Back to Journals » ClinicoEconomics and Outcomes Research » Volume 15
Cost Analysis of High-Flow Oxygen Therapy Compared with Conventional Oxygen Therapy in Severe COVID-19 in Colombia: Data from a Randomized Clinical Trial
Authors Prada SI , Garcia-Garcia MP, Ospina-Tascón GA, Rosselli D
Received 16 March 2023
Accepted for publication 30 August 2023
Published 6 October 2023 Volume 2023:15 Pages 733—738
DOI https://doi.org/10.2147/CEOR.S412087
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Professor Giorgio Colombo
Sergio I Prada,1,2 Maria P Garcia-Garcia,1 Gustavo A Ospina-Tascón,3,4 Diego Rosselli5
1Fundación Valle del Lili, Centro de Investigaciones Clínicas, Cali, Colombia; 2Universidad Icesi, Centro PROESA, Cali, Colombia; 3Department of Intensive Care, Fundación Valle del Lili, Cali, Colombia; 4Translational Medicine Laboratory in Critical Care (TransLab-CCM), Universidad Icesi, Cali, Colombia; 5Clinical Epidemiology and Biostatistics Department, Pontificia Universidad Javeriana, Bogota, Colombia
Correspondence: Sergio I Prada, Centro de Investigaciones Clínicas, Fundación Valle del Lili, Cra. 98 18-49, Cali, Valle, Colombia, Email [email protected]
Background: A randomized clinical trial (HiFlo-COVID-19 Trial) showed that among patients with severe COVID-19, treatment with high-flow oxygen therapy (HFOT) significantly reduced the need for invasive mechanical ventilation support and time for clinical recovery compared with conventional oxygen therapy (COT). However, the cost of this strategy is unknown.
Objective: We examined total cost of HFOT treatment compared with COT in real-world setting.
Methods: We conducted a post-trial-based cost analysis from the perspective of a managed competition healthcare system, using actual records of billed costs. Cost categories include general ward, intensive care unit, procedures, imaging, laboratories, medications, supplies, and others.
Results: A total of 188 participants (mean age 60, 33% female) were included. Average costs (and standard deviation) in the HFOT group were USD $7992 (7394) and in the COT group USD $ 10,190 (9402). Differences, however, did not reach statistical significance (P=0.093). However, resource use was always less costly for the HNFO group, with an overall percentage decrease of 27%. Two categories make up 72% of all savings: medications (41%) and intensive care unit (31%).
Conclusion: For patients in ICU with severe COVID-19 the cost of treatment with HFOT as compared to COT is likely to be cost-saving due to less use of medications and length of stay in ICU.
Keywords: SARS-CoV-2, COVID-19, cost analysis, economic evaluation, high-flow nasal oxygen, conventional oxygen therapy, high-flow oxygen therapy, clinical trial, cost, Colombia
Introduction
Most COVID-19 patients have either asymptomatic or mild disease,1 but those progressing to acute hypoxemic respiratory failure impose a substantial burden on health care systems.2,3 In pre-pandemic conditions, acute hypoxemic respiratory failure from etiologies different from SARS-CoV-2 infection has been related to significant increases in both hospital and Intensive Care Unit (ICU) length of stay and overall medical expenses, with cost estimations around USD 54.3 billion in the United States in 2009.4
In general, the management of hypoxemic respiratory failure relies on oxygen supplementation aiming to improve oxygenation and support respiratory effort by using various techniques ranging from low flow oxygen systems up to invasive mechanical ventilation and Extracorporeal Membrane Oxygenation (ECMO). During the early stages of the COVID-19 pandemic, there was no high-quality evidence about the best approach for the most severe cases of respiratory. Early observations reported an unexpected high mortality among patients under invasive mechanical ventilation,5 and some reports warned about the risks of early intubation and mechanical ventilation.6 The use of ECMO in severe COVID-19 also led to conflicting results,7,8 contributing to increased uncertainties. As SARS-CoV-2 pandemic progressed, critical care physicians recognized that respiratory support in severe COVID-19 cases should not have differed from usual care of acute hypoxemic respiratory failure, and non-invasive respiratory support techniques use increased progressively.9
