, there are few data on the combination of radiotherapy and pyrotinib in the treatment of HER2-positive BCBM in the real world, and no study has shown which radiotherapy fractionation mode can achieve the best efficacy. The aim of this paper is to investigate the efficacy and safety of radiotherapy combined with pyrotinib and different modes of radiotherapy fractionation in patients with HER2-positive BCBM, in order to determine the best treatment mode for these patients.
Materials and Methods
Inclusion Criteria
1. Invasive BC with pathologically confirmed HER2-positive expression, defined as HER2 +++ on immunohistochemical staining and/or positive by fluorescence in situ hybridization; 2. BM confirmed by MRI or enhanced CT (patients with contraindications to MRI, at least one or more lesions and brain metastases ≥1cm); 3. Age ≥18 years and ≤80 years, female; 4. Estimated survival of not less than 2 months; 5. ECOG score 0–2; 6. Normal major organ function and no contraindication to treatment.
Exclusion Criteria
1. Patients with BM or other causes of cerebral hemorrhage confirmed by CT or MRI; 2. Patients with multiple factors affecting oral administration and absorption of drugs; 3. Patients with serious concomitant diseases; 4. Women who are pregnant or breastfeeding; 5. Uncompleted radiotherapy and lost to follow-up.
Clinical Data
We collected data of 92 patients with HER2-positive BCBM who were diagnosed with BCBM in the Department of Oncology of the First Affiliated Hospital of Bengbu Medical College from November 2018 to April 2023 and were treated with brain radiotherapy combined with pyrotinib or pyrotinib alone. Of these patients, 66 received radiotherapy combined with pyrotinib (group A) and 26 received pyrotinib alone (group B). In group A, 18 patients received conventional fractionated radiotherapy (2Gy/F, 36–60Gy/18-30F), and 48 patients received HFRT (≥3Gy/F, 30–60Gy/5-18F). The position of patients for radiotherapy was supine and fixed with thermoplastic cephaloplast. The radiotherapy equipment was 6MV-X-ray medical linear accelerator, and the planning system was Pinnacle system. Using CT simulation positioning machine or MRI positioning, and then target area outlining, GTV is defined as the imaging visible brain metastatic lesions, excluding the surrounding oedema area, the PTV for GTV three-dimensional outward 3mm generation and based on the anatomical barriers to modify the use of dose-volume histograms (DVH) to assess the target volume of the conformity, homogeneity, the amount of critical organs and critical organ volume. Each time the patient was positioned, it was ensured that the patient’s positional fixation was consistent with that of the simulated positioning, and the error was within the permissible range, and the radiotherapy was performed under the guidance of cone-beam CT images. All patients received 1 cycle of pyrotinib in combination with capecitabine over 21 days, with the initial dose and local treatment (dose and mode of radiotherapy) selected by the physician based on the results of previous clinical trials and the patient’s condition, and recorded in the electronic medical record.
Assessment of Baseline Clinical Characteristics
Patient information such as age, hormone receptor type, TNM stage, metastases at diagnosis, ECOG score, extracranial metastases, number of brain metastases, size of brain metastases, prior HER2-targeted therapy, and radiotherapy were collected from the electronic medical record system.
HER2 overexpression was defined as a HER2 3+ or positive FISH gene test. Estrogen receptor (ER) and progesterone receptor (PR) status were measured by IHC. A positive IHC result was defined as ER/PR ≥1%. Hormone receptor (HR) positive was defined as ER/PR positive, and HR negative was defined as ER and PR negative.
Assessment of Efficacy
Baseline examination of all measurable lesions was performed before treatment, and routine imaging examination and measurement were performed. According to RECIST v1.1, complete remission (CR) was defined as the disappearance of all target lesions, partial remission (PR) was defined as a ≥30% reduction in the total length diameter of baseline lesions, disease progression (PD) was defined as an increase in the total length diameter of baseline lesions by >20%, a minimum absolute increase of 5 mm, or the appearance of new lesions, and stable disease (SD) was defined as a reduction in the total length diameter of baseline lesions but not reaching PR or an increase but not reaching PD, objective remission rate (ORR) was defined as CR+PR, and clinical benefit rate (CBR) was defined as CR+PR+SD ≥6 months. Overall survival (OS) was defined as the time from initiation of pyrotinib to death. Intracranial progression-free survival (IC-PFS) was defined as the time from the initiation of pyrotinib to the first appearance of PD in an intracranial lesion. Adverse reactions were assessed according to CTCAE 5.0.
