Back to Journals » International Journal of Nephrology and Renovascular Disease » Volume 17
Effect of Executive Function on Health-Related Quality of Life in Children with Chronic Kidney Disease
Authors Wijaya EA , Solek P, Rachmadi D, Rahayuningsih SE, Tarigan R , Hilmanto D
Received 3 August 2023
Accepted for publication 21 December 2023
Published 8 January 2024 Volume 2024:17 Pages 17—28
DOI https://doi.org/10.2147/IJNRD.S428657
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Professor Pravin Singhal
Elrika Anastasia Wijaya, Purboyo Solek, Dedi Rachmadi, Sri Endah Rahayuningsih, Rodman Tarigan, Dany Hilmanto
Department of Child Health, Faculty of Medicine, Universitas Padjadjaran, Hasan Sadikin General Hospital, Bandung, West Java, Indonesia
Correspondence: Dany Hilmanto, Tel +628122266879, Email [email protected]
Introduction: As the highest function in the brain that regulates our daily activity, executive dysfunction might affect someone’s health-related quality of life (HRQoL), especially in those with chronic diseases, including chronic kidney disease (CKD). Neurocognitive functions, including intelligence quotient (IQ) and executive function can be affected through various mechanisms in CKD. However, there was still no specific study regarding how IQ and executive function might affect HRQoL in children with CKD.
Purpose: To assess Executive Function’s impact on HRQoL and to find association between treatment modalities and CKD stages with HRQoL in children with CKD.
Methods: A cross sectional study was conducted at Pediatric Nephrology Clinic at Hasan Sadikin General Hospital, Bandung, Indonesia from September 2022 to April 2023. We included 38 children whose age range were 6– 16 years 11 months old with CKD stage III – V. Assessment tools used were: BRIEF questionnaire for executive function; WISC III tool for IQ; PedsQLTM questionnaire generic module for HRQoL. Data was analyzed using SPSS ver. 26.0.
Results: Total number of samples was 38. Complete examinations were done on 30 patients. Eight other patients did not undergo the IQ test. There was a negative correlation between executive function components scores (GEC, BRI, MI) with HRQoL scores on parents’ proxy in all domains. We found no correlation between HRQoL and IQ scores, but we found a correlation between IQ and CKD stage. There was a significant difference in HRQoL from the children’s perspective among the three modalities; children who underwent conservative treatment were having the best HRQoL scores.
Conclusion: Interventions to improve executive function of children with CKD should be done to improve their HRQoL in the future. Early diagnosis and treatment of CKD should be done at the earliest to improve neurocognitive function and HRQoL.
Keywords: chronic kidney disease, neurocognitive function, children, executive function, intelligence quotient, health related quality of life
Introduction
Chronic Kidney Disease (CKD) is a progressively debilitating disease with a high mortality and morbidity rate.1 Based on the data from a study by the ItalKid Project in Italy which consisted of children and young adult younger than 20 years old, the incidence of CKD was 12.1 cases and the prevalence was 74.7 cases out of 1 million population of people younger than 20 years old.2 Studies by El Shafei et al (2018) and Pardede et al (2019) showed that HRQoL was found to be low in children with CKD, and in turn, this might affect their condition and productivity in adulthood.3,4 Health related quality of life in children with CKD of all stages could be affected by many things such as therapeutic modalities, long duration of disease, maternal education, older age, and also disturbance in neurocognitive function.3,5,6 It has been known that CKD could cause reduction of cognitive function too such as deficit on academic skill, executive function, visual memory, and also verbal memory through various mechanisms. As we know, cognitive performance is one of the components of HRQoL.6 Thus, any interference in neurocognitive function might affect someone’s HRQoL and an early intervention to improve neurocognitive deficit in children with CKD might make a difference in their HRQoL later in the future. However, up until now, the correlation between neurocognitive function and HRQoL in children with CKD had never been described yet in any preceding studies.
This study aimed to determine the correlation between neurocognitive function, especially IQ and executive function (which are some of the major components of neurocognitive function) with HRQoL in children with CKD, and to estimate the IQ range of children with CKD. We also aimed to find whether treatment modalities and CKD stage were associated with HRQoL in children with CKD.