High-flow Oxygen Therapy (HFOT) through a nasal cannula is a technique whereby heated and humidified oxygen is delivered to the nose at high flow rates, improving oxygenation and reducing breathing effort.10,11 Pre-pandemic data suggested that high flow nasal cannula might decrease the need for tracheal intubation and reduce the risk of escalation of oxygen therapy in patients with acute respiratory hypoxemic failure,12,13 with no apparent impact on mortality rates.13–15 Similarly, preliminary data in patients with severe COVID-19 suggested that HFOT could prevent tracheal intubation,9,16 at the same time, two randomized clinical trials concluded that among patients with severe COVID-19, use of high-flow oxygen through a nasal cannula significantly decreased the need for mechanical ventilation support and time to clinical recovery compared with Conventional (low-flow) Oxygen Therapy (COT).17,18 A recent systematic review of 23 mostly observational studies suggests that HFOT compared to COT was associated with reduced need for invasive ventilation and shorter length of stay (LOS).19
Few publications have addressed the cost-effectiveness of HFOT. Studies from United Kingdom and Australia show that HFOT reduced costs by reducing LOS and overall resources.20,21 In this study, we aimed to measure cost differences between HFOT and COT in patients with severe COVID-19 in three Colombian hospitals, based on data from a multicenter clinical trial.17
Materials and Methods
From August 2020 to January 2021, a randomized open-label clinical trial was conducted in the general wards, emergency rooms and ICU in three hospitals in Colombia. A total of 220 adults (18 years and older) with severe COVID-19 were randomized to HFOT through a nasal cannula vs COT to assess hospital length of stay, need for intubation and mechanical ventilation, and time for clinical recovery, evaluated in a 28-day period (more details on the protocol can be found in ClinicalTrials.gov identifier: NCT04609462, the acronym for trial is HiFLo trial).17 The original protocol included only clinical data; no resource use analysis was planned. In this study, a post-trial cost analysis using administrative data corresponding solely to our center was conducted.
We took the perspective of the Colombian healthcare system and included only direct healthcare-related costs; societal costs were not considered. Colombia’s health system is best described as a managed competition. Costs were recorded in Colombian pesos (COP) by the hospital administrative billing system but are reported in this paper in 2021 US dollars, after using an exchange rate of 3800 COP per 1 USD. Costs for both groups were categorized as general ward, ICU, imaging, laboratories, medications, procedures, supplies, and other costs. Since patients were billed at different unitary prices due to different negotiations with insurers, we standardized unitary prices using the charge fee schedule of the insurer with the most patients in the data set.
We calculated the mean unadjusted and adjusted total cost for the patient’s entire stay. Cost models are adjusted for age (<60 and ≥60 years), ratio of partial pressure of arterial oxygen to fraction of inspired oxygen (PaO2/FIO2) at randomization, and comorbidities (arterial hypertension, diabetes, obesity [body mass index >30 kg/m2], chronic obstructive pulmonary disease, kidney failure, heart failure, and Child-Pugh class A-B liver cirrhosis). We used generalized linear models to compare total costs between groups, using a gamma distribution and log-link function, adjusting for baseline characteristics. We compared the fit of candidate models (linear regression, linear regression of log total costs, gamma log distribution, and inverse Gaussian distribution), and found that the gamma model with identity link performed the best based on mean absolute error, root mean squared error, pseudo-R squared, probability plots, and quantile–quantile plots. There was no need for an uncertainty analysis since data used corresponded to actual records on the institutional billing charts. Analyses were undertaken using Stata, version 16.0 (College Station, TX). The study protocol was approved by our institutional review board.
