Back to Journals » Journal of Asthma and Allergy » Volume 16
Effect of Air Pollutants and Meteorological Factors on Daily Outpatient Visits of Allergic Rhinitis in Hohhot, China
Authors Wang X, Gao C, Xia Y, Xu X, Li L, Liu Y, Yao X, Cao N, Li Z, Fang X
Received 11 July 2023
Accepted for publication 9 October 2023
Published 1 November 2023 Volume 2023:16 Pages 1217—1228
DOI https://doi.org/10.2147/JAA.S430062
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Luis Garcia-Marcos
Xue Wang,1,* Chenghua Gao,2,* Yuan Xia,1 Xiaoqian Xu,1 Lehui Li,1 Yan Liu,1 Xing Yao,3 Ning Cao,1 Zichao Li,1 Xin Fang1
1Public Health College, Inner Mongolia Medical University, Hohhot, People’s Republic of China; 2School of Public Health and Emergency Management, Southern University of Science and Technology, Shenzhen, 518055, People’s Republic of China; 3Infection Control Department, Inner Mongolia People’s Hospital, Hohhot, People’s Republic of China
*These authors contributed equally to this work
Correspondence: Xin Fang, Public Health College, Inner Mongolia Medical University, Hohhot, Inner Mongolia, People’s Republic of China, Tel +86 18686066179, Email [email protected]
Objective: There is limited evidence that atmospheric pollutants are associated with the number of allergic rhinitis (AR) visits. This study aimed to investigate the relationship between atmospheric pollutants and meteorological factors and the number of daily visits for AR in Hohhot City, providing a theoretical basis for further research on the effects of atmospheric pollutants on AR.
Methods: Microsoft Excel 2016 was used to collect and organize the AR outpatient consultation data, air pollution and meteorological data in Hohhot City during 2018– 2020, and the data were descriptively analyzed and Spearman correlation test was performed using SPSS22.0; A generalized additive model was built in R4.2.3 to analyze the effect of air pollution on the number of AR visits and its lagged and cumulative effects, while the robustness of the model was tested using a two-pollutant analysis. Finally, we analyzed the effects of the interaction of temperature, relative humidity and pollutants on the number of AR visits.
Results: The daily average concentrations of PM2.5, PM10, SO2, NO2, CO, and O3 in Hohhot during 2018– 2020 were 38.1 μg/m3, 83.3 μg/m3, 36.1 μg/m3, 15.1 μg/m3, 14.2 mg/m3, and 99.95 μg/m3, respectively, with the concentrations of PM2.5 and PM10 exceeding the secondary limit of the national standard. The results of the generalized additive model analysis showed that the RR and 95% CI of the effect of each 10 μg/m3 increase in pollutant concentration (1 mg/m3 increase in CO) on the number of AR outpatient clinics were 1.008 (1.001– 1.016), 1.002 (1– 1.005), 1.072 (1.033– 1.113), 1.020 (1007– 1.034), 1.033 (1.014– 1.052), 0.987 (0.9804– 0.9936).
Conclusion: Short-term exposure to PM2.5, PM10, SO2, NO2, and CO was significantly associated with an increase in AR clinic visits, and short-term exposure to O3 was significantly associated with a decrease in allergic rhinitis clinic visits.