Follow Up
As of July 2023, there were 66 patients in group A, 54 patients achieved IC-PFS and 45 patients died of PD or other causes. There were 26 patients in group B, 25 patients achieved IC-PFS and 15 patients died of PD or other causes.
Statistical Analysis
Count data were expressed as cases (%), and comparisons between groups were made using the χ2 test or Fisher’s exact probability method, and survival analyses and confidence intervals were estimated using the Kaplan–Meier method. The moderating effect of covariates on OS was assessed by univariate and multivariate Cox proportional risk models. SPSS 27.0 was used to complete all statistical tests with a significance level of 0.05 for two-sided tests.
Results
Baseline Characteristics
Ninety-two patients with HER2-positive BM treated with pyrotinib-based therapy from November 2018 to April 2023 were included in this research. The baseline data of the patients are shown in Table 1, including 66 patients in the radiotherapy combined with pyrotinib group (group A) and 26 patients in the pyrotinib group (group B), which accounted for 71.7% and 28.3% of the overall proportion, respectively. The median age of the patients was 52 (27–79) years, 38 (41.3%) patients were hormone receptor positive, 64 (70%) patients with liver, bone or lung metastases, 7 (7.6%) patients had metastases in all three sites, 73 (79.3%) patients with ECOG scores of 0–1, and 19 (20.7%) patients with scores of 2. In terms of anti-HER2 treatment, 59 (64.1%) patients had received trastuzumab and 18 (19.6%) patients received trastuzumab combined with pertuzumab. We also divided the patients in group A into the conventional segmentation group (2Gy/F) and the HFRT group (≥3Gy/F) according to the different modes of radiotherapy segmentation. The data of the patients in the two groups are shown in Table 2.
 |
Table 1 Patient Characteristics at Presentation |
 |
Table 2 Clinical Data of Group A Patients |
Characteristics
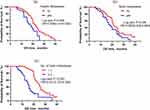
With a median follow-up of 25 months, IC-PFS and OS were achieved in 79 (85.9%) and 60 (65.2%) patients. The overall IC-PFS was 11 months (9.993–12.007) (see Figure 1a), and the overall OS was 20 months (18.417–21.583) (see Figure 1b).
Differences in Survival Outcomes Between the A Group and B Group
Comparing IC-PFS and OS between group A and group B, The Log rank test showed that there was a statistically significant difference in IC-PFS (12 months vs 8 months, P < 0.001) (see Figure 1c) and OS (20 months vs 16 months, P = 0.065) (see Figure 1d) between the two groups. For HER2-positive BC patients with BM, the efficacy of radiotherapy combined with pyrotinib was better than that of pyrotinib alone in terms of IC-PFS and OS. The ORR of patients in group A was 54.5% (36/66), 7 patients reached CR and 29 patients reached PR. The ORR of patients in group B was 34.6% (9/26), no patient reached CR and 9 patients reached PR. The intracranial response rate in group A was higher than that in group B and was statistically significant (P = 0.047). The CBR of patients in group A was 89.4% (59/66), 27 patients reached SD, of which 23 patients had SD duration ≥6 months. The CBR of patients in group B was 69.2% (18/26), 14 patients reached SD, of which 9 patients had SD duration ≥6 months. The CBR of group A was higher than that of group B, and it was statistically significant (P = 0.041). More detailed information can be found in Table 3.
 |
Table 3 Comparison of the Efficacy for the 2 Groups |
Differences in Survival Outcomes Between Conventional Fractionated Radiotherapy Group and HFRT Group
We also divided the patients in group A into the conventional segmentation group (2Gy/F) and the HFRT group (≥3Gy/F) according to the different modes of radiotherapy segmentation. A statistically significant difference was found between the two groups by the Log rank test in terms of IC-PFS (10 months vs 12 months, P = 0.001) (see Figure 1e), and the difference in OS (16 months vs 24 months, P < 0.001) (see Figure 1f). The results showed that the patients with HFRT could get better local control and long-term prognosis compared with the patients with normal segmentation, the difference was statistically significant (P < 0.001). The results indicated that patients treated with HFRT could have better local control and long-term prognosis compared with normal segmentation.