Results
The multicenter trial analyzed 199 patients, 99 patients were randomly assigned to receive HFOT through a nasal cannula and 100 to COT.17 Due to confidentiality restrictions, we were only allowed to access cost data in our hospital, which enrolled most patients in the trial. We included in this paper 94 (50%) participants from the COT group and 94 (50%) from the HFOT group (Table 1). Overall, the median age was 60 years old (range 26–88), and 62 (33%) were females. Comorbidities included hypertension in 77 (41%) patients and diabetes in 36 (19%). Patients were treated either in the hospital general ward/emergency room or ICU, 18 (19%) patients from both HFOT and CTO were treated in the former, and 76 (81%) in each group in the latter. Most patients were treated both in the general ward and the ICU, except for 9 patients (10%) in the HFOT group and 12 (13%) in the COT group that were hospitalized directly in the ICU; 5 patients (5%) in the HFOT group and 4 (4%) in the COT group did not require ICU. A total of 23 patients (5 females) died during the trial, 8 in the HFOT group and 15 in the COT group.
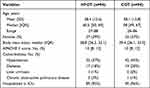 |
Table 1 Baseline Participant Characteristics |
Average and median costs, by category, for both groups are depicted in Table 2. Total direct healthcare costs for the health system were 27% lower in the HFOT group versus the COT group, and the HFOT group was less costly in each cost category. Three categories make up 72% of all savings: Medications (41%) and ICU (31%). Notice the wide standard deviations in all cost categories, and that median costs are always well below the mean costs.
 |
Table 2 Mean and Median Costs, by Category, of Patients in Each Group |
Table 3 gives an adjusted mean cost comparison per patient for both groups. Adjusted mean differences are negative for all cost categories and for total cost per patient. Two categories achieve statistical significance in the cost difference at the conventional 5% threshold: imaging and clinical laboratories. Total cost was statistically significant at a 10% threshold, as well as the ICU category.
 |
Table 3 Adjusted Comparison of Costs in the Hi-Flo Trial |
Discussion
We conducted a post-trial-based cost analysis of the HFOT and COT interventions using the data of a recent randomized clinical trial. Even though no statistically significant differences in costs were found at the conventional 5% threshold, results showed HFOT costs consistently lower than COT costs, both overall total direct healthcare costs and costs per category. Moreover, medications and ICU stay accounted for almost three quarters of total savings.
A 2016 NHS study on HFOT cost-effectiveness in acute respiratory failure patients found a cut-off point of a difference of maximum 4% intubated patients when compared to standard oxygen in order to generate cost-savings, authors estimated cost savings of £364 per patient pre intubation and £144 per patient post-intubation.20 Similarly, Fealy et al, in a cost saving simulation in HFOT, calculated the cost of oxygen therapy as the number of oxygen devices used on per-patient. The authors reported a consumable cost saving per patient with HFOT associated with a significant difference in the number of intubations, more patients discharged from ICU and fewer patients using three or more oxygen delivery devices.21 These studies are the only two papers that report costs in the literature. Our study coincides with the main conclusion of both that HFOT is cost-saving. Similarly, both studies found that the main drivers are lower length of stay in the ICU and lower use of consumables. However, our study is the first one to use real-world data evidence in a COVID-19 setting based on an RCT, as opposed to the previous literature that use models and simulation data, thus providing stronger evidence in a high-stakes context (COVID-19).
We found a mean expenditure of a patient under COT to be USD 2198 more than a HFOT patient, which would translate in 27% cost savings, comparatively higher than the figures reported in the literature. These findings suggest that HFOT in adult patients with severe COVID-19 infection as first-line oxygen management therapy does not result in higher hospitalization expenditure. In the HiFLo trial, the use of high-flow oxygen through a nasal cannula when compared to COT in patients with severe COVID-19 reported a significant decrease in need for mechanical ventilation support (66%) and time for clinical recovery within 28 days (11 days vs 14 days), with no difference in hospital length of stay.17
Reduced costs may also be explained by clinically improving patients’ respiratory condition, potentially reducing associated complications, diminishing the need of additional interventions, in addition to decreasing days required in the ICU, thereby reducing costs of procedures, medication, physicians’ fees, and ultimately overall total hospital stay costs, while possibly favoring bed turnover providing healthcare for all in a pandemic.
