Back to Journals » Breast Cancer: Targets and Therapy » Volume 15
Early Real-World Treatment Patterns and Clinical Outcomes in Patients with Metastatic Breast Cancer Treated with Eribulin After Prior Immuno-Oncology or Antibody–Drug Conjugate Therapy
Authors Goyal RK , Zhang J, Davis KL, Sluga-O'Callaghan M, Kaufman PA
Received 7 June 2023
Accepted for publication 16 October 2023
Published 17 November 2023 Volume 2023:15 Pages 855—865
DOI https://doi.org/10.2147/BCTT.S422025
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 4
Editor who approved publication: Dr Pooja Advani
Ravi K Goyal,1 Jingchuan Zhang,2 Keith L Davis,1 Martina Sluga-O’Callaghan,1 Peter A Kaufman3
1Health Economics, RTI Health Solutions, Research Triangle Park, NC, USA; 2Eisai Inc., Nutley, NJ, USA; 3Larner College of Medicine, Division of Hematology/Oncology, University of Vermont Cancer Center, Burlington, VT, USA
Correspondence: Peter A Kaufman, Larner College of Medicine, Division of Hematology/Oncology, University of Vermont Cancer Center, 111 Colchester Avenue, EP2, Burlington, VT, 05401, USA, Email [email protected]
Introduction: Eribulin was approved by the FDA in 2010 for the treatment of metastatic breast cancer (MBC) in the United States (US). More recently, several immuno-oncology (IO) and antibody–drug conjugate (ADC) regimens have been approved for MBC. We assessed the treatment patterns and clinical outcomes in MBC patients treated with eribulin following treatment with an IO or ADC in US clinical practice.
Materials and Methods: In a retrospective patient medical chart review study, patients with MBC, aged ≥ 18 years, who initiated eribulin therapy between March 1, 2019, and September 30, 2020, treated with either prior IO or ADC in the metastatic setting were included. Patient demographics, treatment characteristics, and clinical outcomes were analyzed descriptively. Real-world progression-free survival (rwPFS) and overall survival (OS) were estimated using Kaplan–Meier analyses.
Results: In the study population (N=143), median age at eribulin initiation was 62 years; 64% were Caucasian, and 67% had triple-negative MBC (TNBC). Eribulin therapy was used in the second to fifth line of therapy in the metastatic setting; median treatment duration was 7.2 months. The overall response rate for eribulin was 59.4%. Median rwPFS and OS from eribulin initiation were 21.4 months (95% CI, 12.9-not estimable [NE]) and 24.2 months (95% CI, 17.5-NE), respectively. In patients with TNBC, median rwPFS and OS from eribulin initiation were 12.0 months (95% CI, 8.8-NE) and 18.3 months (95% CI, 14.9-NE), respectively.
Conclusion: These real-world data provide evidence for the clinical effectiveness outcomes of eribulin treatment among MBC patients previously treated with an IO or ADC.
