Back to Journals » Integrated Blood Pressure Control » Volume 14
Burden of Undiagnosed Hypertension among Adults in Urban Communities of Southwest Ethiopia
Authors Mogas SB , Tesfaye T , Zewde B , Tesfaye Y , Kebede A , Tadesse M, Gudina EK , Tamiru D , Dadi LS
Received 2 December 2020
Accepted for publication 26 April 2021
Published 21 May 2021 Volume 2021:14 Pages 69—76
DOI https://doi.org/10.2147/IBPC.S293251
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Dr Steven Atlas
Solomon Berhanu Mogas, 1 Temamen Tesfaye, 2 Belay Zewde, 3 Yonas Tesfaye, 4 Ayantu Kebede, 1 Mulualem Tadesse, 5 Esayas Kebede Gudina, 6 Dessalegn Tamiru, 7 Lelisa Sena Dadi 1
1Department of Epidemiology, Jimma University, Jimma, Oromia Region, Ethiopia; 2School of Nursing and Midwifery, Jimma University, Jimma, Oromia Region, Ethiopia; 3Department of Biomedical Sciences, Jimma University, Jimma, Oromia Region, Ethiopia; 4Department of Psychiatry, Jimma University, Jimma, Oromia Region, Ethiopia; 5School of Medical Laboratory Science, Jimma University, Jimma, Oromia Region, Ethiopia; 6Department of Internal Medicine, Jimma University, Jimma, Oromia Region, Ethiopia; 7Department of Nutrition and Dietetics, Jimma University, Jimma, Oromia Region, Ethiopia
Correspondence: Solomon Berhanu Mogas
Department of Epidemiology, Jimma University, P.O.Box-378, Oromia Region, Ethiopia
Tel +251913458961
Email [email protected]
Background: Hypertension (HTN) is the leading risk factor for mortality due to cardiovascular diseases, it accounts for 7% of global disability adjusted life years. In 2015, it was estimated that around 1.13 billion adults had HTN globally with a high prevalence in low and middle-income countries where the health system is weak to diagnose, treat, and control HTN. Most people with HTN are asymptomatic and go undiagnosed for years. Therefore, the aim of this study was to assess the burden of undiagnosed HTN among adults in urban communities of Southwest Ethiopia.
Methods: A community-based cross-sectional study involving 915 adults from June 17 to July 27, 2019 was performed. WHO STEPS questionnaire was used to collect data, and the collected data were entered using Epi Data version 3.1and analyzed using SPSS version 20, respectively. Binary logistic regression was used to check for a possible association between outcome and independent factors. P-value < 0.05 and 95% CI were used on multivariable logistic regression analysis as threshold for significant statistical association.
Results: Undiagnosed HTN in the study area was 21.2% (194). Age (AOR=1.04, 95% CI=1.02– 1.05), BMI with overweight (AOR=2.52, 95% CI=1.35– 4.71), triglyceride (AOR=1.83, 95% CI=1.29– 2.59), and waist to hip ratio (AOR=1.62, 95% CI=1.03– 2.54) were factors significantly associated with HTN.
Conclusion: As compared to studies performed before, the risk of undiagnosed HTN in the current study was high. Age, BMI, triglyceride, and waist to hip ratios were found to be the significant factors for it. Preventing the risk factors and screening of HTN should be promoted for early detection, prevention, and treatment of the burden of the disease on the population.
