Back to Journals » Infection and Drug Resistance » Volume 17
Contezolid-Containing Regimen Successfully Treated Multiple Drug Resistance Mycobacterium Abscessus Complex Infection of Skin: A Case Report and Literature Review
Authors Gao X, Ding C, Xie D, Wang Q, Jiang P, Wang Y, Xiong Y
Received 6 December 2023
Accepted for publication 13 March 2024
Published 27 March 2024 Volume 2024:17 Pages 1243—1249
DOI https://doi.org/10.2147/IDR.S453541
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Prof. Dr. Héctor Mora-Montes
Xusheng Gao, Caihong Ding, Dan Xie, Qing Wang, Peipei Jiang, Yuyu Wang, Yu Xiong
Department of Tuberculosis, Shandong Public Health Clinical Center, Shandong University, Jinan, Shandong, People’s Republic of China
Correspondence: Yu Xiong, Department of Tuberculosis, Shandong Public Health Clinical Center, Shandong University, No. 11, Lieshishan East Road, Licheng District, Jinan, Shandong, People’s Republic of China, Tel +8615589995880, Email [email protected]
Background: In recent decades, there has been a substantial surge in the incidence of non-tuberculous Mycobacteria (NTM) infections. However, the diagnosis and management of NTM globally present significant challenges, particularly in cases involving Mycobacterium abscessus complex (MABC) infection where effective therapeutic options are limited.
Case Presentation: We reported a 38-year-old female patient who was infected with MABC of skin due to “beauty needle” at a beauty salon, with mass on both cheeks, accompanied by redness, and pain, and some of them was ulcered and effused. Puncture pumping pus from bilateral cheek mass for many times, rinsed with “metronidazole”, and oral “cephalosporin” treatment did not work. Therefore, she came to our hospital. MABC was detected in abscess paracentesis pus by nucleic acid mass spectrometry, and was proved by the cultured result of the pus. Thus, the patient was diagnosed as skin MABC infection, and anti-NTM treatment was taken. However, adverse reactions such as tinnitus, hepatotoxicity and neurovirulence occurred during the initial treatment. After adjusting to the contezolid-containing regimen, these adverse reactions improved. After nearly 6 months of treatment, the cheek mass was gradually reduced and the skin ruptures were gradually healed. Follow-up for 10 months showed that the patient’s facial symptoms were significantly improved, and no drug-related adverse reactions happened.
Conclusion: This was the first successful case of multiple drug resistance MABC infection of skin treated with contezolid-containing antibiotic management strategies, which exhibited remarkable efficacy and good safety in this intractable disease.
Keywords: Mycobacterium abscessus complex, antibiotic therapy, contezolid, Case report
Introduction
Non-Tuberculous Mycobacteria (NTM), represents a diverse group of mycobacteria distinct from the Mycobacterium tuberculosis complex and the Mycobacterium leprae. Over the past few decades, the incidence of NTM infections has significantly risen due to factors such as population aging and an increase in immunocompromised individuals. This surge has established NTM as a prominent public health concern.1–4 Presently, more than 190 species and subspecies of NTM have been identified, with dozens capable of causing diseases in humans. Mycobacterium avium complex (MAC) and Mycobacterium abscessus complex (MABC) contribute to 70% to 95% of NTM infections.5 Skin infections, especially fast-growing mycobacteria, frequently manifest as non-healing ulcers, subcutaneous abscesses, draining sinuses, or indurated nodules. The histopathological presentation varies depending on the evolution of the disease and the immune status of the host.6 MABC exhibits inherent resistance to most first-line anti-tubercular drugs, displaying susceptibility only to a limited range of antibiotics and demonstrating a propensity for rapid development of resistance. Coupled with extended disease courses, high rates of recurrence, medication-related adverse effects, and drug-drug interactions, treatment success rates for MABC-related diseases are disappointingly low, typically ranging from 50% to 66%, resulting in elevated mortality rates. This situation poses considerable challenges to anti-infective therapy.7–9
Both domestic and international guidelines5,10,11 provide recommendations for NTM treatment that for the treatment of MABC skin and soft tissue infections, therapeutic approaches involving amikacin (AMK), cefoxitin (CFX), clarithromycin (CLA), or azithromycin are suggested. In cases of resistance to CLA or azithromycin, treatment options encompass linezolid or Minocycline (MINO).However, the formulation of guideline-based treatment plans for NTM, especially MABC patients, is fraught with challenges. These include the high cost of medications, limited accessibility, and the relatively elevated occurrence of adverse effects associated with amikacin. Therefore, there is an urgent need for research into antimicrobial therapy options for MABC-induced infectious diseases. Contezolid, a kind of novel and potent antibiotics, is classified as an oxazolidinone antibiotic with a primary spectrum targeting aerobic Gram-positive bacteria. It’s structurally derived from linezolid and demonstrates antibacterial potential that’s comparable to, or slightly better than, that of linezolid.12 Furthermore, contezolid mitigates the neurologic and hematologic toxicities found in its predecessors. It reduces inhibition of monoamine oxidase, lowers drug-drug interactions, and thus enhances safety in clinical applications.13 Contezolid exhibits robust antibacterial activity against most clinically pathogenic NTM reference strains.14 This feature positions it as a promising alternative for the treatment of MABC-related infectious diseases, even though there’s limited literature on its long-term application in managing NTM ailments.