Keywords: real world evidence, metastatic breast cancer, immuno-oncology, antibody drug conjugates, eribulin, patient medical chart review
Introduction
Nearly 300,000 women in the United States (US) will be diagnosed with breast cancer in 2022, with an estimated 43,250 deaths.1 Approximately 6% of newly diagnosed breast cancer patients are reported to be de novo metastatic (stage IV disease) at the time of diagnosis, among whom the 5-year survival rate was 29%.1 In addition, approximately 20−30% of patients with initial early-stage disease eventually develop metastatic disease.2–4 The goals for treatment of patients diagnosed with metastatic breast cancer (MBC) are to relieve symptoms, slow disease progression, and prolong life. Consistent with the National Comprehensive Cancer Network (NCCN) guidelines, it is widely accepted to assess all patients for hormone receptor (HR) and human epidermal growth factor receptor 2 (HER2) status, as treatment decisions and outcomes vary substantially based on HR and HER2 status.5 Triple-negative breast cancer (TNBC) continues to be a particularly challenging subtype of breast cancer with a poor prognosis and accounts for roughly 10–14% of all breast cancer cases, but approximately 30% of cases of MBC.1,6,7
Eribulin mesylate (eribulin) was approved by the US Food and Drug Administration (FDA) in 2010 for treatment of patients with MBC who have received at least 2 prior chemotherapy regimens for metastatic disease, including an anthracycline and a taxane in either the metastatic or adjuvant setting. This approval was based on findings from the Phase 3 EMBRACE trial (NCT00388726) in which eribulin significantly improved overall survival (OS) by 2.5 months in women who had received 2 to 5 prior lines of chemotherapy in the metastatic setting over treatment of physician’s choice.8 In another phase 3 study (NCT00337103), eribulin-treated patients did not have a significant improvement in OS as compared to patients treated with capecitabine in the first, second, or third line of chemotherapy in the metastatic setting, although a numerical trend favoring eribulin was demonstrated.9 Interestingly, in a subsequent pooled analysis of both of these trials, eribulin was seen to have a significant improvement in OS, as compared to the control arm. Further, upon subgroup analysis, patients with TNBC were seen to be a subgroup of patients with MBC with the greatest benefit from eribulin.10 In addition to these and other clinical trial data, real-world studies support the safety and effectiveness of eribulin in MBC overall and in subgroups by receptor status.11,12
In recent years, clinical studies and subsequent approvals of a number of targeted therapeutics, such as immuno-oncology (IO) and antibody–drug conjugate (ADC) therapies, have rapidly shifted the treatment landscape for MBC. Antibody-based IOs targeting immune checkpoints like programmed cell death protein 1 (PD-1) and programmed death-ligand 1 (PD-L1) have become a powerful tool for treating certain subsets of MBC by interrupting pathways that block the immune system from recognizing cancer cells.13 In March 2019, atezolizumab was granted accelerated approval by the FDA and became the first checkpoint inhibitor IO approved for TNBC when used in combination with paclitaxel protein-bound.14,15 In addition, sacituzumab govitecan, an ADC that targets trophoblast cell surface antigen 2 (Trop-2), a biomarker expressed on approximately 85% of breast cancers,16 was approved in April 2020 for metastatic TNBC.17 The targeted approach of both IO and ADC therapies makes them potent anticancer treatments; however, essentially all patients with MBC will eventually develop progressive disease on IO or ADCs, and there remains a critically important need for additional treatment regimens.13,18,19 With the evolving therapeutic landscape and increased use of these and other IOs and ADCs in the clinic today, there is limited evidence and understanding of the real-world treatment patterns and clinical outcomes of patients with MBC treated with eribulin who were previously exposed to either an IO or ADC. In order to fill this gap, our study aimed to assess treatment patterns and clinical outcomes in patients with MBC treated with eribulin following either IO or ADC therapy in routine clinical practice in the US.
Materials and Methods
Study Design
A noninterventional, retrospective, patient medical chart review was performed. Oncologists consenting to participate in the study were recruited from academic and community practices across all regions of the US and provided data from the records of eligible patients diagnosed with MBC. Deidentified data were collected via a secure electronic data collection form. Participating physicians were oncologists who had treated at least 2 MBC patients with eribulin after prior atezolizumab or sacituzumab govitecan since 2019 and were responsible for treatment decisions regarding these patients. Patients eligible for this study were female; were aged 18 years or older; had a histologically confirmed diagnosis of MBC; initiated treatment with eribulin between March 1, 2019, and September 30, 2020; and before initiating eribulin, had received atezolizumab or sacituzumab govitecan in either clinical practice or in a clinical trial setting. Patients who received eribulin as part of clinical trials or with other malignant neoplasms (except nonmelanoma skin cancer and early-stage breast cancer) prior to diagnosis of MBC were not eligible. The RTI Institutional Review Board (IRB) waived full IRB review or informed consent from patients because of the use of deidentified patient data.
