Back to Journals » Neuropsychiatric Disease and Treatment » Volume 20
Clinical Characteristics of Asymptomatic Thromboembolism in Psychiatric Inpatients: A Retrospective Study
Authors Geng Y, Zhang P, Pan Y, Wang H, Chen Y, Lai J , Hu S
Received 7 November 2023
Accepted for publication 27 February 2024
Published 7 March 2024 Volume 2024:20 Pages 515—522
DOI https://doi.org/10.2147/NDT.S438835
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Roger Pinder
Yimeng Geng,1,* Peifen Zhang,1,* Yanmeng Pan,1,* Huaizhi Wang,2 Yi Chen,1 Jianbo Lai,1,3,4 Shaohua Hu1– 4
1Department of Psychiatry, The First Affiliated Hospital, Zhejiang University School of Medicine, Hangzhou, 310003, People’s Republic of China; 2Department of Psychiatry, Wenzhou Medical University, Wenzhou, 325035, People’s Republic of China; 3The Key Laboratory of Mental Disorder’s Management in Zhejiang Province, Hangzhou, 310003, People’s Republic of China; 4Brain Research Institute of Zhejiang University, Hangzhou, 310003, People’s Republic of China
*These authors contributed equally to this work
Correspondence: Shaohua Hu, Department of Psychiatry, The First Affiliated Hospital, Zhejiang University School of Medicine, The Key Laboratory of Mental Disorder’s Management, Brain Research Institute of Zhejiang University, Hangzhou, 310003, People’s Republic of China, Email [email protected]
Purpose: Venous thromboembolism (VTE) poses a significant threat to individuals’ health, yet its correlation with mental disorders remains underappreciated. Here, we conducted a retrospective analysis to explore the characteristics of psychiatric patients presenting with VTE.
Methods: We retrospectively analyzed psychiatric inpatients with elevated plasma D-dimer levels at the Mental Health Center, First Affiliated Hospital, Zhejiang University School of Medicine, from January 2014 to January 2022. The inclusion criteria comprised comprehensive demographic and clinical profiles, including laboratory and imaging findings.
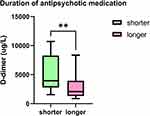
Results: A cohort of 33 eligible patients was included, with plasma D-dimer levels ranging from 880 to 10,700 μg/L FEU. Significantly higher D-dimer levels were observed in patients diagnosed with severe mental disorders (SMD), such as schizophrenia and bipolar disorder, compared to those with mild mental disorders (MMD), including depression and anxiety disorders (p = 0.007). Furthermore, individuals receiving antipsychotic medications for less than one year exhibited elevated D-dimer levels compared to those on treatment for over one year (p = 0.005). However, normalization of D-dimer levels did not demonstrate a significant association with psychiatric diagnosis or treatment duration (p > 0.05).
Conclusion: Our findings suggest that patients diagnosed with SMD or those undergoing antipsychotic treatment for less than one year may have elevated D-dimer levels, indicating a potential predisposition to VTE severity. This underscores the importance of recognizing VTE risk in individuals with severe mental disorders and warrants further investigation into the impact of antipsychotic treatment duration on thrombotic risk.
