Back to Journals » International Journal of Women's Health » Volume 16
Decision To Delivery Time and Its Predictors Among Mothers Who Underwent Emergency Cesarean Delivery At Selected Hospitals of Northwest Ethiopia, 2023: Prospective Cohort Study
Authors Hussein BA, Damtew BS , Abdi HB , Gudayu TW
Received 24 September 2023
Accepted for publication 22 January 2024
Published 9 February 2024 Volume 2024:16 Pages 249—264
DOI https://doi.org/10.2147/IJWH.S436755
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Professor Elie Al-Chaer
Beker Ahmed Hussein,1 Beyene Sisay Damtew,1 Hinsermu Bayu Abdi,1 Temesgen Worku Gudayu2
1Department of Midwifery, College of Health Sciences, Arsi University, Asella, Ethiopia; 2Department of Clinical Midwifery, College of Medicine and Health Sciences, University of Gondar, Gondar, Ethiopia
Correspondence: Beker Ahmed Hussein, Email [email protected]
Background: The decision to delivery time is the interval between the decision and the childbirth by emergency caesarean delivery. The Royal College of Obstetricians and Gynecologists and the American College of Obstetricians and Gynecologists recommend that the decision to delivery time interval is less than 30 min. Additionally, the decision to delivery time varies across institutions and countries.
Objective: The aim of this study was to determine the decision to delivery time and its predictors among women who underwent emergency cesarean delivery at selected hospitals of Northwest Ethiopia, 2023.
Methods: An institutional-based prospective cohort study was conducted at selected hospitals of Northwest Ethiopia, among women who underwent emergency cesarean delivery from November 1 to January 30, 2023. A total of 285 participants were enrolled, and data collected using structured and pre-tested questionnaires. A systematic sampling technique was used. Data were entered into Epi-Data version 4.6 and then exported to STATA 15 for further analysis. The log rank test was utilized to compare group differences. The time is estimated by using the Kaplan–Meier curve and Cox proportional-hazard regression analysis was carried out to determine the predictors.
Results: From 285 participants, 56 (21.8%) women delivered within the recommended 30 min. The overall median survival time was undetermined and the restricted mean survival time was 48.9 min (95% CI: 47.4– 50.5). The average decision to delivery time is affected among women who hesitate to accept consent (AHR: 0.17, 95% CI: 0.02– 1.25), cord prolapses (AHR: 1.36, 95% CI: 0.46– 3.94), rank of surgeon (AHR: 0.42. 95% CI: 0.42– 1.08), no free operation room table (AHR: 0.27, 95% CI: 0.28– 0.94), regional anesthesia (AHR: 0.56, 95% CI: 0.25– 1.28), and use of a bladder flap (AHR: 0.33, 95% CI: 0.16– 0.85).
Conclusion: Overall decision to delivery times among women who underwent emergency cesarean section at selected hospitals were longer than the recommended time.
Keywords: decision time, emergency cesarean delivery
A Letter to the Editor has been published for this article.
Background
The period from the decision to perform a cesarean delivery until the baby was delivered is known as the decision to delivery time, and is measured in minutes.1
The amount of time it takes to prepare the patient and the theater, provide anesthesia, and deliver the baby includes all of these factors. The decision to delivery time must be as quick as possible since an emergency caesarean section is done when the life of the mother or fetus is in urgent danger during delivery.2 The suggested decision to delivery time is within 30 min, according to the American College of Obstetricians and Gynecologists (ACOG) and the Royal College of Obstetricians and Gynecologists (RCOG), as two such organisations.3 In contemporary obstetrics, normal caesarean births are provided to women as an elective procedure for a several reasons, or they are carried out in an emergency due to fetal or maternal problems, or both.4 Caesarean sections can be categorized as emergency, urgent, planned, or elective depending on how serious the fetal or maternal condition is. The categorization states that emergency CS is carried out when the woman, the fetus, or both are in grave danger.5 The anesthesiologist and trained assistant, the obstetrician and assistant, a theater nurse, and neonatal support staff are all involved in the complicated and multidisciplinary cesarean section operation.6 It is necessary to gather this crew, as some of them must review the patient and also get her ready. Before surgery can be performed, certain patients may require additional care and stabilization to make sure their condition is at its best. Even while in the event of an emergency cesarean section the DDT must be regarded as having been completed as a goal, failure to stabilize the patient may increase the risk of maternal death and morbidity as a result of the surgery or anesthesia problem.7 A hospital that offers obstetric care should be able to react to an emergency within the required timeframe. The dangers associated with an emergency cesarean section, however, might be substantially higher in underdeveloped countries than in developed countries since it may take longer to start one there and resources may not be sufficient.8 Three delays prevent pregnant and laboring women from obtaining the professional care they require in a timely manner. These delays might be caused by a lack of supplies, inadequate knowledge or experience of the provider, or a lack of basic equipment.9
