Back to Journals » Neuropsychiatric Disease and Treatment » Volume 20
Comparative Analysis of Personality Traits in Major Depressive Disorder and Bipolar Disorder: Impact, Differences, and Associations with Symptoms
Authors Li T, Li R, Zhao L, Sun Y, Wang C, Bo Q
Received 11 December 2023
Accepted for publication 16 February 2024
Published 23 February 2024 Volume 2024:20 Pages 363—371
DOI https://doi.org/10.2147/NDT.S451803
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Taro Kishi
Tian Li,1,2 Ruinan Li,1,2 Lei Zhao,1,2 Yue Sun,1,2 Chuanyue Wang,1,2 Qijing Bo1,2
1The National Clinical Research Center for Mental Disorders & Beijing Key Laboratory of Mental Disorders & Beijing Institute for Brain Disorders Center of Schizophrenia, Beijing Anding Hospital, Capital Medical University, Beijing, 100088, People’s Republic of China; 2Advanced Innovation Center for Human Brain Protection, Capital Medical University, Beijing, 100069, People’s Republic of China
Correspondence: Qijing Bo, The National Clinical Research Center for Mental Disorders & Beijing Key Laboratory of Mental Disorders & Beijing Institute for Brain Disorders Center of Schizophrenia, Beijing Anding Hospital, Capital Medical University, No. 5 Ankang Lane, Dewai Avenue, Xicheng District, Beijing, 100088, People’s Republic of China, Tel +86-10-58303119, Email [email protected]
Purpose: This cross-sectional study aimed to compare the personality traits of patients with major depressive disorder (MDD) and bipolar disorder (BD) with those of healthy individuals. The goal was to gain insight into the potential impact of personality traits on the development and manifestation of mood disorders.
Methods: One hundred seventy-eight patients with mood disorders were analyzed as either MDD or BD, with each group containing euthymic and depressive members: e-MDD, d-MDD, e-BD, and d-BD. Mood status was assessed using the Young Mania Rating Scale (YMRS), and the 17-item Hamilton Depression Rating Scale (HAMD-17). Ninety-five healthy individuals served as controls. Personality traits were assessed with the Eysenck Personality Questionnaire.
Results: The scores for neuroticism in the patient groups were comparable, but each group had higher scores compared to the control group (P < 0.001). Each patient group exhibited significantly lower scores for extraversion compared to the control group, with e-MDD, d-MDD, and d-BD showing particularly notable differences (P < 0.001); these groups scored significantly lower than the e-BD (P = 0.041, 0.009, 0.038). In patients with BD, there was an inverted association between extraversion score and HAMD total score (P = 0.010, r = – 0.27), and a positive association with the YMRS total score (P = 0.022, r = 0.24). In the MDD group, there was a positive association between the neuroticism score and HAMD total score (P = 0.021, r = 0.25).
Conclusion: Patients with mood disorders are characterized by lower extraversion and higher neuroticism. Level of neuroticism associated with depression severity in MDD. Patients with BD may be more extraverted, but their extraversion can be affected by depressive episodes. Extraversion may be a feature of BD, and may differentiate BD from MDD. Personality traits are related to disease diathesis and state, and shaped by symptom manifestations.
