Back to Journals » International Journal of Women's Health » Volume 16
Effect of Decision-to-Delivery Time of Emergency Cesarean Section on Adverse Newborn Outcomes at East Gojjam Zone Public Hospital, Ethiopia, March 2023: Multicenter Prospective Observational Study Design
Authors Damtew BS , Gudayu TW , Temesgan WZ , Hailu AM
Received 21 November 2023
Accepted for publication 25 February 2024
Published 7 March 2024 Volume 2024:16 Pages 433—450
DOI https://doi.org/10.2147/IJWH.S451101
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Professor Elie Al-Chaer
Beyene Sisay Damtew,1 Temesgen Worku Gudayu,2 Wubedle Zelalem Temesgan,2 Alemu Merga Hailu3
1Department of Midwifery, Arsi University, Assela, Ethiopia; 2Department of Midwifery, University of Gondar, Gondar, Ethiopia; 3Department of Midwifery, Wollega University, Nekemte, Ethiopia
Correspondence: Beyene Sisay Damtew, Email [email protected]
Background: An emergency cesarean section requires prompt delivery to reduce the risk for a pregnant woman or newborn. Studies have been conducted to investigate the relationship between decision-to-delivery time and neonatal outcomes, but the findings are contradictory. Therefore, this study aimed to assess the average of decision-to-delivery time of an emergency cesarean section and its effect on adverse neonatal outcomes at East Gojjam Zone Public Hospital.
Methods: A multicenter prospective study design would be carried out between November 2022 and January 2023. Using the consecutive method, a sample of 352 mother-newborn pairs was studied. Direct observation and face-to-face interviews were undertaken to gather the data using a semi-structured questionnaire. For both data input and analysis, Epi Data version 4.6 and Stata version 14 software were used. Both the crude and adjusted odds ratios were computed. Measure of significance was based on the adjusted odds ratio with a 95% confidence interval and a p-value of less than 0.05.
Results: Decision-to-delivery time interval within 30 minute was seen in 21.9% of emergency cesarean delivery. The study found a significant relationship between the first-minute low Apgar score and the delayed decision-to-delivery time interval (OR = 2.6, 95% CI: 1.1– 6, p = 0.03). In addition, determinant factors for poor 1st-minute Apgar scores include danger signs during pregnancy (AOR: 2.9, 95% CI: 1.1– 7.8, p = 0.03), women referred from another facility (AOR: 2.6, 95% CI: 1.5– 4.6, p = 001), and non-reassuring fetal heart rate (AOR: 4.2, 95% CI: 1.1– 17, p = 0.04). A delayed decision-to-delivery time interval is not statistically significantly associated with a low 5th-minute Apgar score or neonatal intensive care unit (NICU) admission.
Conclusion: The study found unfavorable 1st-minute Apgar score and a longer decision-to-delivery period than recommended. This duration and negative newborn outcomes may be reduced by increasing and involving comprehensive obstetric and neonatal care facilities with skilled emergency obstetric surgeons, such as clinical midwife, integrated emergency surgeon officers, and physician.
Keywords: decision-to-delivery time, cesarean delivery, fetal outcomes, Ethiopia
Introduction
Cesarean delivery is an incision of the abdomen and uterus to deliver the fetus, membrane, and placenta. It is commonly performed in Western countries; a study done in Texas shows one in three pregnant mothers undergo cesarean delivery.1 It is a life-saving procedure for either the mother or the fetus. Even though it is a lifesaving procedure, rapid increments of cesarean section carry adverse maternal and fetal outcomes.2
Cesarean section is the best course of action in 15% of deliveries to ensure the health of the mother and fetus as recommended by World Health Organization (WHO). The increasing rates of emergency Caesarean Sections raise various questions about whether they should be considered a normal delivery in the twenty-first century since the majority of cesarean deliveries are performed for obstetrical reasons, but some are simply requests of mothers that involve several risks for their newborns.3
The decision-to-delivery interval (DDI) of emergency cesarean section (CS) should not be more than 30 minutes, according to the National Institute of Clinical Excellence (NICE) recommendations, and a delay of more than recommended minutes in the presence of maternal or fetal impairment can have adverse effects.4 Decision-to-delivery time is the timeline between decisions and the actual delivery of the newborn.5 Emergency cesarean sections are performed immediately to reduce morbidity and mortality by preparing health professionals for special precautions.6 According to World Health Organization (WHO) reports from a systematic review of different continents, there was a higher incidence of neonatal respiratory distress syndrome with cesarean delivery.7 A retrospective study conducted in Germany shows a high risk of neonatal morbidity with emergency cesarean delivery.8 After an emergency cesarean section, there were high neonatal intensive care unit (NICU) admissions, severe acidosis, intrauterine death (stillbirth), and an Apgar score of 3 at 5 minutes.9 A study conducted in Brazil found that emergency cesarean deliveries resulted in NICU admissions and neonatal deaths.10
The majority of urgent cesarean section (CS) decision-to-delivery interval (DDI) reactions was longer and mostly affected by facility resources and the availability of staff.11 Measuring the effect of time from decision to delivery was used by a health professional to know and prevent unfavorable fetal outcomes.12 Since adherence to teamwork improves time from decision to delivery, as the WHO recommended.13