It has been noted that a variety of factors, such as team preparedness, team communication, team availability, severity of fetal–maternal problems, seniority of the surgeon, availability of obstetricians and anesthesia staff, time and day of operation, and kind of anesthesia, might impact the decision to delivery time (DDT).10 Facilities and service providers must be ready for quick emergency action and prepared in advance to solve the issue. To reduce morbidity and mortality associated with delayed decision to delivery time (DDT), further measures should be taken: a 24-hour cesarean surgery room that is housed within the labor and delivery ward, well-trained personnel who are available seven days a week, effective teamwork, and a delivery room with all the necessary equipment for emergency action.2,11 Compared to elective and vaginal births, the perinatal and maternal outcomes of emergency cesarean delivery are worse. Quality obstetric care services, such as reducing third delays and delays in getting appropriate treatment, such as shortening the time between decision and delivery in the event of emergency cesarean delivery, are one strategy to combat this. Standardization of the decision to delivery interval is important for medico-legal problems as well as quality.12,13 Hence, this study aimed is to assess the decision to delivery time and its predictors among women who underwent emergency cesarean delivery.
Methodology
Study Area and Design
A prospective cohort study was conducted from November 1 to January 30, 2023 among women who underwent emergency cesarean delivery at selected hospitals of Northwest Ethiopia.
Source Population
All pregnant women who underwent emergency cesarean delivery at selected hospitals of Northwest Ethiopia were included.
Study Population
Pregnant women whose emergency cesarean delivery was done during the study period were included.
Eligibility Criteria
Inclusion Criteria
Pregnant women who underwent emergency cesarean delivery were included.
Exclusion Criteria
Women with multiple pregnancies were excluded.
Those stating total refusal of emergency cesarean delivery were excluded.
Sample Size Determination
A single population proportion formula was used to calculate the sample size by considering the following statistical assumptions.
P=the proportion of women who had a decision to delivery time interval below 30 min is 21.3%, from a study done in Ethiopia.14
Zα/2=the corresponding Z score of the 95% CI.
d=margin of error (5%) and N=sample size.
N=(Zα2)2×p(1–p)/(d)2
N=(1.96)2×0.213×0.787/(0.05)2=259, and then after adding 10% loss follow-up, the final sample size was 285.
Sampling Procedure
Two hospitals were selected by simple random sampling that were found in Northwest Ethiopia. Prior to data collection, the average number of women who underwent emergency cesarean delivery was estimated using reports from the previous three months. According to data from the past three months, each hospital had an average case flow of 562 for Debre Markos Comprehensive Specialized Hospital and 45 for Lumame Primary hospital. The sample size was allocated for two hospitals proportionally based on the estimated numbers of women who underwent emergency cesarean delivery in two hospitals over three months when the data collection was conducted. A kth interval (562+45)/285≈2 of the total estimated numbers of women who underwent emergency cesarean delivery in the two hospitals over three months to the calculated sample size was approximated. The first participant (women) was recruited by a lottery method. The sample of women with emergency cesarean delivery was obtained from each hospital by using a systematic random sampling technique with a sampling interval of k=2 (Figure 1).
 |
Figure 1 Schematic presentation of the sampling procedure at selected hospitals of Northwest Ethiopia, 2023. |
Study Variables
Dependent Variable
Occurrence of the decision to delivery time within 30 min.
Independent Variable
Sociodemographic:
age, educational status, marital status, place of residence, and attendant educational status.
Obstetrics History
ANC follow-up, BPCR, presence of scar, and cervical dilation at decision.
Indication of Cesarean Section
Cord prolapses, NRFHBP, abruption, CPD, and uterine rupture.
Type of Anesthesia
General, spinal, and epidural.
Surgeon’s Rank
Senior and resident.
Time and Day of the Week When the Surgery Will Be Performed
Weekday, weekend, daytime, and night-time.
