Back to Journals » Breast Cancer: Targets and Therapy » Volume 15
Differences in Treatment Outcomes Between Patients with HER2-Low versus HER2-Zero, Hormone Receptor-Positive Advanced-Stage Breast Cancer Treated with Ribociclib
Authors Sharaf B , Abu-Fares H, Tamimi F , Al-Sawajneh S, Salama O, Daoud R, Alhajahjeh A , Al-Lababidi S, Abdel-Razeq H
Received 22 April 2023
Accepted for publication 14 July 2023
Published 28 July 2023 Volume 2023:15 Pages 541—548
DOI https://doi.org/10.2147/BCTT.S415432
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Professor Harikrishna Nakshatri
Baha’ Sharaf, Hala Abu-Fares, Faris Tamimi, Suhaib Al-Sawajneh, Osama Salama, Rand Daoud, Abdulrahman Alhajahjeh, Sawsan Al-Lababidi, Hikmat Abdel-Razeq
Department of Internal Medicine, King Hussein Cancer Center, Amman, Jordan
Correspondence: Hikmat Abdel-Razeq, Department of Internal Medicine, King Hussein Cancer Center, Queen Rania Al Abdullah Street, P.O. Box: 1269, Amman, 11941, Jordan, Tel +962-6 5300460, Ext: 1000, Email [email protected]
Background: Metastatic breast cancers (MBC) with no expression of human epidermal growth factor receptor-2 (HER2) are recently classified into two groups; HER2-zero [HER2-immunohistochemistry (IHC) score of 0 (IHC-0)] and HER2-low, defined as those with IHC score of 1+ or 2+ with negative in situ hybridization (ISH) assay. We investigate differences in treatment outcomes between both groups treated with endocrine therapy (ET) and the CDK4/6 inhibitor ribociclib.
Methods: Data were retrospectively collected for patients with HR-positive+/HER2−negative MBC who received ribociclib with an aromatase inhibitor (AI) or fulvestrant and were divided into two groups: HER2-zero and HER2-low.
Results: A total of 257 patients, median age 48 (22– 87) years, all with MBC who were treated with ET and ribociclib were enrolled. One hundred and thirty-seven (53.3%) patients had de novo MBC, and majority (n = 162, 63.0%) received ribociclib as a first-line therapy. In total, 114 (44.4%) patients had HER2-zero (IHC-0), while 143 (55.6%) others had HER2-low disease. The overall response rate (ORR) was 52.0% for the HER2-zero group compared to 39.4% for the HER2-low group, p = 0.005. The median PFS was 22.2 (95% confidence interval [CI], 19.4-NR) months for HER2-zero versus 17.3 (95% CI, 14.1– 20.6) months for HER2-low, P = 0.0039. In multivariable analysis, HER2-low expression remained significant determinant of inferior PFS after adjusting for other factors, including the site of metastasis, prior chemotherapy, and the line of treatment.
Conclusion: In patients with MBC treated with ET and ribociclib, level of HER2 negativity may affect treatment outcomes; patients with HER2-zero had better response rate and PFS compared to those with HER2-low disease. These findings, if confirmed in larger studies, may help oncologists select patients with HER2-low for better treatment options.
Keywords: breast cancer, CDK4/6 inhibitors, endocrine therapy, HER2-low, HER2-zero
Introduction
Breast cancer continues to be the most commonly diagnosed cancer worldwide,1 with an estimated 2.3 million new cancer cases and 0.7 million cancer-related deaths in 2020.2 Human epidermal growth factor receptor-2 (HER2)-positive breast cancer constitutes around 15–20% of all patients, and is considered prognostic and predictive marker for disease response to different treatment modalities. Over the past years, many drugs were developed targeting HER2 in different disease settings with significant improvement in overall response rate (ORR), PFS and overall survival (OS), which in turn changed the natural course of HER2-positive breast cancer. However, the expression level of HER2 does not follow all or non-theory, as it is a spectrum of negative to positive depending on the intensity of IHC.
