Back to Journals » Journal of Healthcare Leadership » Volume 16
Crafting Tomorrow’s Medical Leaders: Insights from Medical Students and Interns in Saudi Arabia
Authors Albednah FA , Albishri SB , Alnader RY, Alwazzan L
Received 2 December 2023
Accepted for publication 8 March 2024
Published 13 March 2024 Volume 2024:16 Pages 141—156
DOI https://doi.org/10.2147/JHL.S452919
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 4
Editor who approved publication: Professor Zhanming Liang
Fahed A Albednah,* Saad B Albishri,* Raghad Y Alnader,* Lulu Alwazzan*
College of Medicine, Imam Mohammad Ibn Saud Islamic University (IMSIU), Riyadh, Saudi Arabia
*These authors contributed equally to this work
Correspondence: Fahed A Albednah, Email [email protected]
Introduction: Leadership is increasingly recognized as a crucial competency in medicine, with physicians expected to provide leadership skills throughout their careers. This study explores the perceptions, attitudes, and interests of medical students and interns in Saudi Arabia regarding medical leadership. Medical graduates are expected to “provide leadership skills that enhance team functioning, the learning environment, and the healthcare delivery system”, according to the Association of American Medical Colleges (AAMC).
Methods: A cross-sectional study was conducted from January to July 2023, involving 519 medical students and interns in Saudi Arabia. An online survey covered demographic data, perceptions, attitudes, interests, and self-perceived leadership skills. A pilot study was conducted to ensure the questionnaire’s validity and reliability. Data were analyzed using SPSS 26, employing descriptive statistics and inferential tests.
Results: Most participants had a positive perception of leadership (38.3%), with higher scores associated with medical specialties as a career choice (p < 0.001). The majority expressed average interest in medical leadership (29.1%). Communication and organizational skills were highly self-rated leadership attributes. Barriers to leadership implementation included lack of interest (49.3%), inadequate training (45.1%), and time constraints (43.2%). Only 14.6% rated leadership education in medical school as “very good”.
Conclusion: This study underscores the importance of leadership in medical education. Integrating comprehensive and structured leadership programs into medical curricula, addressing barriers, and promoting awareness can foster future medical leaders. Continuous evaluation and adaptation are essential for ensuring the relevance and effectiveness of leadership training.
Keywords: medical leadership, medical education, medical students, Saudi Arabia, medical curricula
Introduction
Leadership is essential in medicine. Almost all physicians assume substantial leadership duties throughout their careers. For medical students, leadership has become a crucial competency. Medical graduates are expected to “provide leadership skills that enhance team functioning, the learning environment, and the healthcare delivery system”, according to the Association of American Medical Colleges (AAMC).1,2 Although “management” and “leadership” are sometimes used interchangeably, they typically refer to different strategies for bringing about change. Most experts consider that leaders motivate, inspire, and coordinate plans to provide direction for individuals and the systems in which they operate. In contrast, managers are process-oriented and employ problem-solving to direct individuals and resources to meet goals previously defined by leadership.3 Leadership and management skills are seen as critical aspects of postgraduate medical education. However, for engagement to be effective, it must begin early in medical training. Undergraduate medical education concentrates on disease diagnosis and management, with little emphasis on the systems concerns surrounding healthcare delivery and results or the team effort available to deliver safe and high-quality healthcare.3 The need to have clinical leadership has sparked the adoption of leadership training across multiple medical schools in their curricula. According to the Association of American Medical Colleges, one of the core expectations for medical students entering residency is leadership competency.2 A Systemic review published in 2017 illustrated the correlation between leadership styles and measures of quality care was robustly established. Leadership emerged as a fundamental element crucial for the seamless and integrated delivery of care, a recognition shared by both patients and healthcare professionals.4
Globally, numerous studies have explored the subject of medical leadership on an international scale. A cross-sectional study was conducted in 2015–2016, and 2349 final-year students from ten United Kingdom (UK) medical schools received an online questionnaire. According to the survey, UK medical students desired and recognized the value of management and leadership training, but they believed they needed adequate instruction in these areas. This demonstrates a discrepancy between the need for management and leadership training and the quality of training offered by UK medical schools.5 A 2020 systematic review of medical students’ preparedness for leadership roles in clinical practice found that students perceived leadership as hierarchical and were less prepared to take up clinical leadership roles.6 Moreover, a qualitative study conducted in Qatar explored the incorporation of leadership competencies into the curriculum of a US medical college in Qatar. The research delved into the perspectives of both medical students and faculty regarding the integration of leadership in the medical curriculum. Findings revealed that 79% of survey respondents viewed leadership as a core competency, yet 55% believed that students were not adequately taught leadership skills. Insights from focus groups and interviews highlighted students advocating for increased emphasis on leadership training, while faculty suggested that leadership, though beneficial, was implicitly integrated into the curriculum. Additionally, faculty members emphasized the necessity for further research before explicitly implementing leadership training.7
