Back to Journals » Infection and Drug Resistance » Volume 17
Development of a Risk Prediction Model for Infection After Kidney Transplantation Transmitted from Bacterial Contaminated Preservation Solution
Authors Guo M, Pan C, Zhao Y, Xu W, Xu Y, Li D, Zhu Y, Cui X
Received 8 November 2023
Accepted for publication 3 March 2024
Published 13 March 2024 Volume 2024:17 Pages 977—988
DOI https://doi.org/10.2147/IDR.S446582
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Professor Suresh Antony
Mingxing Guo,1,* Chen Pan,1,* Ying Zhao,1 Wanyi Xu,1 Ye Xu,1 Dandan Li,1 Yichen Zhu,2 Xiangli Cui1
1Department of Pharmacy, Beijing Friendship Hospital, Capital Medical University, Beijing, People’s Republic of China; 2Department of Urology, Beijing Friendship Hospital, Capital Medical University, Beijing, People’s Republic of China
*These authors contributed equally to this work
Correspondence: Xiangli Cui, Department of Pharmacy, Beijing Friendship Hospital, Capital Medical University, Beijing, People’s Republic of China, Email [email protected] Yichen Zhu, Department of Urology, Beijing Friendship Hospital, Capital Medical University, Beijing, People’s Republic of China, Email [email protected]
Background: The risk of transplant recipient infection is unknown when the preservation solution culture is positive.
Methods: We developed a prediction model to evaluate the infection in kidney transplant recipients within microbial contaminated preservation solution. Univariate logistic regression was utilized to identify risk factors for infection. Both stepwise selection with Akaike information criterion (AIC) was used to identify variables for multivariate logistic regression. Selected variables were incorporated in the nomograms to predict the probability of infection for kidney transplant recipients with microbial contaminated preservation solution.
Results: Age, preoperative creatinine, ESKAPE, PCT, hemofiltration, and sirolimus had a strongest association with infection risk, and a nomogram was established with an AUC value of 0.72 (95% confidence interval, 0.64– 0.80) and Brier index 0.20 (95% confidence interval, 0.18– 0.23). Finally, we found that when the infection probability was between 20% and 80%, the model oriented antibiotic strategy should have higher net benefits than the default strategy using decision curve analysis.
Conclusion: Our study developed and validated a risk prediction model for evaluating the infection of microbial contaminated preservation solutions in kidney transplant recipients and demonstrated good net benefits when the total infection probability was between 20% and 80%.
Keywords: risk prediction model, kidney transplant, nomogram, risk factors
Introduction
Due to the need for immunosuppressive therapy used for avoiding graft rejection, infection in the post-transplant period represents a major cause of in-hospital morbidity and mortality among solid organ transplantation (SOT) recipients, especially in the first month after transplantation.1,2 Immediately post-transplant infections are usually derived from the donor, recipient, or technical complications of surgery.3 Transmission of pathogens via preservation solution (PS) is a potential route for donor-derived infections (DDIs) in the early stage after transplantation.4 However, the relationship between microbial contamination in PS and infection events has not been determined, as most infections are not caused by donors.5–7 According to reports, the incidence of preservation solution contamination can reach up to 77.8% in deceased-donor kidney transplant (KT) recipients.8 Although contamination of the PS of donated organs is frequent, the incidence of PS-related infection is relatively low (10%, 95% CI: 7% to 15%).9 Contamination of PS during procurement seemed to be the major mechanism.10 Therefore, in the case of positive PS cultures, the infectious risk for recipients is unknown.
In the case of positive PF cultures, there is no consensus for prescribing prophylactic antibiotics. Previous studies have shown that in cases when PS bacterial culture in kidney transplantation is positive, the frequency of antibiotic prescription was high, and there are significant differences among respondents, leading to significant uncertainty in decision-making.11 A systematic review and meta-analysis showed that there were differences in the rates of infections due to pathogenic microorganisms between SOT recipients who received pre-emptive treatment and those who did not, but without statistical significance.9 So far, the benefits of using prophylactic antibiotics for systemic treatment have not been confirmed, but this may have a significant impact on the selection of multidrug-resistant bacteria in kidney transplant recipients. Therefore, in the case of contaminated preservation solutions, it is necessary to identify potential infected recipients and develop targeted antibiotic prevention strategies to prevent all recipients from indiscriminately receiving or not receiving antibiotic prevention strategies.
