Back to Journals » Orthopedic Research and Reviews » Volume 16
Computed Tomography Findings and Classification of Traumatic Lumbosacral Spine Injuries: Insights from the AOSpine Classification System
Authors Pham TD, Hoang NT , Le TB , Ha TH, Nguyen TT
Received 14 October 2023
Accepted for publication 16 January 2024
Published 26 January 2024 Volume 2024:16 Pages 35—42
DOI https://doi.org/10.2147/ORR.S444675
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Professor Clark Hung
Thuy Dung Pham,1 Ngoc Thanh Hoang,2 Trong Binh Le,2 Thi Hien Ha,2 Thanh Thao Nguyen2
1Department of Radiology, Binh Dinh General Hospital, Binh Dinh, Vietnam; 2Department of Radiology, Hue University of Medicine and Pharmacy, Hue University, Hue, Vietnam
Correspondence: Thanh Thao Nguyen, Department of Radiology, Hue University of Medicine and Pharmacy, Hue University, Hue, Vietnam, Email [email protected]
Purpose: The main objective of this study was to provide a description and classification of lumbosacral spine injuries based on the new AOSpine classification system.
Methods: A cross-sectional study was conducted on 75 patients with lumbosacral spine trauma who were admitted to Hue University of Medicine and Pharmacy Hospital in Hue, Vietnam, between April 2021 and July 2022. All patients underwent lumbosacral computed tomography, and each injured vertebra was classified according to the AOSpine classification system. The frequency and percentage of subtypes of lumbosacral spine trauma were determined.
Results: The mean age of the patients was 50.6 ± 16.1 years, and the male-to-female ratio was 1.5:1. Falls and traffic accidents were found to be the main causes of injuries. Among the patients, 78.7% did not exhibit any neurological symptoms, while 1.3% experienced complete hemiplegia and 20% had incomplete hemiplegia. The most common fracture subtype was A3, accounting for 34.6% of cases.
Conclusion: This study provides valuable insights into the demographics, associated injuries, and classification of traumatic lumbosacral spine injuries based on the new AOSpine classification system. The study found that falls and motor vehicle accidents were the main causes of these injuries, with a higher proportion of male patients. The majority of injuries were classified as type A fractures, while type C fractures were the least common. Sacral fractures were relatively infrequent and often associated with pelvic ring fractures. These findings contribute to our understanding of lumbosacral spine trauma and can aid in the development of more effective treatment protocols.
Keywords: lumbosacral spine injury, AOSpine classification, computed tomography
Introduction
Traumatic spinal injuries can have severe consequences, leading to long-term medical, psychological, social, and financial impacts on patients, their families, and society.1 The global incidence of traumatic spinal injury is estimated to be 10.5 cases per 100,000 individuals, resulting in over 700,000 cases worldwide each year.2 Road traffic accidents and falls are the most common causes of spine trauma.3,4 Studies have shown that 30% of spinal injuries involve the thoracolumbar and lumbosacral spine.5 Adult thoracolumbar fractures can result in injury to the spinal cord or cauda equina in approximately 10% to 38% of cases.6 Sacral fractures are often seen in high-energy trauma scenarios, particularly those involving pelvic-ring injuries. Motor vehicle collisions, pedestrian accidents, motorcycle accidents, falls, and crush injuries are common mechanisms of sacral fractures, with up to 25% of cases involving neurological deficits.7
It is crucial for radiologists to accurately describe the morphology of spinal injuries, enabling effective communication with physicians regarding the type and stability of the injury.1 This information is of utmost importance for the spine surgeon to select the most suitable treatment option. Various classification systems have been proposed over the years to facilitate communication and develop treatment protocols for spinal fractures. However, no classification system has achieved universal acceptance. In 2013, Vaccaro et al introduced the AOSpine thoracolumbar injury classification system, which combines the strengths of two previous systems (Magerl system and TLICS) while overcoming their limitations.8 This classification system classifies fracture morphology into three major types: type A (compression injury), type B (posterior or anterior tension band injury), and type C (translational injury). It also incorporates the assessment of neurological deficits and the impact of important medical conditions on treatment.8 AOSpine also developed the Sacral Classification System, which characterizes sacral fracture morphology based on levels of posterior pelvic and spinopelvic instability. Type-A fractures (lower sacrococcygeal) do not involve posterior pelvic or spinopelvic instability, type-B fractures (posterior pelvic) involve posterior pelvic instability but not spinopelvic instability, and type-C fractures (spinopelvic) involve spinopelvic instability.9 This classification system also includes modifiers that indicate patient-specific characteristics that may influence treatment and prognosis, as well as the patient’s neurological status. Kepler et al and Vaccaro et al developed a treatment algorithm for thoracolumbar spine injuries based on the AOSpine classification system and the Thoracolumbar AOSpine Injury Score (TL AOSIS). The TL AOSIS score is calculated by summing the scores for vertebral morphology injury (0–8 points), neurological status (0–4 points), and case-specific modifiers (0–1 point).10 Based on the algorithm, Vaccaro et al recommended surgical intervention for injuries with TL AOSIS above 5, conservative treatment for injuries scoring 3 or lower, and for injuries scoring 4 or 5, both surgical and conservative treatments were considered equally acceptable.11 This study aims to describe and classify lumbosacral spine injuries using the new AOSpine classification system.