The effect of time on fetal outcome in a study conducted in England suggests that women who undergo cesarean delivery after 65 minutes have a 3% stillbirth rate.14 Delayed DDI time has a significant with unfavorable neonatal outcomes.15 According to a study in Berlin, 64.6% of decisions to incisions are completed within 10 minutes, 34.3% within 11–20 minutes, and only 1.1% take longer than 20 minutes. Women who underwent urgent indication of emergency cesarean section (EmCS) have low Apgar score outcomes.16
Based on epidemiological data, 46% of neonatal deaths occur within 24 hours in developing countries.17 A study done in Nigeria shows that neonates delivered with DDI greater than 75 minutes were more likely to die compared to those delivered within 30 minutes, and anesthesia time delay was the major cause of delay in carrying out emergency cesarean sections.18 According to a study conducted in Bahir Dar, Ethiopia, a decision-to-delivery time interval of emergency cesarean sections performed within 30 minute was 14.3 and 20.3%, and a decision-to-delivery time interval above the recommended time interval significantly affected adverse fetal outcomes.19,20 In Ethiopia, emergency cesarean delivery was by obstetrician, IESO, and MSc in clinical midwifery. Integrated Emergency Surgeon Officers (IESOs) are a specialized group of medical professionals in Ethiopia who provide emergency surgical care in resource-limited settings.21
Various studies have been conducted to investigate the relationship between DDI and neonatal outcomes, but the findings are contradictory. Some research recommends that a decision-to-delivery time greater than thirty minutes and within thirty minutes does not correlate with fetal outcomes. A study done in North Gondar supports this statement.22 Some other research shows adverse fetal outcomes increase with a delayed decision-to-delivery time. A study done in Bahir Dar supports this statement.19 The effect of prolonged DDI on fetal outcomes was the focus of this investigation.
Based on the 30-minute DDI recommendation, different findings indicate that the decision to a delivery time interval of 30 minutes has three phases: the decision to the operating room interval, which takes 10 minutes; the time arrived at the operating room to the incision time, which takes 15 minutes; and the incision to delivery time, which takes 5 minutes.23 This paper revealed the most delayed time phase and how it affects fetal outcomes.
Nowadays, increasing the rate of cesarean sections highly affects the time from decision-to-delivery and birth outcome.24 Prolonging the decision-to-delivery gap constitutes a third-phase delay in the provision of emergency obstetric care.
Materials and Method
Study Area
There are thirteen zones in the Amhara National Regional State, and East Gojjam is located in one of them. The East Gojjam Zone’s capital city, Debre Markos, is located about 300 kilometers (km) northwest of Ethiopia’s capital city, Addis Ababa. There are eleven Hospitals in the zone which are 10 primary Hospital (Lumame Primary Hospital, Bechena Primary Hospital, Mota Primary Hospital, Yejube Primary Hospital, Debre Elias Primary Hospital, Debre Work Primary Hospital, Shebel Primary Hospital, Dejen Primary Hospital, Mertolemaria Primary Hospital, Bibugn Primary Hospital) and one specialized Hospital (Debre Markos comprehensive specialized Hospital)
Study Design
A multicenter prospective observational study25,26 was conducted from November to January 2022/23.
Population
Source population: all pregnant mothers who undergo emergency cesarean section at East Gojjam Zone public Hospital.
Study population: all pregnant mothers who undergo emergency cesarean section at East Gojjam zone selected Hospital during the data collection period.
Inclusion and Exclusion Criteria
Inclusion criteria: All pregnant mothers who undergo emergency cesarean section.
Exclusion criteria: All pregnant mothers who undergo emergency cesarean section with preterm, ruptured uterus before decision, congenital anomalies, and twin pregnancy.
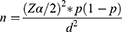
Sample Size Determination
The sample size for this study was determined by using a single population proportion formula by considering the following assumptions; 29.5% proportion of decision to a delivery time of emergency cesarean section done,27 95% level of confidence, and 5% margin of error.
Where n = required sample size
@= level of significant
z = standard normal distribution curve value for 95% confidence level = 1.96
P = proportion of decision-to-delivery time of emergency cesarean section
d = margin of error
With a 10% non-response rate the final sample size was 352.
Sampling Technique
There are eleven public hospitals in East Gojjam zone, among these Hospitals 30% are selected based on tier only one Specialized Hospital (Debre Markos Specialized); among 10 primary hospital; the two randomly selected, Yejube and Lumame are included in the study area with total population underwent emergency cesarean section last year at the same study period which is November–January were 643 (Figure 1)
 |
Figure 1 Schematic presentation of the sampling procedure. |
Study Variable
Dependent variable: Adverse fetal outcome of emergency cesarean section: first-minute Apgar score < 7, fifth-minute Apgar score < 7, NICU admission, stillbirth, and newborn death within 48 hours.