Our study aimed to develop a risk prediction model for infection of deceased-donor kidney transplant recipients after microbial contamination of preservation solution, as well as provide reference for individualized use of antibacterials in deceased-donor kidney transplant recipients.
Methods
Study Design and Data Sources
The protocol was approved by the Ethics Committee of Beijing Friendship Hospital and was conducted in accordance with the principles of the Declaration of Helsinki (2022-P2-358-01). Based on the use of medical records obtained from previous clinical diagnosis and treatment, the privacy and personal identity information of the subjects were protected, and it was difficult to contact patients to sign informed consent forms, resulting in significant waste of human and material resources. The research project did not involve personal privacy and commercial interests. This retrospective study applied to the Ethics Committee for an exemption from informed consent and was approved. All kidneys were donated voluntarily with written informed consent and the transplants were conducted in accordance with the Declaration of Istanbul. This retrospective single-center study included 484 deceased-donor renal transplant recipients from the Beijing Friendship Hospital affiliated with Capital Medical University between June 1, 2019, to June 30, 2022. Among them, 171 deceased-donor kidney transplant recipients with contaminated preservation solutions were collected for subsequent clinical data collection. All recorded infection events occurred during the hospitalization period of the transplant surgery. Recipients were monitored for microbial infections in the blood, urine, and drainage fluid for the first 7 days post-transplant.
Definition
Bloodstream infection (BSI) is defined according to the Centers for Disease Control and Prevention guidelines (available at: http://www.cdc.gov/nhsn/pdfs/pscmanual/17pscnosinfdef_current.pdf). Bacteraemia was considered when any bacterial species was found in bloodstream samples. ESKAPE pathogens were enterococcus faecium, staphylococcus aureus, Klebsiella pneumoniae, Acinetobacter baumannii, Pseudomonas aeruginosa, and Enterobacter spp. Delayed graft function (DGF) was defined as a decrease in the daily serum creatinine by less than 10% for three consecutive days during the first week after KT or serum creatinine failed to decrease to 400 mmol/L within the first postoperative week. Abnormal liver function was defined as increased levels of alanine and aspartate aminotransferase, gamma glutamyltransferase, alkaline phosphatase, and total bilirubin. A graft-site infection was defined as patients having positive microbiological results in peri-renal allograft fluid collections (obtained by puncture or surgery). Infection after transplantation is defined as isolation of any microorganism from a clinically relevant sample obtained under sterile conditions. Infection related to preservation solution (I-PS) was defined when the pathogenic microorganisms in the infectious episodes were the same as the microbial strains cultured in the PS and had the same antibiotic susceptibility profiles.
Microbiological Analysis
Pathogen isolation and culture were carried out based on the National Clinical Testing Protocols (China), and suspected strains were identified using a VITEK 32 automated microbial analyzer (BioMerieux, Craponne, France). Drug susceptibility was detected using the minimum inhibitory concentration (MIC) and disk diffusion method (Oxoid Ltd, UK) and were interpreted in reference to the Clinical and Laboratory Standards Institute (CLSI, 2018).
Immunosuppressive Therapy
The typical immunosuppressive induction therapy regimen was methylprednisolone (1000 mg of methylprednisolone was intravenously infused on the operation day; 500 mg on the first and second days after KT, respectively) and basiliximab (20 mg of basiliximab administered during operation and fourth day after surgery). For kidney transplant recipients with a high risk of rejection, 1.5–2.0 mg × kg−1 × d−1 of rabbit antihuman thymocyte immunoglobulin (ATG) with the administration of methylprednisolone was administered for 3–5 days after KT. The routine triple maintenance immunosuppressive regimen was a composite of oral tacrolimus (or cyclosporine A), mycophenolate mofetil (MMF), and prednisone.