Differences in Survival Outcomes Among Patients with Different Stratification Factors
Lung metastases occurred in 31 (33.7%) patients and 61 (66.3%) patients had no lung metastases, the Kaplan–Meier test showed a significant difference in OS between the two groups (19 months vs 21 months, P = 0.006) (see Figure 2a). Bone metastases occurred in 39 (42.4%) patients and 53 (57.6%) patients had no bone metastases, and the Kaplan–Meier test showed a significant difference in OS between the two groups (17 months vs 21 months, P= 0.036) (see Figure 2b). It suggested that the prognosis of patients with lung and bone metastases was significantly worse than that of patients without lung and bone metastases. In addition, the OS of patients with ≤3 BM was longer than that of patients with >3 BM (24 months vs 15 months, P < 0.001) (see Figure 2c). There was no statistically significant difference in the OS of patients with BM ≤2cm and >2cm in maximum diameter (20 months vs 20 months, P = 0.955).
Cox Regression Analysis of Influencing Factors for Patient OS
Univariate Cox regression analysis was used to study the correlation between clinical characteristics and OS in patients with BM from HER2-positive BC. Only T stage, ECOG score, lung, liver, bone metastases, number of BM and radiotherapy mode were found to be possible predictors of OS in patients. After incorporating multifactorial Cox regression analysis, we found that ECOG score, number of BM, and radiotherapy mode were independent prognostic factors for patients’ OS (Table 4).
 |
Table 4 Analysis of the Correlation Between Clinical Factors and Overall Survival |
Toxic and Side Effects
No critical untoward reactions, for example, cognitive dysfunction, were observed in patients in both groups. The most usual untoward reaction was diarrhea in both groups A and B (87.9% vs 76.9%). Grade 3 or higher adverse reactions were observed in 39.4% of patients in group A (26/66) and 34.6% of patients in group B (9/26). There were no treatment-related deaths in either group A or group B. Specific safety data are shown in Table 5.
 |
Table 5 Treatment-Related Adverse Reactions in the 2 Groups |
Discussion
BCBM seriously threatens the life of BC patients. In recent years, the diagnosis and treatment of BC patients have made great progress, but the prognosis of patients with BM is still poor, these patients lack active and effective treatment.32 Relatively little research has been done on the treatment of BCBM, and most patients with BCBM have been excluded from clinical trials of new drugs.5 Local therapy combined with anti-HER2 systemic therapy is currently recommended for these patients, but the optimal modality remains unclear.33 Therefore, more studies are needed to explore how to improve the survival of these patients. This study included 92 patients with HER2-positive BCBM and aimed to determine the best treatment for this group of patients and prolong the survival of patients with HER2-positive BCBM.