Preparation for Emergency Cesarean Delivery
Resuscitative measures, obtaining consent, and unavailability of logistics.
Operational definitions
Event: if the delivery occurs in less or equal 30 min it was considered as an event, whereas above 30 min is considered as a censored observation.
Start time: decision time.
End time: delivery of the neonate by emergency cesarean section.
Emergency cesarean section: when the CS is done in labor or due to any complication that necessitates immediate cesarean delivery.
Decision time: when the surgeon who performed the procedure decided to do emergency cesarean delivery.
Data Processing and Analysis
Data were entered into Epi-Data version 4.2 after checking for completeness, and then the data were cleaned and transferred to STATA 15 statistical software for analysis. Before running the Cox proportional hazard regression model to simultaneously assess the association between multiple covariates and survival, multicollinearity was checked using the variance inflation factor (VIF) for continuous variables. All variables were found to be <10. The proportional hazard assumption (PHA) was checked to identify the combined effects of several covariates on the hazard ratio, using scaled Schoenfeld residual tests (PH test), and all variables fulfilled this assumption (P-value>0.05). The log rank test was utilized to compare group differences and the decision to delivery time was estimated using the Kaplan–Meier curve. To identify potential predictors of time to decision of delivery, a bivariable Cox proportional regression model was fitted for each explanatory variable and variables that would have a P-value less than 0.025 were included in the multiple Cox regression model. In the multiple Cox analysis, variables that have a P-value less than 0.05 were significant predictors of decision to delivery time. The adjusted hazard ratio was used to show the strength of association between each predictor variable and the outcome variable.
Data Collection Procedure
Data were collected using a standardized questionnaire. Six bachelor midwives were involved in the data collection. Once the study subject was recruited by systematic sampling techniques they were followed from the time the decision was made by the surgeon until the delivery of the neonate by emergency cesarean delivery. The decision to do an emergency cesarean delivery, the indication of the procedure, the time of the operation transfer, the duration of the anesthesia, the total time from the decision to the birth of the fetus, and the time the anesthesia team was informed were all obtained from the patient’s charts and by direct observation. The moment the doctors made the decision to perform an emergency caesarean delivery and the time at which the operation was done were recorded. The length of time it took to transfer to the operating room, choose anesthesia, administer it, and perform the procedure were all afterwards noted.afterward
Data Quality Control
Before data collection, a pretest on 5% of the sample was conducted. Both the supervisor and the data collectors received a two-day training. Daily completion and consistency checks were made on the completed questionnaire. Daily data cleaning was carried out, and the data collectors received quick feedback.
Results
Sociodemographic Characteristics of Study Participants
A total of 285 women who underwent category-1 cesarean section with a response rate of 100% were studied. The majority of women (120, 42.1%) in this study were aged between 25–29 years with a mean of 28±5.006. The majority of the respondents are married (261, 91.6%). Around 66 (23.2%) had a level of education of high school, diploma, and above. Around 135 (47.4%) are housewives. Regarding participants' residence, 194 (68.1%) were urban (Table 1).
 |
Table 1 Socio-Demographic Characteristics of Women Undergoing Emergency Cesarean Delivery at Selected Hospitals of Northwest Ethiopia, 2023 (n=285) |
Obstetric Characteristics of Study Participants
The findings showed that 37.9% of the respondents were primigravid. The majority of the respondents had ANC visits. Around 63.2% of women had been counseled on BPCR plan during ANC follow-up. Sixty-five (22.8%) participants had a previous history of cesarean section. The majority of the participants (258, 90.5%) accepted informed consent immediately after she was counseled for CS. In this study the main indication for emergency cesarean delivery is non-reassuring fetal heart rate (NRFHR) (Table 2).
 |
Table 2 Obstetrical Characteristics of Women Undergoing Emergency Cesarean Delivery at Selected Hospitals of Northwest Ethiopia, 2022/23 (n=285) |
Regarding the indication of emergency cesarean delivery, around 36.10% were women with NRFHR, 13% had grade three meconium, 10.9% with CPD, 10.20% are with two c/s scars, 4.60% are with cord prolapse, and 3.90% are with other indications (Figure 2).
 |
Figure 2 Decision to delivery time among women underwent emergency cesarean delivery with different indications at selected hospitals of Northwest Ethiopia, 2023. |
Regarding the rank of the surgeon, from 285 study participants around 30.53% of emergency cesarean deliveries are performed by IESO, followed by MSc clinical Midwifery students who account for around 28.42%, and the remaining 25.26% and 15.79% are performed by senior and MSc clinical Midwife respectively (Figure 3).