Infection Prophylactic Protocol
A 2 g ceftazidime q12h or cefzoxime q12h regimen was routinely administered to recipients who received deceased donor kidney transplantation. If the doctor considered the recipient to have a high-risk factor for multidrug-resistant bacterial infection before kidney transplantation, such as a history of ICU infection or infection in other parts of the donor, the prophylactic antibiotic for the subject was meropenem 1g q12h. Antibiotics were discontinued after 7–8 days post-transplant if patients had no symptoms of infection or normal laboratory parameters of infection were observed. The antimicrobial therapy could be modified according to the resistance profile of the microorganisms identified in the donors’ and recipients’ specimens and the PS. The antibiotics regimen dosage was adjusted according to kidney function. When patients had fever or confirmed bacterial infection in combination with test indicators, targeted antimicrobial therapy was initiated. In addition, blood, urine, and abdominal drainage fluid were collected for microbiological analysis. Prophylactic antifungal protocol with caspofungin or micafungin was employed on day seven after KT.
Clinical Data Collection
The patients’ demographic and clinical characteristic data were reviewed from the electronic medical record system. Data analyzed for cases and controls included the subjects’ baseline characteristics (sex, age, and BMI), comorbidities (diabetes mellitus, hypertension, anemia, myocardial infarction, and HBsAg), smoking, primary nephrosis, types of dialysis (hemodialysis and peritoneal dialysis), length of dialysis time, repeated re-transplant, preoperative ALB, preoperative creatinine ≥ 1000 µmol/L or not, antibacterial drugs for prevention (meropenem and ceftazidime/cefzoxime), pathogens (ESKAPE and fungus), drug intervention, laboratory findings (creatinine, WBC, GR, LY, Hgb, PLT, PCT, ALT, and AST), clinical symptoms and outcomes (fever, rejection, DGF, bleeding, blood transfusion, hemofiltration, and transfer to ICU), and immunosuppressive drugs (rabbit anti-human thymocyte immunoglobulin, sirolimus, and mizoribine).
Statistical Analysis
The continuous variables conforming to normal distribution were expressed as the mean ± standard deviation (SD), and the independent t-test was used for inter-group comparison. Non-normally distributed continuous variables were presented as the median (interquartile range), and groups were compared using the Mann–Whitney U-test. Categorical variables were expressed as number (percentage) and analyzed using the χ2 test or Fisher’s exact test.
The initial predictors were selected based on the reported literature and the data available to us. To identify risk factors for infection, univariate logistic regression was utilized and variables with a P-value of <0.2 and of clinical importance were included in the initial multivariate logistic regression model for analysis. Both stepwise selection with Akaike information criterion (AIC) was used to identify variables for multivariate logistic regression. Selected variables were incorporated in the nomograms to predict the probability of infection for deceased-donor kidney transplant recipients after microbial contamination of PS. The regression coefficients were applied to each individual observation to define a linear predictor.
The performance of prediction models was evaluated by discrimination ability and calibration. Model discrimination – the ability of the models to differentiate between patients who did or did not have infection – was evaluated with C-index (area under the curves [AUC]). A perfect model will have an AUC of 1 whereas a non-informative model will have an AUC of 0.5. Generally, an AUC of >0.7 indicates that the estimation is reasonable. Model calibration – the ability of the models to produce unbiased estimates of the probability of infection – was evaluated graphically with calibration plots (plots of observed versus predicted risk) and statistically by computing the Brier. Model discrimination and calibration measures were calculated using 1000-fold cross-validation bootstrap resampling to avoid bias.
Decision curve analysis (DCA) was used to evaluate the clinical benefit and practicability of the nomogram constructed using the selected variables. All data were analyzed using the R software (R Studio 3.6.3). An online prediction tool (Shiny App) was prepared using the DynNom package in R. All tests were 2 sided, and P < 0.05 was considered to be statistically significant.
Results
Patient Characteristics
A total of 484 deceased-donor kidney transplantation recipients were initially assessed, and 171 KT recipients within the contaminated PS were collected for follow-up clinical data. The positive rate of contaminated PS in deceased-donor kidney transplantation recipients was 35.33% (171/484). Among them, 69 cases of KT recipients developed infections after KT. The incidence of infection among the KT recipients within the contaminated PS was 40.35% (69/171). Only 18 cases were ultimately identified as I-PS. The incidence of I-PS among the KT recipients within the contaminated PS was 10.53% (18/171).