Keywords: personality traits, mood disorders, neuroticism, extraversion
Introduction
Mood disorders, or affective mental disorders, are characterized by significant and lasting changes in mood or emotion, with various causes. The two main categories of mood disorders are major depressive disorder (MDD) and bipolar disorder (BD). Both MDD and BD severely restrict social functioning and reduce quality of life.1,2 MDD is the second leading cause of disability in the world,3 and in China is the more prevalent, with 12-month and lifetime rates of 2.1 and 3.4%, respectively. The 12-month and lifetime prevalence rates of BD are far lower (0.5 and 0.6%).4 The symptoms of MDD and BD overlap, which can lead to misdiagnosis and treatment errors.5 Furthermore, there is a risk that MDD may transition to BD.6
Personality traits may be associated with mood disorders. The expression of personality relies on relatively stable traits with close connections to emotional experience, while personality traits may also directly influence affective states.7 However, the association between personality traits and mood disorders requires clarity. Some have proposed that personality traits can result in greater vulnerability to the development of mood disorders (the vulnerability hypothesis).8–10 Others, that the emotional disorder itself affects personality (the scar hypothesis): the experience of persistent emotional disorders may lead to personality changes and personality deviations.11,12
Previous studies of the personality traits associated with mood disorders have been inconsistent. For example, the scores for neuroticism in patients with MDD or BD have been either higher or equal than that of healthy individuals, while scores for extraversion have been variously reported as lower, higher, or similar.7,13–18 Comparing the 2 mood disorders, the scores for neuroticism in patients with BD are either higher, lower, or equal to that of patients with MDD, and extraversion scores have been higher or equal.7,16,17,19 Sample size, different assessment tools could contribute to the inconsistent findings.
The Eysenck Personality Questionnaire (EPQ) is a widely used tool in the personality literature, measuring 3 personality dimensions: neuroticism; extraversion; and psychoticism. The differences in degrees of these dimensions constitute the characteristics of a person’s unique personality.20 Neuroticism is a measure of a person’s emotional instability, which is relatively stable over time, and not affected by environmental and physical health conditions.21,22 Some studies have suggested that neuroticism is associated with depression and suicide.9,23,24 Neuroticism can predict depressive episodes and prognosis, and potentially screen for affective disorders.18 Extraversion would correlate positively with certain symptoms of BD.25 The higher the extraversion score, the more likely it is to increase some behavioral problems.26 The relationship between psychoticism and mood disorders, such as MDD and BD, has yielded inconsistent results in existing studies, necessitating further research for confirmation. The scores for both neuroticism and extraversion may be affected by current state, either depressive or euthymic.13,17,27 However, many studies did not consider the patients’ current state.
To better understand the personality traits of patients with mood disorders, the present study compared patients with MDD or BD, depressive or euthymic, relative to that of a control group of healthy individuals. In this cross-sectional study, our primary objective was to comprehensively compare the personality traits exhibited by patients diagnosed with MDD and BD with those of the healthy controls. By examining the variations in personality traits between these groups, we aimed to shed light on the potential influence of these traits on the development and manifestation of mood disorders. Through this investigation, we sought to a better understanding of the complex interplay between personality and mood disorders, ultimately aiding in the improvement of diagnostic and treatment approaches in clinical settings.
Methods
The clinical research ethics committee of Beijing Anding Hospital approved the research plan. All of the participants or their guardians provided written informed consent. Our study complies with the Declaration of Helsinki.
Participants
This was a cross-sectional study conducted at the hospital. All participants were enrolled through the outpatient department from September 2014 to September 2016. Evaluations were performed by qualified psychiatrists who were trained in method levels and scales. Diagnoses were made using the Structured Clinical Interview for DSM-IV Axis I disorders-Patient Edition (SCID-I/P).28,29
For inclusion, participants conformed to the following criteria: aged between 16 and 60 years, and with ≥9 years of formal education. Patients diagnosed BD or MDD according to the DSM-IV, who were currently euthymia or depression, with Young Mania Rating Scale (YMRS)30 total score ≤6. Euthymia was defined as having a total score of ≤7 on the Hamilton Depression Scale (HAMD)-17.31 Healthy subjects had no history of mental disorders.
Potential participants with any of the following were excluded: a previous medical history or current major medical or neurological disease; a history of, or current, serious abuse of drugs or alcohol; received modified electroconvulsive therapy in the previous 3 months; serious suicidal thoughts or suicide attempts; or pregnancy.
Finally, the study population comprised 5 groups: 41 and 47 euthymic and depressive patients with MDD (e-MDD and d-MDD, respectively); 56 and 34 euthymic and depressive patients with BD (e-BD and d-BD); and 95 healthy individuals (control).