 |
Figure 3 Decision to delivery time among women who underwent emergency with the rank of surgeon at selected hospitals of Northwest Ethiopia, 2023. |
The Incidence Rate and Median Decision to Delivery Time
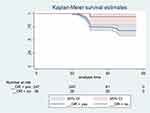
The study participant was followed for a minimum of 18 min and a maximum of 56 min with a median follow-up time of 35±8.14 min. Two hundred eighty five participants were followed for different periods of maximum of eighten minute and gives 10,060 persons minutes of obsrvation. Around 62 (21.8%) developed the event (delivered within 30 min) (95% CI: 17.2–27.3) while 223 (78.2%) women were censored (95% CI: 73–83.2). The overall decision to delivery time rate was 0.6 per 100-person minute (95% CI: 30–45.) The median decision to delivery time overall could not be calculated because the largest observed analysis time was censored.
Instead of computing the total median survival time, the mean survival time confined to the longest follow-up period was calculated. The overall restricted mean survival time was 48.9 min (95% CI: 47.4–50.5) (Figure 4).
 |
Figure 4 The overall restricted mean decision to delivery time among women who underwent emergency cesarean delivery at selected hospitals of Northwest Ethiopia, 2023. |
Comparison of Survival Status for Different Factors with the Log Rank Test
The log rank test was performed to test the equality of survival curves for the presence of any notable variations in survival rates across the various levels of the categorical factors taken into account in the research. The test results in this study demonstrated a substantial difference in the survival function for several categorical variables. Accordingly, the Kaplan–Meier analysis revealed strong evidence of variations in decision to delivery timeframes. It was found that the mean decision to delivery time for women who accepted informed consent was 48.4 min (95% CI: 46.7–50.1), which was shorter than those who delayed to accept at 54.9 min (95% CI: 52.7–57). With a p-value of 0.020, this difference was statistically significant (Figure 5).
The mean decision to delivery time for mothers with indication for cord prolapse is 32 min (95% CI: 28.7–35.3), which is shorter than with their courtparts such APH (39 min), obstructed labor (47 min), GIII MSAF (46.9 min), NRFHRP (48.8 min), CPD (50.4 min), two C/S scars (48.6 min), and others (51.4 min). This difference was statistically significant with p-value=0.000 (Figure 6).
The mean decision to the delivery time for women whose OR material was prepared was 48 min (95% CI: 46.3–49.8) which is shorter than their counterparts at 54.5 min (95% CI: 52.4–56.5), and testing equality among the groups with p-value of 0.006 was statistically significant among the group (Figure 7).
The mean decision to the delivery time for women whose free functional OR tables were present was 47.7 min (95% CI: 45.9–49.6) which is shorter with their counterparts at 54.3 min (95% CI: 2.5–56.2), and testing equality among the groups with p-value of 0.002 was statistically significant among the group (Figure 8).
The mean decision to the delivery time for women with general anesthesia was 37 min (95% CI: 30.2–44.3) which is shorter than for women with regional anesthesia at 49.5 min (95% CI: 47.9–51.1), and testing equality among the groups with p-value of 0.000 was statistically significant among the group (Figure 9).
Testing Proportional Hazards Assumption
A Cox regression model was used to examine the effects of sociodemographic, obstetrics, and treatment characteristics of patients on the decision to delivery time. The following variables were included in the model as predictors: residence, birth preparedness and complication readiness, consent, indication, bladder flap, working time, rank of the surgeon, types of anesthesia, OR material prepared, and free functional OR table present were all significantly associated with decision to delivery time. A goodness-of-fit (GOF) test was conducted to assess the proportional hazard (PH) assumptions of the Cox model for given predictor variables. The findings indicated that all variables included in the model satisfied PH assumptions (p-value>0.05) with a global test of 0.5005 (Table 3).
 |
Table 3 Goodness-of-Fit Test Assessing Proportional Hazards Assumption |
After preserving the Schoenfeld and scaling the Schoenfeld, the proportional hazards assumption test residuals suggested that both covariate-specific and global tests are not violated (fulfilled). Hence, the Cox regression model is best for these data.
