Back to Journals » Psoriasis: Targets and Therapy » Volume 12
Dimethyl Fumarate as Therapeutic Alternative in Moderate-to-Severe Psoriasis: Our Experience
Authors Rosés Gibert P, de la Torre Gomar FJ, Saenz Aguirre A, Gimeno Castillo J , González Pérez R
Received 22 March 2022
Accepted for publication 14 June 2022
Published 29 June 2022 Volume 2022:12 Pages 177—185
DOI https://doi.org/10.2147/PTT.S367060
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Prof. Dr. Uwe Wollina
Pau Rosés Gibert, Francisco Javier de la Torre Gomar, Amaia Saenz Aguirre, Javier Gimeno Castillo, Ricardo González Pérez
Dermatology Department, Araba University Hospital, Vitoria-Gasteiz, Spain
Correspondence: Pau Rosés Gibert, Araba University Hospital, Jose Atxotegi Kalea, s/n, Vitoria-Gasteiz, Araba, 01009, Spain, Email [email protected]
Purpose: Dimethyl fumarate (DMF) is an oral formulation approved for the treatment of moderate-to-severe psoriasis in adult patients requiring systemic therapy. Here, we describe our clinical experience with DMF for moderate-to-severe psoriasis in Spain.
Patients and Methods: This is a retrospective study including 30 adult patients with moderate-to-severe psoriasis under treatment with DMF between September 2018 and January 2020. Patients were treated with DMF as per its Summary of Product Characteristics and the median duration of treatment was 15 weeks (4– 55 weeks). Psoriasis Area and Severity Index (PASI) and body surface area (BSA) severity scales were evaluated from baseline to week 36 and adverse events (AEs) developed during treatment were described.
Results: The efficacy of DMF was assessed at week 8 and at week 36 (n = 5), both PASI and BSA were 0. At week 24, median PASI showed a decrease in both the last observation carried forward (LOCF; n = 23) and the observed cases (OC) (n = 10): from 10 to 6 and from 10 to 1.5, respectively. Median BSA also showed a decrease from 19 to 10 in LOCF and from 17 to 3 in OC. The most frequent AEs were diarrhoea (40.0%), flushing (13.3%) and lymphopenia (3.3%). In 47.1% patients, AEs have been solved by adjusting the DMF dose. Treatment discontinuation rate due to AEs was 43.3%.
Conclusion: Our clinical experience indicates that DMF could be an effective and safe treatment for moderate-to-severe psoriasis in adult patients.
Keywords: dimethyl fumarate, moderate-to-severe psoriasis, clinical experience, retrospective study
Introduction
Psoriasis is the most frequent chronic immune-mediated inflammatory skin disease with an estimated prevalence of 2–4% in Europe.1,2 Psoriasis is a multifactorial disorder, influenced by genetic, environmental, and immunological factors.3–5 One-third of patients have a moderate-to-severe form of the disease, and chronic plaque psoriasis represents the most common type of psoriasis affecting approximately 90% of patients.5–7 Plaque psoriasis is associated with psychological, cardiovascular, metabolic, and arthritic comorbidities,6,8 and causes discomfort, pain, and itching affecting the quality of life.3 The available treatments for moderate-to-severe psoriasis include both biological and non-biological systemic treatments.6,7,9,10
The European S3-Guideline on the systemic treatment of Psoriasis vulgaris11 recommended the use of systemic treatment for induction and long-term treatment of psoriasis.1 To assess the impact of psoriasis, an established parameter to measure the severity of skin symptoms is the Psoriasis Area and Severity Index (PASI). Additional tools include the body surface area (BSA) and the Physician Global Assessment (PGA).1 According to the European S3-Guideline, a moderate-to-severe disease is defined as PASI >10.11
Fumaric acid esters (FAEs), small molecules with anti-inflammatory and immune-modulatory effects, have been extensively used in Germany since 1959.1,6,7 The mixture of a FAE, dimethyl fumarate (DMF), together with calcium, magnesium, and salts of monoethyl fumarate was officially registered in 1994 by the German Drug Administration and, since then, became the most frequently used systemic therapy for psoriasis.1,6 DMF alone, as an oral formulation, has been approved by the European Medicines Agency (EMA) to treat moderate-to-severe plaque psoriasis among adult patients requiring systemic therapy in 2017.1,3,12 Treatment with DMF was shown to be safe, with mild treatment-emergent adverse events (AE) occurrence and severity,6 and to be effective in certain localizations such as the scalp, nails, or palmoplantar region.7 Although clinical trials indicated that DMF was effective, safe, and comparable to the FAE mixture in treating adults with moderate-to-severe plaque psoriasis,6,7 limited data on its safety and efficacy are available in clinical practice, with the exception of Germany and a few other European countries.7,13–16
The selection of systemic therapy for psoriasis should be based on individual factors, such as the patient’s age and sex, the existence of comorbidities, and co-medication, among others,1 since the response to treatment varies according to the patient’s characteristics and drug-specific side effects.6 Hence, clinical experience is needed to guide clinical practice. In this study, we describe our clinical experience in treating moderate-to-severe psoriasis with DMF in Spain, a country with little therapeutic experience with FAEs.