This was the first successful case of multiple drug resistance MABC infection of skin treated with contezolid-containing regimen, which exhibited remarkable efficacy and good safety in this deadly disease. The study was approved by the Ethics Committee of Shandong Public Health Clinical Center. Written informed consent was obtained from the patient for the publication of any potentially identifiable images or data included in this article. In addition, the patient and her family were aware of her condition and previous treatment history, and know that the contezolid used was new to the market, as well as the situation of other patients who have used this drug.
Case Details
A 38-year-old female was admitted to the hospital on November 10, 2022 due to “redness and swelling of masses on both cheeks for more than 4 months”. More than 4 months ago, the patient received bilateral cheek injections of a product nicknamed “beauty needle” (composed of polyvinyl pyrolidone, niacinamide, mannitol, purified water) at a beauty salon. About 10 days later, the bilateral cheek masses appeared with redness, swelling and pain. The patient took pus extraction from the bilateral cheek masses many times at the beauty salon (the specific description of pus was unclear and the number of extractions was not specified). The bilateral cheeks were rinsed with 100mL metronidazole once a day more than 10 days. Oral antibiotic treatment of an unspecified cephalosporin was given for more than 10 days (unknown dosage), but the treatment did not work. Then, the patient was admitted to our hospital for further treatment (D1). She was in good health and had no prior history of underlying diseases, allergy, trauma, surgery, or blood transfusion. Physical Examination: T: 36.6°C; P: 80 times/min; R: 20 times/min; BP: 108/78 mmHg. She was conscious with no neck resistance. Bilateral lung auscultation revealed clear breath sounds without wheezes, crackles, or rhonchi. Cardiac examination showed no heart murmur. Multiple masses appeared on both cheeks including some fusions, with the maximum mass size of about 3cm x 1cm located on the right cheek (Figure 1A and B). Some of the masses were red in surface, with wave feeling, high skin temperature and tenderness. Ulcerations were seen on part of the surface with purulent discharge. Many scars of different lengths can be seen on both cheeks, and the longest scar can reach about 3 cm in length. A more serious manifestation is in the right cheek.
After admission, further relevant laboratory investigations (Table 1) and imagological examination were performed. Facial mass ultrasound (Figure 1C) showed that, several low echo areas in the subcutaneous tissue of bilateral maxillofacial region were detected; and 2 hypoechoic areas were found in the right maxillofacial subcutaneous, extending to the skin with the size of about 2.8cm x 0.7cm and 2.0cm x 0.4cm respectively. The uneven echo of the subcutaneous tissue of bilateral maxillofacial region was considered as inflammatory changes; the subcutaneous low echo area of the right maxillofacial region was considered as abscess.