The BBB prevents chemotherapeutic drugs and targeted drugs, for instance, trastuzumab and pertuzumab from entering the central nervous system (CNS), so these drugs have limited effect on BM,34 Compared to monoclonal antibodies, the physical properties of small-molecule TKIs allow them to cross the BBB, thereby increasing the concentration of the drug in CNS, suggesting that TKIs may be a reasonable therapeutic route for the treatment of CNS metastases.35 In the PHENIX trial, capecitabine combined with pyrotinib increased mPFS by 7.0 months (11.1 months vs 4.1 months, P < 0.001) and ORR (68.6% vs 16.0%, P < 0.001) compared with capecitabine alone in patients with HER2-positive metastatic BC, as well as longer PFS in patients with BM (6.9 months vs 4.2 months, P = 0.011), suggesting that patients with BM could benefit from pyrotinib treatment.36 In another retrospective study, patients in the pyrotinib group had better mPFS than those in the lapatinib group (6.5 months vs 3.5 months, P < 0.05).37 The remission rate of brain symptoms with pyrotinib treatment is as high as 100%, which significantly improves the quality of life of patients.38 Therefore, any drug for BM must have the permeability of BBB. Recently, a new scheme for the treatment of BCBM is to use a nano-sized drug delivery system, which brings a new treatment scheme for such patients.39
Radiotherapy is a routine option for local control of BM. Earlier studies have indicated that radiotherapy can improve the permeability of BBB and improve the efficacy of drugs,40 Concurrent pyrotinib treatment enhances radiotherapy sensitivity.41 Local control rates for BM treated with pyrotinib and radiotherapy were higher than those for BM not treated with radiotherapy, and remission of cranial symptoms treated with considering the patient’s willingness for treatment, patients were selected for treatment with pyrotinib or radiotherapy combined with pyrotinib regimen. In this study, intracranial ORR in group B was 34.6%, which was lower than cohort A (74.6%) of the PERMEATE study, which may be due to the fact that most of the patients enrolled in this study had metastases from multiple sites. For the different treatment regimens, the intracranial ORR in cohort A was 54.5%, whereas the intracranial ORR in cohort B was 34.6%, which was significantly different between the two groups (P = 0.047), and the CBR in cohort A (89.4%) was significantly higher than that in cohort B (69.2%), which was statistically significant (P = 0.041). The study demonstrated that radiotherapy in combination with pyrotinib could affect the patients’ intracranial ORR and was significantly superior to that of pyrotinib alone. In addition, there are some preclinical molecular targets that can improve the efficacy of radiotherapy and the treatment of BCBM, novel pathways under investigation include targeting long non-coding RNAs or transcription factors that may drive BC metastasis to the brain and reduce treatment efficacy.42 Through the study of these new pathways and transfer factors, therapeutic effects can be better improved in the future.
In the PERMEATE trial, the median IC-PFS of patients with BM treated with pyrotinib combined with capecitabine was 5.6 to 11.3 months.27 In this study, the median IC-PFS of patients in group B was 8 months, which was basically consistent with the results of previous studies, and patients in group A received radiotherapy combined with pyrotinib, and their median IC-PFS was 12 months, which was higher than that of earlier studies,43 IC-PFS was statistically different between the two groups (P < 0.001). Research by Chen et al30 79 patients with BM from HER2-positive BC were included, 35 patients in group A received pyrotinib in combination with radiotherapy, and 44 patients in group B were treated with pyrotinib or at an interval of greater than 3 months from radiotherapy to the brain, and the results of the study showed that IC-PFS was better in group A than in group B (15.0 months vs 6.0 months, P = 0.056). Consistent with the results of this research, the addition of radiotherapy prolonged IC-PFS in patients, and radiotherapy combined with pyrotinib treatment had better local efficacy than pyrotinib alone, but this was a retrospective study, and future large-sample prospective randomised controlled trials are needed to better understand the efficacy of radiotherapy combined with pyrotinib.
Similar to previous studies,30 compared with pyrotinib alone, radiotherapy combined with pyrotinib did not significantly improve the OS of the patients, in this study the median OS of group A and B was (20 months vs 16 months, P = 0.065). The OS of group A was better than that of group B, but not statistically significant, which may be due to the small sample size in this study.