Materials and Methods
Study Design
A total of 30 adult patients with moderate-to-severe psoriasis (PASI ≥10; BSA affected ≥10%) under treatment with DMF between September 2018 and January 2020 in one Spanish center were included in this retrospective study. All patients signed the informed consent form. This study was conducted according to the Declaration of Helsinki principles and approved by the Ethics Committee of the University Hospital of Araba.
Treatment
Patients, who met criteria for systemic treatment, have been treated with DMF by up-titrating the dose during the first nine weeks of treatment, according to the Summary of Product Characteristics (SmPC),12 reaching a median maximum dose of 240 mg per day (60–720 mg/day) (Table 1). From week 10, patients could receive up to two tablets of DMF 120 mg three times daily. The maximum daily dose allowed was 720 mg of DMF. Dose escalation could be adjusted either by reducing the dose for tolerability or by achieving the desired efficacy. The median duration of the treatment was 15 weeks (minimum 4 weeks; maximum 55 weeks). All patients in treatment with DMF were described, regardless of treatment duration. Those patients who discontinued treatment have been switched to another systemic treatment and followed up.
 |
Table 1 DMF Dose Scale |
Outcomes
An evaluation of demographic characteristics and absolute PASI and affected BSA severity scales was conducted (from baseline to week 36). Data on previous treatments, comorbidities as well as side effects developed during treatment were also included. Adverse events have been collected retrospectively by searching in the clinical records of the patients.
Statistical Analysis
All parameters were depicted descriptively for the final analysis. For continuous variables, descriptive measures (number, mean, standard deviation, median, minimum and maximum values) were calculated.
Results
Study Population
A total of 57% of patients were women, and the mean (standard deviation [SD]) age was 50 (15.8) years. The mean body mass index (BMI) (SD) was 27 (5.7) and half of the patients were overweight and 17% were obese. Median absolute PASI (min.-max.) before treatment was 10 (3.6–20) and median absolute BSA affected (min.-max.) before treatment was 17 (3–59) (Table 2).
 |
Table 2 Epidemiology of Our Patients Diagnosed with Moderate-to-Severe Psoriasis and Treated with Dimethyl Fumarate |
A total of 56.7% of patients had comorbidities, being the most frequent smoking (23.3%), hypercholesterolemia (13.3%), hyperlipidemia (13.3%), and hypertension (13.3%) (Figure 1).
 |
Figure 1 Comorbidities observed in our patients treated with dimethyl fumarate. Abbreviation: COPD, chronic obstructive pulmonary disease. |
Overall, 40% of patients received concomitant treatments, with a mean (SD) number of concomitant treatments of 1.9 (1.28). The most frequent concomitant treatments were antihypertensive (30%), anticholesterolemic (20%), and proton pump inhibitors (PPI) (20%) (Figure 2A). Moreover, 80% of patients received one or more previous systemic treatments for psoriasis, mainly phototherapy (in 35% of patients), acitretin (21%), or methotrexate (13%) (Figure 2B).