Demographic data and clinical details are displayed in Table 1. The median age of the patients who underwent KT within the contaminated PS was 44 years (IQR 34.5, 54), and 63.16% (108/171) of the patients were male. Overall, 5.85% (10/171) of the KT recipients were repeatedly re-transplanted. As for comorbidities, hypertension and anemia are the most common concomitant diseases, accounting for 95.96% (164/171) both, followed by diabetes mellitus and myocardial infarction, accounting for 16.37% (28/171) and 14.04% (24/171), respectively.
 |
Table 1 Characteristics of KT Within Microbial Contaminated Preservation Solution |
Characteristics of Pathogenic Bacteria in PS and Infection Sites
For strains repeatedly detected in the same part of the same patient, only one pathogen detected for the first time is included in the calculation of pathogen distribution. A total of 194 strains were detected in PS, and 85 strains were detected at the infection site after KT. The types of pathogenic bacteria retrieved from PS and infection site are shown in Figure 1. In the PS, the most common isolated pathogens were Klebsiella pneumoniae (27, 13.92%), staphylococcus epidermidis (25, 12.89%), and enterococcus faecium (24, 12.37%). At the infection site after KT, the main isolated pathogens were enterococcus faecium (12, 14.12%), Klebsiella pneumoniae (10, 11.76%), and staphylococcus haemolyticus (9, 10.59%).
Among the 18 cases ultimately identified as I-PS, possible pathogenic bacteria included Klebsiella pneumoniae (8, 44.44%), enterococcus faecium (5, 27.78%), enterococcus faecalis (2, 11.11%), candida tropicalis (1, 5.56%), candida parapsilosis (1, 5.56%), candida albicans (1, 5.56%).
Characteristics of Perioperative Infection in Kidney Recipients and Unfavorable Clinical Outcomes
The infection characteristics during the perioperative period of kidney transplantation are shown in Table 2. Surgical site infection (41, 59.42%) was the most frequent perioperative infection types, followed by urinary tract infection (36, 52.17%) and bloodstream infection (13, 18.84%). Similar results were presented in I-PS, as surgical site infection (14, 77.78%), urinary tract infection (11, 61.11%), and bloodstream infection (7, 38.89%).
 |
Table 2 Pathogenic Bacteria Characteristics and Unfavorable Clinical Outcomes of Kidney Transplantation |
Among 69 infected patients, 50 cases (72.46%) presented with single-focal infection. For the I-PS, 8 cases (44.44%) presented with single-focal infection and 10 cases (55.56%) presented with ≥2 types of infection.
Among all 69 perioperatively infected patients, 53 patients (76.81%) presented as single-pathogen infections, the other 16 patients (23.19%) presented as multi-pathogen infections. For the I-PS, 11 cases (61.11%) presented as single-pathogen infections, while remaining 7 patients (38.89%) presented as multi-pathogen infections. And 2 cases (11.11%) with four kinds of pathogenic bacteria infections were seen in perioperative infection group, which were also attributed to I-PS.
Of the 69 recipients infected with pathogens, one case died during the perioperative period of KT. This case was also an I-PS. The mortality rate of perioperative infection was 1.45%, and the mortality rate in I-PS was 5.56%. Among the 69 recipients infected with pathogens, abnormal liver function (34, 49.28%), diarrhea (24, 34.78%) and blood transfusion (19, 27.54%) were the most common clinical symptoms or outcomes. However, in I-PS, blood transfusion (5, 27.78%) and DGF (5, 27.78%) were the most common clinical symptoms or outcomes.
Univariate Analysis
To screen risk factors for perioperative infection, we performed univariate analysis of patients with and without infection among the contaminated PS after KT, as shown in Table 1. A total of 13 variables were identified as potential risk factors for infection after KT (P < 0.2): age (P=0.152), length of dialysis time (P=0.099), preoperative creatinine (P=0.099), ESKAPE (P=0.116), intervene (P=0.117), creatinine ≥ 400 ummo/L (P=0.056), LY (P=0.015), PCT (P=0.071), fever (P=0.031), DGF (P=0.057), blood transfusion (P=0.151), hemofiltration (P=0.057), and sirolimus (P=0.052). No potential risk signals of fungi were found in this univariate analysis. Fungal contamination in PS has been proven to be strongly associated with DDIs, such as Candida arteritis and subsequent graft loss or even death.12–14 In our analysis, there were fewer fungal cases, which might lead to the possibility of false negative. In order to ensure the rigor of the study, we finally included the fungal variables in the subsequent multivariate analysis.