Keywords: asymptomatic thromboembolism, D-dimer, psychiatric disorder, risk factors
Introduction
Venous thromboembolism (VTE), which includes deep vein thrombosis (DVT) and pulmonary embolism (PE), stands as the third most prevalent cardiovascular disorder, with an overall incidence ranging from 1 to 2 per thousand inhabitants.1,2 VTE is acknowledged as a multifactorial disorder, and associated risk factors, such as psychosocial elements, have garnered increased attention.3,4 Recent findings highlight VTE as a significant contributor to sudden death among inpatients with psychiatric disorders.5
Estimates from the global burden of disease position psychiatric disorders among the top 20 causes of disability.6 Previous investigations have shown that individuals with psychiatric disorders typically experience a reduced life expectancy, on average, by at least 10 years compared to the general population, primarily due to an elevated risk of cardiovascular disease.7–9 Notably, approximately 4% of unanticipated sudden deaths among psychiatric patients are linked to PE, with VTE incidence peaking at 11.6% within a three-month timeframe in this population.10,11 Moreover, reports suggest an exponential increase in VTE incidence with advancing age, particularly among patients older than 40 years.12 However, diagnosing VTE among psychiatric patients presents significant challenges, potentially attributed to factors such as the sedative effects of medications, immobilization, or psychopathological symptoms. Furthermore, symptomatic VTE occurrences could lead to fatal outcomes. Consequently, early screening for asymptomatic VTE, identification of potential triggering factors, and implementation of effective diagnostic measures among psychiatric patients are imperative.
In this study, we undertook a retrospective investigation targeting asymptomatic venous thromboembolism (VTE) among psychiatric inpatients, conducting a comprehensive analysis of the demographic and clinical characteristics of this cohort.
Methods
Participants
The study received approval from the Institutional Review Board of the First Affiliated Hospital, Zhejiang University School of Medicine. Informed consent was waived due to the retrospective nature of the study. Discharge diagnoses were used as search terms in the hospital’s electronic medical record system to identify psychiatric inpatients from January 2014 to January 2022 at the Mental Health Center, First Affiliated Hospital, Zhejiang University School of Medicine. Mental disorder diagnoses followed the criteria outlined in the fourth and fifth editions of the Diagnostic and Statistical Manual of Mental Disorders.
Inclusion criteria involved individuals meeting specific conditions: D-dimer levels exceeding 700μg/L FEU (the upper normal limit), confirmation of VTE through arteriovenous color Doppler ultrasonography of the lower limbs or computed tomography angiography of the pulmonary artery, and an absence of known VTE symptoms such as pain, swelling, difficulty breathing, or hemoptysis. Exclusion criteria included arterial thromboembolism, coagulation dysfunction, severe abnormalities in liver and kidney function, serious infections, gastrointestinal diseases leading to dehydration, recent surgery or trauma, physical limitations, sedentary or bedridden status for extended periods, and pregnancy or lactation.
Measures
The study involved gathering patients’ demographic data, clinical profiles, and results from laboratory and imaging tests. This included information such as age, gender, height, weight, smoking history, duration and diagnosis of psychosis, history of cerebrovascular disease and hypertension, psychotropic medication usage, and plasma D-dimer levels both before and after anticoagulant therapy. Body mass index (BMI) was calculated by dividing weight (in kilograms) by the square of height (in meters).
The clinical presentation of asymptomatic VTE is characterized by the absence of obvious symptoms such as swelling or pain in the legs, chest pain, breathing difficulties, or hemoptysis. Diagnosis relies on elevated D-dimer levels and imaging, i.e., PE reveals the presence of pulmonary thrombosis by computed tomography pulmonary angiography (CTPA), while DVT reveals the presence of venous thrombosis by vascular ultrasound.
Data Analysis
The analysis of the collected data was executed with SPSS, version 21.0. To better elucidate our research findings, we utilized GraphPad Prism 9.4.0 for data visualization. The Mann-Whitney U-test was used to assess the difference between the two numerical variables. Categorical variables are checked precisely by Fisher. The results are presented as mean, standard deviation, and median (minimum–maximum) values for quantitative data and as frequency (n) and percentage (%) values for categorical data. Two-sided, p< 0.05 was considered statistically significant.
Results
Demographic Characteristics
Our study included 33 psychiatric patients who met the specific inclusion and exclusion criteria. Among them, 24 cases presented with asymptomatic VTE manifested as pulmonary embolism (PE), and 9 were diagnosed with deep vein thrombosis (DVT). The distribution of mental health diagnoses included 12 patients with anxiety disorder (AD), 11 with major depressive disorder (MDD), 6 with schizophrenia (SCZ), and 2 with bipolar disorder (BD). Other diagnoses comprised somatoform disorder (SD) and alcoholic dependence syndrome (ADS), each in one patient. Patients were categorized into major mental disorder (SMD) and mild mental disorder (MMD) groups based on severity, with SMD diagnoses including SCZ, BD, SD, and ADS, and MMD diagnoses including AD and MDD.
