Back to Journals » Pediatric Health, Medicine and Therapeutics » Volume 14
Diagnostic and Management Strategies of Food Protein-Induced Enterocolitis Syndrome: Current Perspectives
Authors Mulé A, Prattico C, Al Ali A, Mulé P, Ben-Shoshan M
Received 18 July 2023
Accepted for publication 13 October 2023
Published 24 October 2023 Volume 2023:14 Pages 337—345
DOI https://doi.org/10.2147/PHMT.S404779
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Professor Roosy Aulakh
Angela Mulé, Catherine Prattico, Adnan Al Ali, Pasquale Mulé, Moshe Ben-Shoshan
Division of Allergy and Clinical Immunology, Department of Pediatrics, Montreal Children’s Hospital, McGill University Health Centre, Montreal, QC, Canada
Correspondence: Moshe Ben-Shoshan, Division of Allergy and Clinical Immunology, Department of Pediatrics, Montreal Children’s Hospital, McGill University Health Centre, 1001 Decarie Blvd, Montreal, QC, H4A 3J1, Canada, Tel +1 514 412-4400, Fax +1 514 412-4288, Email [email protected]
Abstract: Food protein-induced enterocolitis syndrome (FPIES) is a form of non-IgE mediated food allergy that presents with delayed gastrointestinal symptoms after ingestion of the trigger food. The data regarding FPIES are sparse, despite being recognized as a distinct clinical entity. This narrative review presents the characteristics of this disorder in the pediatric population, as well-standard diagnostic and management protocols. FPIES can be classified into acute and chronic subtypes, and some cases may develop into an IgE-mediated allergy. Given that skin prick tests and specific IgE levels are negative in the majority of cases, diagnosis relies on clinical history and oral food challenges. Management involves elimination diets, assessment of tolerance through oral food challenges, and rehydration in the event of a reaction. Future research should focus on improving diagnostic methods, illustrating underlying pathogenesis and biomarkers, and assessing long-term natural history. Increased knowledge and awareness for FPIES are required.
Keywords: FPIES, non-IgE mediated food allergy, oral food challenge, elimination diet
Introduction
Adverse reactions to food may be immune or non-immune mediated. Immune-mediated reactions to food, also known as food allergy, may be immunoglobulin E (IgE), non-IgE, mixed IgE/non-IgE, or cell mediated.1–3 Food protein-induced enterocolitis syndrome (FPIES) is a form of non-IgE mediated food allergy that manifests as delayed gastrointestinal symptoms after ingestion of the culprit food.3,4 FPIES imposes a burden on patients and their families, as food avoidance and dietary restrictions are necessary.5 Moreover, the common treatment used for classical IgE mediated allergies such as epinephrine and antihistamines is not viable.5,6 While FPIES is recognized as a distinct clinical entity, the data regarding FPIES are sparse, especially in the pediatric population. Therefore, the purpose of this review is to highlight the characteristics of this disorder in children, as well as the current diagnostic and management strategies.
Definition and Natural History
FPIES can manifest itself with a wide-array of symptoms. Symptoms can include vomiting, diarrhea, lethargy, hypotonia, hypotension, hypothermia, and metabolic derangements.7 FPIES may be sub-classified into acute and chronic cases. Acute FPIES is associated with intermittent ingestion of the culprit food at a lower dose, while chronic FPIES is associated with daily ingestion.8 In addition, a subset of patients exhibit an unusual form of FPIES, referred to as atypical FPIES, which is characterized by a potential for the condition to progress into a typical IgE-mediated hypersensitivity.8
FPIES typically begins during infancy, however it is now being increasingly recognized in older age groups.7 FPIES often presents when complementary foods are introduced in a child’s diet.9 Infantile FPIES is reported to often resolve by the time school age is reached, mainly for milk and egg.10 Therefore, the natural history of FPIES in infants is generally favorable. However, in some cases FPIES may have more persistent phenotypes.7 The main food triggers can vary depending on age, phenotype, and geographical location, however, all foods have the capacity to induce FPIES.5,11 While the distribution of these main triggers varies by country and/or region, CM, fish, egg, and grains are the most frequently reported common triggers globally.12 In the Mediterranean region, fish is one of the most common triggers, while three studies conducted in Australia reported rice as the main trigger, followed by CM.12 In infants and children with acute FPIES in the United States, rice and oat are the primary triggers, followed by cow’s milk (CM), soy, egg, fish, fruits, and vegetables, according to a retrospective study.13 In chronic FPIES, CM and soy have been identified as the most common triggers, specifically in countries that use soy-based formula for infants.14 Shellfish and fish are reported to be the main triggers in older children and adults, followed by wheat, egg, and dairy.15–17 Approximately 60% of infants with FPIES may experience a reaction to a single food.10,18 Additionally, approximately 1 in 3 infants may react to 2 to 3 different foods, while 1 in 10 infants may react to multiple foods.10,18 Among adults, it is reported that 60% of those with seafood-FPIES may exhibit reactions to a single food group (either selfish or fish).7
Prevalence and Incidence