Methods
A cross-sectional study was conducted to examine traumatic lumbosacral spine fractures. During the period from April 2021 to July 2022, a total of 75 patients with such fractures were identified at our institution. The inclusion criteria included acute traumatic spine injuries ranging from T11 to S5. Exclusion criteria comprised of infections, tumors, previous spine surgeries, or pathological fractures. Computed tomography (CT) images in the axial, coronal, and sagittal planes were available for all patients. Demographic variables, including gender, age, cause of the accident, and neurological status (assessed using the American Spinal Injury Association Impairment Scale, AIS), were documented. Each injured vertebra was classified according to the AOSpine classification system. Approval for the study was obtained from the Ethics Committee of Hue University Medicine and Pharmacy in Vietnam, with registration number H2021/157. All patients gave written informed consent.
Results
The study included a total of 75 patients, comprising 45 (60%) men and 30 (40%) women. The average age of the patients was 50.6 ± 16.1 years, ranging from 12 to 83 years old. Falls accounted for 68% of the injuries, followed by motorcycle accidents (22.7%), car accidents (1.3%), and other causes (8%). According to the AIS classification, the neurological status of the patients was as follows: 1.3% were classified as A, 20% as B-D, and 78.7% as E. Twenty out of the 75 patients (26.7%) had nonspinal injuries in addition to their spinal injuries. Lumbosacral injuries were commonly associated with long bone fractures (40%) and chest injuries (25%), while head injuries were less frequent. Demographic and neurological information can be found in Table 1.
 |
Table 1 Demographic Characteristics and Neurological Status of the Study Patient |
In total, there were 108 injured vertebrae among the 75 patients. Of these, 53 patients had one injured vertebra, and 22 patients had two or more injured vertebrae. Table 2 provides information about the fracture injury levels. The most common segment of injury was the thoracolumbar junction (T11-L2), accounting for 81.5% of cases, with L1 being the vertebra most frequently injured (49%) (Table 2).
 |
Table 2 Level of Injury |
Based on the AOSpine classification system, type A fractures were the most common, representing 89.4% of cases. Type B fractures accounted for 9.6% of cases, while type C fractures were identified in 1% of cases. Subtype A3 had the highest percentage among all fracture morphologies, making up 34.6% of cases. There were no B3-type lesions observed in our study. Table 3 illustrates the percentage of fracture types classified according to the AOSpine classification (Table 3).
 |
Table 3 Morphological Classification of Thoracolumbar Fractures According to the AOSpine System |
Among the 4 patients with sacral fractures, one case was classified as subtype A2, two cases were subtype B2 according to the AOSpine classification system, and the remaining case had a fracture on the median sacral crest. Two cases of sacral fractures were combined with fractures of the ilium and pubic bone, and one case involved a fracture on the L5 transverse process. One of these cases presented with a neurological deficit.
Among the patients studied, there were 73 patients with thoracolumbar spine injuries, including 29 cases (39.1%) with TL AOSIS ≤3 was classified in the conservative treatment group, 23 cases (31.5%) with scores ≥ 6 were placed into the surgical treatment group and 21 cases (28.8%) with scores 4 or 5 were categorized into the consideration group for either conservative or surgical treatment (Table 4).