Methods
This cross-sectional study was conducted at the Pediatric Nephrology Outpatient Clinic of Hasan Sadikin General Hospital, Bandung, West Java, Indonesia (Tertiary Hospital), from September 2022 – April 2023. The hospital had been equipped well to provide treatment for children with CKD; it had already had pediatric nephrologists, renal hemodialysis and peritoneal dialysis unit for children, and also provided inpatient and outpatient care for children with CKD. However, we were still unable to do kidney transplant on the children by the time the study was conducted. Children who were diagnosed with CKD in stage III–V, with ages ranging from 6 years to 16 years and 11 months who could answer questions were included in the study. We excluded patients who had previously been diagnosed with Intellectual Disability, Autism Spectrum Disorder, or other mental disorders or syndromes. Patients whose parents were unwilling to participate in the study were also excluded. Samples were chosen using the convenience sampling method. The minimal sample size needed for this study was 30 samples; sample size was measured with confidence interval of 95% and power value of 90%. The parents were given informed consent regarding the study. The patient was included in the study only after the parents agreed. Afterwards, IQ test would be scheduled. The IQ test was performed using the Weschler III tool by a professional child psychologist at the Medical Rehabilitation Unit of Hasan Sadikin General Hospital. This tool is written in numbers on a full-range IQ scale. A higher IQ score indicated that the children were more intelligent academically. This test had been proven to have a good fit (p-value = 0.066) when tested on Indonesian children.7 Executive function was determined using BRIEF questionnaire. The questionnaire consisted of 86 questions for parents or the patient’s care provider. Eight components of executive function were analyzed: inhibitory, shifting, emotional control, working memory, plan/organize, organization of materials and monitor. Inhibitory, shifting and emotional control were components of Behavior Regulation Index (BRI). Working memory, plan/organize, organization of materials and monitor were components of Metacognition Index (MI). The mean score of those two indexes was determined as Global Executive Composite (GEC). All components were written as T-score. The higher the T-score, the worse the child’s executive function. It has been translated to various languages including Bahasa Indonesia, with good validity (r = 0.521–0773 in all test domains) and reliability (internal consistency was α = 0.62–0.84 and test-retest score was 0.87). Executive function can be considered as disturbed when the T-score is > 60. Health-related quality of life was determined using the PedsQLTM generic module, which had been proven to have a good internal consistency reliability for the Total Scale Score (alpha = 0.88 child, 0.90 parent report), Physical Health Summary Score (alpha = 0.80 child, 0.88 parent), and Psychosocial Health Summary Score (alpha = 0.83 child, 0.86 parent).8 The PedsQLTM module was filled by the parents in the parents’ section and by the patient in the patient’s section, and was divided into four domains: physical domain (consisted of 8 questions), emotional domain (consisted of 5 questions), social domain (consisted of 5 questions) and school domain (consisted of 5 questions). The answer of each item was scaled from 0–5; score 0 means that the question had never bothered the subject and score 5 means the question had always been a problem to the subject. The HRQoL score from each item was counted after the score was converted, and the total HRQoL score was finally determined. The higher the score, the better the child’s HRQoL was. Explanation about how to fill the questions was given before the parents and the patient started to answer the questionnaire. The license to use PedsQLTM questionnaires was obtained from Mapi Research Trust (ID no 276849) and permission to use BRIEF questionnaire was obtained from Edduwar I Riyadi, Psychiatrist as the license owner. Staging of CKD was determined using the estimated glomerular filtration rate (eGFR) with the Schwartz formula, with creatinine value obtained from the patient’s last routine blood examination or from the patient’s last kidney nuclear scan result.
Data were analyzed using SPSS ver. 26.0. The correlations between both executive function and IQ with HRQoL were analyzed using Pearson’s correlation due to evenly distributed data. We also analyzed the correlations between IQ and eGFR with executive function using Spearman’s rank due to unevenly distributed data.
This study was approved by the Ethics Committee of Hasan Sadikin General Hospital (number LB.02.01/X.6.5/193/2022) and adhered to the Declaration of Helsinki.