There are limited data regarding the epidemiology of FPIES, therefore the exact prevalence of the condition remains unknown.11 The wide range of symptoms, absence of diagnostic biomarkers, occurrence of misdiagnosis, and absence of specific diagnostic markers also contribute to the limited epidemiological data.7 However, data suggest that FPIES is not rare, with a cumulative incidence of 0.015% reported in children younger than 2 years old in Australia, 0.7% reported in infants in Spain, and 0.36% reported in infants in the United Kingdom.19 Additionally, a cumulative incidence of 0.34% for milk-induced FPIES was reported in the Israeli population.20 Moreover, the population prevalence estimates for children and adults in the United States are 0.51% and 0.22%, respectively.19 The prevalence of chronic FPIES is also not well-established due to the challenge of distinguishing FPIES symptoms from those of other food protein enteropathies.21 Five to 25% of FPIES patients are reported to have atypical FPIES, with a higher prevalence of sensitization to CM and egg.11
Pathogenesis
FPIES is categorized as a non-IgE mediated food allergy where the immune response acts through cell-mediated mechanisms.22 However, pathogenic pathways have yet to be established.23 Symptom occurrence in FPIES typically manifests within 1 to 4 hr, which is longer than immediate reactions observed in IgE-mediated allergies, which usually present within less than 2 hr.11 Conversely, the time of symptom occurrence in FPIES is shorter than delayed cell-mediated food reactions and can manifest anywhere between several hours and days.11 This suggests that both adaptive and innate immune responses are likely involved in FPIES.11 Although FPIES is classified as a non-IgE mediated food allergy, roughly 5% to 30% of individuals presenting with FPIES exhibit low levels of IgE antibodies specific to the trigger food.7
Diagnosis
Diagnostic Tests
The majority of FPIES patients have negative skin prick tests and undetectable sIgE levels.24 However, it is important to note that a positive skin prick test and/or detectable sIgE levels are associated with atypical FPIES.10 The lack of specific diagnostic testing in the majority of FPIES cases, as well as non-specific FPIES-related symptoms likely account for the delay in diagnosis, with some studies reporting a median delay of 4–7 months.25 Consequently, diagnosis of acute FPIES relies on detailed clinical history and recognition of symptoms that align with acute FPIES diagnostic criteria, as well as the use of food challenges when diagnosis is unclear after considering patient history (Table 1).24,26 Furthermore, while there is no laboratory testing specific to the diagnosis of acute FPIES, various confirmatory tests are available to assist in supporting the diagnosis and to rule out potential differential diagnoses.26 On the other hand, the most important diagnostic modality for chronic FPIES is the use of elimination diets (Table 1).26
 |
Table 1 Diagnostic Modality and Management for Acute and Chronic FPIES |
Suggestive History (Table 2)
Acute FPIES is mainly characterized by the manifestation of repetitive and projectile vomiting, which typically occurs within 1 to 4 hr (generally 2 hr) of after ingestion of the trigger food (Table 2).17 This may be accompanied by diarrhea (within 6 to 8 hr after food ingestion), concurrent lethargy, hypotonia, pallor, and/or hypothermia.17 These symptoms generally subside within 24 hr.17 Severe reactions that occur during an OFC or an acute episode are linked to prolonged diarrhea and abdominal pain, which last for a few days or weeks.7
 |
Table 2 Clinical Characteristics of Infantile and Adult FPIES |
Chronic FPIES is mainly characterized by the presence of frequent watery diarrhea, which can occasionally contain blood or mucus.27 This is accompanied by intermittent and progressively worsening vomiting, which can occur over a period of days or weeks, which is associated with poor weight gain or weight loss.7,27 Children presenting with CM or soy FPIES may initially exhibit chronic symptoms during infancy and acute symptoms when reintroducing food after a period of avoidance.7,27
FPIES in older children and adults typically manifests as acute symptoms within 1 to 4 hr after ingestion of the trigger food, which is often seafood.7 There are reports of patients tolerating the culprit food regularly beforehand with no identifiable trigger event leading to the development of FPIES.7 The main symptoms reported include severe abdominal pain, which is followed by diarrhea and vomiting.28 Extreme cases may include loss of consciousness.17
Oral Challenges and Elimination Diets
Oral food challenge is currently the gold standard diagnostic test for acute FPIES.26 However, it is not necessary if there is a history of severe reactions and patients become asymptomatic upon elimination of the suspected food.7 A critical criterion for diagnosing chronic FPIES is rapid symptom resolution upon the elimination of triggering food(s) and the subsequent recurrence of acute symptoms when that food is reintroduced.26 To help guide challenges and elimination diets for diagnosis, physicians can employ a step-wise approach to food introduction similar to the method for food protein-induced allergic proctocolitis (FPIAP) suggested by Uncuoglu et al (Table 3).29 This process involves introduction of common FPIES culprits first like milk and egg, followed by more atypical FPIES triggers like fruits and vegetables.