Clinical Assessment
Patients’ sociodemographic characteristics and clinical data were collected using a questionnaire designed for the study. Mood status was assessed using the Young Mania Rating Scale (YMRS),30 17-item Hamilton Depression Rating Scale (HAMD-17),31 and Hamilton Anxiety Rating Scale (HAMA).32
Eysenck Personality Questionnaire (EPQ)
Personality was assessed using the Chinese version of the EPQ.20,33 This is a questionnaire consisting of 4 scales to measure psychoticism, neuroticism, extraversion, and lie, using a dichotomous (yes/no) response format, with scores of 1 or 0. The adult questionnaire comprises 88 items, specifically 24, 23, 21, and 20 items in the neuroticism, psychoticism, extraversion, and lie scale categories, respectively. The coincidence rates with the 90 items of the original questionnaire for psychoticism, neuroticism, extraversion, and lie were 87.5%, 95.0%, 97.8% and 87.8%.33
Statistical Analysis
Data were entered using EpiData software version 3.1 and analyzed with SPSS 22.0 for Windows (SPSS, Chicago, IL, USA). Comparisons were performed using Pearson’s chi-squared tests for categorical variables. The one-way analysis of variance was used to compare the demographic and neuropsychological tests among the 5 groups, and multivariate analysis of variance (MANOVA) was conducted with the EPQ dimensions as dependent variables. Covariates adjusted for individual demographic variables and clinical characteristics was also estimated among the study groups. Associations between EPQ dimensions and clinical characteristics were analyzed using Pearson’s correlation analysis. The multiple correlations problem was controlled for by applying the Bonferroni correction. For all analyses, the level of statistical significance was set at P < 0.05, 2-tailed.
Results
Demographic and Clinical Characteristics
The 5 groups (e-MDD, d-MDD, e-BD, d-BD, and control) did not differ with respect to gender or years of education (Table 1). Patients with e-MDD were significantly older than those of the other patient groups (F = 4.93, P < 0.001), but not the control group.
 |
Table 1 Demographics and Other Characteristics of the Study Groups |
EPQ Scores
The data conforms to a normal distribution. The group designation was used as the independent variable, and the 3 personality dimensions (psychopathy, extraversion, and neuroticism) were the dependent variables for MANOVA (Table 2). Lie has no clinical research value, and the groups did not differ significantly. The Bonferroni correction was applied to the results. There were differences in EPQ scores among the groups (Figure 1). Since age was a significant difference among the groups, age was used as a covariate for EPQ analysis. The analysis showed that age did not significantly affect the results.
 |
Table 2 EPQ Scores |
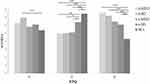 |
Figure 1 Comparison of EPQ scores among the d-MDD, d-BD, e-MDD, e-BD, and healthy control group. *P < 0.05 (2-tailed); **P < 0.01 (2-tailed); ***P < 0.001 (2-tailed). |
Psychoticism Scores
The d-BD group had higher psychoticism scores compared with the control group (P < 0.001), but the other groups were comparable to the control.
Extraversion Scores
The extraversion scores of the d-MDD, e-MDD, and d-BD groups were significantly lower than that of the control group (P < 0.001). The e-BD group score for extraversion was also significantly lower than the control group (P = 0.031). The extraversion scores of the d-MDD and e-MDD groups were similar, as were the scores of the d-MDD and d-BD groups. The e-MDD, d-MDD, and d-BD groups had significantly lower extraversion scores compared with the e-BD group (P = 0.041, 0.009, and 0.038, respectively).
Neuroticism Scores
Compared with the control individuals, the d-MDD, e-MDD, d-BD, and e-BD groups had higher neuroticism scores (P < 0.001), but the 4 patient groups were comparable.