Hormone receptor (HR)-positive, HER2-negative metastatic breast cancer (MBC) represents around 80% of histologic subtypes of invasive breast cancer.3 Except in cases of visceral crisis, where chemotherapy is indicated,4 the combination of a CDK4/6 inhibitor (ribociclib, palbociclib, abemaciclib) with endocrine therapy (an aromatase inhibitor or fulvestrant) has become the standard-of-care first-line treatment for patients with metastatic HR-positive, HER2-negative breast cancer, with substantial improvement in both PFS and OS.5–9
HER2 expression is currently assessed by immunohistochemistry (IHC) as per the American Society of Clinical Oncology (ASCO)/College of American Pathologists (CAP) guidelines, with IHC 0, +1 or +2 with a negative in situ hybridization (ISH) being classified as HER2-negative.10 The quantification of HER2 status using immunohistochemistry (IHC) is as follows: 0 indicates no staining or staining on the cell membrane in less than 10% of tumor cells, 1+ represents faint or barely perceptible staining in more than 10% of tumor cells with no or weak intensity, and 2+ indicates weak to moderate staining covering the entire cell membrane in more than 10% of tumor cells.
However, an emerging body of evidence in recent years suggests that patients with the HER2-negative subtype are not the same. Clinical behavior and response to therapies might differ in relation to intensity of IHC expression. Compared to patients who do not express any IHC (IHC-zero), patients with IHC +1 or those with +2 and negative ISH, have poor prognostic factors, including larger tumor sizes, higher histological grades, higher Ki-67 score and more regional lymph node involvement.11–14
Even though the prognostic significance of low HER2 expression is still being investigated, its predictive role has now been firmly elucidated.15 Most clinical trials use IHC 1+, or IHC 2+ and ISH- negative as the definition of HER2-low breast cancer, and the proportion of people with HER2-low expression is as high as 45–55%.16–18
The entity of HER2-low breast cancer has recently changed the treatment landscape of MBC, as the low HER2 expression became a valid therapeutic target. Breast cancer with low (IHC +1) or moderate expression of HER2 (IHC+2) without amplification are not candidates for conventional anti-HER2 agents.19 However, results from recent clinical trials have shown that such group of patients can be treated with antibody-drug conjugates,20 like trastuzumab deruxtecan21 and trastuzumab duocarmazine.22 The DESTINY-Breast-04 trial utilized a novel antibody–drug conjugate (ADC) trastuzumab deruxtecan in HER2-low MBC and showed improvement in both PFS and OS.15
With this novel data, and the rapidly expanding HER2-low terminology in MBC, several questions may be raised related to the differential response to various therapeutic modalities in relation to intensity of IHC expression. In this study, we aimed to evaluate the differences in outcome between patients with HER2-low and HER2-zero disease in patients treated with ribociclib and endocrine therapy for advanced HR-positive disease.
Methods
Patients’ Population
We retrospectively reviewed patients with HR-positive/HER2-negative MBC who received ribociclib with an aromatase inhibitor (AI) or fulvestrant in any metastatic setting (visceral or bone-only), and at any phase of the disease course (de novo metastasis or recurrent). Estrogen receptor (ER) and progesterone receptor (PR) were detected by IHC and were considered positive if ≥1%, while HER2 negativity was defined as IHC-0, +1 or +2 with a negative ISH, as recommended by the American Society of Clinical Oncology (ASCO)/College of American Pathologists (CAP) guidelines and were then divided into two groups: HER2-zero and HER2-low. HER2-zero was defined as IHC-0, and HER2-low was defined as IHC 1+ or IHC 2+/ISH-negative.
Patients were enrolled if they had metastatic breast cancer confirmed histologically, HR-positive/HER2-negative and received a combination of both CDK4/6 inhibitors plus AI or fulvestrant. Patients with second primary cancer and those with no adequate follow-up data were excluded. The study was approved by the Institutional Review Board (IRB) at King Hussein Cancer Center. Because the data were deidentified and collected retrospectively, informed consent was waived.