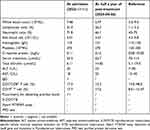 |
Table 1 Laboratory Findings at Admission and Half a Year of Post-Treatment |
Clinical Course
At admission (D1), it was diagnosed as a cutaneous MABC infection. During the treatment, the patient could not receive clofazimine because of the skin mucosal coloring side effects. Specific antimicrobial regimens used in this patient can be shown in Figure 2. Moxifloxacin 0.4g qd, azithromycin 0.5g qd, linezolid 0.6g qd, CFX 2g q8h intravenous infusion, MINO 100 mg bid anti-MABC treatment were given simultaneously starting on the next day post admission (D2). The abscess was punctured and drained under ultrasonic guidance, and the drainage volume was about 3–5mL of abscess each time, which was used for bacterial culture, drug sensitivity test and nucleic acid mass spectrometry detection. The testing method and experiments from nucleic acid extraction to final MS analysis were established and conducted by Shanghai Conlight Medical Co., Ltd. The mass spectrometry results were analyzed with Typer 4.0 software (Agena Bioscience). NTM were detected in pus bacterial culture. MAB and M. abscessus subsp.massiliense (MMA) were identified with the analysis of deoxyribose nucleic acid by mass spectrometry. Wide type gene, erm (41)28, was detected, which means that the clinical isolates of Mycobacterium abscessus might be inducible macrolide resistance. Therefore, azithromycin was discontinued, and AMK 0.6g qd was added. Symptoms gradually improved and the patient was discharged after 10 days of hospitalization (D10). After discharge, moxifloxacin, linezolid, AMK and MINO were given because CFX was not available. Tinnitus occurred during the treatment so AMK was discontinued at approximately day 20 post discharge (D30).
On November 21, 2022 (D13), the result of MABC drug sensitivity test (Table 2) showed that it was sensitive to amikacin, clarithromycin, and linezolid; intermediate to moxifloxacin and cefoxitin, and, resistant to minocycline, imipenem, tobramycin and cotrimoxazole. The patient could not obtain tigecycline outside the hospital. About 3 days after discharge, the regimen was adjusted to moxifloxacin (0.4g qd), linezolid (0.6g qd) and clarithromycin (0.5g bid). Tinnitus developed during treatment, and amikacin was discontinued approximately 20 days after discharge (D30). At D50, numbness in lower limbs and liver function impairment occurred. Liver function improved after the dosing of linezolid was reduced (0.3g qd) and liver protection treatment with bicyclol (50mg tid) and polyene phosphatidylcholine capsule (0.456g tid) were performed. But the numbness in lower limbs could not be tolerated. All antibiotics were discontinued at D65. At D81, the symptoms gradually improved after contezolid (0.4g q12h), Moxifloxacin, CLA were added for continued treatment.
 |
Table 2 Antimicrobial Susceptibility Results for MAB Cultured from Pyogenic Fluids |
After nearly 6 months of treatment, the cheek mass was gradually reduced and the skin ruptures were gradually healed (Figure 1D and E). Regular review of blood routine, liver and kidney function and electrocardiogram showed no obvious adverse reactions. Facial mass ultrasound: the uneven echo of bilateral maxillofacial subcutaneous tissue, irregular bar hypoechoic and isoecho phase arrangement, about 1.4cm x 0.4cm in the larger area on the right side, and about 1.3cm x 0.6cm in the larger area on the left (Figure 1F). Follow-up for 10 months showed that the patient’s facial symptoms were significantly improved (Figure 1G and H), and no drug-related adverse reactions happened.
Discussion
MABC often found in water, soil, and dust can lead to skin and soft tissue infections following skin injuries caused by inoculation, minor traumas, or surgical procedures. The rising popularity of cosmetic treatments has contributed to an increased incidence of skin and soft tissue infections. Cosmetic surgeries and other common procedures like acupuncture, tattooing, and foot treatments have been associated with a higher risk of these infections. While there have been several cases reported regarding the occurrence of MABC infections following plastic surgery,1–4,15 MABC infection after facial injections of “beauty needle” is notably rare. This study marked the first report of a successful long-term treatment using an antibiotic regimen containing contezolid for soft tissue infection with MABC following facial injections, providing preliminary evidence for the clinical application of contezolid in the treatment of MABC infections.
The recommended medications according to the guidelines5,10,11 are amikacin or amikacin inhalation solution, cefoxitin, clarithromycin, or azithromycin, linezolid or minocycline, with a minimum treatment duration of four months. In this study, patients were initially in good health and, upon diagnosing MABC infection, received a combined treatment regimen consisting of moxifloxacin, azithromycin, linezolid, cefoxitin, and minocycline. However, it’s crucial to acknowledge the significant variability in NTM patients’ conditions. NTM often exhibits natural resistance to multiple antibiotics and can develop resistance quite easily during the treatment process, making it challenging for a considerable portion of patients to adhere to the standard regimens recommended by the guidelines. Similarly, in our case, the patient had to discontinue azithromycin and minocycline due to resistance issues. Furthermore, antibiotic regimens for NTM patients tend to be rather complex, and adverse drug reactions are taken as a concern by clinical practitioners. In our case, the patient had to stop amikacin due to adverse effects, including tinnitus, and linezolid was discontinued due to liver impairment and intolerable numbness in the lower extremities.