The main clinical trial was conducted between the first and second COVID-19 wave in Colombia, which may limit extrapolation of results. This study was performed in a high complexity hospital, with trained specialized personnel in critical care, which is exceptional in our socioeconomic context. Moreover, the trial was designed to obtain clinical results, and resource use or overall costs were not part of the original outcomes.
Despite the apparent difference in overall costs, and in each one of the categories analyzed, the overall result did not reach statistical significance at the conventional p = 0.05 level. Sample size, which was estimated for the clinical outcomes, may be part of the explanation. Additionally, healthcare costs in complex situations tend to have a peculiar distribution, with a long tail at the high end.22 This variability in the distribution, which is represented by wide standard deviations and median values well below the mean, may also add to the complexity of the analyses required to establish true differences. A larger-scale RCT would be needed in order to prove if the trend we found reaches that threshold conventionally established for statistical significance.
Conclusions
For patients in ICU with severe COVID-19 the cost of treatment with HFOT as compared to COT is likely to be cost-saving due to less use of medications and length of stay in ICU.
Data Sharing Statement
The cost data that support the findings of this study are available from corresponding author upon request.
Ethics Approval
This study was conducted in accordance with the principles of the Declaration of Helsinki, Ethics approval was granted by Fundación Valle del Lili’s ethical committee. Informed consent was obtained from all individual participants included in the study. Consent to publish has been granted by all authors.
Acknowledgment
This paper was accepted for poster presentation at ISPOR 2023 in Boston, MA, USA. The abstract was indexed and published at the conference proceedings.
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Funding
Fundación Valle del Lili.
Disclosure
The authors declare no competing interests in this work.
References
1. Wu Z, McGoogan JM. Characteristics of and important lessons from the coronavirus disease 2019 (COVID-19) outbreak in China: summary of a report of 72 314 Cases from the Chinese Center for Disease Control and Prevention. JAMA. 2020;323(13):1239–1242. PMID: 32091533. doi:10.1001/jama.2020.2648
2. Grasselli G, Zangrillo A, Zanella A, et al. Baseline characteristics and outcomes of 1591 patients infected with SARS-CoV-2 admitted to ICUs of the Lombardy Region, Italy. JAMA. 2020;323(16):1574–1581. doi:10.1001/jama.2020.5394
3. Rosselli D. COVID-19 in Colombia: the first 90 days. Acta Neurol Colomb. 2020;36(1):1–6. doi:10.22379/24224022287
4. Lee CC, Mankodi D, Shaharyar S, et al. High flow nasal cannula versus conventional oxygen therapy and non-invasive ventilation in adults with acute hypoxemic respiratory failure: a systematic review. Respir Med. 2016;121:100–108. doi:10.1016/j.rmed.2016.11.004
5. Richardson S, Hirsch JS, Narasimhan M, et al. Presenting characteristics, comorbidities, and outcomes among 5700 patients hospitalized with COVID-19 in the New York City area. JAMA. 2020;323(20):2052–2059. doi:10.1001/jama.2020.6775
6. Tobin MJ. Basing respiratory management of COVID-19 on physiological principles. Am J Respir Crit Care Med. 2020;201(11):1319–1320. doi:10.1164/rccm.202004-1076ED
7. Lebreton G, Schmidt M, Ponnaiah M, et al. Extracorporeal membrane oxygenation network organisation and clinical outcomes during the COVID-19 pandemic in Greater Paris, France: a multicentre cohort study. Lancet Respir Med. 2021;9(8):851–862. doi:10.1016/S2213-2600(21)00096-5