Up to our knowledge, only two studies have been conducted in Saudi Arabia regarding medical leadership. A study was conducted among medical students at King Abdulaziz University (KAU), Jeddah, Saudi Arabia, aiming to determine the perceptions and attitudes of medical students toward medical leadership and management. Most medical students have acknowledged the importance of a clinician’s medical leadership obligations, and most believe there should be more medical leadership training opportunities during their undergraduate years.8 Another study was conducted among medical students in Riyadh, Saudi Arabia to evaluate their perception and attitudes towards leadership training. The findings underscored the considerable importance assigned to physician leadership within the community, as evidenced by the high ratings given by students. Totally, more than half of the participating students expressed a strong inclination for additional training across various leadership domains. A majority of students, exceeding 50%, indicated a keen interest in incorporating mentoring or coaching, classes specifically designed for younger learners with training, and leadership courses into the curriculum to enhance their leadership skills.9 Nonetheless, these studies possess limitations stemming from inconsistencies in the application of the measurement tool, as well as the lack of statistical validation for the tools used. Furthermore, the scope of the research was confined to specific cities, thereby limiting the generalizability of the findings to the broader landscape of medical leadership across the entire nation’s medical schools. Overall, there is a widespread need for comprehensive studies on medical leadership throughout the nation in Saudi Arabia.
This study has four aims. First, to assess the perceptions and attitudes of medical students/interns toward medical leadership in Saudi Arabia. Second, to determine medical students’/interns’ interest in medical leadership in Saudi Arabia. Third, to identify an association between the specialty of choice and interest in medical leadership in Saudi Arabia. Finally, to evaluate the self-perception of medical students/interns regarding their leadership skills.
Methods
Study Design
This observational cross-sectional study was conducted in Saudi Arabia from January 2023 to July 2023. The study population involved all clinical-year medical students (fifth year and sixth year) and interns (seventh year) living in Saudi Arabia. A convenient sampling method was implemented. Data collectors distributed the survey to all medical students and interns through emails and messaging apps. The progress of data collectors was monitored on a weekly basis.
Data Collection Tool
Participants were requested to complete an online survey. The questionnaire was divided into 4 sections. The first section involved medical students’/interns’ demographic data and their future current choice of specialty. The second section assessed medical students’/interns’ perceptions, attitudes, and interests toward medical leadership. The third section evaluated the self-perception of medical students/interns regarding their leadership skills. The fourth section described the current medical leadership education and training in medical schools and the definition of medical leadership according to the participants.
The questionnaire was based on two studies, one in the United Kingdom and one in Qatar, that assessed medical students’ attitudes, perceptions, and interests in medical leadership.5,7 Both studies developed instruments based on the current literature and conducted a pilot study to ensure face validity and clarity. In our study, a combination of both surveys was implemented to measure the attitudes, perceptions, and interests of medical students/interns in medical leadership. Items regarding self-perception of medical leadership skills were derived from the UK study,5 which developed questions based on the Medical Leadership Competency Framework (MLCF). Items from the fourth section were also based on questions utilized in both studies. In total, the survey contains 36 items. The perception, attitude, and interest of medical students/interns toward medical leadership have been assessed using a 12-item scale (4 items each), with 5-point Likert scale categories ranging from “strongly disagree” coded with 0 to “strongly agree” coded with 4 as the answer option. The total score for each domain has been calculated by adding all items: perception (4 items), attitude (4 items), and interest (4 items). Scores ranging from 0 to 16 points were achieved. The higher the score, the higher the perception/attitude/interest toward medical leadership. The cutoff points of <50%, 50% to 75%, and >75% were used to classify the scores of medical students/interns as poor/negative/low, moderate/neutral/average, and good/positive/high levels. Concerning the specialty of choice, the identified “medical specialties” comprised dermatology, emergency medicine, family medicine, internal medicine, neurology, pediatrics, psychiatry, and radiology. Meanwhile, the designated “surgical specialties” included anesthesiology, ENT (ear, nose, and throat), general surgery, neurosurgery, OB/GYN (obstetrics/gynecology), ophthalmology, orthopedics, pediatric surgery, plastic surgery, and urology. Any specialty selected by the participants that did not align with these predefined categories was systematically classified as “others” in the study. A pilot study was conducted to ensure the questionnaire’s validity and reliability.