Previous studies have shown that single SRS is not always feasible, especially in BM of larger diameters and/or located in the vicinity of critical structures, and that single high-dose radiotherapy is not only limited by the maximum tolerated dose to the surrounding organs at risk (such as brain stem or optic nerve, etc.), but also increases the risk of acute and late CNS side effects.17 HFRT is mostly used in this situation to maintain a high rate of intracranial control while reducing radiation-induced CNS toxicity. A study by Fokas et al showed that44 HFRT can be used for BM with large diameters and/or in the vicinity of key structures, and there is no significant difference between HFRT and SRS in terms of median survival and local progression-free survival. HFRT has low central nervous system toxicity and is an effective and safe treatment. In the study of patients with BM from lung cancer, the large split-mode radiotherapy has a short duration, saves medical resources and does not increase the incidence of adverse effects and has a high safety profile.45 In this study, we divided group A into conventional segmentation group (2Gy/F) and hypofractionated radiotherapy group (≥3Gy/F) according to different radiotherapy segmentation modes, and the IC-PFS (10 months vs 12 months, P = 0.001) and OS (16 months vs 24 months, P < 0.001) between the two groups, and the results showed that patients treated with hypofractionated radiotherapy had a better local control rate and long-term prognosis.
In this research, we investigated the prognosis of patients with HER2-positive BCBM by Cox regression analysis. The results showed that T stage, ECOG score, lung, liver, bone metastases, number of BM, and radiotherapy mode were possible predictors of OS in patients. This is in agreement with Hackshaw46 Ma et al.31 After multifactorial Cox regression analysis, we found that ECOG score, number of BM, and radiotherapy mode were independent prognostic factors for OS in patients. In a study from the SEER database (n = 206913), the incidence of BM was higher in patients with multiple extracranial metastases (bone, liver, and lung) than in patients with bone metastases alone (28.0% vs 8.6%), suggesting that visceral metastases are a risk factor for BM.47 Some studies have identified several potential biomarkers associated with BCBM, and their quantitative analysis may be a reliable indicator for evaluating the rationality of MRI imaging in BC patients with asymptomatic BM.48 Brain MRI screening is only recommended when a patient has symptoms of suspected intracranial metastases, and the chances of early treatment of BM will be greater if closer brain monitoring can be performed when the patient has high-risk factors like visceral metastases.27
Showing no difference with earlier issued data,31,36 The security analysis of this research showed that the most usual untoward reaction was diarrhea. No critical untoward reaction was observed in either group, suggesting that the overall safety tolerability of pyrotinib for BM was acceptable, the safety of radiotherapy combined with pyrotinib was manageable, and the addition of radiotherapy did not significantly increase side effects in patients.
The major strengths of this research are that it is the first to investigate the prognostic impact of different radiotherapy segmentation modalities in patients with HER2-positive BCBM, and it further explores the availability and security of radiotherapy combined with pyrotinib versus pyrotinib therapy alone in a realistic study. However, this was a retrospective study with a small sample size, and there were some biases and confounders in the results (eg, the study did not control for the modality of radiotherapy, such as HFRT, HFRT+WBRT, WBRT), and these confounders may have impacted patient survival. In the next, larger randomised controlled trials are needed for determining the optimal treatment modality for BCBM.
Conclusion
Based on these results, the treatment modality of HFRT combined with pyrotinib is recommended for patients with HER2-positive BCBM, which can improve the local control and survival of patients.
Data Sharing Statement
The data supporting the results in the manuscript can be obtained from the corresponding author based on reasonable request.
Ethics Approval and Consent to Participate
This retrospective study approved by the Institutional Review Board of The First Affiliated Hospital of Bengbu Medical College (approval number: 2023YJS152). Given that this study was conducted relying on retrospective data collected as part of routine clinical practice, ethical committee waived the consent, and individual informed consent was not obtained. In this retrospective study, no patient identifiers were used and data were anonymized. This study followed the Declaration of Helsinki (2013 revision)
Acknowledgments
The authors wish to thank patients and their kin for supporting our work and thank editors as well as reviewers for reading the manuscript.
Funding
This work was founded by the Natural Science Foundation of Anhui Education Department (No. KJ2021A0699).
Disclosure
The authors report no conflicts of interest in this work.