Treatment regimens involved atypical antipsychotics, selective serotonin reuptake inhibitors (SSRIs), benzodiazepines, and other psychotropic medications. The duration of antipsychotic medication usage varied from 1 month to 20 years. Sedative drugs, like benzodiazepines (e.g., alprazolam), were administered in 17 patients (51.5%), while atypical antipsychotic drugs (e.g., olanzapine and clozapine) were prescribed in 14 cases (42.4%). Additionally, 13 patients had hypertension, and 21 patients had a history of cerebrovascular disease. Detailed demographic characteristics are presented in Table 1
 |
Table 1 Clinical Demographic Characteristics of Patients |
Factors Associated with Plasma Levels of D-Dimer
Plasma D-dimer levels were routinely measured within the first few days of hospitalization, with a mean observed level of 4060.00 ± 2824.88μg/L FEU, ranging from 920 to 10700μg/L FEU, significantly surpassing the normal range of 0–700μg/L FEU. Analysis revealed a correlation between pre-treatment D-dimer levels, the severity of mental illness, and medication duration. Specifically, patients diagnosed with severe mental disorders (SMD) exhibited higher D-dimer levels compared to those diagnosed with mild mental disorders (MMD) (p=0.007) (Figure 1). Moreover, patients receiving antipsychotic medication for less than a year demonstrated elevated D-dimer levels relative to those treated for more than a year (p=0.005) (Figure 2). However, no significant association was observed between pre-treatment D-dimer levels and factors such as thrombus type, history of hypertension, or cardiovascular disease (p>0.05).
The Recovery of D-Dimer Levels After Anticoagulant Treatment
Following the diagnosis of VTE, patients typically undergo conventional anticoagulant therapy, commonly involving subcutaneous injections of low-molecular-weight heparin (LMWH) or oral warfarin, typically administered over a duration of approximately one week.13 In our study, 27 patients (81.8%) received conventional LMWH treatment, while the remaining 6 (18.2%) were administered oral warfarin for a similar duration.
After initiating treatment, D-dimer levels were reassessed. Among the patients, 26 (78.8%) showed a significant reduction in plasma D-dimer levels, with 16 (48.5%) returning to within the normal D-dimer range. Notably, the reduction in D-dimer levels following treatment, as well as the normalization of D-dimer values, were observed independently of factors such as gender, age, and type of mental illness, among others. Detailed features are outlined in Table 2.
 |
Table 2 Recovery of D-Dimer Levels in Patients After Anticoagulant Therapy |
Discussion
VTE poses a significant challenge in hospitals, requiring careful attention. The D-dimer test is reliable for ruling out VTE in outpatient and emergency settings,14,15 and also works well for hospitalized patients.16 Notably, individuals with psychosis have a higher risk of VTE,17–19 highlighting the importance of regularly checking their D-dimer levels for asymptomatic VTE. Our study reveals significant findings regarding patients diagnosed with asymptomatic VTE. Specifically, individuals diagnosed with severe mental disorders (SMD) had higher D-dimer levels compared to those with mild mental disorders (MMD). Additionally, patients in their first year of antipsychotic medication showed elevated D-dimer levels compared to those with a longer medication duration.
D-dimer, a marker indicating fibrinolysis activity, plays a vital role in diagnosing VTE.20 Our study found differences in D-dimer levels among patients with asymptomatic VTE, with lower levels seen in those with mild mental disorders (MMD) compared to severe mental disorders (SMD) (p=0.007). This difference might be because SMD patients tend to be less physically active, which can increase the risk of VTE.21 Higher D-dimer levels at VTE diagnosis could also suggest a higher chance of recurrence and a worse prognosis,22 as seen in COVID-19 patients.23 Therefore, SMD patients with high D-dimer levels may have a poorer outlook regarding VTE.