Pilot Testing
Face Validity
The survey was presented to 3 experts in research after its initial establishment. They revised the content of the sheet, improved it, and then affirmed using it. After that, the questionnaire was proposed to a linguist to check the appropriateness of wording, grammar, and language use, and some enhancement was done. A pilot study (involving 26 participants) was conducted to ensure that the understanding of the targeted population toward the questionnaire is uniform with no flaws and that the gathered information is sufficient to serve the study objectives.
Content Validity
The survey was directed to three different experts in medical education, who were asked to read the goals and comprehensively examine the questionnaire by utilizing three measures: “essentiality”, “relevance”, and “clarity”. The essentiality of each item was ranked as either “Essential”, “Not essential but useful”, or “Not essential”. The relevance and clarity of each item were placed on two separate scales as either “Highly relevant/clear”, “Quite relevant/clear”, “Somewhat relevant/clear”, or “Not relevant/clear”. The content validity ratio (CVR) was calculated using the Lawshe method. Items with CVR values below 0.62 were considered for modification or deletion. Only one item was recommended to be deleted. Only item 3 (all dimensions): The item has a CVR value below the acceptable threshold, indicating that the experts did consider it essential, relevant, or clear.10
Reliability
A pilot study was conducted among 26 medical students/interns. Students were asked to complete the final version of the questionnaire. Cronbach’s alpha was calculated to check the statistical reliability of the following parts of the questionnaire (assessment of perception, attitude, and interest of medical students/interns toward medical leadership). Cronbach’s alpha for the assessment of perception toward medical leadership (4 items) was 0.725; for the assessment of attitude toward medical leadership (4 items), it was 0.710; and for the assessment of interest toward medical leadership (4 items), was 0.774, which proved statistical validity in all of these parts respectively.
Ethical Consideration
Based on the Declaration of Helsinki, Institutional Review Board approval was obtained from the Medical Research Unit, College of Medicine, Imam Mohammad ibn Saud Islamic University, Riyadh, Saudi Arabia, Project Number 418/2023, on January 20, 2023.
Participation in this study was voluntary; participants were notified of their consent and invited to participate. Participants did not earn a material income due to their participation.
Statistical Analysis
The data were analyzed using the software program Statistical Packages for Software Sciences (SPSS) version 26 (Armonk, New York, IBM Corporation, USA). Descriptive statistics were given as numbers and percentages (%) for all categorical variables, while continuous variables were calculated and summarized as mean and standard deviation. The differences in the perception, attitude, and interest scores have been conducted using the Mann–Whitney Z-test and the Kruskal Wallis H-test. Normality tests were performed using the Shapiro–Wilk test and the Kolmogorov–Smirnov test. The perception, attitude, and interest scores follow the normal distribution. Thus, the parametric tests were applied. A paired sample t-test was used to determine the difference between pre and post-PISQ-IR scores. Values were considered significant with a p-value of less than 0.05.