 |
Figure 2 (A) Concomitant treatments (% patients). (B) Previous psoriasis treatments (% patients). Abbreviations: n, number; PPI, proton pump inhibitors; SD, standard deviation. |
Efficacy Outcomes
Efficacy of DMF was first observed at week 8 and increased in the following weeks of treatment. At baseline, median absolute PASI before receiving DMF was 10 (range 3.6–20) and median absolute BSA was 17.2 (range 3–59). At week 8 (n = 25), median absolute PASI decreased to 8 (Figure 3) and the median absolute BSA to 15 (Figure 4). At week 36 (n = 5), both median absolute PASI and BSA were 0.
 |
Figure 3 Absolute PASI from baseline to week 36. Abbreviations: n, number; PASI, Psoriasis Area and Severity Index. |
 |
Figure 4 BSA from baseline to week 36. Abbreviations: BSA, body surface area; n, number. |
After 24 weeks of DMF treatment, median absolute PASI showed a decrease in both the last observations carried forward (LOCF; n = 23) and the observed cases (OC) (n = 10): from 10 to 6 and from 10 to 1.5, respectively (Figure 5). Median absolute BSA affected also showed a decrease from 19 to 10 in LOCF patients and from 17 to 3 in OC patients (Figure 6).
 |
Figure 5 Absolute PASI at baseline and after 24 weeks of treatment. Abbreviations: LOCF, last observation carried forward; n, number; OC, observed cases; PASI, Psoriasis Area and Severity Index. |
 |
Figure 6 BSA at baseline and after 24 weeks of treatment. Abbreviations: BSA, body surface area; LOCF, last observation carried forward; n, number; OC, observed cases. |
Safety Outcomes
DMF treatment has been well tolerated in 13 patients (43.3%), while 17 patients (56.7%) presented AEs: 12 diarrhoea (40.0%), 4 flushing (13.3%) and 1 lymphopenia (3.3%). Among patients with AEs, in 47.1% of them, AEs have been solved by adjusting the DMF dose and in 11.8% of them AEs have been solved without any intervention (Figure 7).
 |
Figure 7 Patients (%) reporting adverse events during DMF treatment. Abbreviations: AEs, adverse events; DMF, dimethyl fumarate; n, number. |
Treatment discontinuation rate was 43.3%, being AEs (especially diarrhoea) the most frequent reason for treatment discontinuation in 23.3% of patients, followed by the lack of efficacy (10.0%) and patient’s decision (10.0%) (Table 3).
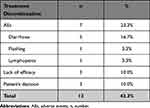 |
Table 3 Reasons of Treatment Discontinuation (Out of n Total = 30) |
Discussion
Plaque psoriasis affects the quality of life and is associated with multiple comorbidities.6,8 Among the available systemic treatments, FAEs represent an efficient and safety treatment option for adults with moderate-to-severe chronic plaque psoriasis.13–16 Although FAEs are broadly used in some European countries,2,13–16 limited data on the safety and efficacy of DMF in clinical practice in Spain are available. In this retrospective study, we describe our clinical experience for the treatment of moderate-to-severe psoriasis with DMF.
In this study, DMF was effective for treating moderate-to-severe psoriasis with a notable improvement in absolute PASI and affected BSA from week 8 of treatment. At week 8 absolute PASI decreased from 10 to 8 and affected BSA from 17.2 to 15. In half of the patients (53%) a decrease in the median absolute PASI and BSA affected was observed at week 16 of treatment (absolute PASI from 10 to 4.9 and affected BSA from 17.2 to 7.5) and at week 36 both median absolute PASI and BSA were 0. After 24 weeks of treatment with DMF, median absolute PASI decreased from 10 to 6 in LOCF patients and from 10 to 1.5 in OC patients, and median absolute BSA affected decreased from 19 to 10 in LOCF patients and from 17 to 3 in OC patients. Our results are in line with other studies of DMF.3,6,7 Similarly, preliminary results of DIMESKIN 1 study3 showed a significant median absolute PASI decrease from 11.9 to 5.3 in LOCF patients and from 12.3 to 2.0 in OC patients after 24 weeks of DMF treatment and a significant median affected BSA from 13.8 to 6.4 in LOCF patients and from 15.0 to 2.0 in OC patients. A BSA decrease with DMF was also previously found in the BRIDGE trial6 where the decrease in affected BSA was observed from week 3 onwards.