Keywords: allergic rhinitis, air pollutants, time series study, interaction effect
Introduction
Air pollution is a major environmental risk factor affecting global health events. The human respiratory tract is directly connected to the outside world and is susceptible to air pollution and meteorological changes that can induce or exacerbate other systemic diseases. It has been shown that air pollution may lead to an increased incidence of respiratory diseases,1,2 cardiovascular diseases3,4 and population-based allergic diseases,5 and that there is a significant lag effect of air pollution on health. In recent years, with the industrialization of cities, westernized lifestyles, and drastic environmental changes, the incidence of AR has shown a significant increase, with prevalence rates as high as 50% of the global population.6 Previous studies have shown that the prevalence of allergic rhinitis varies regionally, and there is growing evidence that both environmental and genetic factors play important roles in the aetiology of allergic diseases.7,8
China has a large population and even slight increases in pollutant concentrations can lead to significant health losses. Air pollutant concentrations are higher in the northern regions of China due to the dry climate and the burning of coal for heating in the winter, which can have more serious health effects.9 Hohhot is located on the northern border of China (Figure 1), with pocket-shaped landscapes with openings facing southwest, where air pollutants are blocked and retained to easily accumulate and aggregate, and diffusion conditions are poor, making it easy to form heavily polluted weather under unfavorable meteorological conditions. According to the composite index of ambient air quality in the Ecological Environment Bulletin of Inner Mongolia Autonomous Region in 2021, the air quality in Hohhot was below the average level of the autonomous region. In 2018, Wang Xueyan et al10 reported the current status of the prevalence of AR in six cities in Inner Mongolia region, and the prevalence rate of up to 32.4% has far exceeded the average level of the major cities in China in the previous statistics. A survey found that Risk factors related to AR include air pollutants, smoking history, antibiotic use, food allergy, drug allergy, asthma, family decoration in recent two years, etc. There are seasonal differences in the peak clinical symptoms of AR patients in Inner Mongolia, mainly from July to September. Artemisia annua, Chenopodium album and ragweed are the main pollen allergens in this area, and dust mite is the second largest allergen for AR patients in this area.11 Therefore, this study investigated the short-term effects of air pollutants and meteorological factors on allergic rhinitis by analyzing the data of atmospheric pollutants, meteorology, and allergic rhinitis outpatient clinics in Hohhot over the past 3 years, with the aim of evaluating the health effects of air pollutants and meteorological factors and providing a scientific basis for future disease prevention and control.
 |
Figure 1 Geographical location of Hohhot, Inner Mongolia. |
Materials and Methods
Source of Information
Allergic rhinitis outpatient data were obtained from the case records of daily outpatient clinics in Inner Mongolia Autonomous Region People’s Hospital during the 3-year period from January 1, 2018, to December 31, 2020, including patient number, gender, age, International Classification of Diseases code (ICD-10), and date of diagnosis. Allergic rhinitis diseases were included according to ICD-10 (J30.401); non-Hohhot household cases were excluded according to home address; cases treated for trauma, surgery, and other reasons were excluded according to disease diagnosis; repeated outpatient cases were delimited by 28 d, and events occurring after more than 28 d were recorded as another event; case data with missing information were revalidated, and those that were still unavailable after revalidation were excluded medical records; clinical information that met the study criteria was extracted according to this criterion to create an allergic rhinitis database. The air pollutant data (PM2.5, SO2, etc.) and meteorological data (temperature, humidity, barometric pressure, etc.) for the same period were obtained from the China Air Quality Online Monitoring and Analyzing Platform and the China Meteorological Science Data Sharing Service Network.
Statistical Analysis
Descriptive Analysis and Spearman Correlation Analysis
The mean, standard deviation, median, quartile, minimum and maximum values of the pollutants, meteorological factors and the number of outpatient visits for allergic rhinitis were calculated using SPSS 22.0 statistical software to get a basic idea of the situation. Since the distribution of pollutant concentration and meteorological factor information was non-normal, the correlation between each pollutant and meteorological factor was analyzed by Spearman rank correlation, and the correlation coefficient (r) was used to express the degree of correlation between the variables, and significance was tested at the test level ɑ=0.05. When r>0, it means that there is a positive correlation between the variables; when r<0, it means that there is a negative correlation; the closer the absolute value of the correlation coefficient is to 1, the stronger the correlation is.
Generalized Additive Model
Time series analysis (TSA) has been widely used in environmental epidemiology and is the most commonly used method to study the acute effects of air pollution and meteorological factors on human beings.12 Generalized Additive Models (GAM) are the most widely used time series models, which can simultaneously assess the effects of both linear and nonlinear relationships with the dependent variable. Environmental factors that have linear and nonlinear relationships with the dependent variable can be assessed simultaneously, while correcting for a variety of confounders.13 For the total population, the number of allergic rhinitis day visits is a small probability event, which can be considered to approximate a Poisson distribution. Therefore, in this study, a time series analysis of pollutants, meteorological factors, and the number of allergic rhinitis clinic visits was performed using a generalized summation model based on the Poisson distribution. Natural cubic spline (ns) was used to control for the long-term trend by treating the date, and the day of the week (dow) effect was controlled by a dummy variable. As the relationship between meteorological factors and outpatient attendance was also nonlinear, it was also controlled for with ns. The degrees of freedom of the model parameters were selected by using Akaike’s information criterion (AIC) and referring to related literature, and the smaller the value of AIC, the better the fit of the model.