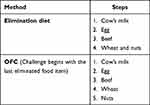 |
Table 3 Step-Wise Approach to Elimination Diets and OFCs29 |
A food challenge is conducted when there is uncertainty regarding the culprit food.30 Challenges should be performed in a medical setting under physician supervision due to the possibility of severe symptoms.30 Many different protocols for FPIES exist, however, the optimal protocol has yet to be established.31 The suggested dose of the challenge food being administered is 0.3 g food protein per kg of body weight (range 0.06–0.6 g).26 It is also suggested that 3 g food protein, 10 g total food, or 100 mL liquid should not be exceeded.26 Three equal doses of the cumulative serving size may be administered over a period of 30 min and patients should be observed 4–6 hr after ingestion.30 Smaller starting doses and/or longer periods of observation may be considered more appropriate for patients with a history of severe symptoms.30 If a very low starting dose is used and tolerated, a second full dose may be offered 2–3 hr after initial feeding, followed by a 4-hr observation period.30 Since most reactions occur 1 hr after ingestion, it is difficult to attribute the severity of the reaction to three equal doses within the suggested 30-min period. Therefore, some physicians have proposed feeding with 25% of the total dose (0.3 g protein/kg body weight) followed by a full dose 4 hr later if no reaction occurred.11 Similarly, a starting dose 33% of the total dose has been suggested, however, neither protocol has been systematically tested.32,33 In patients with allergic sensitization, dosing should follow guidelines for IgE-mediated food allergy.30 The suggested dosing should be altered to reflect guidelines for IgE-mediated food for patients with evidence of allergic sensitization.30 However, this must be done with the extended observation period of FPIES challenges.30
If a reaction occurs during an OFC, administration of normal saline fluid bolus (20 mL/kg) is recommended if IV access is present. This may be given in conjunction with IV ondansetron (0.15 mg/kg, max dose 16 g) in patients older than 6 months. For a mild reaction, oral rehydration at home may be appropriate.34 International evidence-based guidelines state that OFCs should be conducted in a medical facility equipped for fluid resuscitation, however, this is frequently debated.7,30,35,36 The recommendation was put forward as a cautionary measure due to the risk of dehydration and hypotension as 45%–95% of published OFCs were treated with IV, steroids, or both.26,30,37 An estimated 15% of patients develop severe reactions with hypotension.5 Patients who are more likely to need IV access are younger and have a history of more severe reactions.32,35 Many institutions adhere to this recommendation, however, access may be difficult and painful for patients or stressful for caregivers.30 Additionally, dehydration, a known risk for difficult peripheral venous access, may complicate IV administration, which could delay treatment and increase risk of infection and infiltration after multiple IV attempts. Thus, the cost of treatment would increase owing to more staff time and equipment and it may cause more stress to the patient. Therefore, IV rehydration following an OFC should be considered a high-risk procedure.35 Due to the unpredictability of reaction severity, home OFC is not recommended.38 Recent data suggest a possible trend towards less intravenous treatment given the possibility of intramuscular or oral ondansetron.30 Ultimately, IV access may depend on the severity of past reactions. IV access in infants with CM-FPIES or soy-FPIES challenged before 12 months may be strongly recommended as it has been observed that the shorter time since initial reaction, the more likely a moderate-to-severe reaction following OFC.35 It can be recommended for patients with a history of severe symptoms after low doses or those who required IV resuscitation or prolonged hospitalization.38 For mild risk, it can be performed in an outpatient setting with a plan for rapid transfer to an emergency setting.30,38
Differential Diagnosis (Table 4)