Study Measures and Outcomes
Data on patient demographics, clinical characteristics, and eribulin treatment characteristics were collected from patient medical records. For the purposes of this study, lines of therapy were counted from diagnosis with metastatic disease, not from diagnosis with early-stage breast cancer. Therefore, some patients may have received treatment prior to the first line used in this study. Systemic therapies that were considered in defining a line of therapy included the following as mono- or combination therapies: chemotherapies, CDK4/6 inhibitors, hormonal therapies, HER2-targeted therapies, immunotherapies, ADC, phosphoinositide 3-kinase (PI3K) inhibitor, Poly(ADP-ribose) polymerase (PARP) inhibitors, angiogenesis inhibitor, mammalian target of rapamycin (mTOR) inhibitor, and tyrosine kinase inhibitors.
Clinical outcomes have been assessed since the initiation of eribulin treatment. The real-world best overall response was abstracted as recorded by the physician in the patient’s medical chart at the time of assessment and categorized as complete response (CR), partial response (PR), stable disease, or progressive disease. Real-world progression-free survival (rwPFS) was calculated from the date of eribulin initiation to the earliest date of physician-documented progression or death due to any cause while on eribulin treatment or within 90 days after eribulin treatment discontinuation but before the subsequent treatment was initiated; patients with no documented progression or death event were censored at the earliest of (1) 90 days after eribulin treatment discontinuation, (2) start of the next line of therapy, or (3) the last available follow-up in the medical record. The 90-day window following treatment discontinuation was used in consideration that any progression event shortly after discontinuation could be reasonably attributable to that treatment, in the absence of any subsequent therapy line. Overall survival was calculated from the date of eribulin initiation to death due to any cause; patients with no death event were censored at the last available follow-up in the medical record.
Statistical Analyses
All analyses were conducted using SAS Studio (SAS Institute, Inc.; 2011). Descriptive statistics (mean, median, interquartile range, and standard deviation [SD]) were reported for continuous variables. Categorical variables were described as counts and frequencies. Time-to-event variables such as time to treatment discontinuation, rwPFS, and OS were assessed using Kaplan–Meier methods. All study measures and clinical outcomes were analyzed among the total sample (post-IO and post-ADC eribulin-treated patients) and separately among the subgroups of (1) patients treated with eribulin post ADC (sacituzumab govitecan) and (2) TNBC patients.
Results
Physician Characteristics
A total of 53 physicians consented to participate in this study. Physicians practiced in the community setting (57%) as well as in the academic setting (42%). These physicians had a median of 16 years in practice, and on average, physicians spent approximately 91% of their time in direct patient care. Practices were located throughout the US (20.8% in the Northeast, 34% in the South, 18.9% in the Midwest, and 26.4% in the West) and were primarily in urban (64.2%) or suburban (34.0%) settings.
Patient Characteristics
Of the 143 patients with MBC included in our study, over two-thirds (n=96, 67.1%) had TNBC, 21.0% had HR+/HER2- tumors, and 8.4% had HER2+ tumors. The median age of patients at eribulin initiation was 62 years. The majority were Caucasian (63.6%) and non-Hispanic (80.4%) in the overall cohort, while the TNBC subgroup had a slightly higher proportion of African American patients than the overall study cohort (30.2% vs 25.2%). Based on the available medical history data, any early-stage breast cancer diagnosis prior to MBC was reported for 11.2% of patients. The most commonly reported comorbidities were hypertension (41.3%), depression (18.2%), diabetes (16.1%), and chronic pulmonary disease (11.2%). At eribulin initiation, the majority of patients (86.8%) had Eastern Cooperative Oncology Group (ECOG) scores of 0–2. The inclusion criteria required all patients to have metastatic disease diagnoses, with lymph nodes (51.8%), bone (42.7%), lung (42.0%), and liver (30.8%) being the most common sites. Full demographic and clinical characteristics are summarized in Table 1.