The basic model is expressed as:
In our model, Yt is the actual number of AR visits on day t and εt is the expected number of AR visits on day t; β0 is the residual; βxt is a regression coefficient representing the coefficient of linear effect on the number of visits; xt is the pollutant concentration on day t; s is a spline smoothing function for the time series at t; q is a nonparametric spline smoothing function used to control for the meteorological variables (including mean temperature, relative humidity, and barometric pressure); df is the degrees of freedom of the natural spline function; and dow is a dummy variable to control for weekly effects. We consider 6–10 df as calendar time and 3–7 df as environmental factors.
Relative Risk Calculation
At the same time, the relative risk (RR) of allergic rhinitis outpatient visits due to each 10 μg/m3 increase in pollutant concentration was calculated with the formula: RR = EXP (β × 10). Since the health effects of air pollution have a certain lag, this study analyzed the single-day lag effect of air pollutants from 0 to 7 days (lag0-lag7) and the cumulative lag effect from 2–8 days (lag01-lag07). lag0 is the value of air pollutant concentration on the day of exposure, lag1 is the air pollutant concentration of the day before the exposure, and so on up to lag7. Cumulative lag is the moving average of pollutant concentrations on the day of exposure and the days before exposure, eg, lag02 represents the three-day average of air pollutant concentrations for lag0, lag1, and lag2.
Sensitivity Analysis
In addition, sensitivity analyses were conducted for the health effects of pollutant exposure to evaluate the stability of the model results by constructing a two-pollutant model in which the pollutant concentration corresponding to the optimal lag (the lag with the largest effect in a single-day lag) was used as the study variable and other pollutants with the same lag were introduced. R4.2.3 software mgcv, gam package was used for the analysis with a test level of 0.05.
Interaction
On the basis of the above studies, the effects of the combined effects of mean temperature, relative humidity and pollutants on the number of deaths from related diseases were analyzed, and three-dimensional spatial maps of the effects of the combined effects of mean temperature, relative humidity and pollutants on the number of outpatient visits for phase allergic rhinitis were fitted to give a visual picture of the effects of the combined effects of the two on the number of outpatient visits by means of the described spatial distribution characteristics.
Results
Description of the Data
Table 1 shows the basic statistics of daily outpatient visits, air pollutants and meteorological factors in Hohhot AR from 2018 to 2020. The daily average concentrations of PM2.5, PM10, SO2, NO2, CO, and O3 during the study period were 38.1 μg/m3, 83.3 μg/m3, 36.1 μg/m3, 15.1 μg/m3, 14.2 mg/m3, and 99.95 μg/m3, respectively. According to the national “Ambient Air Quality Standard (GB3095-2012)”, the limit of the secondary concentration of the daily average concentrations of PM2.5 and PM10 in Hohhot during the study period exceeded the national standard values (15 μg/m3, 45 μg/m3), and the average concentrations of SO2, NO2, CO, and O3 did not exceed the national secondary limit values. The average temperature in Hohhot during the three-year period was 7.4 °C, with a daily minimum of −21.36 °C and a daily maximum of 27.99 °C, and the relative humidity during the study period was 46.81%, with a minimum of 9.25% and a maximum of 95%. The AR clinic had a minimum of 0 and a maximum of 173 daily outpatient visits during the three-year period.
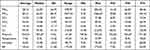 |
Table 1 Characteristics of Daily Number for Allergic Rhinitis (AR) Outpatients, Air Pollutants, and Meteorological Factors |
Time series plots of atmospheric pollutants, meteorological factors and daily AR visits showed similar trends for PM2.5, PM10, SO2, NO2 and CO, all showing the highest levels of pollution in the winter and lighter levels in the summer (Figure 2). The pollution cycle of O3 is significantly different from that of the other atmospheric pollutants, with the highest levels of pollution in the summer and lighter levels in the winter. The number of allergic rhinitis visits in July and August was higher than that of other pollutants. high in July and August, with a clear long-term and seasonal trend.