Due to the presentation of nonspecific gastrointestinal symptoms, FPIES diagnosis may be challenging.39 The differential diagnosis includes the following: idiopathic cyclic vomiting syndrome, gastrointestinal disorders (including severe surgical disorders such as malrotation), and extraintestinal disorders (including serious surgical and metabolic disorders such as fatty acid oxidation disorder).40 In acute presentations, FPIES may mimic sepsis, other infectious diseases, acute gastrointestinal episodes, surgical emergencies, and food allergies.39 In chronic presentations, FPIES may resemble malabsorption syndromes, metabolic disorders, primary immunodeficiencies, neurological conditions, coagulation defects, and other types of non-IgE mediated food allergy.39
 |
Table 4 Differential Diagnosis and Clinical History |
Differential Diagnosis of Acute FPIES
Patients with acute FPIES are often misdiagnosed with sepsis when presenting at an emergency room, which may lead to immediate treatment for the wrong disease.41 Acute FPIES and sepsis share similar onset symptoms including weakness, vomiting, hyperpnea, tachycardia, neurological impairment, oliguria, and hypotension.39 The second most commonly reported differential diagnosis is acute dehydration, which is caused by gastroenteritis.5 This condition typically manifests with fever and begins with vomiting, which typically progresses to diarrhea.39 Fever is not a common symptom of FPIES, and stool studies will present as negative.39 Furthermore, FPIES in neonates has been reportedly associated with a potential differential diagnosis of necrotizing enterocolitis, which manifests as instability, lethargy, vomiting, diarrhea, and acidosis.39 Diagnosis is mainly based on symptoms occurring in premature babies and supporting imaging.39 Creating a distinction between FPIES and necrotizing enterocolitis is crucial as the management approaches required for each condition differ.39
Differential Diagnosis of Chronic FPIES
Celiac disease also came into differential diagnosis with FPIES in some cases.39 Common symptoms associated with celiac disease include diarrhea, abdominal distention, short stature, anemia, and developmental delay.39 Some of these symptoms also manifest in patients who present with chronic forms of FPIES.39 Furthermore, chronic FPIES can be difficult to recognize, especially due to the trigger food being consumed freely by the infant, which leads to a prolonged diagnostic journey.39
Management
Acute and Chronic FPIES management
In the event of an acute FPIES reaction, whether from an accidental exposure or positive OFC, the most pressing risks are dehydration and, in some cases, hypovolemic shock. For patients with mild symptoms defined by 1–2 episodes of emesis and no/mild lethargy, oral rehydration by breastfeeding or formula for infants and clear liquids for older children is recommended.38,42 Patients receiving treatment for a mild reaction should seek medical attention if lethargic, floppy/hypotonic, or hypothermic.7,26 If the patient is older than 6 months and experiencing a mild reaction, ondansetron, a 5-HT3 receptor antagonist, may be recommended.7,26,30,38,43 Ondansetron has an antiserotoningergic effect that may play a role in gut secretion and motility through the nervous pathway.42,43 It appears to reduce severity of frequency of profuse vomiting in acute mild-moderate FPIES, but must be avoided in patients with a history of heart defects/arrhythmia. Use of ondansetron is debated, however, a prescription for oral ondansetron is recommended for at-home reactions considering its effectiveness in reducing emesis and its safety profile when administered orally in healthy children.42 In the event of such a reaction, a first dose should be administered in conjunction with oral rehydration at the first sign of symptoms and repeat if vomiting occurs within 10 min of the first dose until a medical setting is reached.30,42
For patients experiencing a severe reaction, characterized by >3 episodes of emesis with mild/severe lethargy, hypotonia, pallor, or cyanotic appearance, the priority is restoration of stable hemodynamics through aggressive isotonic fluid resuscitation (ex: 10–20 mL/kg boluses of normal saline repeated as necessary and dextrose saline as a continuous intravenous maintenance infusion).26,42 International Consensus guidelines published in 2017 recommend the use of corticosteroids (methylprednisolone 1 mg/kg (max 60–80 mg)) to reduce presumed cell-mediated inflammation during a reaction.26,30,44 However, no studies have established the use of corticosteroids. Intramuscular or intravenous ondansetron administration is recommended to reduce the severity of profuse vomiting. A study by Sopo et al compared parenteral ondansetron with traditional therapy (intravenous fluids and methylprednisolone [1 mg/kg]) and found that only 19% of children treated with ondansetron continued vomiting compared with 93% of children treated traditionally.45 In the most severe cases, electrolyte repletion, sodium bicarbonate for metabolic acidemia, and methylene blue for methemoglobinemia can be given.26,30,38