Keywords: adult, burden, Ethiopia, hypertension, Jimma town, risk, undiagnosed
Corrigendum for this paper has been published
Introduction
Hypertension (HTN) is the leading risk factor for mortality due to cardiovascular diseases and responsible for 7% of global Disability Adjusted Life Years.1,2 In 2015, it was estimated that around 1.13 billion adults had HTN globally with high prevalence in low and middle-income countries where the health system is weak to diagnose, treat, and control HTN.3
In African regions, the prevalence of HTN was highest among adults with an age adjusted prevalence of 25.9%. But, this prevalence varied significantly by population group, occupation, and degree of urbanization.4 This implies a massive economic burden for the continent in two ways; one is a cost of caring for complications arising from HTN, and the second is indirect costs as a result of lost productivity of workers struck by the complications of it like stroke, heart failure, and ischemic heart diseases. Besides the above losses, loss of savings and assets associated with rehabilitation following stroke or dialysis of renal failure were also there.5
Globally, if the current blood pressure levels persist over 10 years and if HTN goes untreated, it will nearly costs US$1 trillion, and indirect costs could be as high as US$3.6 trillion annually.6
Despite HTN being a public health concern that we cannot ignore, most people with HTN are asymptomatic and go undiagnosed for years. HTN rarely causes symptoms and it is known as the “silent killer”.7,8 Therefore, to halt the complications of HTN and design the right intervention mechanism, surveillance of both detected and undetected HTN is important.9 Both in developed and developing countries undiagnosed HTN is a problem. In the USA, around one in six or 11 million adults with HTN do not known that they have it and are not being treated. Similarly, in China only 44.7% of hypertensive patients are awarethat they are hypertensive. The existence of a high prevalence of undiagnosed HTN will definitely lead to a substantial health and economic burden.10,11
In developing countries, several studies assessed undiagnosed HTN prevalence in diverse populations.12,13 A systematic review conducted in Sub-Saharan Africa found that only 27% of people with HTN know their HTN status.14 Therefore, due to this, a large proportion of those in the region with HTN probably remain undiagnosed, untreated, or inadequately treated. So, this signals the need to increase the detection rate of existing HTN and the provision of resources for adequate treatment which helps to control the societal and economic effect of cardiovascular diseases in the region.14–16
Different factors contribute to undiagnosed HTN status. A study conducted to assess the relationship between undiagnosed HTN and health-related variables found that physical examination, utilization of health services, Body Mass Index (BMI), chronic illnesses, self-rated health status, and headache were significantly associated factors with undiagnosed HTN.17
In Ethiopia, based on pooled epidemiological studies, the prevalence of HTN is found to be 23.7% in urban and 14.7% in rural areas.18 Early diagnosis and treatment are essential for HTN management, however, in developing countries like Ethiopia, though the prevalence of HTN is very high and intervention design depends on the level of the known HTN. The majority of the communities are not aware of their HTN status and left undiagnosed, untreated, and uncontrolled. In addition, the number of studies conducted in Ethiopia to assess communities’ awareness about their HTN status is very scarce.19 So, this study was planned to assess the burden of undiagnosed HTN among adults in an urban community of Southwest Ethiopia.
Methods and Materials
Study Setting and Period
The current study was performed in Jimma Town from June 17 to July 27, 2019. The town is found in the Southwest part of Ethiopia, Oromia Regional State, and 352 km from the capital city Addis Ababa.
Study Design and Population
A community-based cross-sectional study was performed on the adult populations aged ≥18 years in Jimma town. All adult residents who had lived at least 6 months in the town prior to the data collection were included. However, those adults with known and medically diagnosed with HTN, pregnant women, and adults with physical deformity (kyphosis, sclerosis) were excluded to control for the potential for misclassification of physical measurements like BMI, WC, and waist to hip ratio due to Kyponic posture and pathological hardening of tissue by kyphosis, and sclerosis, respectively.
Sample Size and Sampling Procedure
A single population proportion formula was used to determine the sample size by considering 95% CI, 4% margin of error, 10% non-response rate, 1.5 design effects, and 23.7% HTN prevalence.18 The final sample size was 956.
To select the study participant’s, a multi-stage sampling technique was performed on 17 Kebeles (the lowest administrative structure in Ethiopia) found in the study area. First, six Kebeles from 17 were selected using a simple random sampling technique, and based on the proportion to size of the Kebeles, a Systematic random sampling technique was used to select study units. For households (HHs) with more than one study subject, a lottery method was used to select a participant.
Data Collection Technique and Measurement
The WHO STEPS questionnaire,20 was adapted based on the objective and local context of the study setting, was used to collect the data. The data collection tool was initially prepared in English and translated to the local languages Afan Oromo and Amharic. Pre-test was performed in Agaro town 2 weeks before applying it to the final data collection. A stepwise approach was performed to collect socio-demographic, behavioral, physical data, and biochemical measurements. Seven trained professional nurses selected based on qualification, prior experience, and ability to speak the local language. Training on interviewing approach, sample taking, anthropometric measurement, and data recording were given to the data collectors for 4 days before the real data collection. Close supervision by the research team were performed during the interviews and measurements by the data collectors.