Relationship Between Air Pollution, Environmental Factors and AR Outpatients
Spearman rank correlation was used to analyze the correlation between air pollution and meteorological factors, and the results are shown in Figure 3. There was a negative correlation between O3 and other pollutants, and significant positive correlations were found among the remaining pollutants. There were significant negative correlations between temperature and PM2.5 (r= −0.39, P<0.01), PM10 (r= −0.26, P<0.01), SO2 (r= −0.55, P<0.01), and CO (r= −0.16, P<0.01), while there was a positive correlation between temperature and O3 (r=0.86, P<0.01). Relative humidity showed negative correlations with PM10 (r= −0.16, P<0.05), SO2 (r= −0.17, P<0.01) and O3 (r= −0.04, P=0.21), and negative correlations with PM2.5 (r=0.08, P<0.01), NO2 (r=0.004, P=0.90) and CO (r=0.02, P=0.37) showed positive correlations.
Short-Term Effects of Air Pollutants on Allergic Rhinitis
After adjusting for long-term trends in time, temperature, relative humidity, and weekly effects to explore the effects between air pollutants and daily outpatient visits for allergic rhinitis at different lag times are shown in Figure 4. The single-day effects of PM2.5 and PM10 both reached a maximum at exposure lag1, at which time the RR and 95% CI of the effects of pollutant concentrations on AR outpatient visits for every 10 μg/m3 of increase in pollutant concentration were 1.008 (1.001–1.016) and 1.002 (1.000–1.005), respectively. The effects of SO2 were maximized at lag5 1.072 (1.033–1.113), NO2 at lag2 1.020 (1007–1.034), CO at lag6 1.033 (1.014–1.052), and O3 reaches a maximum of 0.987 (0.980–0.994) at lag4. In the cumulative lag model, the effects of atmospheric pollutants PM2.5, PM10, SO2, NO2, and CO on AR all showed an upward trend with the accumulation of time. The cumulative effects of PM2.5, PM10, SO2, and CO all reached a maximum at lag07, when the RR and 95% CI of the effect of every 10 μg/m3 increase in pollutant concentration on the number of outpatient visits for population AR were 1.036 (1.014–1.052), 1.987 (0.9804–0.9936), respectively. were 1.036 (1.02–1.051), 1.011 (1.006–1.017), 1.199 (1.081–1.33), and 1.031 (1.004–1.058), respectively, and the cumulative effect of NO2 was maximized at lag06 1.055 (1.024–1.087), and the cumulative effect of O3 changed with time, first increasing and then decreasing. changes, increasing and then decreasing, with a maximum effect of 0.9802 (0.968–0.993) at lag05, and all the cumulative effect of air pollutants is stronger than the single-day effect.
Two-Pollutant Model
To further evaluate the robustness of the model, a dual-pollutant model was developed based on the strongest lag effect of the single-pollutant model. Considering the strong covariance between PM2.5 and PM10, PM10 was included in PM2.5, so PM10 was excluded from the dual-pollutant model for PM2.5, but PM (10–2.5) was included in the model. Specific results for AR relative risks and 95% CI based on the dual-pollutant model are given in Table 2. When PM (10–2.5), SO2, NO2, CO, and O3 were included, there was no significant change in the relative risk values for PM2.5. Similarly, after introducing other pollutants into the single pollutant model for the gaseous pollutants SO2, NO2, CO, and O3, the results show that the change in RR values remains insignificant, suggesting that the model developed is robust.
 |
Table 2 The RR of the Effects of Air Pollutants on Outpatients with Allergic Rhinitis (AR) in Two-Pollutant Model |
Interaction of Temperature and Pollutants
From the results of Spearman correlation analysis, temperature was positively correlated with AR and negatively correlated with PM2.5, PM10, SO2 and NO2. Therefore, we used the concentration of atmospheric pollutants with the strongest effect to study the interaction between atmospheric pollutants and temperature. Figure 5 shows the effect of the interaction of atmospheric pollutants and air temperature on the clinic visits of patients with allergic rhinitis. The results show that PM2.5 and PM10 peaks are similar, with peaks occurring at high-temperature-high pollutant concentration levels and low-temperature-high pollutant concentration levels. The interactions of SO2, CO, and air temperature on AR outpatient visits are unimodal, with all peaking at high-temperature-high pollutant levels. The peaks for NO2 occur at low-temperature-high pollutant levels. O3 showed high portal volumes except for high temperature-low pollutant concentration levels.