Independent variable: Socio-demographic factors, obstetric factors, decision to different activity, Indications for emergency cesarean section, procedure-related factors, Provider and resource factor.
Operational Definition
Decision time: when the physician or the surgeon who performs the cesarean section decides to prepare her for operation delivery.
Delivery time: when all parts of the fetus are delivered via incised abdomen and uterus.
Emergency cesarean section: An immediate threat to the life of the woman or fetus.
Decision-to-delivery time: A time range from the decision for EmCS to delivery of a newborn. More than 30 min was taken as a delayed decision-to-delivery time, while less than or equal to 30 minutes was the appropriate time for an emergency cesarean section.28,29
Transfer time: The time from the decision to arrive at the operation theater.
Anesthesia time: The time taken from arrival at the operation theater to skin incision time.30
Adverse neonatal outcome: Presence of the following fetal outcomes within 48 hours: stillbirth, 1st -minute Apgar score of <7, 5th minutes of Apgar score <7, admission to the NICU, and newborn death.19,31
Data Collection Tool, Method, and Procedure
The data collection tool was adapted from a previous study and modified using a literature review and collected using a semi-structured questionnaire face-to-face interview and observation.19 Six BSc midwives and one MSc male midwife supervisor were chosen, and they received training on how to gather data, how to communicate study participants, how to observe them, how to save information, and how to have a better handle on the entire data collecting process.
Data Quality Control
To maintain consistency and improve understandability, the questions are written in English, translated into Amharic, and then returned to English. A 5% pretest for response, language clarity, and questionnaire appropriateness was conducted at Bechena Primary Hospital.
Data Processing and Analysis
After being checked, coded, and put into Epi Data version 4.6, the data were exported to Stata IC14 for analysis. The socio-demographic, obstetric, professional, resource and decision-to-different-time activity characteristics of the participants were presented using descriptive statistics. The adverse neonatal outcomes would initially be determined; then, the results would be dichotomized into yes or no, depending on the outcomes. Finally, binary logistic regression was fitted to determine the relationship between decision-to-delivery time and fetal outcomes.
Ethics Approval and Consent to Participate
All methods were conducted according to the ethical standards of the declaration Helsinki. The study was conducted under the Ethiopian Health Research Ethics Guidelines. Ethical clearance was obtained from the University of Gondar’s Ethical Review Committee with Ref-MIDW/30/2015 E.C. A formal letter of administrative and case team manager approval was obtained from the three hospitals. Informed consent was taken from each of the study participants.
Results
Result of Socio-Demographic Characteristics
Within the study period, 95% of mothers provided complete answers to the interview questions.
Among the study’s participants, 292 (87.4%) are from comprehensive specialized hospitals, and 12.6% are from primary hospitals.
The research population’s median age was 28±5 years, with most participants aged 25–29.
The majority of the study’s participants (91.3%) are married, and 47% are housewives. Nearly two-thirds of the study participants (67.7%) are living in urban.
Regarding maternal education, only 21.6% of them have level of diploma and above (Table 1).
 |
Table 1 Socio-Demographic Characteristics of Study Participants at East Gojjam Zone, Ethiopia, March 2023 |
Obstetrics Related Factors
One hundred and seventy-six (52.7%) study participants decided to have an emergency cesarean section during the latent stage of labor. Over sixty percent of them (61.1%) are multigravida.
About 95.5% of the study’s participants had at least one ANC follow-up. Over half of them (55.63%) contain at least four and above ANC contact.
A total of 59.9% of pregnant women with ANC contacts receive advice on birth preparedness and complication readiness. Eighteen (47.3%) of the mother’s symptoms and signs of antepartum hemorrhage were present during her pregnancy. About 64.1% of the study participants were referred from another facility, and nearly all of them (96.7%) were term pregnancies. When informed of the need for an emergency cesarean section, 89.5% of the study participants immediately consented to the operation (Table 2).
 |
Table 2 Obstetric Factor of the Study Population at East Gojjam Zone Public Hospital, March 2023 |
Facility Resource, Professional, and Procedure-Related Factor
At the study institution, there were two functional tables in each of the two primary hospitals and four functional tables in the comprehensive specialized hospital. When the women arrived at the operating room for an emergency cesarean section, about 84% of the free-function operating tables were there. Eighty-six percent of the equipment required for operations is on hand in the operating room when women arrive.