8. Barbaro RP, MacLaren G, Boonstra PS, et al. Extracorporeal membrane oxygenation for COVID-19: evolving outcomes from the International Extracorporeal Life Support Organization Registry. Lancet. 2021;398(10307):1230–1238. doi:10.1016/S0140-6736(21)01960-7
9. Demoule A, Vieillard Baron A, Darmon M, et al. High-flow nasal cannula in critically ill patients with severe COVID-19. Am J Respir Crit Care Med. 2020;202(7):1039–1042. doi:10.1164/rccm.202005-2007LE
10. Mauri T, Turrini C, Eronia N, et al. Physiologic effects of high-flow nasal cannula in acute hypoxemic respiratory failure. Am J Respir Crit Care Med. 2017;195(9):1207–1215. doi:10.1164/rccm.201605-0916OC
11. Mauri T, Alban L, Turrini C, et al. Optimum support by high-flow nasal cannula in acute hypoxemic respiratory failure: effects of increasing flow rates. Intensive Care Med. 2017;43(10):1453–1463. doi:10.1007/s00134-017-4890-1
12. Frat JP, Thille AW, Mercat A, et al. High-flow oxygen through nasal cannula in acute hypoxemic respiratory failure. N Engl J Med. 2015;372(23):2185–2196. doi:10.1056/NEJMoa1503326
13. Rochwerg B, Granton D, Wang DX, et al. High flow nasal cannula compared with conventional oxygen therapy for acute hypoxemic respiratory failure: a systematic review and meta-analysis. Intensive Care Med. 2019;45(8):563–572. doi:10.1007/s00134-019-05590-5
14. Ni YN, Luo J, Yu H, et al. Can high-flow nasal cannula reduce the rate of endotracheal intubation in adult patients with acute respiratory failure compared with conventional oxygen therapy and noninvasive positive pressure ventilation? A systematic review and meta-analysis. Chest. 2017;151(4):764–775. doi:10.1016/j.chest.2017.01.004
15. Ou X, Hua Y, Liu J, Gong C, Zhao W. Effect of high-flow nasal cannula oxygen therapy in adults with acute hypoxemic respiratory failure: a meta-analysis of randomized controlled trials. CMAJ. 2017;189(7):E260–E267. doi:10.1503/cmaj.160570
16. Mellado-Artigas R, Ferreyro BL, Angriman F, et al. High-flow nasal oxygen in patients with COVID-19-associated acute respiratory failure. Crit Care. 2021;25(1):58. doi:10.1186/s13054-021-03469-w
17. Ospina-Tascón GA, Calderón-Tapia LE, García AF, et al. Effect of high-flow oxygen therapy vs conventional oxygen therapy on invasive mechanical ventilation and clinical recovery in patients with severe COVID-19: a randomized clinical trial. JAMA. 2021;326(21):2161–2171. doi:10.1001/jama.2021.20714
18. Frat JP, Quenot JP, Badie J, et al. Effect of high-flow nasal cannula oxygen vs standard oxygen therapy on mortality in patients with respiratory failure due to COVID-19: the SOHO-COVID randomized clinical trial. JAMA. 2022;328(12):1212–1222. doi:10.1001/jama.2022.15613
19. Paraskevas T, Oikonomou E, Lagadinou M, et al. The role of high flow nasal oxygen in the management of severe COVID-19: a systematic review. Acta Med Port. 2022;35(6):476–483. doi:10.20344/amp.16686
20. Eaton Turner E, Jenks M. Cost-effectiveness analysis of the use of high-flow oxygen through nasal cannula in intensive care units in NHS England. Expert Rev Pharmacoecon Outcomes Res. 2018;18(3):331–337. doi:10.1080/14737167.2018.1411804
21. Fealy N, Osborne C, Eastwood GM, Glassford N, Hart G, Bellomo R. Nasal high-flow oxygen therapy in ICU: a before-and-after study. Aust Crit Care. 2016;29(1):17–22. doi:10.1016/j.aucc.2015.05.003
22. Echeverri ED, Ruiz-Morales AJ, Rondon M, Rosselli D. Una aproximación a la distribución de los costos directos de la diabetes tipo 2 en Colombia. Salud Pública Méx. 2022;64(5):449–450. doi:10.21149/13822
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