Physical Measurements
The waist circumference, waist to hip ratio, the height and weight needed to calculate body mass index (BMI), and blood pressure were taken. Using a stadiometer (Seca, Germany) the height of the study participants was measured to the nearest 0.1 cm with the subjects positioned at the Frankfurt Plane and the four points (heel, calf, buttocks, and shoulder) touching the vertical stand and their shoes taken off. Before starting the measurements of height, the stadiometer was checked using calibration rods. Weights were measured with the subjects wearing light clothes and shoes taken off using a digital weight scale to the nearest 0.1 kg. The validity of the scale was checked every morning and between the measurements using an object of a known weight. BMI was calculated by dividing weight in kilograms of adults with height in meters squared formula. BMI<18.5 kg/m2 was considered as underweight, 18.5–24.9 kg/m2 was normal, 25–29.9 kg/m2 was overweight, and BMI≥30 kg/m2 was obese.21
Waist circumferences (WC) were measured at the midway between the lowest costal margin at the mid-clavicular line and the anterior superior iliac spine using fixed tension tape. WC values >80 cm for women and >94 cm for men were considered high according to the WHO recommendation.22
Blood pressure (BP) was measured from adults in a sitting position from the right arm in triplicate using an Aneroid Sphygmomanometer with small, medium, and large cuff size,23 as fit to the subjects after 5 minutes of rest. The subsequent measurements were performed 5 minutes apart from the first measurement taken. Using the WHO recommendation, the mean systolic and diastolic blood pressures of adults were considered for analysis. Hypertension is defined as systolic BP of ≥140 mmHg and/or diastolic BP of ≥90 mmHg.24
Biomedical Measurements
Low-density lipoprotein (LDL), high-density lipoprotein (HDL), random and fasting blood glucose, triglyceride (TG), and total cholesterol (TC) level measurements were done. Five millileters of venous blood was collected from adults to determine their lipid profiles and random and fasting blood glucose levels. Serum was carried out in ABX Pentra 400 Automated Chemistry Machine (Horiba ABX SAS, 34184 Montpellier, France) at Jimma Medical Center (JMC) Clinical chemistry core laboratory to determine lipid profile and random and fasting blood glucose. Low-density lipoprotein level of study participants was calculated by using Friedewald formula.25
DM was diagnosed based on the American Diabetes Association and IDF diabetes mellitus classification criteria with fasting blood glucose (FBG) of ≥126 mg/dL and random blood glucose (RBG) of ≥200 mg/dL being considered as positive for DM.26,27
TC ≥ 200 mg/dL of adults was considered as high and if it is <200 mg/dL as normal. The optimal level of LDL was less than 100 mg/dL and greater than 100 mg/dL was defined as high. Triglycerides level was considered as normal when it was less than 150 mg/dL and if greater than 150 mg/dL considered high. HDL is considered as desirable if it is >40 mg/dL for men and >50 mg/dL for women, otherwise it was classified as low.28 All laboratory values were determined by a laboratory technologist, who did not know the participant’s history or other measurements.
Variables
Undiagnosed HTN was the outcome variable; Socio-economic and demographic (age, sex, education, income, religion, ethnicity, occupation, family size) factors, behavioral factors (current Alcohol consumption, current cigarette smoke, current Khat chew, physical activity, and sedentary lifestyle), Anthropometric measurements (waist to hip ratio, waist circumference, and BMI), and Biochemical tests (TC, LDL, HDL, triglyceride and Blood Glucose) were the independent variables.
Data Management and Statistical Analysis
First, the data were checked for completeness and consistency, cleaned for outliers and missing values. Epi-Data version 3.1 and SPSS version 20 was used for data entry and analysis, respectively. Descriptive analyses of the background characteristics and potential factors for HTN of study participants were performed. Binary logistic regression was performed to determine the association between HTN and explanatory variables. First, Bivariate analysis was performed to nominate variables for the next analysis using a p-value≤0.25, and multivariable logistic regression analyses were used to assess the presence and strength of association between explanatory variables and the outcome variable. Adjusted odds ratios (AORs) with their corresponding 95% confidence intervals (CIs) at a p-value≤0.05 were used to determine the presence of association and its strength. Variance inflation factor (VIF) was used to check for multicollinearity between explanatory variables. VIF value of 1–10 was used to declare the absence of multicollinearity.