In cases of chronic FPIES management involves mainly elimination diets. A reaction can be expected to resolve in 4–12 hr (for acute FPIES) or 3–10 days (for chronic FPIES) after discontinuing the trigger food.24 Elimination diets are recommended for managing both acute and chronic cases of FPIES (Table 1).26
Dietary Management and Assessment of Tolerance
Although the median age of tolerance acquisition varies by food trigger, ~60% of patients acquire tolerance by the age 5 years. Most patients with FPIES to CM acquire by age 3 years, while the median ages of resolution for fish-FPIES range from 37 months to 7 years.12 Until tolerance is acquired, avoidance of the food trigger is recommended. Patients do not need to avoid any foods with precautionary allergen labeling (ie: labeled as may contain the trigger food) unless there is a history of severe reaction to minute amounts.24,26 However, avoidance of cooked/baked forms of the food trigger (eg: baked milk or egg) is recommended unless the baked form is already tolerated. There is no compelling data to support whether baked forms should be challenged for tolerance.24,26 A successful elimination diet is determined by food availability, family resources, caregivers cooking skills, the number of allergens to avoid and diet duration.42
For infants with CM-FPIES, continued breast milk is recommended. The maternal diet does not need to be restricted to eliminate the infant’s allergens as reactions through breast milk are rare.26,30,36 If uncertain, a supervised OFC with breast milk can be conducted.30 If feeding by breast milk is not possible, a hypoallergenic formula is recommended. Most infants tolerate an extensively hydrolyzed formula, however, approximately 10–20% of infants may still react and require transition to an amino acid-based formula (ie: elemental formula).24,26,30,34,42 For children with CM-FPIES or soy-FPIES, avoidance of both foods is recommended because of co-allergies in several countries, especially the United States.26,34 Since the usual age of FPIES presentation overlaps with early stages of weaning (4–6 months), infants with CM-FPIES or soy-FPIES should be gradually introduced to new foods since these patients have a significant risk of having solid-food-FPIES.26,34,42 During the first year of life, the child can progressively be introduced to all foods, according to their requirements and taste as well as familial and cultural habits with the aim of preventing aversive eating behaviour. Low-risk foods such as fruits and vegetables can be introduced first, followed by meat and cereal grains. Introduction of grains, rice, and fish, which are associated with high risk of atypical-FPIES should be done with high caution. These foods should be introduced as single ingredients, waiting at least a few days before introducing another.24,34,37,42 Tolerance to a food from one group increases the likelihood of tolerance to all food from that group.24 Oral food challenges are most often performed to test for the acquisition of tolerance.30 Re-introduction to a trigger food is often conducted 12–18 months after initial presentation. To help determine the course of elimination diets and OFCs in order to assess tolerance, a step-wise approach to food introduction by Uncuoglu et al may be employed, as previously mentioned for the diagnosis of FPIES (Table 3).29
Counseling for dietary management and consultation with a dietitian is highly recommended as the impact of an FPIES restrictive diet on growth has been well observed in both IgE- and non-IgE-mediated food allergy. FPIES patients should therefore be assessed for weight, stature, and where appropriate, head circumference to inform dietary management and provide feeding guidance.36 The psychosocial impact on parents has been observed to increase anxiety, stress, and worry, which negatively impacts the introduction and expansion of nutritious solid foods in children with FPIES. This delay may also lead to missing oral-motor and behavioral milestones essential in developing normal eating habits, which further increases the risk of feeding difficulties and consequently, growth. If the patient experiences any micronutrient deficiency, the cause should be addressed and corrected with supplementation.30,36,42