Interaction Between Relative Humidity and Pollutants
Correlation analysis showed that outpatient visits for allergic rhinitis were positively correlated with relative humidity and negatively correlated with PM10, SO2, and NO2. Figure 6 shows the effect of the interaction of atmospheric pollutants and relative humidity on outpatient visits for AR patients. At low relative humidity and high pollutant concentrations, outpatient visits were highest for PM2.5 and CO. PM10 and SO2 showed higher AR visits at high humidity-high pollutant concentrations. the highest peaks for O3 occurred at low pollutant concentrations-low humidity. and NO2 showed relatively stable outpatient visits, except for low values at low relative humidity and high pollutant concentrations.
Discussion
Hohhot is a typical northern city, belonging to a semi-arid region, with a mid-temperate continental monsoon climate, typical of the Mongolian Plateau continental climate, with obvious climatic changes in the four seasons, and a large temperature difference between the year and the day.14 Meteorological factors and pollutants show cyclical fluctuations. O3, RH, and temperature are higher in the summer and lower in the winter, and air pollutants (PM2.5, PM10, SO2, NO2, and CO) are characterized by “higher in the winter” as a result of winter heating by the residents of Hohhot, PM10, SO2, NO2 and CO) are characterized by “higher in winter and lower in summer”.
Effects of Air Pollutants on Daily AR Visits
In recent years, the prevalence of AR has increased rapidly, especially in the western and northern regions.10,15 According to domestic reports, the total prevalence rate of AR in the western China was as high as 34.31% in 2005.16 In 2009, it was found that the total average prevalence rate of AR in the northern China was 9.3%.17 Meta-analysis on the relationship between allergic rhinitis and environmental air pollutants in China showed that PM2.5, PM10, NO2 and SO2 all increased the risk of allergic rhinitis.18 We carried out a study on the influence of ambient air pollutants on the number of allergic rhinitis outpatients in Hohhot, it also found that elevated short-term exposure levels of PM2.5, PM10, SO2, NO2, and CO had a significant effect on the increase in the number of AR outpatient visits in Hohhot. A domestic study19 showed that each 10 μg/m3 increase in air pollutant concentration (1 mg/m3 for CO) caused an increase in AR clinic visits in Xinxiang of 1.036 (1.020–1.051), 1.011 (1.006–1.017), 1.199 (1.081–1.33), 1.055 (1.024–1.087), and 1.033 (1.014–1.052). Studies in Beijing and Chongqing have obtained similar results to ours.20,21 Studies in Europe and Korea have similarly shown that PM2.5, PM10, SO2, NO2, and CO exposures increase the incidence of allergic rhinitis.22,23 However, Hajat et al found that the correlation between PM2.5, PM10, and AR was not significant in London.24 This may be due to the differences in risk factors for exposures between the cities, including environmental factors (geographic location, climate type, and air quality), populations (children, adults, and elderly), and allergen exposure (timing, dose, and quantity). In-depth studies should be conducted to clarify the relationship between the specific chemical composition of particulate matter (eg, ions, dust, black carbon, heavy metals, volatile organic compounds) and the source of AR. The effect of O3 on AR is still controversial. The results of this study show that short-term exposure to O3 may be related to the reduction of outpatient visits to allergic rhinitis, which is consistent with the results of the studies conducted in London,24 and in Xinxiang19 in China. This may be related to the lower O3 concentration in Hohhot, where Bocci et al reported that the effect of ozone on specific diseases is closely related to the exposure measure, and that low-dose exposure to O3 activates the antioxidant system of the blood.25 On the other hand, it may also be related to the lifestyles of the residents, where crowds of people go out in hot and highly radiated weather to reduce their exposure to O3.