Associations Between EPQ and Clinical Assessments
Among patients with BD, the extraversion score was negatively associated with the HAMD total score (P = 0.010, r = –0.27), and positively associated with the YMRS total score (P = 0.022, r = 0.24). Among patients with MDD, the psychoticism score was positively associated with the YMRS total score (P = 0.012, r = 0.27), and HAMD total score (P = 0.049, r = 0.21); the neuroticism score was also positively associated with the HAMD total score (P = 0.021, r = 0.25) (Table 3).
 |
Table 3 Correlations Between Dimension Scores of the EPQ with Scores of the Scales (HAMD and YMRS) in Patients |
Discussion
The current study applied the EPQ to investigate the personality traits of patients with mood disorders, BD or MDD (and each with members that were currently depressive or euthymic). The results indicated that, whether in the depressive or euthymic state, the extraversion scores of patients with either MDD or BD were lower than that of the control group of healthy individuals, while the neuroticism scores were higher. It was determined that personality traits were associated with mood disorders, and the expression of the depressive symptoms of mood disorders colors the assessment of personality, especially the extraversion dimension. This finding is consistent with previously published reports7,19,21,23,27, and confirms that the personality traits of patients with mood disorders differ from the healthy control. Even among euthymic patients, the difference cannot be ignored.
Most previous studies suggested that there was no significant difference in the extraversion dimension between patients with MDD or BD.16,17,19,23 Yet, the present findings showed that patients with e-BD exhibited more extraversion characteristics than did patients with e-MDD. This suggests that the high extraversion score may be a possible feature of BD and affected by mood state. The extraversion score was negatively affected by the depressive state in patients with BD, as the d-BD scored lower than did the e-BD. In patients with MDD, introversion (lower extraversion score) is more likely qualitative, and not affected by the depressive state. The discrepancies in findings of previous studies may be due to differences in the questionnaires used15,17,21,23 and patient selection. This suggests that the EPQ could be a suitable scale for clinical assessment of mood disorders.
Many studies have shown that patients with mood disorders, MDD or BD, have higher scores for neuroticism compared with healthy individuals.10,17,19,26,34,35 In the present study, the neuroticism scores of both the MDD and BD groups were higher than that of the control, and the difference in the scores of the patient groups was not pronounced. Many studies have corroborated that neuroticism is the most representative personality trait of mood disorders.17,21,22 Although levels of neuroticism decline after a depressive episode, they tend to be moderately preserved.36 Some studies have suggested that high neuroticism is not specific to mood disorders, but nevertheless it has been associated with many mental disorders,37,38 and there may be a genetic component.22 A recent study also confirmed that higher neuroticism was positively associated with incidence and recurrence of depression.39
Further research on these questions is required. Research attention should also be given to extraversion as a trait in mood disorders, as it is more specific. The present study also found that patients in the d-BD group had higher scores for psychoticism compared with the control, but this was not true for the other 4 patient groups. Psychoticism could not be used to differentiate MDD and BD. This is consistent with previous research results.7,21 It is interesting that in the series d-MDD, d-BD, e-MDD, and e-BD, the scores for extraversion gradually increased, while the scores for neuroticism decreased. According to this trend, it may be assumed that the extraversion score would be higher in patients with mania, but unfortunately, there were no mania patients in the current study—the influence of manic symptoms in correlation analyses was not adequately explored, as the YMRS total score was ≤6. This invites more study of trends in the personality traits of mood disorders.
There are 2 current hypotheses regarding the influence of personality traits on mood disorders. The vulnerability hypothesis states that personality traits can lead to emotional vulnerability, which can promote the development of mood disorders. According to the scar hypothesis, the experience of the persistent mood disorder itself may lead to personality changes and deviation.8,40 Most studies support the vulnerability hypothesis, and there is evidence that neuroticism is a risk factor for depression. There is little evidence to support the scar hypothesis.10 The current study is a cross-sectional study, and therefore cannot confirm either hypothesis. This is a limitation of the study. The design of the study also does not have the ability to build a sequence of personality traits and clinical manifestations of mood disorders. The relationship between personality and mood disorders may be pathoplastic and dependent on state. Cohort or family studies are needed.