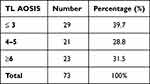 |
Table 4 TL AOSIS of Injury |
Discussion
The mean age of worldwide traumatic spinal injury patients is 39.8 (SD ± 12.2) and the male-to-female ratio is 3.37 on average.2 In a study of 508 spinal injury patients, associated injuries were reported in 47% of cases, with head injuries being the most frequent (26%), followed by chest injuries (24%) and long bone injuries (23%). The majority of the patients were of working age, with males being more commonly affected.12 Falls (44.2%), motorcycle accidents (25.6%), and car accidents (18.6%) were the most common causes of injury.13 Our study reflects similar demographics, causes of injury, and associated injuries as those mentioned above. Injuries to the lumbosacral spine were usually the result of high-energy blunt trauma, with chest trauma and long bone fractures being common related injuries.
Imaging is crucial for assessing stability, classification, and prognosis of spinal injuries.14 Different classification systems have been proposed for thoracolumbar spinal fracture, but many have limitations in reliability and reproducibility.15–17 The AOSpine classification system, based on CT scan, has been developed to address these limitations.
In our study, 89.4% of thoracolumbar vertebrae injuries were classified as type A, 9.6% as type B, and 1% as type C. The most common subtype was A3 (34.6%), followed by A1 (14.4%). The subtypes A2 and C have equal proportions (1%). There was no B3 subtype in our study. This is consistent with previous studies by Lee et al, where A3 was the most frequently reported subtype (23.5%), and B3 was the least frequently reported subtype (1.8%). They reported 69.3% as type A lesions, 24.1% as type B lesions, and 6.6% as type C lesions.18 Kepler et al reported that type A injuries accounted for 53.0% of cases, type B injuries accounted for 32.4% on average, and type C injuries accounted for 13.4% on average.19 A study by Aigner et al showed subtype A4 had the highest rate (48.2%), followed by subtype A3 (35%), with subtype A2 having the lowest rate (0.41%). Type A was the most common (87.3%), while type C was the least common (4.5%).20 Some examples of injury types of the AOSpine classification system are given in Figures 1–6.
 |
Figure 1 Axial and sagittal CT scan images: Subtype A4 injury. This 22-year-old man fell from a height. He had a neurological deficit (AIS D) and complained of severe back pain. |
 |
Figure 2 Sagittal and coronal CT scan images: Subtype B1 injury (Chance fracture). This 23-year-old man fell from a height. He was neurologically intact and complained of severe back pain. |
 |
Figure 5 Axial and sagittal CT images: Subtype B2 injury. This is a CT image of L2 vertebrae injury of a 51-year-old female patient. She had a heavy object fall on her back. |
 |
Figure 6 Axial and sagittal CT images: A 48-year-old male patient fell from a height. He had L2 vertebrae injury with subtype A2 and L4 vertebrae injury with subtype A1. |
However, there are some studies with different results in terms of subtype distribution. Marques et al reported that type A accounted for 74.2%, type B accounted for 15.3% and type C accounted for 10.6% among the 100 patients. The most common subtype was A1 (28.6%) and the least common was A0 (0.8%).21 According to Rajasekaran et al, type A and B lesions accounted for 40% each, while type C accounted for the remaining 20%. Common subtypes included A3, B1, B2, and C.14 Azimi et al found that there were 43.2% type A lesions, 25.7% type B lesions, and 31.1% type C lesions.22 These differences in subtype distribution may be attributed to variations in sample sizes, mechanisms of injury, and geographical regions.