A seven-year follow-up study found a higher risk of VTE in people taking antidepressants, possibly due to drug-induced blood clotting.24 Possible mechanisms may involve the drug-induced hypercoagulable state, manifested by increased platelet aggregation, antiphospholipid antibodies, hyperprolactinemia, and metabolic symptoms.12,25 Similarly, conventional antipsychotics have been linked to increased VTE risk, especially in the first few months of treatment.26 The nested case-control study showed that individuals who had been prescribed antipsychotics within the past 24 months had a higher risk of VTE than non-users, and that the risk was approximately double for patients who had started the new drug within the past three months.27 This seems to suggest that antipsychotics should initially have a higher risk of blood clots. Our study supported these findings, showing higher D-dimer levels in patients on antipsychotic medication for up to one year (p=0.005). This suggests a higher risk of severe VTE in the first year of treatment. The possible reason is that patients who are just starting treatment may experience lifestyle changes, including reduced activity, which may increase the risk of blood clots. Additionally, during the early stages of treatment, physicians may be adjusting drug doses to achieve optimal efficacy, and higher doses may be associated with an increased risk of blood clots. The specific mechanism needs further exploration.
The risk of thrombosis is related to the duration of the patient’s disease, A longitudinal cohort study shows that individuals with mental disorders have elevated risk for subsequent cardiovascular disease, particularly in the first year after diagnosis.28 However, in our study, no significant difference was found between D-dimer and disease course (p> 0.05). Studies suggest that the type of medication influences D-dimer levels, with first-generation antipsychotics and sedatives being correlated with a higher risk of VTE.26,29,30 In addition, atypical antipsychotics were associated with a higher risk of VTE than conventional antipsychotics.27 However, our study found no significant correlation between D-dimer levels and the use of sedative drugs (p>0.05). We also analyzed the relationship between the use of atypical antipsychotics and D-dimer, and there was no correlation between the two (p>0.05). Additionally, only two patients were prescribed low potency antipsychotics, rendering the data insufficient for statistical analysis.
In future studies, we can stratify patients according to duration of antipsychotic medication and type of disease to make a risk assessment model. Aiming at accurately identifying high-risk patients, early identification and early intervention, and the implementation of targeted preventive measures can ultimately reduce the incidence of VTE and improve the overall health outcomes of psychiatric patients.
Our study has several limitations. The small sample size, retrospective design, and lack of control groups may limit the strength of our findings. Additionally, being conducted at a single center may restrict the generalizability of the results. The absence of imaging assessments and long-term follow-up after discharge are further limitations. Future research should address these limitations by increasing sample sizes, involving multiple centers, incorporating control groups, extending follow-up periods, and conducting comprehensive imaging-based prognostic assessments.
Conclusion
In a nutshell, this retrospective study investigated 33 psychiatric patients diagnosed with asymptomatic VTE during hospitalization. Our findings suggest that individuals with SMD or those in the initial year of antipsychotic medication displayed elevated D-dimer levels compared to those with MMD or longer medication duration. Notably, patients with heightened D-dimer levels, particularly early in antipsychotic treatment or with an SMD diagnosis, warrant careful monitoring and clinical intervention.
Data Sharing Statement
Datasets of this study are available from the corresponding author on reasonable request.
Ethical Statement
This study was conducted in accordance with the Declaration of Helsinki and approved by the institutional review board of the First Affiliated Hospital, Zhejiang University School of Medicine. We have erased patient personal information to ensure that no information will be leaked and patients waived signing informed consent for the study.
Acknowledgments
Thanks to Ms Hongli Qi, Ms Huimin Huang, Ms Yiyi Zhu, Ms Xingle Gao, Mr Danhua Zhang, Mr Jiajun Jiang, Ms Caixi Xi, Ms Lingling Wu, for giving some opinions during the completion of the article.