Interaction of Air Pollutants with Temperature and Humidity
Air pollution and air temperature are not isolated in the environment. In this study, it was found that the increase in PM10, NO2, and O3 concentrations under low temperatures led to varying increases in outpatient visits for AR. Relevant national studies have pointed out that physiological defenses of the upper respiratory tract decrease under low temperatures. Viral infections inhibit the activity of ciliated cells and phagocytosis of alveolar macrophages, which in turn causes the invasion of bacteria, including Streptococcus pneumoniae and Klebsiella pneumoniae.26 Meanwhile, persistent low temperatures may cause the combustion of petroleum products to release more toxic byproducts, such as NO2.27 These factors contribute to the frequency of respiratory illnesses under low-temperature conditions. In this study, it was also found that PM2.5, SO2, and CO lead to the highest number of AR clinic visits at high temperatures, and Ying Zhang et al found that increased PM2.5 concentrations at high temperatures increased the risk of respiratory illnesses.28 This may be due to the fact that sustained high temperatures promote photochemical reactions in the atmosphere, which leads to an increased production of atmospheric pollutants, such as PM2.5. Temperatures may indirectly influence respiratory disease predisposing factors such as viral and bacterial activity and outdoor survival time, leading to an increase in allergic rhinitis sufferers.29
Numerous studies have shown a significant correlation between humidity and respiratory diseases.30,31 The present study demonstrated that the effects of PM2.5, CO, and O3 were more pronounced at low humidity, and that droplet and direct contact transmission were the main modes of transmission of respiratory diseases, and that a low-temperature, dry environment provided suitable conditions for droplet-borne diseases. Studies have shown that exposure to low relative humidity leads to dehydration, decreased elasticity, and weakened cilia motility at all levels of the tracheal and bronchial mucosa, making it difficult to remove dust, bacteria, and other adherents from the airway surface. Dust and bacteria lead to the release of various inflammatory factors, increasing airway reactivity and leading to an increased risk of respiratory disease. And PM10, NO2, and SO2 have more significant effects on allergic rhinitis at high humidity, which is consistent with the findings of Wang et al.32 The effect of relative humidity on the variation of air pollution needs to be further investigated.
Our results will help to understand the effects of air pollution and meteorological factors on AR. In addition, as the average concentration of atmospheric pollutants and the incidence of allergies continue to increase globally, our findings will provide a basis for future research on the effects of increasing concentrations of atmospheric pollutants on AR and may also help to develop relevant health protection strategies. However, there are some limitations in our research. First of all, ecological bias is inevitable Research shows that keeping pets and home decoration are risk factors for allergic rhinitis,33 and regular indoor ventilation is related to the alleviation of rhinitis.34 In this study, the monitoring data of outdoor fixed locations are used as the proxy data for personal exposure to pollutants. Because individuals spend most of their time indoors, it may lead to measurement errors.35 Although the magnitude of the error is difficult to quantify, it usually results in a decrease in the risk estimate.36 This study collected data from only one hospital, and therefore the generalizability of the findings may be limited.
Conclusion
In summary, short-term exposure to PM2.5, PM10, SO2, NO2, and CO in Hohhot had a significant effect on the increase in the number of allergy outpatient visits, and O3 exposure had a significant effect on the decrease in the number of AR outpatient visits. The public should pay more attention to air pollution, and it is recommended that governmental departments rationally allocate health resources and carry out relevant health education to reduce exposure to air pollutants and decrease their health hazards to residents.
Data Sharing Statement
Data available from correspondence author on request.
Ethics Approval and Written Informed Consent
This study was conducted in accordance with the Declaration of Helsinki, and the Ethics Committee of Inner Mongolia Medical University has reviewed the proposed use of human subjects in the above-mentioned projects. It is recognized that the rights and the welfare of the subjects are adequately protected. Due to the retrospective nature of the study, the patient-level data obtained do not require the patient’s informed consent, the Ethics Committee of Inner Mongolia Medical University waived the need for informed consent. We confirmed that the data was anonymized or maintained with confidentiality. The Ethics Committee of Inner Mongolia Medical University has approved papers resulting from the project.
Acknowledgments
The authors would like to thank all the reviewers who participated in the review, as well as the Inner Mongolia People’s Hospital, the Inner Mongolia Autonomous Region Health Committee Foundation Group, and Inner Mongolia Medical University for the “Zhiyuan Talents” project.
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Funding
This study was supported by the Inner Mongolia Autonomous Region [Health Science and Technology Program] under grant [202201229] and the Inner Mongolia Medical University [“Zhiyuan Talents” project] under grant [ZY0201028].