Throughout the study period, there were eight IESO surgeons from the three hospitals performing emergency cesarean sections. IESO conducted the most operations, 120 (35.9%). Second, MSc clinical midwifery students practicing at Debre-Markos Specialized Hospital performed the procedure (26.7%). There were 23.4% and 14.1% of operations performed by obstetricians and clinical midwives, respectively. About 44.6% of anesthesia was given by BSc students, nearly two-thirds of babies delivered by operation were taken, and basic neonatal care was given by a BSC midwifery holder (Table 3).
 |
Table 3 Health Professional, Resource, and Procedure-Related Factors at East Gojjam Zone Public Hospital, March 2023 |
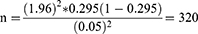
Indication of Emergency Cesarean Section
The most common cause of an emergency cesarean delivery, accounting for 37.7% of cases, was a non-reassuring fetal heartbeat for both tachycardia and bradycardia (NRFHR). Others, grade III meconium-stained amniotic fluid (GIII MSAF) with the latent first stage of labor, cephalo-pelvic disproportion (CPD), two or more cesarean section scars in labor, antepartum hemorrhage, both placenta previa and placenta abruption (APH), and obstructed labor including imminent rupture, are 13.8%, 11.4%, 9.9%, 5.4%, and 4.8%, respectively (Figure 2).
 |
Figure 2 Indication of emergency cesarean section at east Gojjam zone public Hospital, Ethiopia 2023. |
APH: Antepartum hemorrhage, C/S: cesarean section, GIIIMSAF: grade III meconium stained amniotic fluid, LFSOL: latent first stage of labour.
Decision-to-Delivery Time Interval and Decision to a Different Activity
With an interquartile range, the median decision-to-delivery time was 42 (31–55). Only 73 (21.9%) emergency cesarean sections were performed with a decision-to-delivery time within 30 minutes. About 75.1% of emergency C-sections had a delivery time of “31 to 75 minutes.” Only 3% of emergency C-sections have a delayed decision-to-delivery time of more than 75 minutes. About 52.7% of mothers who have decided for ECS were transferred to the operating room within 10 minutes after the decision. For more than 90% of them, anesthesia time took more than 15 minutes. In 93% of cases, the duration from skin incision to newborn delivery was shorter than five minutes. Operation time or the time taken from incision to skin closure of more than 24 minutes accounts for 45% (Table 4).
 |
Table 4 Decision-to-Delivery and Decision to Different Activity Emergency Cesareans Section at East Gojjam Zone Public Hospital |
Socio-Demographic, Obstetric, Facility Resource, Professional, and Procedure Factors Cross Tabulation with Adverse Neonatal Outcomes
Ninety percent of first-minute low Apgar scores and all neonatal deaths were observed at a comprehensive, specialized hospital. Seventy-one percent of low Apgar scores were observed in a patient who was referred from another facility. Among the list of indications, 52.9% of low 1st-minute Apgar scores represent a non-reassuring fetal heart rate.
All stillbirths4 were observed in multigravida mothers and were an indication of antepartum hemorrhage, obstructed labor, NRFHR, and eclampsia.
Female newborns accounted for 75% of stillbirths, whereas male newborns accounted for 85% of neonatal deaths (Table 5).
 |
Table 5 Factors Cross-Tabulated with the Adverse Birth Outcome at East Gojjam Zone Public Hospital, 2023 |
Adverse Neonatal Outcome of Emergency Cesarean Section
Adverse neonatal outcomes were seen for the first minute, fifth minute, NICU admission, stillbirth, and neonatal death.
A poor first-minute Apgar score is present in 36.8% of all newborns, and 11.4% of newborns have a low fifth-minute Apgar score.
About 1.2% of all newborns were stillborn or had no life when they were born, but they were alive when the decision to perform an emergency cesarean section was made.
After being delivered alive, 2.2% of babies died (Figure 3).
 |
Figure 3 Adverse fetal outcome emergency cesarean section at East Gojjam zone Public Hospital, Ethiopia 2023. |
Decision-to-Delivery Time Interval and Factors Associated with Adverse Fetal Outcome of Emergency Cesarean Section
The fetal outcome of a low Apgar score in the first minute was considered a dependent variable, and factors (danger signs during pregnancy, referral from another facility, delayed acceptance of informed consent, anesthesia technique, indication, patient transfer time, anesthesia time, and decision-to-delivery time) were considered independent variables with a COR of p-value below 0.25. The combined effect of the factors was studied using a binary logistic regression test.
With an adjusted odds ratio (AOR), a delayed decision-to-delivery time interval has a 2.6-times lower first-minute Apgar score as compared to within thirty minutes (AOR: 2.6, 95% CI: 1.1–6, p = 0.03). In addition, statistically, a significant factor was observed with those who had danger signs during pregnancy (AOR: 2.9, 95% CI: 1.1–7.8, p = 0.04), were referred from another facility (AOR: 2.6, 95% CI: 1.5–4.6, p = 001), and had an indication of a non-reassuring fetal heart rate (AOR: 4.2, 95% CI: 1.1–17, p = 0.04).
Pregnant mothers who had danger signs during pregnancy had 2.9 times lower first-minute Apgar scores as compared to those who did not have danger signs. Indications for NRFHR had a 4.2-fold lower first-minute Apgar score as compared to the reference indications.
The fifth-minute Apgar score was taken as the dependent variable, and determinant factors (level of institution, patient residence, danger sign during pregnancy, referral status of the patient, number of regional anesthesia attempts, patient transfer time, anesthesia time and decision-to-delivery time interval) were taken as independent factors. A combination effect on the fifth-minute Apgar score was observed with a multivariable logistic regression test for those with a COR of p-value ≤ 0.25.