 |
Table 1 Demographic and Clinical Characteristics |
Treatment Patterns
In the overall study population, 62 patients (43.4%) received eribulin following prior atezolizumab (IO) and 84 (58.7%) received it following prior sacituzumab govitecan (ADC); 3 patients were treated with both regimens before initiating eribulin. Median time to initiation of first systemic therapy line after an MBC diagnosis was 0.4 months (Table 1). Eribulin use was reported to be in the second line (70.6%), third line (16.8%) and fourth or later lines (12.6%) in the metastatic setting (Table 2). A slightly higher proportion of patients used eribulin in later lines in the TNBC subgroup (59.4% in the second line, 22.9% in the third line, and 17.7% in the fourth line or later) and in the post–sacituzumab govitecan subgroup (63.1% in the second line, 17.9% in the third line, and 19.1% in the fourth line). Among all patients, 49% of patients did not receive any prior chemotherapy in the metastatic setting, 35.0% received 1 prior line of chemotherapy, and 16.1% received at least 2 lines of chemotherapy. The distribution for no prior chemotherapy, one line, and at least two lines of chemotherapy was 26.0%, 50.0%, and 24.0%, respectively, for the TNBC subgroup and 58.3%, 23.8%, and 17.9%, respectively, for the post–sacituzumab govitecan subgroup (Table 1). In the overall patient cohort, 44.1% received a prior taxane and 11.2% received a prior anthracycline before eribulin treatment.
 |
Table 2 Eribulin Treatment Characteristics |
At last follow-up, eribulin treatment was ongoing for 28.7% of all patients (Table 2). During the median follow-up of 12.1 months, the median eribulin treatment duration was 5.8 months among those who had discontinued eribulin and 12.5 months among those who were still on treatment in the overall population. The Kaplan–Meier estimate of median time to discontinuation was 7.3 months (95% confidence interval [CI], 6.3–8.5). Among the 71.3% of patients who discontinued eribulin, the most common reasons for discontinuation were progressive disease (43.1%), patient decision (27.5%), and completion of planned treatment course (25.5%).
Clinical Outcomes
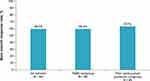
According to physician-reported treatment response taken from patient medical charts, over half of the patients (59.4%) achieved a best response of either a CR or a PR with eribulin treatment (Figure 1); in addition, 25.9% had stable disease and 8.4% had progressive disease. For patients with TNBC, 59.4% achieved a best response of a CR or a PR (Figure 1). In the post–sacituzumab govitecan subgroup, 63.1% of patients were reported with best response as a CR or a PR (Figure 1).
From the date when eribulin therapy was initiated, 35.0% of patients in the overall population experienced a progression or death event (Table 3). The median rwPFS was 21.4 months (95% CI, 12.9-not estimable [NE]) for the overall population, 12.0 months (95% CI, 8.8-NE) for the TNBC subgroup, and 12.9 months (95% CI, 8.8-NE) for the post–sacituzumab govitecan subgroup. The estimated rwPFS rates at 12 months were 61.7% (95% CI, 51.5–70.3%) in the overall cohort, 49.1% (95% CI, 35.0–61.7%) in the TNBC subgroup, and 52.3% (95% CI, 38.7–64.2%) for post–sacituzumab govitecan subgroup (Table 3 and Figure 2). Among patients who received eribulin in the second line, median rwPFS was 21.4 months in the TNBC subgroup and was not reached in the overall population and the post–sacituzumab govitecan subgroup. Among patients who received eribulin in the third line and later, median rwPFS was 6.7 months for all patient cohorts. The 12-month rwPFS rates according to the line of therapy in which eribulin was initiated were, for the overall population, 78.4% (95% CI, 66.6–86.4%) in the second line and 24.6% (95% CI, 11.3–40.5%) in the third line or later; for the TNBC subgroup, 70.6% (95% CI, 48.6–84.5%) in the second line and 22.2% (95% CI, 9.1–38.7%) in the third line or later; and for the post–sacituzumab govitecan subgroup, 74.7% (95% CI, 55.9–86.3%) in the second line and 18.4% (95% CI, 5.7–36.6%) in the third line or later.