Disclosure
The authors report no conflicts of interest in relation to this work and declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
References
1. Danesh Yazdi M, Wei Y, Di Q, et al. The effect of long-term exposure to air pollution and seasonal temperature on hospital admissions with cardiovascular and respiratory disease in the United States: a difference-in-differences analysis. Sci Total Environ. 2022;843:156855. doi:10.1016/j.scitotenv.2022.156855
2. Wang C, Feng L, Chen K. The impact of ambient particulate matter on hospital outpatient visits for respiratory and circulatory system disease in an urban Chinese population. Sci Total Environ. 2019;666:672–679. doi:10.1016/j.scitotenv.2019.02.256
3. Padula AM, Tager IB, Carmichael SL, et al. Ambient air pollution and traffic exposures and congenital heart defects in the San Joaquin Valley of California. Paediatr Perinat Epidemiol. 2013;27(4):329–339. doi:10.1111/ppe.12055
4. Agay-Shay K, Friger M, Linn S, Peled A, Amitai Y, Peretz C. Air pollution and congenital heart defects. Environ Res. 2013;124:28–34. doi:10.1016/j.envres.2013.03.005
5. Eguiluz-Gracia I, Mathioudakis AG, Bartel S, et al. The need for clean air: the way air pollution and climate change affect allergic rhinitis and asthma. Allergy. 2020;75(9):2170–2184. doi:10.1111/all.14177
6. Fuhrman C, Sarter H, Thibaudon M, et al. Short-term effect of pollen exposure on antiallergic drug consumption. Ann Allergy Asthma Immunol. 2007;99(3):225–231. doi:10.1016/s1081-1206(10
7. Kakli HA, Riley TD. Allergic Rhinitis. Prim Care. 2016;43(3):465–475. doi:10.1016/j.pop.2016.04.009
8. Chong SN, Chew FT. Epidemiology of allergic rhinitis and associated risk factors in Asia. World Allergy Organ J. 2018;11(1):17. doi:10.1186/s40413-018-0198-z
9. Wang Y, Ying Q, Hu J, Zhang H. Spatial and temporal variations of six criteria air pollutants in 31 provincial capital cities in China during 2013–2014. Environ Inter. 2014;73:413–422. doi:10.1016/j.envint.2014.08.016
10. Wang XY, Ma TT, Wang XY, et al. Prevalence of pollen-induced allergic rhinitis with high pollen exposure in grasslands of northern China. Allergy. 2018;73(6):1232–1243. doi:10.1111/all.13388
11. Liu XL. Study on the correlation between airborne allergic pollen and allergic rhinitis in Inner Mongolia. Inner Mongolia Autonomous Region, Inner Mongolia People's Hospital, July-June, 2020.
12. Bhaskaran K, Gasparrini A, Hajat S, Smeeth L, Armstrong B. Time series regression studies in environmental epidemiology. Int J Epidemiol. 2013;42(4):1187–1195. doi:10.1093/ije/dyt092
13. Zhang YQ, Zhu YH, Li CL, Feng RJ, Ma L. Realization of generalized addition model in R software. Chin Health Statist. 2015;32(06):1073–1075.
14. Gao C, Yao X, Wang X, et al. Effects of air pollutants and temperature on the number of asthma outpatient visits in Hohhot, China. Int J Environ Health Res. 2022:1–8. doi:10.1080/09603123.2022.2136364
15. Han DM, Zhang L, Huang D, et al. 11 Self-reported prevalence of allergic rhinitis in cities in China. Zhonghua Er Bi Yan Hou Tou Jing Wai Ke Za Zhi. 2007;2007:103.
16. Qian D, Hong SL, Yang YC, Huang JJ, Zou W, Zeng Q. Epidemiological sampling survey of allergic rhinitis in some parts of western China. J Third Milit Med Univer. 2008;2008:(06):539–542.
17. Wang ZH, Lin WS, Wang L. Discussion on epidemiological investigation methods of allergic rhinitis. Chin J Otolaryngol Integ Tradit Chin West Med. 2012;20(02):150–153.