The safety profile of DMF in this study was similar to that previously described with fumarates.3,6,7,17–21 Treatment with DMF was well tolerated in 43% of patients, while 57% of patients presented with AEs. However, in our study, a high rate of the AEs (47%) have been solved by adjusting the DMF dose. In BRIDGE study, gastrointestinal symptoms were more common during the first weeks of treatment with DMF6 and in a non-interventional, retrospective analysis of data from 200 adult psoriatic patients, the main reasons for discontinuing treatment with DMF were gastrointestinal AEs.21
The fact that almost half of the patients with AEs recovered by adjusting the DMF dose highlights the importance of adjusting the dose in the management of patients treated with DMF. Again, in the BRIDGE study, it was indicated that gastrointestinal tolerance was improved by gradually increasing the dose at treatment initiation6 as recommended by the SmPC.12 Moreover, it is recommended to administer the dose with food and to reduce the dose in case of intolerance.11 Regarding lymphopenia, it can be managed with dose adjustment1 and it is recommended to reduce treatment dosage if lymphocyte counts decrease below 0.7 x 109/L and to stop the treatment dose if lymphocyte counts do not increase a month after dose reduction or if they fall below 0.5 x 109/L11 as stated in the SmPC.
In clinical practice, comorbidities and co-medication are a reality, and in our sample, 40% of patients had comorbidities, especially smoking (23%), hypercholesterolemia (13%), hyperlipidemia (13%) and hypertension (13%), and therefore these patients also took other medications, such as antihypertensive drugs (30%), anticholesterolemic drugs (20%) or PPI (20%), among others. Although this aspect needs to be studied further, there is no evidence of metabolic drug interactions for FAEs,1,2,12,22,23 being an advantage over other systemic treatments for moderate-to-severe psoriasis22,24 since the elimination route of DMF is the exhalation of CO2 and not through cytochrome P450 avoiding interaction with other drugs.12
Moreover, 80% of patients received previous systemic treatments for moderate-to-severe psoriasis. However, having received previous systemic treatments did not affect the efficacy and safety of DMF in our sample and our experience indicates that DMF could be an interesting alternative in patients who have been intolerant or failed to previous systemic therapy or patients who cannot use other systemic treatments, patients with comorbidities or with concomitant treatments. In line with our results, the preliminary data from DIMESKIN 1 study showed that, at 24 weeks, therapy with DMF demonstrated a significant improvement mainly in patients previously treated with topical, systemic, or phototherapy.3,4 Although FAEs seem to be a good alternative for those patients with limited treatment choices,1,25 further studies are needed.
The retrospective nature and the small number of patients included are the major limitations of this study. Despite this, this study provides relevant information for the clinical practice on the safety and efficacy of long-term (36 weeks) DMF treatment in patients with individual characteristics.
Conclusion
To sum up, our clinical experience indicates that DMF could be an effective and safe treatment for moderate-to-severe psoriasis in adult patients. Once the initial phase is overcome, DMF allows a clinical improvement that increases throughout the treatment duration. The median maximum dose of DMF is 240 mg, and dose adjustment is key in the management of patients treated with DMF to overcome initial AEs. Furthermore, DMF may be an interesting alternative in patients who cannot use other systemic treatments, patients with comorbidities, or with concomitant treatments.
Abbreviations
AE, adverse event; BMI, body mass index; BSA, body surface area; DMF, dimethyl fumarate; EMA, European Medicines Agency; FAEs, fumaric acid esters; LOCF, last observation carried forward; OC, observed cases; PASI, Psoriasis Area and Severity Index; PPI, proton pump inhibitors; SD, standard deviation; SmPC, Summary of Product Characteristics.
Acknowledgments
The authors would like to thank Alina Gavrus Ion, PhD, from TFS HealthScience for editorial assistance and writing support. This publication was funded by Almirall S.A., Barcelona, Spain.