From the parents’ and adult patients’ perspective support and awareness of FPIES is insufficient. Awareness of FPIES among physicians and medical students has increased since the publication of the International Consensus Guidelines in 2017, however, lack of knowledge of FPIES may still delay diagnosis. A recent survey of patients’ parents and adult patients also identified that lack of support for FPIES management, increased financial burden associated with medical care, fear of reactions and introduction to new foods, are all significant sources of anxiety. Many survey respondents stated that difficulties associated with FPIES management have an effect in social situations such as eating out or attending school activities. Parents and patients also expressed a need for FPIES support groups to aid in management of anxiety and social restrictions associated with FPIES management. Finally, easily accessible resources such as specialized centers, access to a dietitian, and appropriately supervised food challenges were recommended.33
Future Perspectives
Despite advancements in understanding and diagnosing FPIES, there are substantial knowledge gaps that need to be addressed. Due to insufficient epidemiological data, the true prevalence of FPIES is still unknown. Population-based studies are also required to ascertain the incidence and prevalence of FPIES in various populations and age groups. Research should also concentrate on determining the risk factors for FPIES and comprehending the regional and environmental variations in the prevalence of particular food triggers.24 Future research on FPIES will emphasize advancing diagnostic methods, comprehending the disease’s underlying mechanisms, and creating successful treatment plans. Valid diagnostic tools and biomarkers are required to assist in the precise and prompt diagnosis of FPIES and potentially replace the need for food challenges. Future studies should also assess tolerance and determine the best procedures for carrying out OFCs.5,30 Furthermore, there are knowledge gaps regarding the precise pathogenic mechanisms underlying FPIES. Future studies should clarify the immune pathways, including the functions of innate and adaptive immune responses, which contribute to the development of FPIES. Understanding the causes, mechanisms, and factors influencing the switch from non-IgE to IgE-mediated allergy in atypical FPIES can help better understand this condition’s pathogenesis.7,24 Finally, more research is required to comprehend the long-term effects and natural history of FPIES. The prognosis and potential factors influencing the persistence or resolution of the condition can be learned from longitudinal studies that follow the development and resolution of FPIES over time, especially in different age groups. Clinical management and counseling for people with FPIES can be guided by understanding the factors that contribute to the development of tolerance to trigger foods and the chance of later developing other allergic conditions.46
Disclosure
The authors report no conflicts of interest in this work.
References
1. Tuck CJ, Biesiekierski JR, Schmid-Grendelmeier P, Pohl D. Food Intolerances. Nutrients. 2019;11(7):1684. doi:10.3390/nu11071684
2. Gargano D, Appanna R, Santonicola A, et al. Food allergy and intolerance: a narrative review on nutritional concerns. Nutrients. 2021;13(5):1638. doi:10.3390/nu13051638
3. Boyce JA, Assa’ad A, W Burks A, et al. Guidelines for the diagnosis and management of food allergy in the United States: report of the NIAID-sponsored expert panel. J Allergy Clin Immunol. 2010;126(6 Suppl):S1–58. doi:10.1016/j.jaci.2010.10.007
4. Muraro A, Werfel T, Hoffmann-Sommergruber K, et al. EAACI food allergy and anaphylaxis guidelines: diagnosis and management of food allergy. Allergy. 2014;69(8):1008–1025. doi:10.1111/all.12429
5. Leonard SA, Pecora V, Fiocchi AG, Nowak-Wegrzyn A. Food protein-induced enterocolitis syndrome: a review of the new guidelines. World Allergy Organ J. 2018;11(1):4. doi:10.1186/s40413-017-0182-z