Results
This study enrolled 519 medical students and interns. Table 1 describes the medical students/interns’ socio-demographic characteristics. Nearly all were Saudis (92.9%), and 36.6% were medical interns. Students who had a 4 to 4.49 GPA constitute 28.3%. In addition, 50.1% preferred surgical specialties. Figure 1 Display the distribution of responses among medical colleges in Saudi Arabia. Most medical students/interns believe leadership training should be gained during a medical career through problem based learning (PBL) (45.5%), followed by residency training (43.7%) and during the Internship (34.9%) (Figure 2).
 |
Table 1 Socio-Demographic Characteristics of Medical Students and Interns (n=519) |
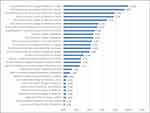 |
Figure 1 Distribution of responses among medical colleges in Saudi Arabia. |
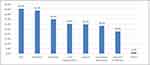 |
Figure 2 Perceptions regarding where leadership training should take place in a medical career. |
Figure 3 illustrates that the primary obstacle to implementing leadership during clinical training was the lack of interest (49.3%), followed by inadequate training (45.1%) and lack of time (43.2%). It was observed that 38.1% of the medical students/interns indicated “The ability to handle responsibilities and make decisions in the medical field” as the best meaning of medical leadership (Figure 4). Additionally, medical students/interns provided definitions of medical leadership in their own words (Supplementary File 1). Regarding self-perception of leadership skills, on a scale of 5 points, communication ideas showed the highest ratings (mean score: 2.67), followed by organization (mean score: 2.61) and acting with integrity (mean score: 2.61) (Figure 5).
 |
Figure 3 Perceived barriers to the implementation of leadership in clinical training. |
 |
Figure 4 Perceived meaning of medical leadership. |
 |
Figure 5 Mean ratings for the self-perception of the leadership skills. |
Table 2 indicates the current leadership education/training and the definition of medical leadership; merely 13.3% reported a “very good” rating in terms of leadership training and education they received during their time in medical school. Additionally, only 14.6% strongly agreed that leadership skills are taught across multiple courses/blocks/rotations in their medical school, and 3.5% strongly agreed that their medical school prioritizes leadership training during clinical rotations. The most common insight of leadership as a core competency of physicians was that “Leadership encompasses important skills such as decision-making, communication, empathy, etc”. (66.1%).
 |
Table 2 Current Leadership Education/Training and the Definition of Medical Leadership (n=519) |
Table 3 presents the assessment of perceptions, attitudes, and interest of medical students/interns towards medical leadership. In the context of perception toward medical leadership, it was noted that the statement “Leadership is a core role that is required to succeed in the medical profession” received the highest rating, with a mean score of 2.77. The total mean perception based on the 4 items was 10.4 (SD 4.32), with poor, moderate, and good perception found in 21.4%, 40.3%, and 38.3%, respectively. Regarding attitude toward medical leadership, it was observed that the rating was highest in the statement, “I think that students should have leadership responsibilities during their clinical training” (mean score: 2.68). The overall mean score of attitude toward medical leadership was 10.3 (SD 4.16). Accordingly, 17.9%, 47%, and 35.1% were considered negative, neutral, and positive attitude levels. As for the interest in medical leadership, it was shown that the highest rating was seen in the statement, “I think clinician’s managerial/leadership opportunities should be highlighted and promoted to medical students” (mean score: 2.74). Accordingly, we found 19.8%, 51.1%, and 29.1%, accounting for low, average, and high-interest levels.
 |
Table 3 Assessment of the Perception, Attitude and Interest Toward Medical Leadership (n=519) |
When measuring the differences in the score of perception according to the socio- demographic characteristics and general awareness about medical leadership (Table 4), it was observed that a higher perception score was more associated with being 5th-year medical students (H=10.404; p=0.006), medical specialties as a future career preference (H=25.828; p<0.001), knowledge of leadership gained through PBLs (Z=7.081; p<0.001), case-based discussion (Z=1.938; p=0.049), lectures (Z=6.760; p<0.001), residency training (Z=3.208; p=0.001), and research endeavors (Z=2.468; p=0.014), and barriers to face in the implementation of leadership in clinical training, such as inadequate training (Z=8.771; p<0.001), lack of time (Z=3.595; p<0.001) and lack of interest (Z=1.958; p=0.025), while the perception score was significantly less among students with GPA lower then 3 (H=34.034; p<0.001), barriers to facing the implementation of leadership in training, such as inadequate budget (Z=3.044; p=0.002) and not seen as necessary (Z=3.215; p=0.001).