In fact, linezolid has shown significant clinical value in the treatment of drug-resistant Gram-positive bacteria and is recommended for the treatment of various infections. However, its potential for neurologic and hematologic toxicity as well as significant inhibition of monoamine oxidase limits its widespread clinical use.16 In our case, after one month of treatment with an antibiotic regimen containing linezolid, the patient’s infection symptoms improved. However, they had to discontinue it due to liver toxicity and intolerable neurotoxicity. On the other hand, contezolid, is a member of the oxazolidinone class of antibiotics. It functions by binding to the 23S RNA on the 25S ribosomal subunit in bacteria, inhibiting bacterial growth by preventing the formation of the functional 70S initiation complex required for translation. In vitro antimicrobial tests and in vivo studies indicate that contezolid exhibits antibacterial activity equivalent to linezolid, especially against some drug-resistant strains of aerobic Gram-positive cocci.17 In a Phase 3 study conducted in China for complicated skin and soft tissue infections, contezolid was found to be non-inferior to linezolid in terms of efficacy but associated with fewer hematological adverse events.18–20 Furthermore, contezolid is primarily metabolized by FMO5 and does not interact with drugs metabolized by the liver enzyme inducers, adrenergic agents, serotonin agents, and the P450 enzyme system.21 Oxazolidinones bind to the 50S ribosomal subunit, inhibiting initiation complex formation and preventing cross-resistance with other antibiotics.18 Currently, there are limited reports regarding the use of contezolid in treating NTM. In our study, the patient’s condition remained stable after switching to contezolid, and the efficacy of the antimicrobial treatment was well-maintained. Notably, there were no treatment-related adverse events throughout the therapy, enhancing our confidence in the long-term practice of treating MABC infections.
This study has several limitations. Firstly, challenges encountered during the patient’s clinical journey resulted in incomplete medical records and missing results from some laboratory tests. Additionally, the treatment of patients in this study involved contezolid and other antibiotics, and the individual efficacy of each treatment warrants further evaluation. Further experimental and clinical research with larger sample sizes is needed to assess the clinical application of contezolid.
Data Sharing Statement
The original contributions presented in the study are included in the article. Further inquiries can be directed to the corresponding author.
Ethics Statement
This study was approved by the Ethics Committee of Shandong Public Health Clinical Center. Written informed consent was obtained from the individual for the publication of any potentially identifiable images or data included in this article.
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Funding
The study was supported by the Key Research and Development Program of Shandong Province (Major scientific and technological innovation projects) (2021SFGC0504), Study on the changes of T lymphocyte subsets and cytokines in peripheral blood of patients with drug-resistant pulmonary tuberculosis treated with tuberculosis pill and moxibustion combined adjuvant therapy (2020M059).
Disclosure
The authors have no conflicts of interest to declare.
References
1. Winthrop KL, Marras TK, Adjemian J, et al. Incidence and prevalence of nontuberculous mycobacterial lung disease in a large U.S. managed care health plan. Ann Am Thorac Soc. 2020;17(2):178–185. doi:10.1513/AnnalsATS.201804-236OC
2. Suresh P, Kumar A, Biswas R, et al. Epidemiology of nontuberculous mycobacterial infection in tuberculosis suspects. Am J Trop Med Hyg. 2021;105(5):1335–1338. doi:10.4269/ajtmh.21-0095
3. Kumar K, Loebinger MR. Nontuberculous mycobacterial pulmonary disease: clinical epidemiologic features, risk factors, and diagnosis: the nontuberculous mycobacterial series. Chest. 2022;161(3):637–646. doi:10.1016/j.chest.2021.10.003