Results
We included 38 patients in the study. However, we were only able to perform IQ tests in 30 patients. Five patients died before we were able to schedule the IQ test, and three other patients declined to complete the IQ test but were willing to complete the BRIEF and PedsQLTM questionnaires. The basic characteristics of the participants are listed in Table 1 with the relationship analysis for each item with the parents’ and children’s HRQoL. After the data was completely collected, three more patients died. Thus, the total number of death in our subject during the study period was eight.
 |
Table 1 Subject Characteristics |
The median age of the subjects in this study was 15 years old and was dominated by boys (63,2%) compared to girls (36,8%). Most participants were high school students (55.3%). Parents’ education was mostly high school (42.1%). Most participants came from a low socioeconomic family, with an income of <2.5 million rupiahs per month (60.5%). Most of the children had stage V CKD (50.0%). Almost all (94.7%) subjects were diagnosed with CKD shorter or equal to less than 60 months while only two subjects were diagnosed with CKD for longer than 60 months. The mean eGFR was 15.0 ranging between 4.2 to 51.8. The mean hemoglobin value was 9.3% ± 2.9 g/dl. Most of the subjects in our study had low Hb levels, which was most likely caused by CKD as the underlying disease. Of the 38 study subjects, eight patients died during the data collection period (21.1%), and 30 patients remained alive (78.9%).
We can conclude that several factors such as gender, hemodialysis as therapeutic modality, severity of CKD, and certain laboratory parameters (eGFR, Hb, Ur, Cr) are related with the HRQoL from both children’s and parents’ perspective. Other factors such as age, nutritional status, educational level of the parents and family income do not have a significant correlation with the HRQoL.
The results of the IQ test score using the WISC III, executive function T-score result using the BRIEF, and HRQoL score using the PedsQLTM are described in Table 2.
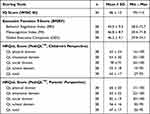 |
Table 2 Results of IQ Scores (WISC III), Executive Function T-Scores (BRIEF), and HRQoL Scores (PedsQLTM) in Children with Chronic Kidney Disease |
The mean WISC III IQ score in children with CKD was 86 ± 13, ranging from 59 – 114 and showing a wide variation in IQ scores from very low to above-average IQ scores in children with CKD in our study. In general, most of the patients’ IQ score in this study could be interpreted as low average.
In most participants, the overall executive function results was normal when measured using the BRIEF questionnaire. However, executive dysfunction was found in various individual aspects. Several aspects of executive dysfunction that we found were: inhibitory (four subjects), adaptation (seven subjects), emotional control (three subjects), initiation (three subjects), working memory (four subjects), planning (three subjects), and material organization (three subjects). Only two patients showed an overall decline in executive function (GEC ≥ 60). One patient had been diagnosed with CKD for > 60 months and had fallen to CKD stage V, with a history of the parents discontinuing treatment by themselves. This patient continued to receive conservative treatment at the time of examination and was considered for renal replacement therapy. Another patient was diagnosed with stage V CKD, had undergone routine HD, and had been diagnosed for approximately 3 years.
In our subjects’ PedsQLTM results, we found that the school domain was the most deteriorated aspect from both the children’s and parents’ perspectives, and the highest score on both perspectives was found on the social domain. Overall, the HRQoL score in children with CKD is lower than in normal, healthy children in this study.
We also tried to see the trend of HRQoL scores based on the children’s CKD stage, and the results are described in Table 3.
 |
Table 3 HRQoL Scores in Children with Chronic Kidney Disease Based on the Disease’s Staging |
In CKD stage III, the mean IQ score was higher compared to those in CKD stages IV and V. Statistical analysis showed a p-value of 0.049, indicating a significant difference between stages III, IV, and V CKD. The quotient score decreased starting from CKD stage IV, with the mean IQ reaching below average. There was also a significant association between IQ and CKD stage. Several mechanisms that had been thought to decrease neurocognitive function in children with CKD were anemia, proteinuria, longer duration of CKD and also lower GFR. Thus, it is possible that those with lower stage of CKD are having a better neurocognitive function, including IQ, since they might have not yet experienced anemia and proteinuria and the duration of CKD is shorter.9
From the above data, we can see that the higher the CKD stage, the lower the HRQoL in all of the domains. This shows that in patients with CKD, the stage of the disease influences HRQoL from both the parents’ and children’s perspectives. Based on the result, we can conclude that slowing down the progression of CKD by diagnosing and treating the disease as early as possible are important for children with CKD.