References
1. Sung H, Ferlay J, Siegel RL., et al. Global cancer statistics 2020: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin. 2021;71(3):209–249. doi:10.3322/caac.21660
2. Shin I. HER2 signaling in breast cancer. Adv Exp Med Biol. 2021;1187:53–79.
3. Ganz PA, Goodwin PJ. Breast cancer survivorship: where are we today. Adv Exp Med Biol. 2015;862:1–8.
4. Siegel RL, Miller KD, Fuchs HE, Jemal A. Cancer statistics, 2022. CA Cancer J Clin. 2022;72(1):7–33. doi:10.3322/caac.21708
5. Bailleux C, Eberst L, Bachelot T. Treatment strategies for breast cancer brain metastases. Br J Cancer. 2021;124(1):142–155. doi:10.1038/s41416-020-01175-y
6. He DJ, Yu DQ, Wang QM, et al. Breast cancer subtypes and mortality of breast cancer patients with brain metastasis at diagnosis: a population-based study. Inquiry. 2021;58:469580211055636. doi:10.1177/00469580211055636
7. Tarantino P, Prat A, Curigliano G. New anti-HER2 agents for brain metastasis: histology-agnostic weapons. Breast Cancer Res Treat. 2021;185(3):879–881. doi:10.1007/s10549-020-05982-y
8. Zahid KF, Kumar S, Al-Bimani K, et al. Outcome of Omani women with breast cancer-associated brain metastases experience from a university hospital. Oman Med J. 2019;34(5):412–419. doi:10.5001/omj.2019.76
9. Corti C, Antonarelli G, Criscitiello C, et al. Targeting brain metastases in breast cancer. Cancer Treat Rev. 2022;103:102324. doi:10.1016/j.ctrv.2021.102324
10. Gobbini E, Ezzalfani M, Dieras V, et al. Time trends of overall survival among metastatic breast cancer patients in the real-life ESME cohort. Eur J Cancer. 2018;96:17–24. doi:10.1016/j.ejca.2018.03.015
11. Costa R, Carneiro BA, Wainwright DA, et al. Developmental therapeutics for patients with breast cancer and central nervous system metastasis: current landscape and future perspectives. Ann Oncol. 2017;28(1):44–56. doi:10.1093/annonc/mdw532
12. Brufsky AM, Mayer M, Rugo HS, et al. Central nervous system metastases in patients with HER2-positive metastatic breast cancer: incidence, treatment, and survival in patients from registHER. Clin Cancer Res. 2011;17(14):4834–4843. doi:10.1158/1078-0432.CCR-10-2962
13. Gullhaug A, Hjermstad MJ, Yri O, Svestad JG, Aass N, Johansen S. Use of radiotherapy in breast cancer patients with brain metastases: a retrospective 11-year single center study. J Med Imaging Radiat Sci. 2021;52(2):214–222. doi:10.1016/j.jmir.2021.01.002
14. Brown PD, Ahluwalia MS, Khan OH, Asher AL, Wefel JS, Gondi V. Whole-brain radiotherapy for brain metastases: evolution or revolution. J Clin Oncol. 2018;36(5):483–491. doi:10.1200/JCO.2017.75.9589
15. Tomasello G, Bedard PL, de Azambuja E, Lossignol D, Devriendt D, Piccart-Gebhart MJ. Brain metastases in HER2-positive breast cancer: the evolving role of lapatinib. Crit Rev Oncol Hematol. 2010;75(2):110–121. doi:10.1016/j.critrevonc.2009.11.003
16. Kann BH, Park HS, Johnson SB, Chiang VL, Yu JB. Radiosurgery for brain metastases: changing practice patterns and disparities in the United States. J Natl Compr Canc Netw. 2017;15(12):1494–1502. doi:10.6004/jnccn.2017.7003