Predictors of Decision to Delivery Time
Following the testing of each variable in turn, the bivariable analyses revealed that residence, birth preparedness and complication readiness, consent, indication, bladder flap, working time, rank of the surgeon, types of anesthesia, time of transfer to OR, time of anesthesia, OR material prepared, and free functional OR table present were all significantly associated with the decision to delivery time.
After controlling confounders in multiple Cox regression analysis, consent, indication for cord prolapses, anesthesia types, free functional OR table present, rank of the surgeon, and bladder flap were independent predictors of the decision to delivery time. The multiple Cox regression analysis revealed that holding other variables constant, women who hesitate to accept informed consent are 83% less likely to have a decision to delivery time within 30 min (AHR: 0.17, 95% CI: 0.02–1.25) whenever there is a follow-up. Holding other variables constant, women with cord prolapse have 1.36 higher hazard of developing the decision to delivery time than those with other indications (AHR: 1.36, 95% CI: 0.46–3.94). Regarding the rank of surgeon, MSc in clinical midwifery students were 58% times less likely to decide on emergency C/S as compared to seniors (AHR: 0.42, 95% CI: 0.420.16–1.08). Moreover, relative to patients who have free functional OR tables present, those who have no free OR table were 73% times less likely to develop the decision to delivery time (AHR: 0.27, 95% CI: 0.28–0.94).
Furthermore, using a bladder flap during emergency C/S is 67% less likely to undergo the decision to delivery time as compared to not using (AHR: 0.33, 95% CI: 0.16–0.85). Emergency cesarean delivery with regional anesthesia is 44% less likely to have decision delivery time as compared with general anesthesia (AHR: 0.56, 95% CI: 0.25–1.28) (Table 4).
 |
Table 4 Cox Regression Analysis of Predictors of Decision to Delivery Time Among Women Who Underwent Emergency Cesarean Delivery at Selected Hospitals of Northwest Ethiopia, 2023 (N=285) |
Discussion
In this cohort study, the aim is to determine the decision to delivery time and its predictors among women who underwent emergency cesarean delivery. At the end of three months of follow-up, 62 (21.8%) women delivered within 30 min or less with a mean DDT of 48.9 min, which is nearly similar with other studies of 19.6%, 21.3% in Gondar Southern Ethiopia, and 20.3% in Bahir Dar.14–16 This may be due to the similarity in the accessibility of logistics in hospitals, the practice and experience of professionals, and types of cesarean delivery. The finding of this study is lower than in Saudi Arabia which was 30.6%, 87.5% in Denmark, 42.4% in India, 45% in Gondar in 2022, and in one study 50.29%, but is comparable with a study in Oman Qatar at 23.8%.17–22 This difference might be occurring due to various studies conducted in different with different set up of institutions and different sample sizes. The findings of this research were greater than those of studies conducted in Tanzania, Kenya, Benin teaching hospital, Nigeria, and Bahir Dar in 2021 which were 14.3%, 12%, 3%, 2.1%, and 5.7%, respectively.1,5,23–25 The difference might be due to general infrastructure, economic differences, multidisciplinary operative room team training, easy accessibility of logistics, and laboratory services.
In this study, the overall incidence of decision to delivery time was found to be 1.2 per 100-women minutes of observation. The mean decision to delivery time was 48.9 min (IQR=29–35; 95% CI: 52.5–61.7). This finding is higher than the studies done in Sunanda17, in Gondar16 by 2020, in Israel26 and in Ireland,27 in Bahir Dar,25 and in Nigeria,5 in 2021. The difference might be the sample size, period, types of emergency cesarean delivery, and institutional differences. On the contrary, this finding is less than the study done in Benin teaching hospital1 which was 106.3±79.5 min, in Indonesia,28 in India,6 in Gondar,16 in Nigeria10 which was 145.3 ± 69.2 min, and in Norway29 which was 52.4 min. The difference might be due to general infrastructure, economic differences, multidisciplinary operative room team training, easy accessibility of logistics, laboratory services, sample size, study period, and types of emergency C/S which include both categories in this study. So, an institution having an adequate operation table, experienced physician, anesthetist, operation room materials, operation room nurse, and urgency of indication could shorten the decision to delivery time interval in the emergency cesarean section. In this study, the presence of a free operation table, consent, indication for cord prolapses, rank of surgeon, anesthesia types, and use of a bladder flap are predictors of decision to delivery time in the multiple Cox regression analysis.