There was a significant difference in HRQoL from the children’s perspectives in the physical, social, and school domains as well as in the total HRQoL score in patients with CKD stage III, IV, and V in this study. From the parents’ perspective, significant differences were found in stage III, IV, and V of CKD in the emotional domain and the total HRQoL score.
From this analysis, we can conclude that there is a relationship among IQ, HRQoL, and CKD stage in children with CKD. The higher the CKD stage, the lower the IQ and HRQoL scores from both the parents’ and children’s perspectives will be.
The correlations between HRQoL and IQ, HRQoL and executive function, eGFR and IQ, as well as between eGFR and executive function are shown in Table 4.
 |
Table 4 Correlation Between Neurocognitive Function (IQ and Executive Function) with HRQoL in Children with Chronic Kidney Disease |
We found no correlation between IQ and HRQoL from either the children’s or parents’ perspective. We also found no correlation between executive functions and HRQoL in children. However, there was a negative correlation between the T-score BRIEF executive function on all aspects (GEC, MI, and BRI) and all domains of HRQoL on parents’ perspectives. The worse the executive function score (shown by the higher T-score result), the worse the children’s HRQoL based on the parents’ perspectives. There was also a significant positive correlation between IQ and eGFR (r=0387; p=0019). The higher the IQ score was, the better the glomerular filtration rate was, showing a better kidney function. All correlations in this study were categorized as moderate to strong, with the Cohen correlation range: 0 0.09 = no correlation; 0.10 – 0.30 = weak correlation; 0.30 – 0.50 = moderate correlation; 0.50 – 1 = strong correlation.
The relationship between treatment modalities with IQ and HRQoL in children with CKD is shown in Table 5 as follows:
 |
Table 5 Relationship Between IQ and HRQoL with Treatment Modalities in Children with CKD |
Based on the above data, there was a relationship between IQ and HRQoL and treatment modalities in children with CKD. There was no significant difference in IQ scores among the three modalities, with the mean score of 85–87. There was no significant relationship between IQ and the treatment modalities used.
There was a significant difference in HRQoL from the children’s perspective among the three modalities available in our study. The best score was found in children who received conservative treatment compared with those who underwent hemodialysis and peritoneal dialysis.
There was no significant difference in HRQoL from the parents’ perspectives between the treatment modalities in children with CKD.
It could be concluded that HRQoL in children with CKD could be affected by several factors such as gender, hemodialysis as therapeutic modality, severity of CKD, and certain laboratory parameters (eGFR, Hb, Ur, Cr). Executive function but not IQ was also correlated with HRQoL from parents’ perspective in children with CKD. Children with higher stage of CKD had lower IQ scores and treatment modalities might affect HRQoL in children with CKD from the children’s perspective. It becomes important to make strategies to prevent further decline of kidney function in children with CKD and to consider doing executive function intervention, to hopefully improve the HRQoL in children with CKD. Further explanations would be discussed in discussion section.
Discussion
Factors That Might Cause Difference in HRQoL from Children’s and Parents’ Perspectives
The HRQoL can be used to determine a person’s perspective of their own well-being. In a condition where the patient has a chronic disease, HRQoL can be used as a parameter to measure the effectivity of the treatment. It could also be done to evaluate the patients’ current satisfaction with their condition and if there is any problem detected, additional programs could be suggested and added for the patient’s treatment accordingly. Several examples of the treatment that could be added were treating the anemia, adding exercise program, treating the depression, etc.10 In a long term, those with better HRQoL might have better outcome and satisfaction of their life. Improved HRQoL could also improve the patient’s work productivity. Thus, measurement of HRQoL becomes important, especially in people with chronic diseases.11 In this study, we found that generally, the parents’ perspectives regarding their children’s HRQoL were better than the children’s perspectives on their own disease, except for the emotional domain. However, the mean difference between children’s and parents’ perspectives was not significant. The overall HRQoL score in our study was relatively low from both children’s and parents’ perspectives. In the previous study by Killís-Pstrusinska et al and Sani et al, HRQoL from parents’ perspectives were mostly lower than from the children’s perspectives.12,13 Low HRQoL from both perspectives show that psychological support is needed not only for the children but also for the parents as the children’s main care provider.