 |
Table 4 Differences in the Score of Perception in Relation to the Socio-Demographic Characteristics of the Medical Students/Interns and General Awareness About Medical Leadership (n=519) |
It was observed that a higher attitude score was more associated with non-Saudis (Z=3.802; p<0.001), being a 5th-year medical student (H=10.509; p=0.005), medical specialties as a future career choice (H=28.890; p<0.001), knowledge about leadership training gained during PBLs (Z=7.771; p<0.001), case-based discussion (Z=2.471; p=0.013), lectures (Z=6.386; p<0.001), Internship (Z=2.594; p=0.009), residency training (Z=3.294; p=0.001) and during research endeavors (Z=3.310; p=0.001), and believed that inadequate training (Z=7.929; p<0.001), lack of time (Z=4.902; p<0.001) and lack of interest (Z=2.635; p=0.008) are barriers to implementation of leadership in clinical training, while the attitude score was significantly less among those with less than 3 GPA (H=37.138; p<0.001) and believed that inadequate budget is a barrier to facing the implementation of leadership in clinical training (Z=4.260; p<0.001) (Table 5).
 |
Table 5 Differences in the Score of Attitude in Relation to the Socio-Demographic Characteristics of the Medical Students/Interns and General Awareness About Medical Leadership (n=519) |
Higher interest score was more associated with non-Saudis (Z=3.456; p=0.001), being 5th-year medical students (H=37.101; p<0.001), having medical specialties as a future career choice (H=32.199; p<0.001), knowledge gained in leadership training during PBLs (Z=7.990; p<0.001), case-based discussion (Z=4.116; p<0.001), lectures (Z=3.279; p=0.001), residency training (Z=3.419; p=0.001), and research endeavors (Z=5.334; p<0.001), and barriers to face in the implementation of leadership in clinical training, such as inadequate training (Z=9.232; p<0.001) and lack of time (Z=3.987; p<0.001), while the interest score was significantly less among students with less than 3 GPA (H=33.500; p<0.001) and those who believed that inadequate budget was a barrier to the implementation of leadership in clinical training (Z=3.209; p=0.001) (Table 6).
 |
Table 6 Differences in the Score of Interest in Relation to the Socio-Demographic Characteristics of the Medical Students/Interns and General Awareness About Medical Leadership (n=519) |
Discussion
Perceptions, Attitudes, and Interest in Medical Leadership Among Medical Students and Interns
Up to our knowledge, this is the first national study to be conducted aimed at determining the perception, attitude, and interest towards medical leadership and their link to the specialty of choice among medical students and interns in Saudi Arabia. Most medical students surveyed had a moderate level of perception (40.3%) towards leadership as a core role that is demanded in the medical field (mean score: 2.77), with the highest perception score associated with medical specialties as a future career preference (H=25.828; p<0.001). This finding is significant as Keluth and Bendriss’s7 paper found that leadership should be a core competency since being a physician comes with the obligation of patient care and ownership. However, in this study, only a minor group of medical students and interns had a very good rating regarding the management and leadership education received during medical school. This points out poor leadership training during their medical career. This is consistent with the findings by Rouhani et al,5 who reported that over 85% of the United Kingdom’s medical students surveyed were not well informed about what a managerial position in medicine entails. A report by the UK General Medical Council supported the findings, which reported that 1 in 10 graduates felt inadequately prepared for practice with core leadership and management competencies as crucial areas of interest.11 In addition, the findings identified a lack of interest, inadequate training, and lack of time as the most common barriers to leadership implementation during clinical training. The findings mirror the systematic review report on the attitudes of medical students to leadership and management conducted by Abbas et al,12 which cited a lack of curriculum time and disinterest in medical students despite the desire for more leadership and management training. Nonetheless, the results established considerable levels of good perception, positive attitude, and high interest in medical leadership and link to specialty choice among medical students and interns despite inadequate training at medical schools. The findings are consistent with the report of the focus group conducted by Quince et al13 involving medical students drawn from medical schools in the United Kingdom, which revealed positive attitude and desire by medical students toward medical leadership responsibilities. The students were more open and accepted the roles of leadership and management education in medical education, although more than half of them rated their training as poor. Furthermore, the findings revealed communication, organizational skills, and integrity as the highest self-rated leadership skills found in medical student/interns. This can be explained by Varkey et al,14 who found qualities such as communication, confidence, integrity, teamwork, and management, among other competencies, to be taught in medical schools and lay proper plans to integrate them across the years of the medical school curriculum and programs. In subsequent research endeavors, it is imperative to explore the evaluation of physicians and their leadership capabilities. For instance, a survey conducted in India aimed at assessing the medical leadership competencies of physicians. Notably, 70% self-evaluated their competencies within the range of “Average to Good”. However, it is noteworthy that the self-assessed competency levels were markedly below the perceived significance of each competency, regardless of demographic variables.15