With an adjusted odds ratio (AOR), a delayed decision-to-delivery time interval has a 3.2-times lower fifth-minute Apgar score as compared to within thirty minutes (AOR: 3.8, 95% CI: 0.6–16, p = 0.2), but statistically no significant difference is observed. However, a significant factor is observed for anesthesia time >15 minutes (AOR: 0.15, 95% CI: 0.03–0.8, p = 0.03). Those mothers who have a danger sign during pregnancy have a 2.1 times lower fifth-minute Apgar score as compared to those who do not have a danger sign, but this is a statistically not significant difference (OR 2.1, 95% CI 0.7–6.4, p = 0.07). Mothers who came from rural areas had a 1.04 times lower fifth-minute Apgar score as compared to those who came from urban areas (OR 1.04, 95% CI 0.5–2.3, P = 0.54); statistically, there was no difference observed.
Neonatal NICU admission was taken as a dependent variable, and determinant factors (patient residences, time of procedure done, intraoperative difficulty, weight of the neonate, and decision-to-delivery time interval) were taken as independent variables.
With an adjusted odds ratio (AOR), a delayed decision-to-delivery time interval is 22% less likely lead to NICU admission compared to within the recommended time interval (AOR: 0.78, 95% CI: 0.3–2.3, p = 0.6), but statistically no significant difference is observed. However, a low birth weight is significantly associated with NICU admission. The odds of weight less than 2.5 kilograms were 9.8 times higher in NICU admissions as compared to the normal weight range (OR 9.8, 95% CI 2.5–37, p = 0.001). Statistically, the residency of a patient (OR 2.2, 95% CI 0.9–5, p = 0.09), the nighttime of the procedure (OR 1.6, 95% CI 0.6–3.9, p = 0.3), and intra-operative difficulty (OR 1.9, 95% CI 0.5–7, P = 0.3) have no association with neonatal NICU admission (Table 6). (COR 95% CI between DDI and Fetal Outcomes (Table 7))
 |
Table 6 Factors Associated with Adverse Fetal Outcome at East Gojjam Zone Public Hospital March 2023 |
 |
Table 7 Table of Binary Logistic Regression Between Decision-to-Delivery Time Interval and Fetal Outcomes |
Discussion
It has become necessary to evaluate the feasibility of recommending a decision-to-delivery time interval of 30 minutes for an emergency cesarean section and its effect on the fetal outcome. This study found that the decision-to-delivery time of an emergency cesarean case within 30 minutes was 21.9%. This study also analyzed the proportion of decision-to-delivery time for emergency cesarean section cases in specialized and primary hospitals. The proportion of decision-to-delivery time for emergency cesarean cases in comprehensive specialized hospitals within 30 minutes was 16%, which is parallel to the study found in Bahir Dar (14.3) and north Gondar (19.6%), but far from the recommended proportion.19,22 This similarity may be because all of them are academic hospitals with medical interns, anesthesia students, and trainees in obstetrics and gynecology surgery who perform the majority of the activity. Additionally, there is also a comparable patient load, limited surgical material, and the educational background of the staff.
The percentage number of emergency cesarean delivery made within 30 minutes at the study’s primary hospital was 63%. This proportion was higher than in a study done in Ethiopia: Bahir Dar, North Gondar, and South Gondar.20,22,32 This difference may be due to there being no surgical waiting list as a result of less patient load, the presence of standby surgical staff during emergency hours, including anesthetists and scrub nurses, and cooperation in patient transfer from the labor rooms to the operation room since there are no students who are training, which led to a busy obstetric service. Also, there are no elective procedures that make operation rooms and tables busy.
This study found the mean time from decision to delivery was 44±15 minutes. This is consistent with the study conducted in Ethiopia: North Gondar (42 minutes), Bahir Dar (43.7 minutes), and India (42 minutes).19,22,33 The reason for this consistency may be that they used a primary data source and a prospective observational follow-up, which are similar to this study’s source of data and study design. On the other hand, this finding is lower than a study done in Uganda (92 minutes) and Nigeria (119.2 minutes).18,34 This may be the outcome of research carried out in Uganda utilizing secondary data; the validity of the data and the time of registration may influence the findings. In Ethiopia, all maternal treatments are free, but in Nigeria, women who require an emergency cesarean section must pay a price for the surgery’s materials before the procedure, which might delay the DDI.