Multivariate Logistic Regression Model
A total of 14 variables were selected as candidate variables for the calculation of the multivariate logistic regression model. Both stepwise selection using the AIC identified the following 6 variables that had the strongest association with infection risk (Table 3): age (P=0.12), preoperative creatinine (P=0.004), ESKAPE (P=0.083), PCT (P=0.15), hemofiltration (P=0.14), and sirolimus (P=0.036).
 |
Table 3 Final Multivariate Analysis for Predicting Risk of Perioperative Infection After Kidney Transplantation |
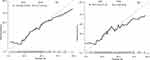
Nomogram and Performance
Nomogram to predict the risk of infection of deceased-donor kidney transplant recipients within contaminated PS is shown in Figure 2. The model showed acceptable discrimination and prediction accuracy for perioperative infection when assessed against the derivation AUC 72.0 (95% confidence interval [CI], 64.3–79.8), Brier index 20.3 (95% CI, 17.8–22.9), and bootstrapped validation datasets AUC 68.2 (95% CI, 59.8–77.6), Brier index 22.6 (95% CI, 19.6–26.6) (Figure 3). The model was designed to be used in the immediate peritransplant period when pathogenic bacteria were detected in the preservation solution, ideally from the day of transplantation up to 2–3 weeks after transplantation. According to the presence of such variables, the risk of infection of deceased-donor kidney transplant recipients after microbial contamination of preservation solution can be predicted (see examples in Figure 4 and mobile application at https://panda0219.shinyapps.io/dynnomapp/).
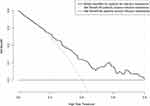
Finally, we explored the potential clinical utility of our model using a decision-curve analysis to examine the “net benefit” of applying the prediction model across a range of infection threshold probabilities (Figure 5). A theoretical risk-model guided strategy (ie, empiric administration of antibiotics) was compared against 2 default strategies: treat all and treat none. A model was only useful at a given disease threshold if it had a higher net benefit than treat all or treat none. Our analysis suggested that the model-directed interventions for infection of deceased-donor kidney transplant recipients after microbial contamination of preservation solution would show net benefit over default strategies when the overall infection threshold probability is between 20% and 80%.
Discussion
We developed and validated a risk prediction model for infection of deceased-donor kidney transplant recipients within microbial contaminated PS. We found that age, preoperative creatinine, ESKAPE, PCT, hemofiltration, and sirolimus were risk factors for perioperative infection after KT within microbial contaminated PS. To the best of our knowledge, our study is the first attempt to develop a risk prediction model of infection in kidney transplant recipients within microbial contaminated PS.
The overall incidence of contaminated PS in deceased-donor kidney transplantation recipients was 35.33% in our kidney transplantation center, which was consistent with a systematic review and meta-analysis among SOT recipients (37%, 95% CI: 27–49%).11 In our study, the incidence of I-PS was 10.53%, which was at a lower level compared to PS contamination. Data of I-PS were frequently available only during the immediate postoperative period. Antibacterial drugs for prevention were an opportunity for intervention, but the optimal antibiotic regimen is not known.15 Bertrand et al reported that the incidence of clinical complications from preservation solutions contamination was negligible.16 Nevertheless, some other research considered it to be a common cause of early post-transplantation infection.17,18 Given the high contamination of the PS and the severity of infection by the transplant recipient, changing the antibiotic prevention strategy or not changing the strategy for all recipients is not the optimal strategy when the preservation solution culture is positive. In our study, no matter whether meropenem or the third-generation cephalosporin (ceftazidime or cefzoxime) were chosen as the perioperative antibiotic, there was no significant difference between the postoperative infection group and the non-infection group (P=0.772, P=0.714). It is necessary to develop a decision support system for diagnosing infection in kidney transplant recipients within microbial contaminated PS, in order to guide the use of antibiotics. For recipients with high infection risk, targeted antibiotic prevention strategies can be implemented, while for recipients with low infection risk, we do not recommend changing prophylactic antibiotics regimen based on preservation solution results when the culture results of the samples sent by the recipients are still unknown. This can avoid unnecessary use of antibiotics and reduce the production of drug-resistant bacteria.