The treatment recommendation based on the TL AOSIS score is an algorithm derived from data representing the result of a survey conducted among experts in the treatment of thoracolumbar spine trauma worldwide.11 According to the research by Nagi et al, TL AOSIS is more aligned with treatment recommendations than TLICS, exhibiting higher sensitivity and lower specificity compared to TLICS. In a study of 70 cases of thoracolumbar spine injuries conducted by Nagi et al, 24 patients (34.3%) scored less than 4 points on the TL AOSIS scale, 32 patients (45.7%) scored above 5 points, and 14 patients (20%) scored 4 or 5 points.23 While further in-depth studies are necessary to confirm the treatment algorithm and assess its outcomes, the proposed algorithm here holds the potential to become a new standard for research and clinical decision-making regarding thoracolumbar spine injuries.11 Sacral fractures are relatively uncommon and exhibit heterogeneous patterns.9 Different sacral fracture classification systems have been proposed based on fracture morphology. Denis et al classify fractures based on the location relative to the foramen and increasing higher risk of neurological injury.24 Roy-Camille et al described a morphological classification for transverse sacral fractures in 1985.25 Vaccaro et al proposed a descriptive system that combines vertical and horizontal patterns for morphological classification.26 However, these classifications are not comprehensive enough and lack prognosis or treatment guidelines.27 The AOSpine sacral fracture classification was described by Spine Knowledge Forum, and takes into account specific patterns of sacral injuries, degree of neurologic deficit, and case-specific modifiers.28 It has demonstrated substantial agreement, making it a reliable system for clinical studies.27
In our study, only 4 patients out of 75 patients had sacral fractures, with subtype B2 (2 cases), subtype A2 (1 case), and median sacral crest fracture (1 case). Two cases had combined lesions of the ilium and pubic bones, including one case with type B2 injury associated with an L5 transverse process fracture. The prevalence and distribution of sacral fracture subtypes may vary across different studies and populations.
Our study has some limitations, including a small sample size and limited MRI images for comparison. Further research with larger sample sizes and comprehensive imaging data is needed to enhance our understanding of these injuries and improve their management.
Conclusion
In conclusion, this study provides valuable insights into the demographics, associated injuries, and classification of traumatic lumbosacral spine injuries based on the new AOSpine classification system. The study found that falls and motor vehicle accidents were the main causes of these injuries, with a higher proportion of male patients. The majority of injuries were classified as type A fractures, while type C fractures were the least common. Sacral fractures were relatively infrequent and often associated with pelvic ring fractures. These findings contribute to our understanding of lumbosacral spine trauma and can aid in the development of more effective treatment protocols.
Ethical Statement
The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). The study was approved by the Ethics Committee of the University of Medicine and Pharmacy, Hue University, Vietnam. Approval number: H2021/157. All patients gave written informed consent.
Acknowledgment
This work was supported by Hue University through the Core Research Program (NCM.DHH.2020.09).
Disclosure
The authors have no conflicts of interest to declare.
References
1. Looby S, Flanders A. Spine trauma. Radiol Clin. 2011;49(1):129–163. doi:10.1016/j.rcl.2010.07.019
2. Kumar R, Lim J, Mekary RA, et al. Traumatic spinal injury: global epidemiology and worldwide volume. World Neurosurg. 2018;113:345–363. doi:10.1016/j.wneu.2018.02.033
3. Fernández Londoño LL, Marchesini N, Espejo Ballesteros D, et al. Epidemiological Review of Spinal Cord Injury due to road traffic accidents in Latin America. Med Princ Pract, 2022;31(1):11–19. doi:10.1159/000520112
4. Bakhsh A, Aljuzair AH, Eldawoody H. An Epidemiological Overview of Spinal Trauma in the Kingdom of Saudi Arabia. Spine Surg Relat Res. 2020; 4(4):300–304. doi:10.22603/ssrr.2019-0118
5. Sekhon LHS, Fehlings MG. Epidemiology, demographics, and pathophysiology of acute spinal cord injury. Spine. 2001;26(Supplement):S2–S12. doi:10.1097/00007632-200112151-00002
6. Levi AD, Hurlbert RJ, Anderson P, et al. Neurologic deterioration secondary to unrecognized spinal instability following trauma–a multicenter study. Spine. 2006;31(4):451–458. doi:10.1097/01.brs.0000199927.78531.b5
7. Rodrigues-Pinto R et al . (2017). Sacral fractures and Associated Injuries. Global Spine Journal, 7(7), 609–616. 10.1177/2192568217701097
8. Vaccaro AR, Oner C, Kepler CK, et al. AOSpine thoracolumbar spine injury classification system: fracture description, neurological status, and key modifiers. Spine. 2013;38(23):2028–2037. doi:10.1097/BRS.0b013e3182a8a381
9. Vaccaro AR, Schroeder GD, Divi SN, et al. Description and reliability of the AOSpine sacral classification system. J Bone Jt Surg Am Vol. 2020;102(16):1454. doi:10.2106/JBJS.19.01153
10. Kepler CK, Vaccaro AR, Schroeder GD, et al. The thoracolumbar AOSpine injury score. Global Spine Journal. 2016; 6(4):329–334. doi:10.1055/s-0035-1563610
11. Vaccaro AR, Schroeder GD, Kepler CK, et al. The surgical algorithm for the AOSpine thoracolumbar spine injury classification system. Eur Spine J. 2016;25(4):1087–1094. doi:10.1007/s00586-015-3982-2
12. Saboe LA, Reid DC, Davis LA, et al. Spine trauma and associated injuries. J Trauma. 1991;31(1):43–48. doi:10.1097/00005373-199101000-00010
13. Barcelos AC, Joaquim AF, Botelho RV. Reliability of the evaluation of posterior ligamentous complex injury in thoracolumbar spine trauma with the use of computed tomography scan. Eur Spine J. 2016;25(4):1135–1143. doi:10.1007/s00586-016-4377-8
14. Rajasekaran S, Vaccaro AR, Kanna RM, et al. The value of CT and MRI in the classification and surgical decision-making among spine surgeons in thoracolumbar spinal injuries. Eur Spine J. 2017;26(5):1463–1469. doi:10.1007/s00586-016-4623-0
15. Wood KB, Khanna G, Vaccaro AR, et al. Assessment of two thoracolumbar fracture classification systems as used by multiple surgeons. JBJS. 2005;87(7):1423–1429.