6. Pudasainee P. Protein Intolerance. Treasure Island (FL): StatPearls Publishing; 2023.
7. Nowak-Wegrzyn A, Berin MC, Mehr S. Food protein-induced enterocolitis syndrome. J Allergy Clin Immunol Pract. 2020;8(1):24–35. doi:10.1016/j.jaip.2019.08.020
8. Hwang JB. Is this symptom even a food allergy?: clinical types of food protein-induced enterocolitis syndrome. Pediatr Gastroenterol Hepatol Nutr. 2014;17(2):74–79. doi:10.5223/pghn.2014.17.2.74
9. Öhlund M, Liljeholm S, Strinnholm Å, Winberg A. Food protein-induced enterocolitis syndrome among children in northern Sweden—A retrospective review from 2004–2018. Acta Paediatrica. 2023;112(7):1558–1564. doi:10.1111/apa.16741
10. Caubet JC, Ford LS, Sickles L, et al. Clinical features and resolution of food protein-induced enterocolitis syndrome: 10-year experience. J Allergy Clin Immunol. 2014;134(2):382–389. doi:10.1016/j.jaci.2014.04.008
11. Calvani M, Anania C, Bianchi A, et al. Update on Food protein-induced enterocolitis syndrome (FPIES). Acta Biomed. 2021;92(S7):e2021518. doi:10.23750/abm.v92iS7.12394
12. Prattico C, Mulé P, Ben-Shoshan M. A systematic review of food protein-induced enterocolitis syndrome. Int Arch Allergy Immunol. 2023;184(6):567–575. doi:10.1159/000529138
13. Blackman AC, Anvari S, Davis CM, Anagnostou A. Emerging triggers of food protein-induced enterocolitis syndrome: lessons from a pediatric cohort of 74 children in the United States. Ann Allergy Asthma Immunol. 2019;122(4):407–411. doi:10.1016/j.anai.2019.01.022
14. Hwang JB, Sohn SM, Kim AS. Prospective follow-up oral food challenge in food protein-induced enterocolitis syndrome. Arch Dis Child Jun. 2009;94(6):425–428. doi:10.1136/adc.2008.143289
15. Tan JA, Smith WB. Non-IgE-mediated gastrointestinal food hypersensitivity syndrome in adults. J Allergy Clin Immunol Pract. 2014;2(3):355–7.e1. doi:10.1016/j.jaip.2014.02.002
16. Du YJ, Nowak-Węgrzyn A, Vadas P. FPIES in adults. Ann Allergy Asthma Immunol. 2018;121(6):736–738. doi:10.1016/j.anai.2018.08.003
17. Gonzalez-Delgado P, Caparrós E, Moreno MV, Cueva B, Fernández J. Food protein-induced enterocolitis-like syndrome in a population of adolescents and adults caused by seafood. J Allergy Clin Immunol Pract. 2019;7(2):670–672. doi:10.1016/j.jaip.2018.07.028
18. Goswami R, Blazquez AB, Kosoy R, et al. Systemic innate immune activation in food protein-induced enterocolitis syndrome. J Allergy Clin Immunol. 2017;139(6):1885–1896.e9. doi:10.1016/j.jaci.2016.12.971
19. Nowak-Wegrzyn A, Warren CM, Brown-Whitehorn T, Cianferoni A, Schultz-Matney F, Gupta RS. Food protein-induced enterocolitis syndrome in the US population-based study. J Allergy Clin Immunol. 2019;144(4):1128–1130. doi:10.1016/j.jaci.2019.06.032
20. Katz Y, Goldberg MR, Rajuan N, Cohen A, Leshno M. The prevalence and natural course of food protein-induced enterocolitis syndrome to cow’s milk: a large-scale, prospective population-based study. J Allergy Clin Immunol. 2011;127(3):647–53.e1–3. doi:10.1016/j.jaci.2010.12.1105
21. Nowak-Węgrzyn A, Katz Y, Mehr SS, Koletzko S. Non-IgE-mediated gastrointestinal food allergy. J Allergy Clin Immunol. 2015;135(5):1114–1124. doi:10.1016/j.jaci.2015.03.025
22. Zhang S, Sicherer S, Berin MC, Agyemang A. Pathophysiology of Non-IgE-Mediated Food Allergy. Immunotargets Ther. 2021;10:431–446. doi:10.2147/itt.S284821
23. Leonard SA, Nowak-Węgrzyn A. Food protein-induced enterocolitis syndrome: an update on natural history and review of management. Ann Allergy Asthma Immunol. 2011;107(2):95–101; quiz 101, 162. doi:10.1016/j.anai.2011.06.004
24. Agyemang A, Nowak-Wegrzyn A. Food protein-induced enterocolitis syndrome: a comprehensive review. Clin Rev Allergy Immunol. 2019;57(2):261–271. doi:10.1007/s12016-018-8722-z
25. Ludman S, Harmon M, Whiting D, du Toit G. Clinical presentation and referral characteristics of food protein-induced enterocolitis syndrome in the United Kingdom. Ann Allergy Asthma Immunol. 2014;113(3):290–294. doi:10.1016/j.anai.2014.06.020
26. Nowak-Węgrzyn A, Chehade M, Groetch ME, et al. International consensus guidelines for the diagnosis and management of food protein-induced enterocolitis syndrome: executive summary-workgroup report of the adverse reactions to foods committee, American Academy of allergy, asthma & immunology. J Allergy Clin Immunol. 2017;139(4):1111–1126.e4. doi:10.1016/j.jaci.2016.12.966