In our study, age, preoperative creatinine, ESKAPE, PCT, hemofiltration, and sirolimus were risk factors for perioperative infection after KT. We found that age increases the risk of infection. Previous studies had shown that older renal transplant recipients are at a high risk of infections due to immunosenescence, frailty, functional impairment and multiple comorbidities, and the risk of infectious death increases exponentially,19,20 which is consistent with our findings. The preoperative creatinine level indirectly reflected the patient’s pre-transplant status and became a risk factor for postoperative infection. In our study, recipients with preoperative creatinine greater than 1000 µmol/L had an increased risk of infection after kidney transplantation. Preoperative high creatinine often indicated insufficient dialysis, the patient’s body was not in good condition before kidney transplantation, immune function may be deficient, and the risk of postoperative infection was increased. A retrospective cohort study indicated that ESKAPE contamination was an independent risk factor associated with DDIs.8 Previous studies had proved that bacteraemia associated with ESKAPE pathogens is frequent in solid organ transplantation and that these organisms might induce significant morbidity and mortality.21 A retrospective single-center study showed that preemptive antibiotic therapy decreased the bloodstream infection rate when preservation fluid was positive for ESKAPE pathogens.6 Therefore, when the ESKAPE pathogen in the PS is positive, the risk of postoperative infection in recipients increases. Clinical doctors should immediately conduct infection risk assessments and actively adjust antimicrobial prevention plans for high-risk patients. Although PCT might be affected by renal function and immune components, PCT was still an important indicator of infection. It has been suggested that elevated serum PCT levels after 1 week of transplantation can indicate infectious complications, and monitoring PCT in the early post-transplant period is a favorable method for early tracking of infectious complications.22 The invasive operation of hemofiltration increases the risk of infection. In our study, hemofiltration is also one of the factors that needs to be considered for increasing the risk of infection. Sirolimus enriches the possibilities of immunosuppressive therapies after renal transplantation. Four lung transplant studies, three multicenter RCTs and one case control, evaluated replacing mycophenolate mofetil or azathioprine with either sirolimus or everolimus. Significantly lower rates of CMV, viral infections, and lower respiratory tract infections were observed, although these were secondary outcomes.23–26 Sirolimus can reduce the incidence of CMV virus and tumors,27,28 but the impact on bacterial infection needs further research.
In the case of contaminated preservation solutions, targeted antibiotic prevention strategies need to be developed to avoid all patients receiving or not receiving treatment indiscriminately. We established a nomogram to predict the risk of infection of deceased-donor kidney transplant recipients within contaminated PS. The model showed acceptable discrimination and prediction accuracy for perioperative infection when assessed against the derivation AUC 72.0 (95% CI, 64.3–79.8), Brier index 20.3 (95% CI, 17.8–22.9), and bootstrapped validation datasets AUC 68.2 (95% CI, 59.8–77.6), Brier index 22.6 (95% CI, 19.6–26.6). Prediction models were typically evaluated in terms of their accuracy and calibration. But it can be hard to know how high an AUC had to be in order to be “high enough” to warrant use of a prediction model, or how much miscalibration would be disqualifying. Decision curve analysis was developed as a method to determine whether use of a prediction model in the clinic to inform decision-making would do more good than harm.29 Therefore, we further use decision curve analysis to examine the “net benefit” of applying the prediction model across a range of infection threshold probabilities. Our analysis suggested that the model-directed interventions for infection of deceased-donor kidney transplant recipients after microbial contamination of preservation solution would show net benefit over default strategies when the overall infection threshold probability between 20% and 80%.
This study also had some limitations. First, this was a retrospective single-center study, and the validation was conducted with retrospective data. This might have generated biases, and the results are subjected to future prospective multicenter studies. Second, the sample size was relatively small to develop a classical risk prediction model, and the validation data sets were not independent samples, which may lead to the instability of our model. Thirdly, this predictive model was obtained through retrospective analysis by our center. Although the internal validation performed well, no external validation was conducted. Therefore, the next step is to collaborate with multiple centers to develop and improve the clinical feasibility of the predictive model for infection after kidney transplantation transmitted from bacterial contaminated preservation solution.