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Funding
This work was supported by the National Natural Science Foundation [No. 81971271 to SH.H.], the Zhejiang Provincial Natural Science Foundation [No. LQ20H090013 to JB.L.], and the Program from the Health and Family Planning Commission of Zhejiang Province [No.2020KY548 to JB.L.].
Disclosure
The authors declare no conflicts of interest related to the subject of this study.
References
1. Delluc A, Tromeur C, Le Ven F, et al. Current incidence of venous thromboembolism and comparison with 1998: a community-based study in Western France. Thromb Haemost. 2016;116:967–974. doi:10.1160/TH16-03-0205
2. Konstantinides SV. 2014 ESC guidelines on the diagnosis and management of acute pulmonary embolism. Eur Heart J. 2014;35(45):3145–3146. doi:10.1093/eurheartj/ehu393
3. Rosengren A, Freden M, Hansson P-O, et al. Psychosocial factors and venous thromboembolism: a long-term follow-up study of Swedish men. J Thromb Haemost. 2008;6(4):936–941. doi:10.4088/JCP.10m06244gry
4. Enga KF, Braekkan SK, Hansen-Krone IJ, et al. Emotional states and future risk of venous thromboembolism: the Tromso Study. Thromb Haemost. 2012;107:485–493. doi:10.1160/TH11-09-0667
5. Maly R, Masopust J, Hosak L, et al. Assessment of risk of venous thromboembolism and its possible prevention in psychiatric patients. Psychiatry Clin Neurosci. 2008;62(1):3–8. doi:10.1111/j.1440-1819.2007.01773.x
6. Vigo D, Thornicroft G, Atun R. Estimating the true global burden of mental illness. Lancet Psychiatry. 2016;3(2):171–178. doi:10.1016/s2215-0366(15)00505-2
7. Nielsen RE, Banner J, Jensen SE. Cardiovascular disease in patients with severe mental illness. Nat Rev Cardiol. 2020. doi:10.1038/s41569-020-00463-7
8. Goldstein BI, Korczak DJ. Links between child and adolescent psychiatric disorders and cardiovascular risk. Can J Cardiol. 2020;36(9):1394–1405. doi:10.1016/j.cjca.2020.06.023
9. Latvala A, Kuja-Halkola R, Ruck C, et al. Association of resting heart rate and blood pressure in late adolescence with subsequent mental disorders: a Longitudinal Population Study of More Than 1 Million Men in Sweden. JAMA Psychiatry. 2016;73(12):1268–1275. doi:10.1001/jamapsychiatry.2016.2717
10. Manu P, Kane JM, Correll CU. Sudden deaths in psychiatric patients. J Clin Psychiatry. 2011;72(07):936–941. doi:10.4088/JCP.10m06244gry
11. Ishida T, Katagiri T, Uchida H, et al. Incidence of deep vein thrombosis in restrained psychiatric patients. Psychosomatics. 2014;55(1):69–75. doi:10.1016/j.psym.2013.04.001
12. Masopust J, Bazantova V, Kuca K, et al. Venous thromboembolism as an adverse effect during treatment with olanzapine: a case series. Front Psychiatry. 2019;10:330. doi:10.3389/fpsyt.2019.00330
13. Wilbur J, Shian B. Deep venous thrombosis and pulmonary embolism: current therapy. Am Fam Physician. 2017;95:295–302.