17. Akagunduz OO, Yilmaz SG, Tavlayan E, Baris ME, Afrashi F, Esassolak M. Radiation-induced ocular surface disorders and retinopathy: ocular structures and radiation dose-volume effect. Cancer Res Treat. 2022;54(2):417–423. doi:10.4143/crt.2021.575
18. Masucci GL. Hypofractionated radiation therapy for large brain metastases. Front Oncol. 2018;8:379. doi:10.3389/fonc.2018.00379
19. Lin NU, Pegram M, Sahebjam S, et al. Pertuzumab plus high-dose trastuzumab in patients with progressive brain metastases and HER2-positive metastatic breast cancer: primary analysis of a Phase II study. J Clin Oncol. 2021;39(24):2667–2675. doi:10.1200/JCO.20.02822
20. Shah N, Mohammad AS, Saralkar P, et al. Investigational chemotherapy and novel pharmacokinetic mechanisms for the treatment of breast cancer brain metastases. Pharmacol Res. 2018;132:47–68. doi:10.1016/j.phrs.2018.03.021
21. Slamon DJ, Leyland-Jones B, Shak S, et al. Use of chemotherapy plus a monoclonal antibody against HER2 for metastatic breast cancer that overexpresses HER2. N Engl J Med. 2001;344(11):783–792. doi:10.1056/NEJM200103153441101
22. Geyer CE, Forster J, Lindquist D, et al. Lapatinib plus capecitabine for HER2-positive advanced breast cancer. N Engl J Med. 2006;355(26):2733–2743. doi:10.1056/NEJMoa064320
23. Swain SM, Baselga J, Kim SB, et al. Pertuzumab, trastuzumab, and docetaxel in HER2-positive metastatic breast cancer. N Engl J Med. 2015;372(8):724–734. doi:10.1056/NEJMoa1413513
24. Verma S, Miles D, Gianni L, et al. Trastuzumab emtansine for HER2-positive advanced breast cancer. N Engl J Med. 2012;367(19):1783–1791. doi:10.1056/NEJMoa1209124
25. Mills MN, Walker C, Thawani C, et al. Trastuzumab Emtansine (T-DM1) and stereotactic radiation in the management of HER2+ breast cancer brain metastases. BMC Cancer. 2021;21(1):223. doi:10.1186/s12885-021-07971-w
26. Xu B, Yan M, Ma F, et al. Pyrotinib plus capecitabine versus lapatinib plus capecitabine for the treatment of HER2-positive metastatic breast cancer (PHOEBE): a multicentre, open-label, randomised, controlled, Phase 3 trial. Lancet Oncol. 2021;22(3):351–360. doi:10.1016/S1470-2045(20)30702-6
27. Yan M, Ouyang Q, Sun T, et al. Pyrotinib plus capecitabine for patients with human epidermal growth factor receptor 2-positive breast cancer and brain metastases (PERMEATE): a multicentre, single-arm, two-cohort, Phase 2 trial. Lancet Oncol. 2022;23(3):353–361. doi:10.1016/S1470-2045(21)00716-6
28. Kioutchoukova I, Lucke-Wold BP. Pyrotinib as a therapeutic for HER2-positive breast cancer. Transl Cancer Res. 2023;12(6):1376–1379. doi:10.21037/tcr-23-333
29. Kim JM, Miller JA, Kotecha R, et al. The risk of radiation necrosis following stereotactic radiosurgery with concurrent systemic therapies. J Neurooncol. 2017;133(2):357–368. doi:10.1007/s11060-017-2442-8
30. Chen J, Zhang H, Zhou J, et al. Efficacy and safety of pyrotinib and radiotherapy vs. pyrotinib-based therapy in patients with HER2(+) breast cancer with brain metastasis: a retrospective cohort study. Ann Transl Med. 2022;10(22):1228. doi:10.21037/atm-22-5352
31. Ma X, Li Y, Zhao Z, et al. Pyrotinib combining with radiotherapy on breast cancer with brain metastasis. Exp Biol Med. 2023;248(2):106–116.