27. Weinberger T, Feuille E, Thompson C, Nowak-Węgrzyn A. Chronic food protein-induced enterocolitis syndrome: characterization of clinical phenotype and literature review. Ann Allergy Asthma Immunol. 2016;117(3):227–233. doi:10.1016/j.anai.2016.03.004
28. Gleich GJ, Sebastian K, Firszt R, Wagner LA. Shrimp allergy: gastrointestinal symptoms commonly occur in the absence of IgE sensitization. J Allergy Clin Immunol Pract. 2016;4(2):316–318. doi:10.1016/j.jaip.2015.09.020
29. Uncuoğlu A, Aydoğan M, Şimşek IE, Çöğürlü MT, Uçak K, Acar HC. A prospective assessment of clinical characteristics and responses to dietary elimination in food protein–induced allergic proctocolitis. J Allergy Clin Immunol. 2022;10(1):206–214.e1. doi:10.1016/j.jaip.2021.10.048
30. Baker MG, Cecilia Berin M, Sicherer S. Update on Food Protein-Induced Enterocolitis Syndrome (FPIES). Curr Allergy Asthma Rep. 2022;22(10):113–122. doi:10.1007/s11882-022-01037-y
31. Nicolaides R, Bird JA, Cianferoni A, Brown-Whitehorn T, Nowak-Wegrzyn A. Oral food challenge for FPIES in practice-a survey: report from the work group on FPIES within the adverse reactions to foods committee, FAED IS, AAAAI. J Allergy Clin Immunol Pract. 2021;9(10):3608–3614.e1. doi:10.1016/j.jaip.2021.06.061
32. Feuille E, Nowak-Wegrzyn A. Medical algorithms: recognizing and treating food protein-induced enterocolitis syndrome. Allergy. 2019;74(10):2019–2022. doi:10.1111/all.13857
33. Vazquez-Ortiz M, Khaleva E, Mukherjee S, et al. Challenges and unmet needs in FPIES from the parents and adult patients’ perspective: an international survey. J Allergy Clin Immunol Pract. 2023;11(4):1306–1309.e2. doi:10.1016/j.jaip.2022.12.017
34. Bird JA, Barni S, Brown-Whitehorn TF, et al. Food protein-induced enterocolitis syndrome oral food challenge: time for a change? Ann Allergy Asthma Immunol. 2021;126(5):506–515. doi:10.1016/j.anai.2021.02.022
35. Ford LS, Konstantinou GN, Caubet J-C. PRO: peripheral intravenous access should always be secured before initiating food protein-induced enterocolitis syndrome oral food challenge. Ann Allergy Asthma Immunol. 2021;126(5):460–461. doi:10.1016/j.anai.2021.01.021
36. Groetch M, Durban G, Meyer R, Venter C, Muraro A, Muraro A. The practical dietary management of food protein-induced enterocolitis syndrome. Ann Allergy Asthma Immunol. 2021;127(1):28–35. doi:10.1016/j.anai.2021.03.007
37. Mehr S, Campbell DE. Food protein-induced enterocolitis syndrome: guidelines summary and practice recommendations. Med J Aust. 2019;210(2):94–99. doi:10.5694/mja2.12071
38. Leonard SA, Miceli Sopo S, Baker MG, et al. Management of acute food protein-induced enterocolitis syndrome emergencies at home and in a medical facility. Ann Allergy Asthma Immunol. 2021;126(5):482–488.e1. doi:10.1016/j.anai.2021.01.020
39. Fiocchi A, Claps A, Dahdah L, Brindisi G, Dionisi-Vici C, Martelli A. Differential diagnosis of food protein-induced enterocolitis syndrome. Curr Opin Allergy Clin Immunol. 2014;14(3):246–254. doi:10.1097/aci.0000000000000057
40. Li BU, Balint JP. Cyclic vomiting syndrome: evolution in our understanding of a brain-gut disorder. Adv Pediatr. 2000;47:117–160.
41. Järvinen KM, Nowak-Węgrzyn A. Food protein-induced enterocolitis syndrome (FPIES): current management strategies and review of the literature. J Allergy Clin Immunol Pract. 2013;1(4):317–322. doi:10.1016/j.jaip.2013.04.004
42. Mastrorilli SA, Procaccianti C, Pagliaro M, Caffarelli G. New insights into food protein-induced enterocolitis in children. Minerva Pediatr. 2020;72(416):23.
43. Michelet M, Schluckebier D, Petit LM, Caubet JC. Food protein-induced enterocolitis syndrome - a review of the literature with focus on clinical management. J Asthma Allergy. 2017;10:197–207. doi:10.2147/jaa.S100379
44. Khanna N, Patel K. FPIES: reviewing the management of food protein-induced enterocolitis syndrome. Case Rep Pediatr. 2016;2016:1621827. doi:10.1155/2016/1621827
45. Vila Sexto L. Latest insights on food protein-induced enterocolitis syndrome: an emerging medical condition. J Investig Allergol Clin Immunol. 2018;28(1):13–23. doi:10.18176/jiaci.0192
46. Li DH, Wong-Pack A, Macikunas AL, Kim H. Adults with possible food protein-induced enterocolitis syndrome with crustacean ingestion. Allergy Asthma Clin Immunol. 2020;16(1):99s. doi:10.1186/s13223-020-00497-z
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