Treatment
Ribociclib was given at a dose of 600 mg orally as the initial dose once daily for 21 consecutive days (day 1–21) in a 4-week cycle. Anastrozole, letrozole or fulvestrant was administered concurrently. Fulvestrant was given at a dose of 500 mg intramuscularly on day-1 and day-15 of cycle-1 and then every 28 days afterward. Anastrozole (1 mg) and letrozole (2.5 mg) were given orally on continuous daily schedule. For premenopausal patients, a gonadotropin-releasing hormone (GnRH) agonist (goserelin) was administered subcutaneously at dose of 3.6 mg every 28 days, starting 1 month before hormonal treatment.
Response Evaluation and Statistical Analysis
The clinical efficacy was evaluated in accordance with the RECIST 1.1 criteria utilizing CT scans every 3 months, or earlier when needed, and bone scans every 6–12 months. Progression-free survival (PFS) was defined as the time from the initiation of CDK4/6 inhibitors to the date of radiological or clinical progression or death and was estimated by the Kaplan–Meier method and compared by the Log rank test. Multivariate Cox regression modeling was performed with covariates including menopausal status (premenopausal versus postmenopausal), prior chemotherapy, site of metastases (visceral versus bone-only), and line of treatment (first-line or beyond).
Results
A total of 257 patients with MBC who received ET and CDK4/6 inhibitors (ribociclib in all patients) were included. Median age was 48 (22–87) years, 122 (47.5%) were premenopausal and except for one patient, all were female. Majority of the tumors were invasive ductal 211 (82.1%) and 137 (53.3%) patients had de novo metastatic disease. At the time of CDK4/6 treatment, 135 (52.5%) had visceral metastases. Majority 162 (63.0%) received ribociclib as a first-line therapy while the others had it as second line and beyond, Table 1.
 |
Table 1 Characteristics of the Patients (n = 257) |
In total, 114 (44.4%) of the patients were HER2-zero (IHC-0), while 143 (55.6%) others had HER2-low disease, as defined above. The ORR for the HER2-zero group was 52.0% compared to 39.4% for the HER2-low group (p = 0.005). The median PFS was 22.2 (95% confidence interval [CI], 19.4-NR) months for HER2-zero versus 17.3 (95% CI 14.1–20.6) months for HER2-low, p = 0.0039 (Figure 1).
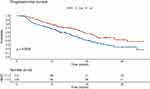 |
Figure 1 Progression-free survival for HER2-low versus HER2-zero. Note: Progression-free survival was higher for HER2-zero. |
In the univariable Cox proportional hazard analysis, PFS was significantly lower in patients with visceral metastasis (HR, 1.81; 95% CI, 1.29–2.54; P = 0.001), received prior chemotherapy (HR, 1.80; 95% CI, 1.27–2.55; P = 0.001), HER2 low (HR, 1.67; 95% CI, 1.19–2.36; p = 0.003), and for whom received ribociclib as a second line or beyond (HR, 2.25; 95% CI, 1.60–3.16; P < 0.001) (Table 2).
 |
Table 2 Univariable and Multivariable Cox Proportional Regression Analysis of Variable with Progression-Free Survival |
On the other hand, there was no significant PFS difference based on histology, tumor grade, time of metastasis either De novo or relapse, menopausal status, or smoking history.
In the multivariable analysis, PFS was lower in HER2-low than in HER2-zero group (HR, 1.51; 95% CI, 1.06–2.13; P = 0.021) after adjustment for site of metastasis, prior chemotherapy, and line of treatment (Table 2).
Discussion
Our study evaluated the differences in treatment outcomes of patients with HER2-low versus those with HER2-zero MBC treated with CDK4/6 inhibitors (ribociclib) and AI or fulvestrant in various metastatic settings, and clearly showed significant differences according to HER2 expression level in favor of those with HER2-zero. Such findings, if confirmed in larger studies, may have significant clinical impact, especially so after the introduction of antibody-drug conjugates (ADC) that have shown a meaningful effect when used to treat HER2-low breast cancer. The data from phase-3 DESTINY Breast-04 trial showed improvement in PFS and OS with ADC trastuzumab deruxtecan compared to investigator choice in HER2-low metastatic breast cancer, thus affirming HER2-low as a distinct entity of breast cancer and resulted in paradigm shift in breast cancer classification. So, our findings may help select a subgroup of HR-positive, HER2-negative patients (HER2-low) with MBC who benefit less from CDK4/6 inhibitors who can be offered other drugs like antibody-drug conjugates as discussed above.