The Need for Integrating Leadership Training into Medical School
Many studies have supported the need to include leadership training programs for medical students in their undergraduate years.3,16 Despite the crowded nature of undergraduate medical curricula, it is crucial to accord medical leadership the same level of significance as any other subject or topic within the field of medicine. Most of the other specialties require only a few to be leaders in their fields; unlike in medicine, most physicians will assume the role of leaders at some point in their careers. In addition, such a skill will enhance patient care and enable future doctors to engage better with their colleagues and improve their teamwork skills. Despite the acknowledged importance of leadership training, the current study underscores a significant gap in medical education. Only 14.6% of surveyed medical students indicated that leadership skills were incorporated across various courses, blocks, or rotations in medical school. Furthermore, a mere 13.5% agreed on the prioritization of leadership training during clinical rotations. The study identifies a pressing need to establish integrated leadership training, emphasizing the incorporation of evaluations, opportunities for personal leadership development reflections, and interactive sessions to enhance leadership skills. These findings highlight a contrast with a U.S.-based survey assessing the prevalence of formal leadership education in undergraduate medical schools. In that survey, around 54.5% of respondents acknowledged the existence of leadership curricula in their medical schools. Within the 48 schools with formal leadership curricula, various methods of content delivery were employed, including mentoring programs (65.1%), dual degree programs (54.5%), workshops (48.8%), seminar/lecture series (41.9%), courses (41.9%), and single seminars (18.6%). Notably, 34.8% of these curricula were mandatory, 32.6% elective, and another 32.6% included both required and elective components. Moreover, 19% of institutions provided longitudinal leadership education throughout the duration of medical school.17 According to current literature, many programs have been implemented that could increase leadership education and training quality in medical schools. For example, the Duke University Schools of Medicine has implemented a Leadership Education and Development curriculum that spans all four years of medical school.18 The curriculum is centered on the competencies that comprise the Duke healthcare leadership model, intending to not only teach these competencies through certain leadership activities but also intentionally explore and foster leadership skills in the context of experimental learning, particularly in hospital or clinical settings. Moreover, a study was conducted at the University of Colorado Denver School of Medicine. They have designed the LEADS (Leadership Education Advocacy Development Scholarship) program to educate medical students in advocacy skills and community health promotion. The LEADS Track required students to complete advocacy skills courses, a summer internship, and a mentored academic project that addresses population health. Students were matched with a faculty mentor and a community-based group. Students expressed feelings of empowerment, increased self-efficacy, and a higher propensity for future involvement in leadership and health advocacy. Sponsors from the community agree that the experience is worthwhile.19 Furthermore, Brody School of Medicine created a program instructed in their curriculum to train medical students to become better leaders and generate a health system change. This included constructing a distinction track in health system transformation and leadership, known as the Leaders in INnovative Care (LINC) Scholars Program. In eight weeks, selected 15 LINC scholars participated in a summer immersion that was developed to deliver foundational knowledge and practical application. Throughout the period, students have engaged in activities including quality improvement, patient safety, team-based care, and population health aiming to improve their knowledge and skills. Students’ Post-training knowledge mean scores have increased by 17 points from the baseline; also, most students have expressed their immersion experience as favorable and rated the experience as highly valuable or valuable, and 87% to 100% rating each of the intended objectives as successfully fulfilled.20 Ultimately, the integration of a medical leadership curriculum into medical school is a critical step in shaping the future of healthcare, aligning with the goals outlined in the Saudi Vision 2030. This visionary plan recognizes the importance of transforming healthcare services and medical education to meet the evolving needs of society. The Saudi Vision 2030 emphasizes the importance of developing a healthcare system that is effective, efficient, and patient-centered.21 To achieve these goals, it is crucial to produce a generation of medical professionals who can lead and innovate in healthcare delivery.