4. Li W, Yazidi A, Pandya AN, et al. MmpL3 as a target for the treatment of drug-resistant nontuberculous mycobacterial infections. Front Microbiol. 2018;9:1547. doi:10.3389/fmicb.2018.01547
5. Daley CL, Iaccarino JM, Lange C, et al. Treatment of nontuberculous mycobacterial pulmonary disease: an official ATS/ERS/ESCMID/IDSA clinical practice guideline. Eur Respir J. 2020;56(1):2000535. doi:10.1183/13993003.00535-2020
6. Uslan DZ, Kowalski TJ, Wengenack NL, et al. Skin and soft tissue infections due to rapidly growing mycobacteria: comparison of clinical features, treatment, and susceptibility. Arch Dermatol. 2006;142(10):1287–1292. doi:10.1001/archderm.142.10.1287
7. Raju RM, Raju SM, Zhao Y, et al. Leveraging advances in tuberculosis diagnosis and treatment to address nontuberculous mycobacterial disease. Emerg Infect Dis. 2016;22(3):365–369. doi:10.3201/eid2203.151643
8. Diel R, Nienhaus A, Ringshausen FC, et al. Microbiologic outcome of interventions against mycobacterium avium complex pulmonary disease: a systematic review. Chest. 2018;153(4):888–921. doi:10.1016/j.chest.2018.01.024
9. Diel R, Lipman M, Hoefsloot W. High mortality in patients with mycobacterium avium complex lung disease: a systematic review. BMC Infect Dis. 2018;18(1):206. doi:10.1186/s12879-018-3113-x
10. Haworth CS, Banks J, Capstick Tet al. British thoracic society guidelines for the management of non-tuberculous mycobacterial pulmonary disease (NTM-PD). Thorax. 2017;72(Suppl 2):969–970. doi:10.1136/thoraxjnl-2017-210929
11. Wu J, Lu AD, Zhang LP, et al. Study of clinical outcome and prognosis in pediatric core binding factor-acute myeloid leukemia. Zhonghua Xue Ye Xue Za Zhi. 2019;40(1):52–57. doi:10.3760/cma.j.issn.0253-2727.2019.01.010
12. Li CR, Zhai QQ, Wang XK, et al. In vivo antibacterial activity of MRX-I, a new oxazolidinone. Antimicrob Agents Chemother. 2014;58(4):2418–2421. doi:10.1128/AAC.01526-13
13. Eckburg PB, Ge Y, Hafkin B. Single- and multiple-dose study to determine the safety, tolerability, pharmacokinetics, and food effect of oral MRX-I versus linezolid in healthy adult subjects. Antimicrob Agents Chemother. 2017;61(4). doi:10.1128/AAC.02181-16
14. Guo Q, Xu L, Tan F, et al. a novel oxazolidinone, contezolid (MRX-I), expresses anti-mycobacterium abscessus activity in vitro. Antimicrob Agents Chemother. 2021;65(11):e0088921. doi:10.1128/AAC.00889-21
15. Ratnatunga CN, Lutzky VP, Kupz A, et al. The rise of non-tuberculosis mycobacterial lung disease. Front Immunol. 2020;11:303. doi:10.3389/fimmu.2020.00303
16. Rabon AD, Fisher JP, MacVane SH. Incidence and risk factors for development of thrombocytopenia in patients treated with linezolid for 7 days or greater. Ann Pharmacother. 2018;52(11):1162–1164. doi:10.1177/1060028018783498
17. Huang JW, Kuo CL, Wang LT, et al. Case report: in situ vaccination by autologous CD16(+) dendritic cells and anti-PD-L 1 antibody synergized with radiotherapy to boost T cells-mediated antitumor efficacy in a psoriatic patient with cutaneous squamous cell carcinoma. Front Immunol. 2021;12:752563. doi:10.3389/fimmu.2021.752563
18. Gordeev MF, Yuan ZY. New potent antibacterial oxazolidinone (MRX-I) with an improved class safety profile. J Med Chem. 2014;57(11):4487–4497. doi:10.1021/jm401931e
19. Morelli T, Fujita K, Redelman-Sidi G, et al. Infections due to dysregulated immunity: an emerging complication of cancer immunotherapy. Thorax. 2022;77(3):304–311. doi:10.1136/thoraxjnl-2021-217260
20. Zhao X, Huang H, Yuan H, et al. A Phase III multicentre, randomized, double-blind trial to evaluate the efficacy and safety of oral contezolid versus linezolid in adults with complicated skin and soft tissue infections. J Antimicrob Chemother. 2022;77(6):1762–1769. doi:10.1093/jac/dkac073
21. Meng J, Zhong D, Li L, et al. Metabolism of MRX-I, a novel antibacterial oxazolidinone, in humans: the oxidative ring opening of 2,3-dihydropyridin-4-one catalyzed by non-P450 enzymes. Drug Metab Dispos. 2015;43(5):646–659. doi:10.1124/dmd.114.061747
 © 2024 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2024 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.