 |
Table 3 Real-World Progression-Free Survival and Overall Survival Following Initiation of Eribulin Therapy |
The median OS from the date of initiation of eribulin was 24.2 months (95% CI, 17.5-NE) for the overall cohort, 18.3 months (95% CI, 14.9-NE) for TNBC subgroup, and 24.2 months (95% CI, 15.7-NE) for the post–sacituzumab govitecan subgroup. The estimated OS rates at 12 and 24 months were 74.6% (95% CI, 66.1–81.2%) and 54.1% (95% CI, 41.1–65.4%), respectively, for the overall cohort; 68.9% (95% CI, 58.0–77.5%) and 41.5% (95% CI, 25.5–56.8%), respectively, for the TNBC subgroup; and 73.9% (95% CI, 62.5–82.3%) and 50.8% (95% CI, 34.6–64.9%), respectively, for the post–sacituzumab govitecan subgroup (Table 3 and Figure 3). Among patients who received eribulin in the second line, median OS was not reached for all patient cohorts. Among patients who received eribulin in the third line or later, the median OS was 10.9 months for all patient cohorts. The 24-month OS rates according to the line of therapy in which eribulin was initiated were, for the overall population, 76.6% (95% CI, 63.1–85.7%) in the second line and 18.5% (95% CI, 6.2–36.1%) in the third line or later; for the TNBC subgroup, 68.6% (95% CI, 47.1–82.8%) in the second line and 19.1% (95% CI, 6.3–37.1%) in the third line or later; and for the post–sacituzumab govitecan subgroup, 76.6% (95% CI, 57.2–88.1%) in the second line and 21.9% (95% CI, 7.5–41.0%) in the third line or later.
 |
Figure 3 Overall Survival on Eribulin Following Immuno-Oncology or Antibody–Drug Conjugate Therapy. Abbreviations: NE, not estimable; OS, overall survival; TNBC, triple-negative breast cancer. |
Discussion
This real-world study provides data on treatment characteristics and clinical outcomes among MBC patients undergoing therapy with eribulin who had been previously treated with an IO or ADC (specifically atezolizumab or sacituzumab govitecan). Patients in our study cohort were from all geographic regions of the US and were distributed across races and ethnicities. Patients started eribulin treatment at a median age of 62 years. Over two-thirds of our study cohort had TNBC, which is expected considering this was the indicated patient population for atezolizumab and sacituzumab govitecan. Patients were estimated to be on eribulin treatment for a median of 7.3 months.
In our real-world study of patients with MBC who initiated eribulin following an IO or ADC, nearly 60% achieved a best response with a complete or partial response with eribulin, and more than half were estimated to be alive after 2 years (median OS, 24.2 months). In the EMBRACE clinical trial, patients treated with eribulin showed a median OS of 13.1 months (compared with 10.6 months in patients treated with physicians’ choice of therapy). The median OS from eribulin found in a clinical trial comparing eribulin and capecitabine was 15.9 months, numerically similar to the EMBRACE trial. The longer observed median OS in this current study may be related to the line of therapy in which patients received eribulin; in the current study, eribulin was most commonly given as a second-line treatment, whereas in the eribulin versus capecitabine trial, eribulin was primarily given as a third-line treatment,9 and EMBRACE trial patients most commonly received eribulin in the fourth or fifth line.8 A recently published real-world study examining clinical outcomes among patients with advanced or metastatic breast cancer treated with eribulin primarily in the third line following chemotherapy or hormone therapy found shorter OS (median 8.3 months) compared to that observed in our study, wherein most patients received eribulin in the second line following IO and had a median survival of 24.2 months.20 Later line outcomes in our study (third line or later) are also consistent with real-world analyses performed in a study of Chinese patients.21
Additionally, the survival of the MBC population has generally improved over the last 2 decades.22 For patients in the TNBC and post–sacituzumab govitecan subgroups, the median OS was over 18 and 24 months, respectively. Consistent with clinical trial data and other studies, our analyses showed that rwPFS and OS rates were considerably lower in patients initiating eribulin in the third or later lines as compared with the second line, while impacts by the TNBC tumor type or by prior IO or ADC exposure were minimal. However, these differences may be explained, at least partially, by prognostic differences between the groups. Our analysis also showed that the difference between median rwPFS (21.4 months) and median OS (24.2 months) was small; however, as noted in the methods, our definition for rwPFS incorporated a 90-day allowance to observe progression or death event after treatment discontinuation, which may partly explain a smaller than expected difference between these two estimates.