Recommendations
The study’s findings support a number of recommendations that aim to better medical curricula’s integration of leadership education and training as well as medical students’ and interns’ attitudes, perceptions, and interest in medical leadership:
Improve Leadership Education in Medical Schools
Leadership training should be prioritized in medical schools by providing thorough and structured leadership programs. These programs should be integrated into current curricula and include practical components like workshops, case studies, and mentorship opportunities. Additionally, efforts should be made to ensure that leadership education is provided continuously throughout the medical school journey, including clinical rotations.
Boost Medical Leadership Awareness
In partnership with professional medical organizations, educational institutions should actively increase awareness of the importance of leadership skills in medicine. This can be accomplished through lectures, conferences, and other medical student awareness efforts. Emphasizing that leadership is a core competency for physicians, comprising skills such as decision-making, communication, and empathy, might assist in positively shifting perceptions.
Adapt Leadership Education to a Wide Range of Student Profiles
Understand that there are differences in the backgrounds, interests, and preferences of medical students. Because of this, leadership education needs to be customized to fit the various needs of medical students. The requirements and interests of students pursuing various medical specializations can be addressed by creating specialized tracks or elective courses in leadership.
Collaborate with Clinical Institutions
Collaboration between medical schools and clinical facilities is critical for offering hands-on, real-world leadership training. Leadership components should be included in clinical rotations and internships, allowing students to apply their knowledge in practical settings while also developing key leadership qualities.
Overcome Barriers in the Implementation of Leadership
Efforts should be made to overcome the challenges highlighted to implementing leadership in clinical training. This includes a lack of enthusiasm, insufficient training, and time constraints. Strategies for addressing these issues may include increasing the relevance and applicability of leadership training, improving training quality, and finding efficient ways to integrate leadership education into existing curricula.
Continuous Evaluation and Improvement
Incorporate feedback tools to continuously analyze and change the efficacy of leadership programs. Regular student assessments and comments can assist in identifying areas for development and ensuring that leadership training stays relevant and valuable to aspiring physicians.
Limitations
There are several limitations inherent to this study; the participants are a small select group, and the focus was on the medical schools that they were enrolled in. Our sample size of 519 may not represent the population for which the scale was intended, and our results may be subject to the influence of chance factors. Also, the study employed an observational cross- sectional study, which can only establish the relations between factors but not causalities. A convenience sampling technique was implemented, which might lack generalizability. Therefore, we highlight the need to conduct a more advanced type of sampling.
Additionally, considering that the study utilized online self-administered questionnaires to collect data, it was challenging to discover insights or observe the behavior of respondents in their natural settings.
Conclusion
Overall, this paper sheds light on various crucial aspects of medical leadership and education of medical students/interns. The findings revealed variations in perceptions, attitudes, and interests among the participants. These differences were linked to factors like their academic year, specialty preferences, and exposure to leadership training. Notably, their favored methods for leadership training were problem-based learning and residency training. However, the paper also highlights notable barriers to the implementation of leadership during clinical training. These hurdles were primarily related to a lack of interest, insufficient training, and constraints on time. Participants, in general, associated medical leadership with essential skills such as decision-making, communication, and empathy. A vital finding was the significant gap in leadership education within medical schools, with only a minority of participants reporting high satisfaction with their leadership education. This underscores the urgency of curriculum improvements.
Data Sharing Statement
If considered suitable, the data conveyed in this study are available upon request from the corresponding author.
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Funding
The study is self-funded, and the authors covered funds.
Disclosure
The authors report that there is no conflicts of interest in this work.
References
1. Clyne B, Rapoza B, George P. Leadership in undergraduate medical education: training future physician leaders. RI Med J. 2015;98(9):36–40.
2. Enders T, Conroy I. Advancing the Academic Health System for the Future: A Report for the AAMC Health Advisory Panel. Washington, DC: Association of American Medical Colleges; 2014.