32. Ording AG, Heide-Jørgensen U, Christiansen CF, Nørgaard M, Acquavella J, Sørensen HT. Site of metastasis and breast cancer mortality: a Danish nationwide registry-based cohort study. Clin Exp Metastasis. 2017;34(1):93–101. doi:10.1007/s10585-016-9824-8
33. Chan WL, Lam TC, Lam KO, Luk MY, Kai-Cheong RN, Kwong LD. Local and systemic treatment for HER2-positive breast cancer with brain metastases: a comprehensive review. Ther Adv Med Oncol. 2020;12:1758835920953729. doi:10.1177/1758835920953729
34. Kim JS, Kim IA. Evolving treatment strategies of brain metastases from breast cancer: current status and future direction. Ther Adv Med Oncol. 2020;12:1758835920936117. doi:10.1177/1758835920936117
35. Chien AJ, Rugo HS. Tyrosine kinase inhibitors for human epidermal growth factor receptor 2-positive metastatic breast cancer: is personalizing therapy within reach. J Clin Oncol. 2017;35(27):3089–3091. doi:10.1200/JCO.2017.73.5670
36. Ma F, Ouyang Q, Li W, et al. Pyrotinib or lapatinib combined with capecitabine in her2-positive metastatic breast cancer with prior taxanes, anthracyclines, and/or trastuzumab: a randomized, Phase II study. J Clin Oncol. 2019;37(29):2610–2619. doi:10.1200/JCO.19.00108
37. Yang H, Wang W. Comparison of pyrotinib or lapatinib with chemotherapy for patients with HER2 positive breast cancer after first-line treatment failure: a retrospective study. Am J Transl Res. 2021;13(9):10863–10870.
38. Gao M, Fu C, Li S, et al. The efficacy and safety of pyrotinib in treating HER2-positive breast cancer patients with brain metastasis: a multicenter study. Cancer Med. 2022;11(3):735–742. doi:10.1002/cam4.4481
39. Klaas E, Sung E, Azizi E, et al. Advanced breast cancer metastasized in the brain: treatment standards and innovations. J Cancer Metastasis Treat. 2023;9:23.
40. Fauquette W, Amourette C, Dehouck MP, Diserbo M. Radiation-induced blood-brain barrier damages: an in vitro study. Brain Res. 2012;1433:114–126. doi:10.1016/j.brainres.2011.11.022
41. Tian W, Hao S, Wang L, Chen Y, Li Z, Luo D. Pyrotinib treatment enhances the radiosensitivity in HER2-positive brain metastatic breast cancer patients. Anticancer Drugs. 2022;33(1):e622–e627. doi:10.1097/CAD.0000000000001199
42. Mampre D, Mehkri Y, Rajkumar S, et al. Treatment of breast cancer brain metastases: radiotherapy and emerging preclinical approaches. Diagn Ther. 2022;1(1):25–38. doi:10.55976/dt.1202216523-36
43. Anwar M, Chen Q, Ouyang D, et al. Pyrotinib treatment in patients with HER2-positive metastatic breast cancer and brain metastasis: exploratory final analysis of real-world, multicenter data. Clin Cancer Res. 2021;27(16):4634–4641. doi:10.1158/1078-0432.CCR-21-0474
44. Fokas E, Henzel M, Surber G, Kleinert G, Hamm K, Engenhart-Cabillic R. Stereotactic radiosurgery and fractionated stereotactic radiotherapy: comparison of efficacy and toxicity in 260 patients with brain metastases. J Neurooncol. 2012;109(1):91–98. doi:10.1007/s11060-012-0868-6
45. Chun SG, Hu C, Choy H, et al. Impact of intensity-modulated radiation therapy technique for locally advanced non-small-cell lung cancer: a secondary analysis of the NRG oncology RTOG 0617 randomized clinical trial. J Clin Oncol. 2017;35(1):56–62. doi:10.1200/JCO.2016.69.1378
46. Hackshaw MD, Danysh HE, Henderson M, et al. Prognostic factors of brain metastasis and survival among HER2-positive metastatic breast cancer patients: a systematic literature review. BMC Cancer. 2021;21(1):967. doi:10.1186/s12885-021-08708-5
47. Kim YJ, Kim JS, Kim IA. Molecular subtype predicts incidence and prognosis of brain metastasis from breast cancer in SEER database. J Cancer Res Clin Oncol. 2018;144(9):1803–1816. doi:10.1007/s00432-018-2697-2
48. Klaas E, Mohamed S, Poe J, Reddy R, Dagra A, Lucke-Wold B. Innovative approaches for breast cancer metastasis to the brain. Arch Med Case Rep Case Study. 2022;6(4):147. doi:10.31579/2692-9392/147
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.