This study shows that a decision-to-delivery time interval above 30 minutes significantly affected the first-minute Apgar score, which is consistent with a study finding in Phuentsholing Hospital.27 This is because they only analyze urgent cases, which might have a major impact on the Apgar score of the first minute, whereas this study covers all categories and uses a comparable urgent indication sample. On the other hand, contrary findings were reported from a study done in Ethiopia, Tanzania, Nigeria, and India.18,19,22,35,36 This may be because they performed their research using urgency categorization categories one and two, whereas our analysis covered all women who had emergency cesarean sections by excluding elective procedures and omitting exclusion criteria. Additionally, those with crash indicators like cord prolapse and fetal heart rate were positively impacted, while those with non-urgent categories two and three, such as those with eclampsia or preeclampsia and failed inductions that did not advance labor, were also impacted by respiratory conditions because fluid-filled lungs were not excreted by the birthing process and that affected the first minute Apgar score.37
In addition to DDI >30 minutes, a danger sign during pregnancy (OR: 2.9, 95% CI: 1.09–7.93, p = 034) significantly affected the first-minute Apgar score: this finding was consistent with a study done in Thailand.38 This consistency may be because danger signs’ effects on birth outcomes are not influenced by geography but rather by their severity and type.
Indication (NRFHR) of this study shows that it significantly affected the first-minute Apgar score (OR: 4.2, 95% CI: 1.1–17, p = 0.04), which was a similar finding reported by Chandra Kant et al,39 but the contrary finding was reported from a study done in Tanzania.35 This controversial report may be the result of the heterogeneity of factors that contribute to NRFHR in the uterus; some factors, such as uterine hyperstimulation and aortocaval compression, cause reversible NRFHR, which is transient and does not affect the first-minute Apgar score. Other factors, such as cord compression and placental detachments, cause irreversible NRFHR, which may affect the first-minute Apgar score.
The duration of DDI (>30 minutes) did not statistically correlate with neonatal outcome of fifth-minute Apgar score and NICU admission; this finding was consistent with studies done in Ethiopia, Tanzania, Nigeria, and India.18,19,22,35,36 This consistency may be due to the fact that all studies used a clinical diagnostic to identify the adverse fetal outcome rather than the most useful diagnosis like umbilical cord blood gas analysis (PH), which indicates intrauterine and post-delivery newborns’ well-being.
This study found that there were four stillbirths and seven neonatal losses within 48 hours. There were nearly the same number of stillbirths (three), a proportional neonatal death that was reported by a study done in Ethiopia.19 This consistent proportion may be due to a similar supply of medical equipment, the staff’s similar educational backgrounds in handling affected neonates early on, and a similar protocol and guidelines used for managing affected newborns.
Low birth weight (<2.5 kg) was significantly associated with NICU admission; this result was consistent with studies done in Ethiopia and Tanzania.40,41 This consistency may be because low-birth weight newborns are more likely to experience problems later in life, and they might have difficulty feeding, increasing weight, and fighting off infection. In addition, they have very little body fat, which makes them frequently struggle to stay warm in comfortable temperatures, which later brings them to the NICU.
Limitation and Strength
Limitation
- It does not contain equal exposure and non-exposure to calculate relative risk, as it was evident that patients could not be randomized at random to have a delivery before or after the 30-minute time. Since it needs follow-up and a long period to have both equal 30-minute and above 30-minute study participants.
- Observational bias.
Strength
- The study uses a representative sample size, much larger than the study conducted previously in Ethiopia.
- The study uses primary data, which gives precise information.
Conclusion
Above three-fourths of emergency cesarean cases were done beyond the recommended decision-to-delivery time interval. The recommended time interval was achieved by crash indications like cord prolapse and antepartum hemorrhage.
The first-minute Apgar score was significantly impacted by the decision-to-delivery time of an emergency C-section with a duration of more than 30 minutes.
The first-minute Apgar score was strongly impacted by pregnant women who had danger signs during pregnancy, those who were referred from another hospital, and those who showed evidence of an abnormal fetal heart rate.
According to this study, prolonged DDT did not have an impact on fifth-minute Apgar and NICU admission.
Acknowledgment
The author’s gratitude goes to University of Gondar College of Medicine and Health science, for Ethical clearance.
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Disclosure
The authors report no conflicts of interest in this work.
References
1. Saade GR, Spong CY. Introduction. Cesarean delivery. Semin Perinatol. 2012;36(5):307. doi:10.1053/j.semperi.2012.04.029
2. He Y, Wu X, Zhu Q, et al. Combined laparoscopy and hysteroscopy vs. uterine curettage in the uterine artery embolization-based management of cesarean scar pregnancy: a retrospective cohort study. BMC Women’s Health. 2014;14:116. doi:10.1186/1472-6874-14-116
3. Sharma S, Dhakal I. Cesarean vs vaginal delivery: an institutional experience. J Nepal Med Assocc. 2018;56(209):535–539. doi:10.31729/jnma.3467
4. National Institute forH, Care E Copyright ©. NICE Process and Methods Guides. Developing NICE Guidelines: The Manual. London: National Institute for Health and Clinical Excellence, unless otherwise stated; 2015.
5. Rashid N, Nalliah S. Understanding the decision-delivery interval in cesarean births. IeJSME. 2007;1(2):61–68. doi:10.56026/imu.1.2.61
6. Tyner JE, Rayburn WF. Emergency cesarean delivery: special precautions. Obstet Gynecol Clin N Am. 2013;40(1):37–45. doi:10.1016/j.ogc.2012.11.003
7. Soto-Vega E, Casco S, Chamizo K, Flores-Hernández D, Landini V, Guillén-Florez A. Rising trends of cesarean section worldwide: a systematic review. Obstet Gynecol Int J. 2015;3(2):00073.