3. Chenm TY. Medical leadership: an important and required competency for medical students. Tzu Chi Med J. 2018;30(2):66–70. doi:10.4103/tcmj.tcmj
4. Sfantou DF, Laliotis A, Patelarou AE, Sifaki-Pistolla D, Matalliotakis M, Patelarou E. Importance of leadership style towards quality of care measures in healthcare settings: a systematic review. Healthcare. 2017;5(4):73. doi:10.3390/healthcare5040073
5. Rouhani MJ, Burleigh EJ, Hobbis C, et al. UK medical students’ perceptions, attitudes, and interest toward medical leadership and clinician managers. Adv Med Educ Pract. 2018;9:119–124. doi:10.2147/AMEP.S151436
6. Barnes T, Yu TCW, Webster CS. Preparedness of medical students and junior doctors for their role as clinical leaders: a systematic review. Med Teach. 2020;42(1):79–85. doi:10.1080/0142159X.2019.1665632
7. Chavan AK, Bendriss R. Leadership curriculum in medical education: exploring student and faculty perceptions in a US Medical School in Qatar. J Healthc Leadersh. 2022;14. doi:10.2147/JHL.S370645
8. Alzahrani SH, Baig M, Omer AR, Algethami MR. Medical students’ perceptions and attitudes toward medical leadership and management. Pak J Med Sci. 2021;37(1):223–228. doi:10.12669/pjms.37.1.2406
9. Alluhaymid Y, Alalwan A, Alobaid N, Alshibani M, Alshaye I. Attitudes toward leadership training among medical students in Riyadh. Arch Clin Biomed Res. 2023;7:248. doi:10.26502/acbr.50170337
10. Lawshe CH. A quantitative approach to content validity. Pers Psychol. 1975;28(4):563–575. doi:10.1111/j.1744-6570.1975.tb01393.x
11. Jagger O. Supporting and driving trainee-led leadership. Future Hosp J. 2015;2(3):211–217. doi:10.7861/futurehosp.2-3-211
12. Abbas MR, Quince TA, Wood DF, et al. Attitudes of medical students to medical leadership and management: a systematic review to inform curriculum development. BMC Med Educ. 2011;11(1):93. doi:10.1186/1472-6920-11-93
13. Quince T, Abbas M, Murugesu S, et al. Leadership and management in the undergraduate medical curriculum: a qualitative study of students’ attitudes and opinions at one UK medical school. BMJ Open. 2014;4(6):e005353. doi:10.1136/bmjopen-2014-005353
14. Varkey P, Peloquin J, Reed D, et al. Leadership curriculum in undergraduate medical education: a study of student and faculty perspectives. Med Teach. 2009;31(3):244–250. doi:10.1080/01421590802144278
15. Gulati K, Sarkar C, Verma V, Singh AR, Gupta SK. Assessment of medical leadership competencies and development needs: first comprehensive study from India. Int J Healthc Manage. 2021;14(2):363–374. doi:10.1080/20479700.2019.1647381
16. Riaz S, Tabassum M. A need analysis for teaching leadership skills to medical students in Pakistan. J Ayub Med Coll. 2021;33(1):75–81.
17. Neeley SM, Clyne B, Resnick-Ault D. The state of leadership education in US medical schools: results of a national survey. Med Educ Online; 2017;22;1:1301697. doi:10.1080/10872981.2017.1301697
18. Leadership Education and Development (LEAD) Curriculum. Duke University School of Medicine. 2022. https://medschool.duke.edu/education/health-professions-education/doctor-medicine-md-program/curriculum/longitudinal-0.
19. Long JA, Lee RS, Federico S, et al. Developing leadership and advocacy skills in medical students through service learning. J Public Heal Manag Pract. 2011;17(4):369–372. doi:10.1097/PHH.0b013e3182140c47
20. Lawson L, Lake D, Lazorick S. Developing tomorrow’s leaders: a medical student distinction track in health system transformation and leadership. Acad Med; 2019;94(3):358–363. doi:10.1097/ACM.0000000000002509
21. Saudi vision. Kingdom of Saudi Arabia; 2023. https://vision2030.gov.sa/
 © 2024 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2024 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