Several other studies reached similar conclusions. A study from Hong Kong reported treatment outcomes on 106 patients treated mostly with palbociclib (85%), majority (77%) of the patients were considered HER2-low and had a shorter median PFS compared with HER2-zero patients; 8.9 versus 18.8 months, p = 0.01.23 Another Greek multicenter study reported real-world data testing the same concept on 191 patients and showed worsening PFS with increasing HER2 expression; 3.35 years for HER2-zero patients, 2.18 years for HER2 +1 patients, and 1.74 years for HER2 +2/ISH-negative patients; however, this difference did not reach statistical significance (p = 0.477).24
However, another Italian study from six oncology units reached a different conclusion. In this retrospective study, 252 consecutive HR-positive/HER2-negative patients, all with MBC were treated with ET plus palbociclib in first-line setting. No significant difference in PFS (p = 0.20) or OS (p = 0.1) was observed between HER2-zero and HER2-low subgroups. However, only 165 (65%) patients were included in the analysis and patients enrolled were significantly older than ours; median age at treatment start was 64 years compared to 48 years in our study.25 Another smaller study that enrolled only 45 patients and utilized palbociclib showed no difference in the efficacy of CDK4/6 inhibitors in HER2-zero and HER2-low groups.26
In our institution, we utilize the widely used Ventana 4B5 assay to determine HER2 status. However, recent studies have uncovered significant inconsistencies and insufficient reproducibility when determining HER2 IHC status, particularly in cases with low expression levels.27 This is due to the limitations of FDA-approved HER2 IHC assays, which primarily focus on identifying positive or negative cases and provide limited assessment and differentiation for cases with low expression (0/1+) levels.28,29 These findings raise concerns regarding the performance of these assays, not only for the historical drugs they were originally approved for, but also for their potential use with new drugs. As a result, there is a need for further investigation into the suitability and effectiveness of these assays in both contexts.
Our study is not without limitations; its retrospective nature and the use of only one CDK4/6 inhibitors (ribociclib) are potential limitations.
However, our data, and the very few published others, should be an eye opener for HER2-low as a distinctive pathological and clinical entity. More studies and clinical trials are anticipated in different settings including neoadjuvant therapy in early-stage breast cancer.30
Conclusions
In patients with MBC treated with ribociclib and ET, level of HER2 negativity may affect treatment outcomes; patients with HER2-zero have better PFS compared to those with HER2-low disease. These findings, if confirmed in larger studies, should help oncologists select patients with HER2-low for better treatment options.
Data Sharing Statement
The datasets generated during and/or analyzed during the current study are available from the corresponding author on reasonable request.
Ethics Declarations
The study was approved by the Institutional Review Board (IRB) (Approval Number: 20 KHCC 136) at King Hussein Cancer Center, and all procedures were performed based on the regulations of Helsinki. Given the retrospective nature of the study and lack of patients’ identifiers, consent to participate was waived the IRB.
Consent for Publication
Data submitted are entirely unidentifiable, and there are no details on individuals reported within the manuscript.
Acknowledgment
The abstract of this paper was presented at the 2022 San Antonio Breast Cancer Symposium (SABCS), San Antonio, TX, USA (06-10 December 2022) as a poster presentation with interim findings. The poster’s abstract was published as a conference proceeding: Cancer Research; 2023; 83 (5_Supplement): P4-07-33. Available at: https://aacrjournals.org/cancerres/article/83/5_Supplement/P4-07-33/717994/Abstract-P4-07-33-Differences-in-Treatment
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Funding
This research was not funded.
Disclosure
The authors declared that they have no conflicting interest.
References
1. World Cancer Research Fund International. Breast cancer statistics. Available from: https://www.wcrf.org/cancer-trends/breast-cancer-statistics/.