Our study provides up-to-date real-world results on the effectiveness of eribulin among patients who were previously treated with recently approved treatment options, likely capturing the shifting landscape of treatment for MBC. In addition, the inclusion of patients regardless of baseline characteristics from community and academic practices in all geographic regions of the US resulted in a diverse patient population more representative of the overall MBC patient population who received eribulin following IO or ADC. A significant proportion of the patients in our study may be underrepresented in clinical trials: 25.2% were African American patients and 25.7% had an ECOG performance status of 2 or greater. This potentially supports the generalizability of the effectiveness of eribulin in a broader real-world patient population.
Although this study involved rigorous analyses of real-world data of eribulin use following prior IO or ADC, there are limitations that should be considered. ADC and IOs were only recently approved in the US, and our results were limited to early observations in clinical practice. Furthermore, data were gathered from participating physicians, which may result in some selection bias. Patients may have been lost to follow-up if transferred to other providers or treatment centers. The treatment patterns reflected in the study represent only the practices of oncologists who agreed to participate in the study and the patients selected for inclusion, which may vary from other physicians and practices. Finally, as in all real-world analyses, our findings are limited by the completeness and accuracy of the data captured by participating oncologists in real-world clinical practice.
Because atezolizumab and sacituzumab govitecan were approved for MBC in 2019 and 2020, respectively, the data collected in this study captured only early adopters of IO and ADC for MBC, some of which may have been “off-label.” It is important to note that in August 2021, atezolizumab’s accelerated approval status for TNBC was voluntarily withdrawn in the US by the manufacturer. As this happened during the data collection period of our study, no amendment was made. The IO therapy pembrolizumab in combination with chemotherapy was approved in November 2020 by the FDA for patients with locally recurrent unresectable or metastatic TNBC whose tumors express PD-L1.23 As our study required that all patients had initiated treatment with eribulin between March 1, 2019, and September 30, 2020, after IO or ADC, pembrolizumab was not considered as a prior IO in our study. Future studies with longer follow-up and updated lists of IOs and ADCs would be valuable for evaluating mature treatment patterns of eribulin in patients previously treated with an IO or ADC. Furthermore, future studies examining the impact of individualized patient profiles on their outcomes following treatment with eribulin post IO or ADC therapy would be beneficial to our ability to tailor treatments by predicting the most beneficial therapeutic agents.
Conclusion
This real-world study provides data on eribulin treatment patterns and clinical outcomes among patients with MBC previously treated with an IO or ADC. Among patients with MBC who initiated eribulin following an IO or ADC, the median rwPFS was 21.4 months, and more than 50% were estimated to be alive after 2 years. Within the TNBC subpopulation, the rwPFS was 12.0 months. The median overall survival was 24.2 months among all patients, 18.3 months for patients with TNBC, and 24.2 months for patients treated with sacituzumab govitecan. Our study findings suggest that eribulin may be a potential treatment option for patients who failed IO or ADC in a prior therapy line for MBC.
Data Sharing Statement
The data for this study will not be available.
Ethical Approval
The RTI Institutional Review Board (IRB) waived full IRB review or informed consent from patients because of the use of deidentified patient data.
Acknowledgments
The authors thank Sara Musetti Jenkins, PhD, and Brian Samsell, PhD, of RTI Health Solutions for medical writing assistance.