Results
Sociodemographic Characteristics of Study Participants
From the total 956 sample size considered for the study, 915 adults participated, which gives a response rate of 95.7%. The median age of the study participants was 35 years. Females comprised 48%, and 71.5% of them were married (Table 1).
 |
Table 1 Sociodemographic Characteristics of Study Participants in an Urban Community of South West Ethiopia, 2019 |
Behavioral Characteristics of Study Participants
From the 915 adults participated in the current study, 7.9% of them smoked cigarettes, 16.7% consumed alcohol, and 35.1% chewed Khat during the study period (Table 2)
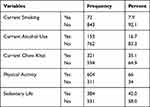 |
Table 2 Behavioral Characteristics of Study Participants in an Urban Community of South West Ethiopia, 2019 |
Anthropometric Characteristics of Study Participants
The current study identified 34% of study participants with a high LDL level, 27.9% with a high level of triglyceride, and 3.1% with undiagnosed DM (Table 3)
 |
Table 3 Anthropometric and Biochemical Characteristics of Study Participants in an Urban Community of South West Ethiopia, 2019 |
Risk of Unrecognized HTN and Factors Associated with It
In the current study, the risk of Undiagnosed HTN was 21.2% (194), and, from this, females contributed 94 (48.4%). We found 18 variables nominated for multivariable analysis and, of them, four variables (age, BMI, triglyceride, and waist to hip ratio) showed a significant association with undiagnosed HTN. The VIF showed no correlation among explanatory variables.
As the age of adults increased by a year, the risk of HTN increased by 1.04 (AOR=1.04, 95% CI=1.02–1.05). The risk of HTN was 2.52-times (AOR=2.52, 95% CI=1.35–4.71) higher among overweight adults than normal-weight adults. Adults with a high triglyceride levels showed a 1.83-times (AOR=1.83, 95% CI=1.29–2.59) higher risk of undiagnosed HTN than adults with normal triglyceride levels. Adults with a high waist to hip ratio were at a 1.62-times (AOR=1.62, 95% CI=1.03–2.54) higher risk of undiagnosed HTN than adults with normal triglyceride levels (Table 4).
 |
Table 4 Multivariable Analysis Result of Undiagnosed HTN and Factors Associated with It |
Discussion
The aim of the current study was determining the burden of Undiagnosed HTH and factors associated it. We found that the undiagnosed HTN in the study area was 21.2% (194), and four variables (age, BMI, triglyceride, and waist to hip ratio) showed a significant association with it.
The risk of HTN in the current study was 21.2%, which was higher as compared to studies performed in the United States of America and Addis Ababa, Ethiopia.8,19 However, it was lower as compared to studies performed in Ireland, in Ghana among Bus Drivers, traders at regional markets in Nigeria, and a systematic review in sub-Saharan Africa.8,12–14 The observed lower risk in the current study might be due to differences in socio-demographic characteristics of study participants. The current study was performed on the general adult populations, but, the studies performed in Ireland, Ghana among Bus Drivers, Nigeria in traders at regional markets, and the systematic review in sub-Sahara were performed on populations with greater vulnerability to HTN as compared to the general adult populations.
In most cases, the damage done by HTN takes place over time. If high blood pressure or HTN is left undiagnosed, it can lead to stroke, heart attack, heart failure, kidney disease or failure, etc.22
In our study, the age of study participant’s was significantly associated with HTN. The finding was supported by different studies.23–25 As age increases, there will be an increased stiffness of the aorta and arterial walls which might in this case contribute to increased blood pressure.25
Overweight adults with BMI >25 showed a higher risk of HTN than normal-weight adults. Similar findings reported from different studies performed before showed an increased risk of HTN among overweights.23,25–29 Earlier onset of cardiovascular morbidity and an increased cardiovascular risk were associated with excess body weight. It is well established that excess body weight is associated with the activation of both the sympathetic nervous system and the renin–angiotensin system contributing to the emergence of HTN. The association between overweight and HTN is through neuroendocrine mechanisms and, most recently, factors resulting from adipose tissue are supposed to play a major role.26
Participants with higher triglyceride levels showed an increased risk of undiagnosed HTN compared participants with normal triglyceride levels. The risk of stroke, heart attack, and heart diseases are affected by the hardening of the arteries (atherosclerosis) which is caused by high triglyceride levels in the body. They can be part of metabolic syndrome, which also includes too much fat around the waist, high blood pressure, high blood sugar, and abnormal cholesterol levels.30
In the current study, adults with a high waist to hip ratio showed a higher risk of undiagnosed HTN than adults with normal waist to hip ratio. Truncal obesity identified by an increased waist–hip ratio (WHR) is a significant risk factor for atherosclerosis. It increases coronary heart disease and one of the mechanisms hypothesized is high blood pressure.31
The community based nature and the large sample size used for the current study were its strength. However, the study did not consider acute and chronic illnesses other than HTN, which may in this case affect the blood pressure of participants and inflate the findings. The study excludes pregnant mothers, and pregnancy induced hypertension and pregnancy pre-existing hypertensions were not considered.