In this study, women who accepted informed consent had a statistically significant association with recommended DDT compared with women who hesitated to accept earlier. In this study, women who hesitated to accept informed consent were 87% less likely to have a decision to delivery time when compared to those who agreed to accept emergency C/S within 30 min. This finding is supported by a study done in Gondar.21 This study found that women whose EmCS was performed under regional anesthesia were 44% less likely to have the recommended DDT than women who were performed under general anesthesia. The findings of this study were in line with those of studies conducted in Israel,19 Indonesia, Norway, and Bahir Dar which showed that general anesthesia shortened the DDT as compared to regional anesthesia.15,26,28,29 The similarity may be a delay in regional anesthesia as a result of technical problems in inducing, and stabilization of clients before regional anesthesia is needed. Women whose emergency cesarean delivery was performed by seniors were more likely to have the recommended DDT than those made by MSc Clinical Midwife and MSc in Clinical Midwifery students. The same result was observed in Norway29 and Bahir Dar.15 This could be because seniors were more experienced and had more exposure than others. A study in Singapore and Hong Kong showed no significant differences in DDI between senior surgeons and residents.
In this study, compared to women with a free OR table, those with no free functional OR table present were 73% less likely to have the recommended decision to delivery time. This finding is in line with studies conducted in different parts like Gondar,21 Gamo Zone,14 and Oman that revealed that women who had no additional OR table while they are preparing for EmCS were associated with a longer decision to delivery time. This might be attributed to the fact that if there is no additional OR table, it causes a prolonged decision to delivery interval secondary to the third delay. Regarding indication for emergency C/S, women with cord prolapse are 1.36 times more likely to have a decision to delivery time when compared with other indications. This may be due to the cord prolapses needing a prompt response from providers to save the life of the fetus. In this study around 92.3% of the study participants with cord prolapse had emergency C/S with recommended time. Another significant variable in this study is the use of a bladder flap which is 67% less likely to have the recommended delivery time within 30 min. This finding was supported by a study done in the USA which shortened the incision to delivery time among non-users.30
Conclusion
The decision to delivery time among women underwent emergency cesarean delivery at DCSH and Lumame Primary Hospital was longer than the recommended interval of time. Only 21.8% of women were delivered within the recommended DDT below 30 min. The presence of a free OR table, hesitated to consent, indication for cord prolapses, rank of surgeon, anesthesia types, and use of a bladder flap are predictors of decision to delivery time in the multiple Cox regression analysis. Despite the importance of doing EmCS as the recommended interval for the improvements of a perinatal outcome as well as quality care for mother and newborn, a substantial number of women had not achieved the recommended DDT (<30 min).
We strongly recommend that material which providers and facilities should be better equipped with a free OR table in advance and ready for a rapid emergency cesarean delivery.
Consent processes are also another important factor that determines the decision to the delivery time at Debre Markos Comprehensive Specialized Hospital and Lumame Primary Hospital. The care provider should give information at antenatal care about the possibility of operational delivery that helps to shorten time spent on the consent process. It would have been better if general anesthesia was used rather than regional anesthesia as a result of technical problems in inducing and stabilization of clients before regional anesthesia is needed. Also, it as better if ECD was performed by seniors because seniors were more experienced and had more exposure than others.
Abbreviations
ACOG, American College of Obstetrician and Gynecologist; ANC, Antenatal care; AHR, Adjusted hazard ratio; BPRC, Birth preparedness and complication readiness; CPD, Cephalo-pelvic disproportion; DCSH, Debre Markos Comprehensive Specialized Hospital; DDT, Decision to delivery time; CD, Cesarean delivery; EmCD, Emergency cesarean delivery; NRFHR, Non-reassuring fetal heart rate; OR, operation room; RCOG, Royal College of Obstetricians and Gynecologists.
Data Sharing Statement
Data will be available from the corresponding author on reasonable request.
Ethical Approval and Informed Consent
All methods were conducted according to the ethical standards of the Declaration of Helsinki. Ethical clearance was obtained from an institutional Research Ethics Review Board (IRB) of University of Gondar with reference number MIDW/30/2015 E.C. In addition, a letter of ethical approval was sent to Debre Markos Comprehensive Specialized Hospital and Lumame Primary Hospital and permission was obtained from the hospital’s administrators. Informed, voluntary, written, and signed consent was obtained from the head of the hospital and mothers. There are no study participants under the age of 18 years. The standard safety measures for the prevention of COVID-19 were strictly followed throughout the data collection period. Before conducting the interviews, information was given to the participants and they were assured for voluntary participation, confidentiality, and freedom to withdraw from the study at any time. The nature and significance of the study was explained to the participants.