Conclusion
Our study developed and validated a risk prediction model for infection of deceased-donor kidney transplant recipients after microbial contamination of preservation solution and demonstrated good net benefits when the overall infection threshold probability between 20% and 80%. We made further efforts to build a brief website version of evaluation tool in order to produce a short, fast, and handy tool for assessing perioperative infection, which may provide a relatively practical tool for clinicians to identify patients with high-risk infection. For recipients with a high risk of infection, targeted antibiotic prevention strategies can be implemented immediately based on the results of PS culture. For recipients with a low risk of infection, antibiotic prevention strategies can be temporarily remain unchanged, waiting for the culture results of the samples sent by the recipients and continuing to observe the patient’s signs of infection. Our clinical prediction tool could be enabled to be better targeting of early interventions for infection after transplant as opposed to indiscriminately prophylaxis or treatment in centers.
Funding
This work was funded by the High Quality Development Research Project in Hospital Pharmacy (Grant Number NIHAYS2302), Beijing Friendship Hospital Research Initiation Fund Project (Grant Number yygdktgl2021-3) and Special Research Fund for Clinical Studies of Innovative Drugs after Market Launch (Grant Number WKZX2023CX).
Disclosure
The authors report no conflicts of interest in this work.
References
1. Dorschner P, McElroy LM, Ison MG. Nosocomial infections within the first month of solid organ transplantation. Transpl Infect Dis. 2014;16(2):171–187. doi:10.1111/tid.12203
2. Avkan-Oguz V, Ozkardesler S, Unek T, et al. Risk factors for early bacterial infections in liver transplantation. Transplant Proc. 2013;45(3):993–997. doi:10.1016/j.transproceed.2013.02.067
3. Fishman JA. From the classic concepts to modern practice. Clin Microbiol Infect. 2014;20:4–9. doi:10.1111/1469-0691.12593
4. Grat M, Ligocka J, Lewandowski Z, et al. Incidence, pattern and clinical relevance of microbial contamination of preservation fluid in liver transplantation. Ann Transplant. 2012;17(3):20–28. doi:10.12659/AOT.883454
5. Mattana AM, Marra AR, Machado AM, et al. Evaluation of the presence of microorganisms in solid-organ preservation solution. Braz J Infect Dis. 2011;15(6):528–532. doi:10.1590/S1413-86702011000600005
6. Li J, Su X, Li J, et al. The association of organ preservation fluid pathogens with early infection-related events after kidney transplantation. Diagnostics. 2022;12(9):2248. doi:10.3390/diagnostics12092248
7. Yahav D, Manuel O. Clinical relevance of preservation-fluid contamination in solid-organ transplantation: a call for mounting the evidence. Clin Microbiol Infect. 2019;25(5):536–537. doi:10.1016/j.cmi.2019.02.025
8. Yu X, Wang R, Peng W, et al. Incidence, distribution and clinical relevance of microbial contamination of preservation solution in deceased-donor kidney transplant recipients: a retrospective cohort study from China. Clin Microbiol Infect. 2019;25(5):595–600. doi:10.1016/j.cmi.2018.12.040
9. Oriol I, Sabé N, Tebé C, et al. Clinical impact of culture-positive preservation fluid on solid organ transplantation: a systematic review and meta-analysis. Transplant Rev. 2018;32(2):85–91. doi:10.1016/j.trre.2017.11.003
10. Corbel A, Ladrière M, Le Berre N, et al. Microbiological epidemiology of preservation fluids in transplanted kidney: a nationwide retrospective observational study. Clin Microbiol Infect. 2020;26(4):475–484. doi:10.1016/j.cmi.2019.07.018
11. Le Berre N, Ladrière M, Corbel A, et al. Antibiotic therapy in case of positive cultures of kidney transplant preservation fluid: a nationwide survey of prescribing practices. Eur J Clin Microbiol Infect Dis. 2020;39(5):915–921. doi:10.1007/s10096-019-03808-4