2. Siegel RL, Miller KD, Jemal A. Cancer statistics, 2020. CA Cancer J Clin. 2020;70(1):7–30. doi:10.3322/caac.21590
3. Howlader N, Altekruse SF, Li CI, et al. US incidence of breast cancer subtypes defined by joint hormone receptor and HER2 status. J Natl Cancer Inst. 2014;106(5). doi:10.1093/jnci/dju055
4. Sbitti Y, Slimani K, Debbagh A, et al. Visceral crisis means short survival among patients with luminal A metastatic breast cancer: a retrospective cohort study. World J Oncol. 2017;8(4):105–109. doi:10.14740/wjon1043w
5. Im SA, Lu YS, Bardia A, et al. Overall survival with ribociclib plus endocrine therapy in breast cancer. N Engl J Med. 2019;381(4):307–316. doi:10.1056/NEJMoa1903765
6. Goetz MP, Toi M, Campone M, et al. MONARCH 3: abemaciclib as initial therapy for advanced breast cancer. J Clin Oncol. 2017;35(32):3638–3646. doi:10.1200/JCO.2017.75.6155
7. Finn RS, Martin M, Rugo HS, et al. Palbociclib and Letrozole in advanced breast cancer. N Engl J Med. 2016;375(20):1925–1936. doi:10.1056/NEJMoa1607303
8. Sledge GW, Toi M, Neven P, et al. The effect of abemaciclib plus fulvestrant on overall survival in hormone receptor-positive, ERBB2-negative breast cancer that progressed on endocrine therapy-MONARCH 2: a randomized clinical trial. JAMA Oncol. 2020;6(1):116–124. doi:10.1001/jamaoncol.2019.4782
9. Hortobagyi GN, Stemmer SM, Burris HA, et al. Ribociclib as first-line therapy for HR-positive, advanced breast cancer. N Engl J Med. 2016;375(18):1738–1748. doi:10.1056/NEJMoa1609709
10. Wolff AC, Hammond MEH, Allison KH, et al. Human epidermal growth factor receptor 2 testing in breast cancer: American Society of Clinical Oncology/College of American Pathologists clinical practice guideline focused update. Arch Pathol Lab Med. 2018;142(11):1364–1382. doi:10.5858/arpa.2018-0902-SA
11. Camp RL, Dolled-Filhart M, King BL, Rimm DL. Quantitative analysis of breast cancer tissue microarrays shows that both high and normal levels of HER2 expression are associated with poor outcome. Cancer Res. 2003;63(7):1445–1448.
12. Ignatov T, Eggemann H, Burger E, Fettke F, Costa SD, Ignatov A. Moderate level of HER2 expression and its prognostic significance in breast cancer with intermediate grade. Breast Cancer Res Treat. 2015;151(2):357–364. doi:10.1007/s10549-015-3407-2
13. Won HS, Ahn J, Kim Y, et al. Clinical significance of HER2-low expression in early breast cancer: a nationwide study from the Korean Breast Cancer Society. Breast Cancer Res. 2022;24(1):22. doi:10.1186/s13058-022-01519-x
14. Eggemann H, Ignatov T, Burger E, et al. Moderate HER2 expression as a prognostic factor in hormone receptor positive breast cancer. Endocr Relat Cancer. 2015;22(5):725–733. doi:10.1530/ERC-15-0335
15. Modi S, Jacot W, Yamashita T, et al. Trastuzumab deruxtecan in previously treated HER2-Low advanced breast cancer. N Engl J Med. 2022;387(1):9–20. doi:10.1056/NEJMoa2203690
16. Agostinetto E, Rediti M, Fimereli D, et al. HER2-low breast cancer: molecular characteristics and prognosis. Cancers. 2021;13(11):2824. doi:10.3390/cancers13112824
17. Tarantino P, Hamilton E, Tolaney SM, et al. HER2-low breast cancer: pathological and clinical landscape. J Clin Oncol. 2020;38(17):1951–1962. doi:10.1200/JCO.19.02488
18. Kurozumi S, Padilla M, Kurosumi M, et al. HER2 intratumoral heterogeneity analyses by concurrent HER2 gene and protein assessment for the prognosis of HER2 negative invasive breast cancer patients. Breast Cancer Res Treat. 2016;158(1):99–111. doi:10.1007/s10549-016-3856-2