Acknowledgment
We would like to thank the study participants for their time and the data collectors and supervisors for their commitment.
Author Contributions
All authors made a significant contribution to the work reported, that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising, or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Funding
A total fund of 25000 Ethiopian birr with a project code of MIDW/30/2015 E.C was received from University of Gondar office of research and publication directorate director.
Disclosure
The authors report no conflicts of interest in this work.
References
1. Chukwudi OE, Okonkwo CA. Decision-delivery interval and perinatal outcome of emergency caesarean sections at a tertiary institution. Pakistan J Med Sci. 2014;30(5):946. doi:10.12669/pjms.305.5470
2. Rashid N, Nalliah S. Understanding the decision-delivery interval in Cesarean births. IeJSME. 2007;1(2):61–68. doi:10.56026/imu.1.2.61
3. Singh R, Deo S, Pradeep Y. The decision-to-delivery interval in emergency Caesarean sections and its correlation with perinatal outcome: evidence from 204 deliveries in a developing country. Trop Doctor. 2012;42(2):67–69. doi:10.1258/td.2012.110315
4. Yentis SM, Richards NA. Classification of urgency of caesarean section. Obstetrics Gynaecol Reproductive Med. 2008;18(5):139–140. doi:10.1016/j.ogrm.2008.03.005
5. Bello FA, Tsele TA, Oluwasola TO. Decision-to-delivery intervals and perinatal outcomes following emergency cesarean delivery in a Nigerian tertiary hospital. Int J Gynecol Obstet. 2015;130(3):279–283. doi:10.1016/j.ijgo.2015.03.036
6. Radhakrishnan G, Yadav G, Vaid NB. Factors affecting decision to delivery interval in emergency caesarean sections in a tertiary care hospital: a cross sectional observational study. Int J Reprod Contraception Obstetrics Gynecol. 2013;2(4):651–657. doi:10.5455/2320-1770.ijrcog20131231
7. Obstetricians ACo. Gynecologists. ACOG Committee Opinion No. 487: preparing for clinical emergencies in obstetrics and gynecology. Obstetrics Gynecol. 2011;117(4):1032–1034. doi:10.1097/AOG.0b013e31821922eb
8. Lumbiganon P, Laopaiboon M, Gülmezoglu AM, et al. Method of delivery and pregnancy outcomes in Asia: the WHO global survey on maternal and perinatal health 2007–08. Lancet. 2010;375(9713):490–499. doi:10.1016/S0140-6736(09)61870-5
9. Health FMo. Management Protocol on Selected Obstetrics Topics. Federal Democratic Republic of Ethiopia; 2010.
10. Owonikoko K, Olabinjo A, Bello-Ajao H, Adeniran M, Ajibola T. Determinants of Decision to Delivery Interval (DDI) in Emergency Caesarean Sections in Ladoke Akintola University of Technology Teaching Hospital Ogbomoso, Nigeria. Clin Mother Child Health. 2018;15:294.