In another study by Eiser et al, it was found that parents’ perspectives of their own lives might affect their perspectives regarding the children’s condition.14 In this study, parents’ socioeconomic status was generally low, with 60.5% of parents having low income and 55.3% were high school graduates. Based on the study by Elshahat et al, treatment expense would get higher with the increasing stage and duration of CKD.15 The expenses for CKD from stage 1–2 to stage 3 was related to a 1.1–1.7-times increase per year, and progression from stage 3 to stage 4–5 was related with 1.3–4.2 times increase, with end-stage renal disease carrying the highest treatment expenses. High expenses and increased CKD stage could possibly contribute to the low HRQoL scores based on the parents’ perspectives, as we found in this study. This condition might also affect the parents’ emotional condition since they might feel burdened and responsible to fulfill their children’s increasing expenses.15
Generally, in this study, the mean HRQoL based on children’s perspectives was lower. A study by Imani et al found that HRQoL based on parents’ perspectives was higher in patients with a higher stage of CKD, especially CKD stage V, similar to the findings of our study.16 This showed that CKD stage was related to both children’s and parents’ perspectives regarding children’s HRQoL. A higher stage might affect the children’s perspective, making it worse compared to the result from the parents’ perspective.
Executive Function and Health Related Quality of Life in Children with Chronic Kidney Disease
Executive function was correlated with all aspects of HRQoL based on the parents’ perspectives in this study. This was in line with the study done by Murphy et al in children with brain tumors which found that there was a correlation between executive function and HRQoL.17 Another study by Schraegle et al in children with epilepsy showed the same result.18 Executive function is often considered as the higher function of the overall neurocognitive function to organize things, such as decision-making, planning, organizing, emotional control, action control, problem solving. It also plays an important role in our daily activity, such as studying, prioritizing things and playing a role in social-behavioral function. A child’s academic achievement can also be affected by executive function, perhaps even more than the child’s natural intelligence.19 Executive function is very sensitive, and even small disturbances such as sleep deprivation or psychological stress can disturb this function. Generally, executive function is compromised in CKD patients. Previous study found executive function declined in patients with CKD compared to normal population.20 As previously mentioned, HRQoL in patients with CKD might also be affected by many factors, including executive function. Mendley et al showed that CKD duration highly affects neurocognitive function, including executive function. In the earlier stages, neurocognitive function disturbances may not be obvious. However, since the beginning, it was found that at least one aspect of neurocognitive function might have already been disturbed.21 That finding was in accordance with the results of our study; we found that at least one aspect of executive function was affected in all samples, but when it was scored in total, the GEC, MI, and BRI were found to be normal except in one patient who had been diagnosed with CKD for > 60 months. In the future, executive dysfunction in these patients might worsen and might become permanent since CKD is an irreversible disease. Early intervention might be needed to prevent this from happening. Treatment compliance is important and other possible executive function interventions might also be considered to prevent further decline in executive function.
From this study, we conclude that executive function interventions might play a role in improving HRQoL in children with CKD. In the long term, executive function disturbance could affect many aspects, such as academic achievement, and even the patient’s daily functioning since their ability to focus and to determine their priorities might shift.22 However, further studies regarding these are still needed in the future. Generally, several interventions that were found to improve executive function based on previous studies were computer games to improve metacognition, behavioral therapy, adaptation in the school teaching method, and, if possible, private tutors can be assigned so that the study method can be tailored individually to meet children’s needs.23–25 Physical activities with both acute exercise (only performed once every session) and chronic exercise (repetitive movements for a certain duration) might also improve several aspects of executive function, such as working memory and inhibitory control.