The study is also limited in that we did not analyze the medication of the patients. Some studies have suggested that antidepressants may affect personality measures, including the extraversion dimension.41,42 This will be controlled for in future studies, and the drug effects will be included in the analysis. The scores for neuroticism and extraversion may be influenced by an individual’s current state, raising the question of whether these impacts on personality are dependent on the current state or if they reflect inherent traits. In order to address this, our objective is to investigate whether the influence on personality is contingent upon the current state or if it represents inherent traits. To accomplish this, we will categorize individuals based on their different states and analyze the results accordingly. However, it is important to consider that this approach (many groups are formed) may hinder the comprehension and interpretation of statistical analyses.
Conclusion
The personality traits of the patients with mood disorders were characterized by lower extraversion and higher neuroticism, relative to the healthy controls. Neuroticism was not specific to BD or MDD, as the scores of these patients were comparable. Psychoticism was particular to d-BD. The BD group had a higher extraversion score than did the MDD; the latter were characterized with introversion. Extraversion may be a feature of BD, and may differentiate BD from MDD. In patients with BD, the degree of extraversion was affected by clinical symptoms. In patients with MDD, the level of neuroticism was associated with the severity of depression. Psychiatrists should systematically assess the personality traits and plan interventions in mood disorders. Further research should include manic BD, to complete the spectrum of states in BD. Longitudinal research is also needed to describe the pathways between personality traits and mood disorders across the entire lifespan, with or without mood episode.
Funding
Supported by Beijing Hospitals Authority Clinical medicine Development of special funding support (No. ZLRK202335) and Beijing Natural Science Foundation (No. 7242073). No investigator benefited from participating in the study.
Disclosure
The authors report no conflicts of interest in this work.
References
1. Sylvia LG, Montana RE, Deckersbach T, et al. Poor quality of life and functioning in bipolar disorder. Int J Bipolar Disord. 2017;5(1):10. doi:10.1186/s40345-017-0078-4
2. Malhi GS, Mann JJ. Depression. Lancet. 2018;392(10161):2299–2312. doi:10.1016/S0140-6736(18)31948-2
3. Rakofsky J, Rapaport M. Mood Disorders. Continuum. 2018;24(3):804–827. doi:10.1212/CON.0000000000000604
4. Huang Y, Wang Y, Wang H, et al. Prevalence of mental disorders in China: a cross-sectional epidemiological study. Lancet Psychiatry. 2019;6(3):211–224. doi:10.1016/S2215-0366(18)30511-X
5. Angst J, Merikangas KR, Cui L, Van Meter A, Ajdacic-Gross V, Rössler W. Bipolar spectrum in major depressive disorders. Eur Arch Psychiatry Clin Neurosci. 2018;268(8):741–748. doi:10.1007/s00406-018-0927-x
6. Nestsiarovich A, Reps JM, Matheny ME, et al. Predictors of diagnostic transition from major depressive disorder to bipolar disorder: a retrospective observational network study. Transl Psychiatry. 2021;11(1):642. doi:10.1038/s41398-021-01760-6
7. Smillie LD, Bhairo Y, Gray J, et al. Personality and the bipolar spectrum: normative and classification data for the Eysenck Personality Questionnaire-revised. Compr Psychiatry. 2009;50(1):48–53. doi:10.1016/j.comppsych.2008.05.010
8. Akiskal HS, Hirschfeld RM, Yerevanian BI. The relationship of personality to affective disorders. Arch. Gen. Psychiatry. 1983;40(7):801–810. doi:10.1001/archpsyc.1983.01790060099013