8. Hillemanns P, Hasbargen U, Strauss A, Schulze A, Genzel-Boroviczeny O, Hepp H. Maternal and neonatal morbidity of emergency caesarean sections with a decision-to-delivery interval under 30 minutes: evidence from 10 years. Arch Gynecol Obstetrics. 2003;268(3):136–141. doi:10.1007/s00404-003-0527-4
9. Pires-Menard A, Flatley C, Kumar S. Severe neonatal outcomes associated with emergency cesarean section at term. J Matern Fetal Neonatal Med. 2021;34(4):629–633. doi:10.1080/14767058.2019.1611770
10. Almeida MA, Araujo Júnior E, Camano L, Peixoto AB, Martins WP, Mattar R. Impact of cesarean section in a private health service in Brazil: indications and neonatal morbidity and mortality rates. Ces Gynekol. 2018;83(1):4–10.
11. Spencer MK, MacLennan AH. How long does it take to deliver a baby by emergency caesarean section? Aust N Z J Obstetrics Gynaecol. 2001;41(1):7–11. doi:10.1111/j.1479-828X.2001.tb01287.x
12. Bloom SL, Leveno KJ, Spong CY, et al. Decision-to-incision times and maternal and infant outcomes. Obstetrics Gynecol. 2006;108(1):6–11. doi:10.1097/01.AOG.0000224693.07785.14
13. Lecerf M, Vardon D, Morello R, Lamendour N, Dreyfus M. Can we do a cesarean section in less than 30min in unsuitable premises in order to follow the recommendations of the ACOG? J Gynecol Obstet Biol Reprod. 2013;42(4):393–400. doi:10.1016/j.jgyn.2012.12.010
14. Thomas J, Paranjothy S, James D. National cross sectional survey to determine whether the decision to delivery interval is critical in emergency caesarean section. BMJ. 2004;328(7441):665. doi:10.1136/bmj.38031.775845.7C
15. Tashfeen K, Patel M, Hamdi IM, Al-Busaidi IHA, Al-Yarubi MN. Decision-to-delivery time intervals in emergency caesarean section cases: repeated cross-sectional study from Oman. Sultan Qaboos Univ Med J. 2017;17(1):e38–e42. doi:10.18295/squmj.2016.17.01.008
16. Heller G, Bauer E, Schill S, et al. Decision-to-delivery time and perinatal complications in emergency cesarean section. Dtsch Arztebl Int. 2017;114(35–36):589–596. doi:10.3238/arztebl.2017.0589
17. Baqui AH, Mitra DK, Begum N, et al. Neonatal mortality within 24 hours of birth in six low-and lower-middle-income countries. Bull World Health Organ. 2016;94(10):752. doi:10.2471/BLT.15.160945
18. Bello FA, Tsele TA, Oluwasola TO. Decision-to-delivery intervals and perinatal outcomes following emergency cesarean delivery in a Nigerian tertiary hospital. Int J Obstetrics Gynaecol. 2015;130(3):279–283. doi:10.1016/j.ijgo.2015.03.036
19. Kitaw TM, Tsegaw Taye B, Tadese M, Getaneh T. Effect of decision to delivery interval on perinatal outcomes during emergency cesarean deliveries in Ethiopia: a prospective cohort study. PLoS One. 2021;16(11):e0258742. doi:10.1371/journal.pone.0258742
20. Kitaw TM, Limenh SK, Chekole FA, Getie SA, Gemeda BN, Engda AS. Decision to delivery interval and associated factors for emergency cesarean section: a cross-sectional study. BMC Pregnancy Childbirth. 2021;21(1):1–7. doi:10.1186/s12884-021-03706-8
21. Gobeze AA, Kebede Z, Berhan Y, Ghosh B. Clinical performance of emergency surgical officers in southern Ethiopia. Ethiop J Health Sci. 2016;26(5):463–470. doi:10.4314/ejhs.v26i5.8
22. Temesgen MM, Gebregzi AH, Kasahun HG, Ahmed SA, Woldegerima YB. Evaluation of decision to delivery time interval and its effect on feto-maternal outcomes and associated factors in category-1 emergency caesarean section deliveries: prospective cohort study. BMC Pregnancy Childbirth. 2020;20(1):164. doi:10.1186/s12884-020-2828-z
23. Sunsaneevithayakul P, Talungchit P, Wayuphak T, Sirisomboon R, Sompagdee N. Decision-to-delivery interval after implementation of a specific protocol for emergency caesarean delivery because of category iii fetal heart rate tracings. J Obstet Gynaecol Canada. 2022;44:1153–1158. doi:10.1016/j.jogc.2022.09.001
24. Beyene MG, Zemedu TG, Gebregiorgis AH, Ruano AL, Bailey PE. Cesarean delivery rates, hospital readiness and quality of clinical management in Ethiopia: national results from two cross-sectional emergency obstetric and newborn care assessments. BMC Pregnancy Childbirth. 2021;21(1):571. doi:10.1186/s12884-021-04008-9