Intelligence Quotient and Health Related Quality of Life in Children with Chronic Kidney Disease
We found that IQ was not correlated with children’s HRQoL from either the children’s or parents’ perspectives. This finding differs from the results of previous studies. In patients with chronic disease, HRQoL might fluctuate and change over time and with disease progression.26,27 In patients with CKD, Kang et al showed that IQ might be affected after the patients had been diagnosed for >60 months. In this study, only two patients had been diagnosed for > 60 months.28 Thus, it is possible that the IQ results of the subjects in our study had not yet been affected by the underlying disease and, as the consequence, the HRQoL was found to not be correlated with IQ in this study. Another factor that might have caused the lack of a correlation between HRQoL and IQ in this study is that we had no baseline IQ in our samples. Thus, we could not conclude whether the patients’ IQ really decreased or whether the IQ results by the time we tested the subjects were the same as their baseline IQ. In clinical practice, we suggest for IQ to be examined on each stage of CKD and for baseline IQ to be gained from children in healthy condition, so that the causal relationship could be determined and prevention could be done in the future.
Staging, Treatment Modalities and Health Related Quality of Life in Children with Chronic Kidney Disease
We found that the higher the CKD stage, the lower the children’s HRQoL were. Children with more advanced CKD stage would have more physical and emotional burden. They could also have sleep disorder, depression, and also anxiety as the disease progresses. These might contribute to the lower HRQoL we found in children with more advanced CKD stage.29
This study also found that HRQoL from the children’s perspective was related to the treatment modality used, and children with CKD who underwent peritoneal dialysis and hemodialysis had lower HRQoL compared to those who underwent conservative therapy. This finding was in line with a previous study by Francis et al, who found that HRQoL was lower in children who underwent dialysis than in those who did not.30 Children who underwent dialysis might experience more pain, have more school abstains, and might also feel bored due to a longer time of therapeutic session, with a higher risk of complications and a higher frequency of hospitalization. These factors might cause children who underwent dialysis to have a lower HRQoL than those who are still on conservative treatment. Children with conservative treatment would not experience the same routine, pain, absence, and frequent hospitalization as those with dialysis. Thus, the might have better HRQoL. Previous studies also showed that children who received kidney transplantation had better HRQoL than those who received other treatment modalities.31 However, we could not analyze the impact of kidney transplantation in children in our samples because we had not yet been able to perform kidney transplantation in children in our hospital.
Study Limitations
In previous studies, CKD duration has been related to executive function, IQ, and HRQoL. In this study, since there were only two patients with a CKD duration > 60 months, the relationship between CKD duration and the study variables could not be determined. This might have affected the overall executive function scores in our study subjects, making it look normal by the time the subjects were tested. This might have also played a role in the absence of a relationship between IQ and HRQoL in this study.
None of the patient in this study had kidney transplantation. Previous studies showed that therapeutic modalities affect both HRQoL and neurocognitive functions. Thus, we could not analyze the impact of kidney transplantation on HRQoL and neurocognitive function in our population. We also only had two patients who underwent PD. To make a better conclusion regarding how treatment modality might affect someone’s HRQoL, bigger sample size on patients who underwent PD is needed.
We also had no baseline IQ or HRQoL results for participants in our study. Thus, we could not determine whether the IQ and HRQoL results of our participants were due to CKD. This might be one factor that caused the lack of a correlation between IQ and HRQoL in our study.
We suggest that in the future, a similar study that includes the subjects’ IQ and HRQoL baseline should be conducted to clearly see how CKD affects IQ and HRQoL. Ideally, neurocognitive function and HRQoL measurements should be performed more than once during the study period to determine the impact of disease progression on these variables and their relationships. Further studies on the best intervention method to retain executive function in children with CKD should be conducted. We also suggest that neurocognitive function and HRQoL assessment should be performed routinely in patients with CKD to monitor decline so that early recognition and intervention can be performed.
Conclusion
In conclusion, our study suggests that Health Related Quality of Life in children with CKD (parent proxy) was affected by the children’s executive function but not affected by the children’s IQ. To enhance the HRQoL of these children, it is essential to consider interventions and care strategies aimed at improving neurocognitive function, particularly executive function. Some interventions that can be considered are behavioral therapy, games or activities to improve metacognitive function, tailored study method for each children in school or using private tutor if possible, and also routine physical activities. However, future research is recommended to explore specific interventions and their clinical implications in the context of CKD management for children.