9. Grav S, Stordal E, Romild UK, Hellzen O. The relationship among neuroticism, extraversion, and depression in the HUNT Study: in relation to age and gender. Issu Ment Health Nurs. 2012;33(11):777–785. doi:10.3109/01612840.2012.713082
10. Christensen MV, Kessing LV. Do personality traits predict first onset in depressive and bipolar disorder? Nord J Psychiatry. 2006;60(2):79–88. doi:10.1080/08039480600600300
11. Wilhelm K, Parker G, Dewhurst-Savellis J, Asghari A. Psychological predictors of single and recurrent major depressive episodes. J Affective Disorders. 1999;54(1–2):139–147. doi:10.1016/s0165-0327(98)00170-0
12. Rothen S, Vandeleur CL, Lustenberger Y, et al. Personality traits in children of parents with unipolar and bipolar mood disorders. J Affective Disorders. 2009;113(1–2):133–141. doi:10.1016/j.jad.2008.05.013
13. Duggan CF, Lee AS, Murray RM. Does personality predict long-term outcome in depression? Brit J Psych. 1990;157:19–24. doi:10.1192/bjp.157.1.19
14. Kim BJ, Linton K, Cho S, Ha JH. The relationship between neuroticism, hopelessness, and depression in older Korean immigrants. PLoS One. 2016;11(1):e0145520. doi:10.1371/journal.pone.0145520
15. Heerlein A, Richter P, Gonzalez M, Santander J. Personality patterns and outcome in depressive and bipolar disorders. Article. Psychopathology. 1998;31(1):15–22. doi:10.1159/000029019
16. Solomon DA, Shea MT, Leon AC, et al. Personality traits in subjects with bipolar I disorder in remission. J Affective Disorders. 1996;40(1–2):41–48. doi:10.1016/0165-0327(96)00039-0
17. Jylha P, Mantere O, Melartin T, et al. Differences in neuroticism and extraversion between patients with bipolar I or II and general population subjects or major depressive disorder patients. J Affective Disorders. 2010;125(1–3):42–52. doi:10.1016/j.jad.2010.01.068
18. Wilks Z, Perkins AM, Cooper A, Pliszka B, Cleare AJ, Young AH. Relationship of a big five personality questionnaire to the symptoms of affective disorders. J Affective Disorders. 2020;277:14–20. doi:10.1016/j.jad.2020.07.122
19. Barnett JH, Huang J, Perlis RH, et al. Personality and bipolar disorder: dissecting state and trait associations between mood and personality. Psychological Medicine. 2011;41(8):1593–1604. doi:10.1017/S0033291710002333
20. Eysenck H, Eysenck S. Manual of the Eysenck Personality Questionnaire. In: Z Differentielle Diagnostische Psychologie. London: University of London Press; 1975:20.
21. Marijnissen RM, Bus BA, Schoevers RA, et al. Atherosclerosis decreases the impact of neuroticism in late-life depression: hypothesis of vascular apathy. Am J Geriat Psych. 2014;22(8):801–810. doi:10.1016/j.jagp.2013.01.001
22. Smith DJ, Escott-Price V, Davies G, et al. Genome-wide analysis of over 106 000 individuals identifies 9 neuroticism-associated loci. Mol Psychiatry. 2016;21(6):749–757. doi:10.1038/mp.2016.49
23. Quilty LC, Sellbom M, Tackett JL, Bagby RM. Personality trait predictors of bipolar disorder symptoms. Psychiatry Res. 2009;169(2):159–163. doi:10.1016/j.psychres.2008.07.004
24. Berlanga C, Heinze G, Torres M, Apiquian R, Caballero A. Personality and clinical predictors of recurrence of depression. Psychiatric Serv. 1999;50(3):376–380. doi:10.1176/ps.50.3.376
25. Watson D, Naragon-Gainey K. Personality, emotions, and the emotional disorders. Clin Psychol Sci. 2014;2(4):422–442. doi:10.1177/2167702614536162
26. Wu PJ, Chang SM, Lu MK, et al. The profile and familiality of personality traits in mood disorder families. J Affective Disorders. 2012;138(3):367–374. doi:10.1016/j.jad.2012.01.015
27. Ulusahin A, Ulug B. Clinical and personality correlates of outcome in depressive disorders in a Turkish sample. J Affective Disorders. 1997;42(1):1–8. doi:10.1016/s0165-0327(96)00099-7
28. First MB, Spitzer RL, Gibbon M, Williams JB. Structured clinical interview for DSM-IV-TR axis I disorders, research version, patient edition. (SCID-I/P) Biometrics Research Department. New York State Psychiatric Institute; 2002.