16. Blauth M, Bastian L, Knop C, et al. Inter-observer reliability in the classification of thoraco-lumbar spinal injuries. Orthopade. 1999;28(8):662–681.
17. Oner F, Ramos L, Simmermacher R, et al. Classification of thoracic and lumbar spine fractures: problems of reproducibility. Eur Spine J. 2002;11(3):235–245. doi:10.1007/s00586-001-0364-8
18. Lee H, Shin S, Yu CG, Wi SM. Reliability and reproducibility analysis of the AOSpine thoracolumbar spine injury classification system in Korea. J Korean Soc Spine Surg. 2022;29(2):27–34. doi:10.4184/jkss.2022.29.2.27
19. Kepler CK, Vaccaro AR, Koerner JD, et al. Reliability analysis of the AOSpine thoracolumbar spine injury classification system by a worldwide group of naïve spinal surgeons. Eur Spine J. 2016;25(4):1082–1086. doi:10.1007/s00586-015-3765-9
20. Aigner R, Bichlmaier C, Oberkircher L, et al. Pedicle screw accuracy in thoracolumbar fractures-is routine postoperative CT scan necessary? BMC Musculoskelet Disord. 2021;22(1):1–7.
21. Marques CA, Graells XS, Kulcheski AL, et al. Reliability of the AO classification of thoracolumbar fractures compared to TLICS and magerl. Coluna/Columna. 2017;16:56–59.
22. Azimi P, Mohammadi H, Azhari S, et al. The AOSpine thoracolumbar spine injury classification system: a reliability and agreement study. Asian J Neurosurg. 2015;10(04):282–285. doi:10.4103/1793-5482.162703
23. Nagi MA, Sakr MM. Accuracy of MRI (TLICS vs AOSIS) in assessment of thoracolumbar spine injuries for guiding treatment. Egypt J Radiol Nucl Med. 2022;53(1):41. doi:10.1186/s43055-022-00715-1
24. Denis F, Davis S, Comfort T. Sacral fractures: an important problem retrospective analysis of 236 cases. Clin Orthop Relat Res. 1988;227 ;67–81.
25. Roy-Camille R, Saillant G, Gagna G, Mazel C. Transverse fracture of the upper sacrum. Suicidal jumper’s fracture. Spine (Phila Pa 1976). 1985;10(9):838–845. doi:10.1097/00007632-198511000-00011
26. Vaccaro AR, Kim DH, Brodke DS, et al. Diagnosis and management of sacral spine fractures. JBJS. 2004;86(1):166–175. doi:10.2106/00004623-200401000-00027
27. Urrutia J, Meissner-Haecker A, Astur N, et al. An independent inter- and intraobserver agreement assessment of the AOSpine sacral fracture classification system. Spine J. 2021;21(7):1143–1148. doi:10.1016/j.spinee.2021.02.005
28. Schroeder GD, Kurd MF, Kepler CK, et al. The development of a universally accepted sacral fracture classification: a survey of AOSpine and AOTrauma members. Global Spine J. 2016;6(7):686–694. doi:10.1055/s-0036-1580611.
 © 2024 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2024 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.