Ethics Statement
The authors assert that all procedures contributing to this work comply with the ethical standards with the Helsinki Declaration. Informed consent regarding the study was given to the parents and the patients before the data was taken. This study has been approved by by the Medical Research Ethics Committee of Dr. Hasan Sadikin General Hospital Bandung, Indonesia.
Acknowledgment
The authors thank Universitas Padjadjaran for the help granted in publishing this study. The authors also thank Edduwar I Riyadi, Psychiatrist for giving the permission for the authors to use the validated BRIEF questionnaire and also for Mapi Research Trust for letting the authors to use the PedsQLTM questionnaire.
Funding
The authors thank the Indonesian Endowment Fund (LPDP) scholarship and Universitas Padjadjaran for the financial help provided to finish and publish the study.
Disclosure
The authors report no conflicts of interest in this work.
References
1. Harambat J, van Stralen KJ, Kim JJ, Tizard EJ. Epidemiology of chronic kidney disease in children. Pediatr Nephrol. 2012;27(3):363–373. doi:10.1007/s00467-011-1939-1
2. Ardissino G, Dacco V, Testa S, et al. Epidemiology of chronic renal failure in children: data from the ItalKid project. Pediatrics. 2003;111(4):e382–7. doi:10.1542/peds.111.4.e382
3. El Shafei AM, Soliman Hegazy I, Fadel FI, Nagy EM. Assessment of quality of life among children with end-stage renal disease: a cross-sectional study. J Environ Public Health. 2018;2018:1–6. doi:10.1155/2018/8565498
4. Pardede SO, Rafli A, Gunardi H. Quality of life in chronic kidney disease children using assessment pediatric quality of life inventoryTM. Saudi J Kidney Dis Transplant. 2019;30(4):812. doi:10.4103/1319-2442.265456
5. Gerson AC, Wentz A, Abraham AG, et al. Health-related quality of life of children with mild to moderate chronic kidney disease. Pediatrics. 2010;125(2):e349–57. doi:10.1542/peds.2009-0085
6. Dotis J, Pavlaki A, Printza N, et al. Quality of life in children with chronic kidney disease. Pediatr Nephrol. 2016;31(12):2309–2316. doi:10.1007/s00467-016-3457-7
7. Tarigan M. Uji Validitas Konstruk Tes Wechsler Intelligence Scale For Children (WISC). J Stud Insa. 2022;9(2):168–186. doi:10.18592/jsi.v9i2.5599
8. Varni JW, Seid M, Kurtin PS. PedsQLTM 4.0: reliability and validity of the pediatric quality of life inventoryTM Version 4.0 generic core scales in healthy and patient populations. Med Care. 2001;39(8):800–812. doi:10.1097/00005650-200108000-00006
9. Wijaya EA, Solek P, Hakim DDL, Rossanti R, Widiasta A, Hilmanto D. Factors affecting neurocognitive function in children with chronic kidney disease: a systematic review. Int J Nephrol Renovasc Dis. 2022;Volume 15:277–288. doi:10.2147/IJNRD.S375242
10. Finkelstein FO, Wuerth D, Finkelstein SH. Health related quality of life and the CKD patient: challenges for the nephrology community. Kidney Int. 2009;76(9):946–952. doi:10.1038/ki.2009.307
11. Soni RK, Weisbord SD, Unruh ML. Health-related quality of life outcomes in chronic kidney disease. Curr Opin Nephrol Hypertens. 2010;19(2):153. doi:10.1097/MNH.0b013e328335f939
12. Kiliś-Pstrusińska K, Medyńska A, Chmielewska IB, et al. Perception of health-related quality of life in children with chronic kidney disease by the patients and their caregivers: multicentre national study results. Qual Life Res. 2013;22(10):2889–2897. doi:10.1007/s11136-013-0416-7
13. Sani F, Tarigan R, Widiasta A. Kualitas hidup anak dengan penyakit ginjal kronik di rumah sakit umum pusat hasan sadikin bandung. Sari Pediatr. 2022;24(1):31–35. doi:10.14238/sp24.1.2022.31-5