29. Li T, Zhou R, Hu J, et al. Translation revision structured clinical interview for DSM-IV-TR Axis I Disorders-Patient Edition (SCID-I/P). Psychiat Res Cent. 2008;2008:1.
30. Young RC, Biggs JT, Ziegler VE, Meyer DA. A rating scale for mania: reliability, validity and sensitivity. Brit J Psych. 1978;133:429–435. doi:10.1192/bjp.133.5.429
31. Hamilton M. A rating scale for depression. J Neurol Neurosurg Psychiatry. 1960;23(1):56–62. doi:10.1136/jnnp.23.1.56
32. Hamilton M. The assessment of anxiety states by rating. Br J Med Psychol. 1959;32(1):50–55. doi:10.1111/j.2044-8341.1959.tb00467.x
33. Gong Y. Revision of Eysenck Personality Questionnaire in China. Psychol Sci Newslett. 1984;1984:(04):13–20+67.
34. Renner F, Penninx BW, Peeters F, Cuijpers P, Huibers MJ. Two-year stability and change of neuroticism and extraversion in treated and untreated persons with depression: findings from the Netherlands Study of Depression and Anxiety (NESDA). J Affective Disorders. 2013;150(2):201–208. doi:10.1016/j.jad.2013.03.022
35. Weber K, Giannakopoulos P, Bacchetta JP, et al. Personality traits are associated with acute major depression across the age spectrum. Aging Mental Health. 2012;16(4):472–480. doi:10.1080/13607863.2011.630375
36. Klein DN, Kotov R, Bufferd SJ. Personality and depression: explanatory models and review of the evidence. Annu Rev Clin Psychol. 2011;7:269–295. doi:10.1146/annurev-clinpsy-032210-104540
37. Deary I, Weiss A, Batty G. Intelligence and personality as predictors of illness and death: how researchers in differential psychology and chronic disease epidemiology are collaborating to understand and address health inequalities. Psychol Sci Public Inter. 2010;11(2):53–79. doi:10.1177/1529100610387081
38. Sparding T, Palsson E, Joas E, Hansen S, Landen M. Personality traits in bipolar disorder and influence on outcome. Article. BMC Psychiatry. 2017;17(1):159. doi:10.1186/s12888-017-1332-0
39. Serrano D, Martí-Lluch R, Cárdenas M, et al. Gender analysis of the frequency and course of depressive disorders and relationship with personality traits in general population: a prospective cohort study. J Affective Disorders. 2022;302:241–248. doi:10.1016/j.jad.2022.01.088
40. Hirschfeld RM, Klerman GL. Personality attributes and affective disorders. Am J Psychiatry. 1979;136(1):67–70. doi:10.1176/ajp.136.1.67
41. Tang TZ, DeRubeis RJ, Hollon SD, Amsterdam J, Shelton R, Schalet B. Personality change during depression treatment: a placebo-controlled trial. Arch. Gen. Psychiatry. 2009;66(12):1322–1330. doi:10.1001/archgenpsychiatry.2009.166
42. Fang A, Porth R, Phillips KA, Wilhelm S. Personality as a predictor of treatment response to escitalopram in adults with body dysmorphic disorder. J Psychiatr Pract. 2019;25(5):347–357. doi:10.1097/pra.0000000000000415
 © 2024 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2024 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