Author Contributions
PRG made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas. All authors have drafted or written, or substantially revised or critically reviewed the article. All authors agreed on the journal to which the article will be submitted. All of them reviewed and agreed on all versions of the article before submission, during revision, the final version accepted for publication, and any significant changes introduced at the proofing stage. All authors agree to take responsibility and be accountable for the contents of the article.
Disclosure
PRG has received honoraria as speaker from Almirall related to this work. JGC reports grants from Almirall, during the conduct of the study. All other authors have no conflicts of interest to declare in this work.
References
1. Mrowietz U, Barker J, Boehncke WH, et al. Clinical use of dimethyl fumarate in moderate-to-severe plaque-type psoriasis: a European expert consensus. Eur Acad Dermatol Venereol. 2018;32(S3):3–14. doi:10.1111/jdv.15218
2. Reich K, Thaci D, Mrowietz U, Kamps A, Neureither M, Luger T. Efficacy and safety of fumaric acid esters in the long-term treatment of psoriasis – a retrospective study (FUTURE). J Dtsch Dermatol Ges. 2009;7(7):603–610. doi:10.1111/j.1610-0387.2009.07120.x
3. Carrascosa J, Daudén E, de la Cueva P, Salgado-Boquete L, Pau-Charles I, Fernandez-Soriano F. Efficacy of dimethyl fumarate in clinical practice among patients with moderate-to-severe plaque psoriasis: interim analysis through 24 weeks from the DIMESKIN 1 study. EMJ Dermatol. 2020;8(Suppl 1):12–19.
4. Carrascosa J, Daudén E, de la Cueva P, Salgado-Boquete L, Pau-Charles I, Fernandez-Soriano F. Improvement of patient-reported outcomes in patients with moderate-to-severe plaque psoriasis on dimethyl fumarate treatment: interim analysis through 24 weeks from DIMESKIN 1 study. EMJ Dermatol. 2020;8(Suppl 1):12–19.
5. Conti A, Giovannini L, Mandel VD, et al. Chronic kidney disease in psoriasis: a cohort study. J Dtsch Dermatol Ges. 2020;18(5):438–445. doi:10.1111/ddg.14087
6. Mrowietz U, Szepietowski JC, Loewe R, et al. Efficacy and safety of LAS41008 (dimethyl fumarate) in adults with moderate-to-severe chronic plaque psoriasis: a randomized, double-blind, Fumaderm®- and placebo-controlled trial (BRIDGE). Br J Dermatol. 2017;176(3):615–623. doi:10.1111/bjd.14947
7. Mrowietz U, Van De Kerkhof P, Schoenenberger A, et al. Efficacy of dimethyl fumarate treatment for moderate-to-severe plaque psoriasis: presentation extracts from the 29 th EADV virtual congress, 29–31 October 2020. Expert Rev Clin Immunol. 2021;17(sup2):1–11. doi:10.1080/1744666X.2021.1919510
8. Parisi R, Iskandar IYK, Kontopantelis E, Augustin M, Griffiths CEM, Ashcroft DM. National, regional, and worldwide epidemiology of psoriasis: systematic analysis and modelling study. BMJ. 2020;m1590. doi:10.1136/bmj.m1590
9. Nast A, Spuls PI, van der Kraaij G, et al. European S3-Guideline on the systemic treatment of psoriasis vulgaris - Update Apremilast and Secukinumab - EDF in cooperation with EADV and IPC. J Eur Acad Dermatol Venereol. 2017;31(12):1951–1963. doi:10.1111/jdv.14454
10. Sbidian E, Chaimani A, Garcia-Doval I, et al. Systemic pharmacological treatments for chronic plaque psoriasis: a network meta-analysis. Cochrane Database Syst Rev. 2020. doi:10.1002/14651858.CD011535.pub3
11. Nast A, Gisondi P, Ormerod AD, et al. European S3-Guidelines on the systemic treatment of psoriasis vulgaris–Update 2015–Short version–EDF in cooperation with EADV and IPC. J Eur Acad Dermatol Venereol. 2015;29(12):2277–2294. doi:10.1111/jdv.13354
12. European Medicines Agency. Skilarence, INN-dimethyl fumarate: summary of product characteristics; 2017. Available from: https://www.ema.europa.eu/en/documents/product-information/skilarence-epar-product-information_en.pdf.