An abstract from this study was presented at the Miami Breast Cancer Conference as a poster presentation with interim findings. The poster’s abstract was published in “Poster Abstracts” in 39th Annual Miami Breast Cancer Conference Abstracts, Volume 36, Issue suppl 3, Page 13; https://www.cancernetwork.com/view/real-world-treatment-patterns-and-clinical-outcomes-in-patients-treated-with-eribulin-after-prior-immunotherapy-io-or-antibody-drug-conjugate-adc-for-metastatic-breast-cancer.
Funding
Eisai Inc. provided financial support for the study. RTI Health Solutions, an independent nonprofit research organization, received funding under a research contract with Eisai Inc. to conduct this study and provide publication support in the form of manuscript writing, styling, and submission.
Disclosure
RKG, KLD, and MSO are full-time employees of RTI Health Solutions, an independent nonprofit research organization, which was retained by Eisai Inc. to conduct the research, which is the subject of this manuscript. Their compensation is unconnected to the studies on which they work. JZ is an employee of Eisai Inc. PAK received research support and/or served as a consultant/advisor for the following: Eisai, Inc., Roche/Genentech Amgen, Novartis, Macrogenics, Polyphor, Lilly, Pfizer, Sanofi, Seagen, Bristol-Myer Squibb, H3 BioMedicine, Zymeworks Therapeutics, and AstraZeneca. The authors report no other conflicts of interest in this work.
References
1. National Cancer Institute. Surveillance, Epidemiology, and End Results (SEER) Program. Cancer stat facts: female breast cancer; 2022. Available from: https://seer.cancer.gov/statfacts/html/breast.html.
2. Berman AT, Thukral AD, Hwang WT, Solin LJ, Vapiwala N. Incidence and patterns of distant metastases for patients with early-stage breast cancer after breast conservation treatment. Clin Breast Cancer. 2013;13(2):88–94. doi:10.1016/j.clbc.2012.11.001
3. Santiago RJ, Wu L, Harris E, et al. Fifteen-year results of breast-conserving surgery and definitive irradiation for Stage I and II breast carcinoma: the University of Pennsylvania experience. Int J Radiat Oncol Biol Phy. 2004;58(1):233–240. doi:10.1016/S0360-3016(03)01460-3
4. Early Breast Cancer Trialists’ Collaborative Group. Effects of chemotherapy and hormonal therapy for early breast cancer on recurrence and 15-year survival: an overview of the randomised trials. Lancet. 2005;365(9472):1687–1717. doi:10.1016/S0140-6736(05)66544-0
5. Bevers TB, Helvie M, Bonaccio E, et al. breast cancer screening and diagnosis, version 3.2018, NCCN clinical practice guidelines in oncology. J Natl Compr Canc Netw. 2018;16(11):1362–1389. doi:10.6004/jnccn.2018.0083
6. Kim H, Lee H, Choi DH, et al. Distribution of tumor subtypes in bilateral breast cancer: comparison between synchronous and metachronous cancer. Asia Pac J Clin Oncol. 2022;18(1):28–34. doi:10.1111/ajco.13444
7. Li X, Yang J, Peng L, et al. Triple-negative breast cancer has worse overall survival and cause-specific survival than non-triple-negative breast cancer. Breast Cancer Res Treat. 2017;161(2):279–287. doi:10.1007/s10549-016-4059-6
8. Cortes J, O’Shaughnessy J, Loesch D, et al. Eribulin monotherapy versus treatment of physician’s choice in patients with metastatic breast cancer (EMBRACE): a phase 3 open-label randomised study. Lancet. 2011;377(9769):914–923. doi:10.1016/S0140-6736(11)60070-6