19. Fehrenbacher L, Cecchini RS, Geyer CE, et al. NSABP B-47/NRG oncology phase III randomized trial comparing adjuvant chemotherapy with or without trastuzumab in high-risk invasive breast cancer negative for HER2 by FISH and with IHC 1+ or 2. J Clin Oncol. 2020;38(5):444–453. doi:10.1200/JCO.19.01455
20. Nakada T, Sugihara K, Jikoh T, Abe Y, Agatsuma T. The latest research and development into the antibody-drug conjugate, [fam-] trastuzumab deruxtecan (DS-8201a), for HER2 cancer therapy. Chem Pharm Bull. 2019;67(3):173–185. doi:10.1248/cpb.c18-00744
21. Takegawa N, Tsurutani J, Kawakami H, et al. [fam-] trastuzumab deruxtecan, antitumor activity is dependent on HER2 expression level rather than on HER2 amplification. Int J Cancer. 2019;145(12):3414–3424. doi:10.1002/ijc.32408
22. Banerji U, van Herpen CML, Saura C, et al. Trastuzumab duocarmazine in locally advanced and metastatic solid tumours and HER2-expressing breast cancer: a Phase 1 dose-escalation and dose-expansion study. Lancet Oncol. 2019;20(8):1124–1135. doi:10.1016/S1470-2045(19)30328-6
23. Bao KKH, Sutanto L, Tse SSW, Man Cheung K, Chan JCH. The association of ERBB2-low expression with the efficacy of cyclin-dependent kinase 4/6 inhibitor in hormone receptor-positive, ERBB2-negative metastatic breast cancer. JAMA Netw Open. 2021;4(11):e2133132. doi:10.1001/jamanetworkopen.2021.33132
24. Douganiotis G, Kesisis G, Lalla E, Korantzis I, Boukovinas I, Papazisis K. Prognostic significance of low HER2 expression in patients with metastatic hormone receptor-positive breast cancer treated with first line CDK4/6 inhibitors: a Greek multicenter real-world data analysis. Cancer Diagn Progn. 2022;2(5):585–591. doi:10.21873/cdp.10146
25. Carlino F, Diana A, Ventriglia A, et al. HER2-low status does not affect survival outcomes of patients with Metastatic Breast Cancer (MBC) undergoing first-line treatment with endocrine therapy plus palbociclib: results of a multicenter, retrospective cohort study. Cancers. 2022;14(20):4981. doi:10.3390/cancers14204981
26. Shao Y, Luo Z, Yu Y, et al. HER2-low expression does not affect the clinical outcomes of metastatic breast cancer treated with CDK4/6 inhibitor: a real-world study. Front Endocrinol. 2022;13:1000704. doi:10.3389/fendo.2022.1000704
27. Robbins CJ, Fernandez AI, Han G, et al. Multi-institutional assessment of pathologist scoring HER2 immunohistochemistry. Mod Pathol. 2023;36(1):100032. doi:10.1016/j.modpat.2022.100032
28. Lambein K, Van Bockstal M, Vandemaele L, et al. Distinguishing score 0 from score 1+ in HER2 immunohistochemistry-negative breast cancer: clinical and pathobiological relevance. Am J Clin Pathol. 2013;140(4):561–566. doi:10.1309/AJCP4A7KTAYHZSOE
29. Casterá C, Bernet L. HER2 immunohistochemistry inter-observer reproducibility in 205 cases of invasive breast carcinoma additionally tested by ISH. Ann Diagn Pathol. 2020;45:151451. doi:10.1016/j.anndiagpath.2019.151451
30. Hurvitz SA, Peddi PF, Tetef ML, et al. TRIO-US B-12 TALENT: Phase II neoadjuvant trial evaluating trastuzumab deruxtecan with or without anastrozole for HER2-low, HR+ early stage breast cancer. J Clin Oncol. 2021;39(15_suppl):TPS603–TPS603. doi:10.1200/JCO.2021.39.15_suppl.TPS603
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