14. Eiser C, Eiser JR, Stride CB. Quality of life in children newly diagnosed with cancer and their mothers. Health Qual Life Outcomes. 2005;3(1):1–5. doi:10.1186/1477-7525-3-29
15. Elshahat S, Cockwell P, Maxwell AP, Griffin M, O’Brien T, O’Neill C. The impact of chronic kidney disease on developed countries from a health economics perspective: a systematic scoping review. PLoS One. 2020;15(3):e0230512. doi:10.1371/journal.pone.0230512
16. Imani PD, Aujo J, Kiguli S, Srivaths P, Brewer ED. Chronic kidney disease impacts health-related quality of life of children in Uganda, East Africa. Pediatr Nephrol. 2021;36(2):323–331. doi:10.1007/s00467-020-04705-1
17. Murphy C, Upshaw NC, Thomas AS, et al. Impact of executive functioning on health‐related quality of life of pediatric brain tumor survivors. Pediatr Blood Cancer. 2021;68(8):e29130. doi:10.1002/pbc.29130
18. Schraegle WA, Titus JB. Executive function and health-related quality of life in pediatric epilepsy. Epilepsy Behav. 2016;62:20–26. doi:10.1016/j.yebeh.2016.06.006
19. Otero TM, Barker LA, Naglieri JA. Executive function treatment and intervention in schools. Appl Neuropsychol Child. 2014;3(3):205–214. doi:10.1080/21622965.2014.897903
20. Johnson RJ, Warady BA. Long-term neurocognitive outcomes of patients with end-stage renal disease during infancy. Pediatr Nephrol. 2013;28(8):1283–1291. doi:10.1007/s00467-013-2458-z
21. Mendley SR, Matheson MB, Shinnar S, et al. Duration of chronic kidney disease reduces attention and executive function in pediatric patients. Kidney Int. 2015;87(4):800–806. doi:10.1038/ki.2014.323
22. Hall PA, Marteau TM. Executive function in the context of chronic disease prevention: theory, research and practice. Prev Med. 2014;68:44–50. doi:10.1016/j.ypmed.2014.07.008
23. Takacs ZK, Kassai R. The efficacy of different interventions to foster children’s executive function skills: a series of meta-analyses. Psychol Bull. 2019;145(7):653. doi:10.1037/bul0000195
24. Liu S, Yu Q, Li Z, et al. Effects of acute and chronic exercises on executive function in children and adolescents: a systemic review and meta-analysis. Front Psychol. 2020;11:554915. doi:10.3389/fpsyg.2020.554915
25. Diamond A, Lee K. Interventions shown to aid executive function development in children 4 to 12 years old. Science. 2011;333(6045):959–964. doi:10.1126/science.1204529
26. Jones JD, Kuhn T, Levine A, et al. Changes in cognition precede changes in HRQoL among HIV+ males: longitudinal analysis of the multicenter AIDS cohort study. Neuropsychology. 2019;33(3):370. doi:10.1037/neu0000530
27. Zyada F, Makar SH, Abdelrahman SM, Labana AH. Assessment of cognitive functions in children on regular hemodialysis and after renal transplantation. Middle East Curr Psychiatry. 2017;24(3):128–133. doi:10.1097/01.XME.0000516380.52486.97
28. Kang NR, Ahn YH, Park E, et al. Intellectual functioning of pediatric patients with chronic kidney disease: results from the KNOW-ped CKD. J Korean Med Sci. 2021;36(20). doi:10.3346/jkms.2021.36.e138
29. Kim D-S, Kim S-W, Gil H-W. Emotional and cognitive changes in chronic kidney disease. Korean J Intern Med. 2022;37(3):489. doi:10.3904/kjim.2021.492
30. Francis A, Didsbury MS, van Zwieten A, et al. Quality of life of children and adolescents with chronic kidney disease: a cross-sectional study. Arch Dis Child. 2019;104(2):134–140. doi:10.1136/archdischild-2018-314934
31. Morales P, Loza R, Vasquez J, Baique P, Reyes M. Quality of life of children with chronic kidney disease undergoing renal replacement therapy. J Kidney. 2018;4(173):1220–2472.
 © 2024 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2024 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