9. Kaufman PA, Awada A, Twelves C, et al. Phase III open-label randomized study of eribulin mesylate versus capecitabine in patients with locally advanced or metastatic breast cancer previously treated with an anthracycline and a taxane. J Clin Oncol. 2015;33(6):594–601. doi:10.1200/JCO.2013.52.4892
10. Twelves C, Cortes J, Vahdat L, et al. Efficacy of eribulin in women with metastatic breast cancer: a pooled analysis of two phase 3 studies. Breast Cancer Res Treat. 2014;148(3):553–561. doi:10.1007/s10549-014-3144-y
11. Mougalian SS, Kish JK, Zhang J, Liassou D, Feinberg BA. Effectiveness of eribulin in metastatic breast cancer: 10 years of real-world clinical experience in the United States. Adv Ther. 2021;38(5):2213–2225. doi:10.1007/s12325-020-01613-6
12. Kazmi S, Chatterjee D, Raju D, Hauser R, Kaufman PA. Overall survival analysis in patients with metastatic breast cancer and liver or lung metastases treated with eribulin, gemcitabine, or capecitabine. Breast Cancer Res Treat. 2020;184(2):559–565. doi:10.1007/s10549-020-05867-0
13. Zou Y, Zou X, Zheng S, et al. Efficacy and predictive factors of immune checkpoint inhibitors in metastatic breast cancer: a systematic review and meta-analysis. Ther Adv Med Oncol. 2020;12:1758835920940928. doi:10.1177/1758835920940928
14. Reddy SM, Carroll E, Nanda R. Atezolizumab for the treatment of breast cancer. Expert Rev Anticancer Ther. 2020;20(3):151–158. doi:10.1080/14737140.2020.1732211
15. US Food and Drug Administration. Highlights of prescribing information: TECENTRIQ (Atezolizumab); 2020. Available from: https://www.accessdata.fda.gov/drugsatfda_docs/label/2021/761034s033s034s035s036s037s038lbl.pdf.
16. Spring LM, Nakajima E, Hutchinson J, et al. Sacituzumab govitecan for metastatic triple-negative breast cancer: clinical overview and management of potential toxicities. Oncologist. 2021;26(10):827–834. doi:10.1002/onco.13878
17. US Food and Drug Administration. Highlights of prescribing information: TRODELVY (sacituzumab govitecan-hziy); 2020. Available from: https://www.accessdata.fda.gov/drugsatfda_docs/label/2022/761115s023lbl.pdf.
18. Gaynor N, Crown J, Collins DM. Immune checkpoint inhibitors: key trials and an emerging role in breast cancer. Semin Cancer Biol. 2022;79:44–57. doi:10.1016/j.semcancer.2020.06.016
19. US Food and Drug Administration. Highlights of prescribing information: HERCEPTIN (trastuzumab); 2018. Available from: https://www.accessdata.fda.gov/drugsatfda_docs/label/2018/103792s5345lbl.pdf#:~:text=HIGHLIGHTS%20OF%20PRESCRIBING%20INFORMATION%20Initial%20dose%20of%204,paclitaxel%20or%20docetaxel%29%20or%2018%20weeks%20%28with%20docetaxel%2Fcarboplatin%29.
20. Kenny L, Beresford M, Brown I, Misra V, Kristeleit H. Eribulin for the treatment of advanced breast cancer: a prospective observational registry study. Eur J Cancer Care. 2022;31(6):e13747. doi:10.1111/ecc.13747
21. Gui X, Liang X, Li H. Effectiveness, safety, and impact on quality of life of eribulin-based therapy in heavily pretreated patients with metastatic breast cancer: a real-world analysis. Cancer Med. 2023;12:16793–16804. doi:10.1002/cam4.6301
22. Caswell-Jin JL, Plevritis SK, Tian L, et al. Change in survival in metastatic breast cancer with treatment advances: meta-analysis and systematic review. JNCI Cancer Spectr. 2018;2(4):ky062. doi:10.1093/jncics/pky062
23. US Food and Drug Administration. Highlights of Prescribing Information: KEYTRUDA (pembrolizumab); 2022. Available from: https://www.accessdata.fda.gov/drugsatfda_docs/label/2021/125514s112lbl.pdf.
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.