13. Balasubramaniam P, Stevenson O, Berth-Jones J. Fumaric acid esters in severe psoriasis, including experience of use in combination with other systemic modalities. Br J Dermatol. 2004;150(4):741–746. doi:10.1111/j.0007-0963.2004.05739.x
14. Burden-Teh E, Lam M, Cohen S. Fumaric acid esters to treat psoriasis: experience in a UK teaching hospital. J Am Acad Dermatol. 2013;68(4):AB52. doi:10.1016/j.jaad.2012.12.217
15. Carboni I, Felice CD, Simoni ID, Soda R, Chimenti S. Fumaric acid esters in the treatment of psoriasis: an Italian experience. J Dermatol Treat. 2004;15(1):23–26. doi:10.1080/09546630310019346
16. Heelan K, Markham T. Fumaric acid esters as a suitable first-line treatment for severe psoriasis: an Irish experience: correspondence. Clin Exp Dermatol. 2012;37(7):793–795. doi:10.1111/j.1365-2230.2012.04351.x
17. Brück J, Dringen R, Amasuno A, Pau-Charles I, Ghoreschi K. A review of the mechanisms of action of dimethylfumarate in the treatment of psoriasis. Exp Dermatol. 2018;27(6):611–624. doi:10.1111/exd.13548
18. van Hezik DF, Bovenschen HJ. Association of lymphopenia and eosinophilia with dimethylfumarate treatment efficacy and tolerability in psoriasis: a retrospective study. J Dermatol Treat. 2020;31(4):378–381. doi:10.1080/09546634.2019.1605135
19. Reszke R, Szepietowski JC. A safety evaluation of dimethyl fumarate in moderate-to-severe psoriasis. Expert Opin Drug Saf. 2020;19(4):373–380. doi:10.1080/14740338.2020.1736553
20. Balak DMW, Gerdes S, Parodi A, Salgado-Boquete L. Long-term safety of oral systemic therapies for psoriasis: a comprehensive review of the literature. Dermatol Ther (Heidelb). 2020;10(4):589–613. doi:10.1007/s13555-020-00409-4
21. Termeer C, Reinhold U, Dirschka T, von Kiedrowski R, Kurzen H. Long-term use of fumaric acid esters for the treatment of psoriasis in daily practice. J Dermatol Treat. 2021;32(6):610–616. doi:10.1080/09546634.2019.1688234
22. Thaçi D, Weisenseel P, Philipp S, et al. Efficacy and safety of fumaric acid esters in patients with psoriasis on medication for comorbid conditions - a retrospective evaluation (FACTS): fumaric acid esters in psoriasis with co-medication. J Dtsch Dermatol Ges. 2013;11(5):429–435. doi:10.1111/ddg.12059
23. Tzaneva S, Geroldinger A, Trattner H, Tanew A. Fumaric acid esters in combination with a 6-week course of narrowband ultraviolet B provides an accelerated response compared with fumaric acid esters monotherapy in patients with moderate-to-severe plaque psoriasis: a randomized prospective clinical study. Br J Dermatol. 2018;178(3):682–688. doi:10.1111/bjd.16106
24. Saurat JH, Guérin A, Yu AP, et al. High prevalence of potential drug-drug interactions for psoriasis patients prescribed methotrexate or cyclosporine for psoriasis: associated clinical and economic outcomes in real-world practice. Dermatology. 2010;220(2):128–137. doi:10.1159/000275198
25. Harries MJ, Chalmers RJG, Griffiths CEM. Fumaric acid esters for severe psoriasis: a retrospective review of 58 cases: FAE for severe psoriasis: a retrospective review. Br J Dermatol. 2005;153(3):549–551. doi:10.1111/j.1365-2133.2005.06728.x
 © 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