18. Wang H, Li XB, Chu XJ, et al. Ambient air pollutants increase the risk of immunoglobulin E-mediated allergic diseases: a systematic review and meta-analysis. Environ Sci Pollut Res Int. 2022;29(33):49534–49552. doi:10.1007/s11356-022-20447-z
19. Wang J, Lu M, An Z, et al. Associations between air pollution and outpatient visits for allergic rhinitis in Xinxiang, China. Environ Sci Pollut Res Int. 2020;27(19):23565–23574. doi:10.1007/s11356-020-08709-0
20. Zhang F, Wang W, Lv J, Krafft T, Xu J. Time-series studies on air pollution and daily outpatient visits for allergic rhinitis in Beijing, China. Sci Total Environ. 2011;409(13):2486–2492. doi:10.1016/j.scitotenv.2011.04.007
21. Yang D, Yan Y, Pu K. The association between air pollutants and daily outpatient visits for allergic rhinitis: a time-series analysis based on distribution lag nonlinear model in Chongqing, China. Risk Manag Healthc Policy. 2022;15:1501–1515. doi:10.2147/rmhp.S373085
22. Kim SH, Lee J, Oh I, et al. Allergic rhinitis is associated with atmospheric SO2: follow-up study of children from elementary schools in Ulsan, Korea. PLoS One. 2021;16(3):e0248624. doi:10.1371/journal.pone.0248624
23. Burte E, Leynaert B, Marcon A, et al. Long-term air pollution exposure is associated with increased severity of rhinitis in 2 European cohorts. J Allergy Clin Immunol. 2020;145(3):834–842.e6. doi:10.1016/j.jaci.2019.11.040
24. Hajat S, Haines A, Atkinson RW, Bremner SA, Anderson HR, Emberlin J. Association between air pollution and daily consultations with general practitioners for allergic rhinitis in London, United Kingdom. Am J Epidemiol. 2001;153(7):704–714. doi:10.1093/aje/153.7.704
25. Bocci V, Borrelli E, Travagli V, Zanardi I. The ozone paradox: ozone is a strong oxidant as well as a medical drug. Med Res Rev. 2009;29(4):646–682. doi:10.1002/med.20150
26. Wang YP, Wang MC, Guan ZY, Tian ZC. Analysis of the relationship between seasonal changes and respiratory diseases. Jilin Meteorol. 2003;2003:(S1):13–14.
27. Duan Y, Liao Y, Li H, et al. Effect of changes in season and temperature on cardiovascular mortality associated with nitrogen dioxide air pollution in Shenzhen, China. Sci Total Environ. 2019;697:134051. doi:10.1016/j.scitotenv.2019.134051
28. Zhang Y, Xin JY, Zhang XL, et al. Interactive effect of temperature, black carbon and PM2.5 on disease death in Beijing. Chin Environ Sci. 2020;40(07):3179–3187. doi:10.19674/j.cnki.issn1000-6923.2020.0356
29. Kinney PL. Climate change, air quality, and human health. Am J Prev Med. 2008;35(5):459–467. doi:10.1016/j.amepre.2008.08.025
30. Trnjar K, Pintarić S, Mornar Jelavić M, et al. Correlation between occurrence and deterioration of respiratory diseases and air pollution within the legally permissible limits. Acta clinica Croatica. 2017;56(2):210–217. doi:10.20471/acc.2017.56.02.03
31. Lukcso D, Guidotti TL, Franklin DE, Burt A. Indoor environmental and air quality characteristics, building-related health symptoms, and worker productivity in a federal government building complex. Arch Environ Occup Health. 2016;71(2):85–101. doi:10.1080/19338244.2014.965246
32. Wang J, Zhao Z, Zhang Y, et al. Asthma, allergic rhinitis and eczema among parents of preschool children in relation to climate, and dampness and mold in dwellings in China. Environ Int. 2019;130:104910. doi:10.1016/j.envint.2019.104910
33. Li CW, Chen DD, Zhong JT, et al. Epidemiological characterization and risk factors of allergic rhinitis in the general population in Guangzhou City in China. PLoS One. 2014;9(12):e114950. doi:10.1371/journal.pone.0114950
34. Lu C, Deng Q, Li Y, Sundell J, Norbäck D. Outdoor air pollution, meteorological conditions and indoor factors in dwellings in relation to sick building syndrome (SBS) among adults in China. Sci Total Environ. 2016;560–561:186–196. doi:10.1016/j.scitotenv.2016.04.033
35. Niu Y, Chen R, Liu C, et al. The association between ambient temperature and out-of-hospital cardiac arrest in Guangzhou, China. Sci Total Environ. 2016;572:114–118. doi:10.1016/j.scitotenv.2016.07.205
36. Zeger SL, Thomas D, Dominici F, et al. Exposure measurement error in time-series studies of air pollution: concepts and consequences. Environ Health Perspect. 2000;108(5):419–426. doi:10.1289/ehp.00108419
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.