25. Ranganathan P, Aggarwal R. Study designs: part 1–An overview and classification. Perspect Clin Res. 2018;9(4):184. doi:10.4103/picr.PICR_124_18
26. Berger ML, Dreyer N, Anderson F, Towse A, Sedrakyan A, Normand S-L. Prospective observational studies to assess comparative effectiveness: the ISPOR good research practices task force report. Value Health. 2012;15(2):217–230. doi:10.1016/j.jval.2011.12.010
27. Dorjey Y, Tshomo Y, Wangchuk D, et al. Evaluation of decision to delivery interval and its effect on feto‐maternal outcomes in category‐i emergency cesarean section deliveries in phuentsholing general hospital, 2020: a retrospective cross‐sectional study. Health Sci Rep. 2023;6(1):e1050. doi:10.1002/hsr2.1050
28. Obstetricians ACo, Gynecologists. ACOG committee opinion no. 487: preparing for clinical emergencies in obstetrics and gynecology. Obstetrics Gynecol. 2011;117(4):1032–1034. doi:10.1097/AOG.0b013e31821922eb
29. Hughes NJ, Namagembe I, Nakimuli A, et al. Decision-to-delivery interval of emergency cesarean section in Uganda: a retrospective cohort study. BMC Pregnancy Childbirth. 2020;20(1):324. doi:10.1186/s12884-020-03010-x
30. Mishra N, Gupta R, Singh N. Decision delivery interval in emergency and urgent caesarean sections: need to reconsider the recommendations? J Obstet Gynecol India. 2018;68(1):20–26. doi:10.1007/s13224-017-0991-6
31. Abdullahi YY, Assefa N, Roba HS. Magnitude and determinants of immediate adverse neonatal outcomes among babies born by cesarean section in public hospitals in Harari Region, Eastern Ethiopia. Res Rep Neonatal. 2021;11:1–12. doi:10.2147/RRN.S296534
32. Degu Ayele A, Getnet Kassa B, Nibret Mihretie G, Yenealem Beyene F. Decision to delivery interval, fetal outcomes and its factors among emergency caesarean section deliveries at South Gondar Zone Hospitals, Northwest Ethiopia: retrospective cross-sectional study, 2020. Int J Women’s Health. 2021;Volume 13:395–403. doi:10.2147/IJWH.S295348
33. Singh R, Deo S, Pradeep Y. The decision-to-delivery interval in emergency Caesarean sections and its correlation with perinatal outcome: evidence from 204 deliveries in a developing country. Trop doctor. 2012;42(2):67–69. doi:10.1258/td.2012.110315
34. Nakintu E, Murokora D. Emergency caesarean sections: decision to delivery interval and obstetric outcomes in nsambya hospital, Uganda-A cross sectional study. J Gynecol. 2016;1(4):122.
35. Hirani BA, Mchome BL, Mazuguni NS, Mahande MJ. The decision delivery interval in emergency caesarean section and its associated maternal and fetal outcomes at a referral hospital in northern Tanzania: a cross-sectional study. BMC Pregnancy Childbirth. 2017;17(1):1–6. doi:10.1186/s12884-017-1608-x
36. Boehm FH. Decision to incision: time to reconsider. Am J Clin Exp Obstet Gynecol. 2012;206(2):97–98. doi:10.1016/j.ajog.2011.09.009
37. Hooper SB, Te Pas AB, Kitchen MJ. Respiratory transition in the newborn: a three-phase process. Arch Dis Childhood-Fetal Neonatal Ed. 2016;101(3):F266–F71. doi:10.1136/archdischild-2013-305704
38. Attah R, Hadiza G. Decision to delivery interval and perinatal outcome for category one caesarean section in a tertiary hospital. Ibom Med J. 2020;13(2):81–89. doi:10.61386/imj.v13i2.192
39. Jadhav CA, Tirankar V, Gavandi P. Study of early perinatal outcome in lower segment caesarean section in severe foetal distress at tertiary care centre. Int J Reprod Contraception Obstetrics Gynecology. 2020;9(3):1259–1268. doi:10.18203/2320-1770.ijrcog20200911
40. Mitao M, Philemon R, Obure J, Mmbaga BT, Msuya S, Mahande MJ. Risk factors and adverse perinatal outcome associated with low birth weight in Northern Tanzania: a registry-based retrospective cohort study. Asian Pac J Reprod. 2016;5(1):75–79. doi:10.1016/j.apjr.2015.12.014
41. Ukke GG, Diriba K. Prevalence and factors associated with neonatal hypothermia on admission to neonatal intensive care units in Southwest Ethiopia–a cross-sectional study. PLoS One. 2019;14(6):e0218020. doi:10.1371/journal.pone.0218020
 © 2024 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2024 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.