14. Wells PS, Anderson DR, Rodger M, et al. Evaluation of D-dimer in the diagnosis of suspected deep-vein thrombosis. N Engl J Med. 2003;349(13):1227–1235. doi:10.1056/NEJMoa023153
15. Le Gal G, Righini M, Roy PM, et al. Prediction of pulmonary embolism in the emergency department: the revised Geneva score. Ann Intern Med. 2006;144:165–171. doi:10.7326/0003-4819-144-3-200602070-00004
16. Karny-Epstein N, Abuhasira R, Grossman A. Current use of D-dimer for the exclusion of venous thrombosis in hospitalized patients. Sci Rep. 2022;12:12376. doi:10.1038/s41598-022-16515-6
17. Lin CE, Chung CH, Chen LF, et al. Increased risk for venous thromboembolism among patients with concurrent depressive, bipolar, and schizophrenic disorders. Gen Hosp Psychiatry. 2019;61:34–40. doi:10.1016/j.genhosppsych.2019.10.003
18. von Kanel R, Margani A, Stauber S, et al. Depressive symptoms as a novel risk factor for recurrent venous thromboembolism: a longitudinal observational study in patients referred for thrombophilia investigation. PLoS One. 2015;10:e0125858. doi:10.1371/journal.pone.0125858
19. Takeshima M, Ishikawa H, Shimizu K, et al. Incidence of venous thromboembolism in psychiatric inpatients: a chart review. Neuropsychiatr Dis Treat. 2018;14:1363–1370. doi:10.2147/NDT.S162760
20. Crawford F, Andras A, Welch K, et al. D-dimer test for excluding the diagnosis of pulmonary embolism. Cochrane Database Syst Rev. 2016;2016(8):CD010864. doi:10.1002/14651858.CD010864.pub2
21. Johansson M, Johansson L, Wennberg P, et al. Physical activity and risk of first-time venous thromboembolism. Eur J Prev Cardiol. 2019;26(11):1181–1187. doi:10.1177/2047487319829310
22. Rinde FB, Jorgensen CT, Pettersen HH, et al. Low D-dimer levels at diagnosis of venous thromboembolism are associated with reduced risk of recurrence: data from the TROLL registry. J Thromb Haemost. 2023;21(7):1861–1868. doi:10.1016/j.jtha.2023.03.026
23. Poudel A, Poudel Y, Adhikari A, et al. D-dimer as a biomarker for assessment of COVID-19 prognosis: d-dimer levels on admission and its role in predicting disease outcome in hospitalized patients with COVID-19. PLoS One. 2021;16(8):e0256744. doi:10.1371/journal.pone.0256744
24. Parkin L, Balkwill A, Sweetland S, et al. Antidepressants, depression, and venous thromboembolism risk: large Prospective Study of UK Women. J Am Heart Assoc. 2017;6:e005316. doi:10.1161/JAHA.116.005316
25. Jonsson AK, Schill J, Olsson H, et al. Venous thromboembolism during treatment with antipsychotics: a review of current evidence. CNS Drugs. 2018;32(1):47–64. doi:10.1007/s40263-018-0495-7
26. Zornberg GL, Jick H. Antipsychotic drug use and risk of first-time idiopathic venous thromboembolism: a case-control study. Lancet. 2000;356(9237):1219–1223. doi:10.1016/S0140-6736(00)02784-7
27. Parker C, Coupland C, Hippisley-Cox J. Antipsychotic drugs and risk of venous thromboembolism: nested case-control study. BMJ. 2010;341(sep21 1):c4245. doi:10.1136/bmj.c4245
28. Shen Q, Mikkelsen DH, Luitva LB, et al. Psychiatric disorders and subsequent risk of cardiovascular disease: a longitudinal matched cohort study across three countries. EClinicalMedicine. 2023;61:102063. doi:10.1016/j.eclinm.2023.102063
29. Di X, Chen M, Shen S, et al. Antipsychotic use and risk of venous thromboembolism: a meta-analysis. Psychiatry Res. 2021;296:113691. doi:10.1016/j.psychres.2020.113691
30. Jonsson AK, Spigset O, Hagg S. Venous thromboembolism in recipients of antipsychotics: incidence, mechanisms and management. CNS Drugs. 2012;26(8):649–662. doi:10.2165/11633920-000000000-00000
 © 2024 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2024 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.