11. Ayano B, Guto A. Indications and outcomes of emergency caesarean section at St Paul’s hospital medical college, Addis Ababa, Ethiopia 2017:(afoul month retrospective cohort study). Gynecol Reprod Health. 2018;2(5):1–12. doi:10.33425/2639-9342.1053
12. Mishra N, Gupta R, Singh N. Decision delivery interval in emergency and urgent caesarean sections: need to reconsider the recommendations? J Obstetrics Gynecol India. 2018;68(1):20–26. doi:10.1007/s13224-017-0991-6
13. Fesseha N, Getachew A, Hiluf M, Gebrehiwot Y, Bailey P. A national review of cesarean delivery in Ethiopia. Int J Gynecol Obstet. 2011;115(1):106–111. doi:10.1016/j.ijgo.2011.07.011
14. Beyene K, Fekadu K, Yihune M, et al. Decision to Delivery Interval, Perinatal Outcome and Factors Following Emergency Cesarean Section in Southern Ethiopia. Ethiopian J Health Sci. 2023;33:1. doi:10.4314/ejhs.v33i1.1
15. Kitaw TM, Limenh SK, Chekole FA, Getie SA, Gemeda BN, Engda AS. Decision to delivery interval and associated factors for emergency cesarean section: a cross-sectional study. BMC Pregnancy Childbirth. 2021;21(1):1–7. doi:10.1186/s12884-021-03706-8
16. Temesgen MM, Gebregzi AH, Kasahun HG, Ahmed SA, Woldegerima YB. Evaluation of decision to delivery time interval and its effect on feto-maternal outcomes and associated factors in category-1 emergency caesarean section deliveries: prospective cohort study. BMC Pregnancy Childbirth. 2020;20(1):1–11. doi:10.1186/s12884-020-2828-z
17. Gupta S, Naithani U, Madhanmohan C, Singh A, Reddy P, Gupta A. Evaluation of decision-to-delivery interval in emergency cesarean section: a 1-year prospective audit in a tertiary care hospital. J Anaesthesiol Clin Pharmacol. 2017;33(1):64. doi:10.4103/0970-9185.202197
18. Fuhrmann L, Pedersen T, Atke A, Møller A, Østergaard D. Multidisciplinary team training reduces the decision‐to‐delivery interval for emergency Caesarean section. Acta Anaesthesiologica Scandinavica. 2015;59(10):1287–1295. doi:10.1111/aas.12572
19. Sait KH. The decision to delivery interval in emergency and non-urgent caesarean sections at king Abdulaziz University hospital. J King Abdulaziz Univ. 2011;98(282):1–16.
20. Nair VV, Nair SS, Venugopalan P. Decision to delivery interval in emergency LSCS and its impact on fetal outcome. Int J Reprod Contraception Obstetrics Gynecol. 2019;8(9):3679–3684. doi:10.18203/2320-1770.ijrcog20193797
21. Tegegne F. Prolonged Decision to Delivery Time Interval and Associated Factor in Emergency Caesarean Section in University of Gondar Comprehensive and Specialized Hospital, 2022. UOG; 2022.
22. Maducolil MK, Ajmal S, Alzebdeh E. Category 1 cesarean section decision to delivery interval: the causes of delay and impact on neonatal outcomes. Int J Pregnancy Child Birth. 2021;10:84–92.
23. Hirani BA, Mchome BL, Mazuguni NS, Mahande MJ. The decision delivery interval in emergency caesarean section and its associated maternal and fetal outcomes at a referral hospital in northern Tanzania: a cross-sectional study. BMC Pregnancy Childbirth. 2017;17(1):1–6. doi:10.1186/s12884-017-1608-x
24. Kanario P, Mburugu P, Kabuga S, et al. Decision to delivery interval of emergency caesarean section and associated maternal and neonatal outcomes in a county hospital in Kenya. East Afr Med J. 2021;98:7.
25. Kitaw TM, Tsegaw Taye B, Tadese M, Getaneh T. Effect of decision to delivery interval on perinatal outcomes during emergency cesarean deliveries in Ethiopia: a prospective cohort study. PLoS One. 2021;16(11):e0258742. doi:10.1371/journal.pone.0258742
26. Weiner E, Bar J, Fainstein N, et al. The effect of a program to shorten the decision-to-delivery interval for emergent cesarean section on maternal and neonatal outcome. Am J Clin Exp Obstet Gynecol. 2014;210(3):224.e1–224. e6. doi:10.1016/j.ajog.2014.01.007
27. Sayegh I, Dupuis O, Clement H, Rudigoz R. Evaluating the decision-to-delivery interval in emergency caesarean sections. Eur J Obstetrics Gynecol Reprod Biol. 2004;116(1):28–33. doi:10.1016/j.ejogrb.2004.01.032
28. Prawitasari S, Widyandana D, Hakimi M, Utarini A. Decision to Delivery Interval in Emergency Cesarean Section at Two Academic Hospitals in Yogyakarta and Central Java, Indonesia. Bali Med J. 2021;10(1):266–272. doi:10.15562/bmj.v10i1.2030
29. Kolås T, Hofoss D, Øian P. Predictions for the decision-to-delivery interval for emergency cesarean sections in Norway. Acta obstetricia et gynecologica Scandinavica. 2006;85(5):561–566. doi:10.1080/00016340600589487
30. Tuuli MG, Odibo AO, Fogertey P, Roehl K, Stamilio D, Macones GA. Utility of the bladder flap at cesarean delivery: a randomized controlled trial. Obstetrics Gynecol. 2012;119(4):815–821. doi:10.1097/AOG.0b013e31824c0e12
 © 2024 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2024 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.