12. Addeo P, Saouli AC, Woehl-Jaegle ML, et al. Candida albicans arteritis transmitted by preservation fluid after liver transplantation. Ann Transpl. 2014;19:64–67. doi:10.12659/AOT.889831
13. Levesque E, Paugam-Burtz C, Saliba F, et al. Fungal complications after Candida preservation fluid contamination in liver transplant recipients. Transpl Int. 2015;28(11):1308–1316. doi:10.1111/tri.12633
14. Albano L, Bretagne S, Mamzer‐Bruneel M-F. Evidence that graft-site candidiasis after kidney transplantation is acquired during organ recovery: a multicenter study in France. Clin Infect Dis. 2009;48(2):194–202. doi:10.1086/595688
15. Rodríguez Faba O, Boissier R, Budde K, et al. European Association of Urology guidelines on renal transplantation: update 2018. Eur Urol Focus. 2018;4(2):208–215. doi:10.1016/j.euf.2018.07.014
16. Bertrand D, Pallet N, Sartorius A, et al. Clinical and microbial impact of screening kidney allograft preservative solution for bacterial contamination with high-sensitivity methods. Transpl Int. 2013;26(8):795–799. doi:10.1111/tri.12130
17. Veroux M, Corona D, Scriffignano V, et al. Contamination of preservation fluid in kidney transplantation: single-center analysis. Transplant Process. 2010;42(4):1043–1045. doi:10.1016/j.transproceed.2010.03.041
18. Wakelin SJ, Casey J, Robertson A, et al. The incidence and importance of bacterial contaminants of cadaveric renal perfusion fluid. Transpl Int. 2005;17(11):680–686. doi:10.1007/s00147-004-0792-6
19. Meier-Kriesche HU, Ojo AO, Hanson JA, Kaplan B. Exponentially increased risk of infectious death in older renal transplant recipients. Kidney Int. 2001;59(4):1539–1543. doi:10.1046/j.1523-1755.2001.0590041539.x
20. Trouillhet I, Benito N, Cervera C, et al. Influence of age in renal transplant infections: cases and controls study. Transplantation. 2005;80(7):989–992. doi:10.1097/01.TP.0000173822.05877.D7
21. Bodro M, Sabe N, Tubau F, et al. Risk factors and outcomes of bacteremia caused by drug-resistant ESKAPE pathogens in solid-organ transplant recipients. Transplantation. 2013;96(9):843–849. doi:10.1097/TP.0b013e3182a049fd
22. Sandkovsky U, Kalil AC, Florescu DF. The use and value of procalcitonin in solid organ transplantation. Clin Transplant. 2015;29(8):689–696. doi:10.1111/ctr.12568
23. Strueber M, Warnecke G, Fuge J, et al. Everolimus versus mycophenolate mofetil De novo after lung transplantation: a prospective, randomized, open-label trial. Am J Transplant. 2016;16(11):3171–3180. doi:10.1111/ajt.13835
24. Sacher VY, Fertel D, Srivastava K, et al. Effects of prophylactic use of sirolimus on bronchiolitis obliterans syndrome development in lung transplant recipients. Ann Thorac Surg. 2014;97(1):268–274. doi:10.1016/j.athoracsur.2013.07.072
25. Snell GI, Valentine VG, Vitulo P, et al. Everolimus versus azathioprine in maintenance lung transplant recipients: an international, randomized, double-blind clinical trial. Am J Transplant. 2006;6(1):169–177. doi:10.1111/j.1600-6143.2005.01134.x
26. Bhorade S, Ahya VN, Baz MA, et al. Comparison of sirolimus with azathioprine in a tacrolimus-based immunosuppressive regimen in lung transplantation. Am J Respir Crit Care Med. 2011;183(3):379–387. doi:10.1164/rccm.201005-0775OC
27. Büchler M, Caillard S, Barbier S, et al. Sirolimus versus cyclosporine in kidney recipients receiving thymoglobulin, mycophenolate mofetil and a 6-month course of steroids. Am J Transplant. 2007;7(11):2522–2531. doi:10.1111/j.1600-6143.2007.01976.x
28. Kauffman HM, Cherikh WS, Cheng Y, et al. Maintenance immunosuppression with target-of-rapamycin inhibitors is associated with a reduced incidence of de novo malignancies. Transplantation. 2005;80(7):883–889. doi:10.1097/01.TP.0000184006.43152.8D
29. Vickers AJ, Holland F. Decision curve analysis to evaluate the clinical benefit of prediction models. Spine J. 2021;21(10):1643–1648. doi:10.1016/j.spinee.2021.02.024
 © 2024 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2024 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.