Conclusion
As compared to studies performed before, the risk of undiagnosed HTN in the current study was high. Age, BMI, triglyceride and waist to hip ratios were found to be factors for it. Due to the existence of the higher risk of HTN in the study population, there will be a great risk of stroke, heart attack, and other cardiovascular diseases secondary to HTN. Preventing the risk factors and regular screening practices should be promoted for early detection, prevention, and treatment of HTN. Health facilities should consider measuring HTN and the potential risk factors during their routine services provision for adults.
Data Sharing Statement
Readers who will be in need of data and materials of the current study can communicate with the correspondence author.
Ethical and Environmental Considerations
The current study was conducted in accordance with the Declaration of Helsinki. Written informed consent was obtained from study participants after giving the important message about the nature of the study. A supportive letter was obtained from the towns and respective Kebele administrations. Ethical clearance was obtained from Jimma University, Institute of Health Ethical Review Committee. Using coding system all the participants’ data were kept confidential and no direct benefit were delivered for the participants except free lipid profiles, blood glucose, and HTN tests. Those who were found to have HTN and abnormal metabolic syndromes were advised and linked to nearby health facilities for further evaluation. All materials and equipment used for the study were safely managed and disposed of accordingly.
Acknowledgments
The authors would like to acknowledge the data collectors and study participants for their positive cooperation to effectively conduct the study. Our sincere gratitude also goes to Jimma University for funding the project.
Author Contributions
All authors made substantial contributions to the conception and design, acquisition of data, or analysis and interpretation of data; took part in drafting the article or revising it critically for important intellectual content; gave final approval of the version to be published; and agree to be accountable for all aspects of the work.
Funding
The research project was funded by Jimma University. The funding source of this study did not have any role in conducting the study or in analyzing data or in the writing of this paper.
Disclosure
The authors declare that they have no competing interests.
References
1. Stephen S Lim, Theo Vos, Abraham D Flaxman, Goodarz Danaei, Kenji Shibuya HA-R. A comparative risk assessment of burden of disease and injury attributable to 67 risk factors and risk factor clusters in 21 regions, 1990–2010: a systematic analysis for the Global Burden of Disease Study 2010A. Lancet. 2014;380(9859):2224–60
2. Global T, Risk M, Diseases C. Cardiovascular disease, chronic kidney disease, and diabetes mortality burden of cardiometabolic risk factors from 1980 to 2010: a comparative risk assessment. LANCET Diabetes Endocrinol. 2014;2(8):634–647. doi:10.1016/S2213-8587(14)70102-0.
3. Zhou B, Bentham J, Di Cesare M, et al. Worldwide trends in blood pressure from 1975 to 2015: a pooled analysis of 1479 population-based measurement studies with 19·1 million participants. Lancet. 2017;389(10064):37–55.
4. Guwatudde D, Nankya-Mutyoba J, Kalyesubula R, et al. The burden of hypertension in sub-Saharan Africa: a four-country cross sectional study. BMC Public Health. 2015;15(1):1–8. doi:10.1186/s12889-015-2546-z
5. van de Vijver S, Akinyi H, Oti S, et al. Status report on hypertension in Africa - Consultative review for the 6th Session of the African Union Conference of Ministers of Health on NCD’s. Pan Afr Med J. 2013;16:1–17. doi:10.11604/pamj.2013.16.1.3150
6. Gaziano TA, Bitton A, Anand S. The global cost of nonoptimal blood pressure. J Hypertens. 2009;27:1472–1477. doi:10.1097/HJH.0b013e32832a9ba3
7. World Health Organization. Hypertension: putting the pressure on the silent killer. Hypertens Putt Press Silent Kill. 2016;1–19.
8. Mosca I, Kenny RA. Exploring differences in prevalence of diagnosed, measured and undiagnosed hypertension: the case of Ireland and the United States of America. Int J Public Health. 2014;59(5):759–767. doi:10.1007/s00038-014-0573-7
9. Park S, Gillespie C, Baumgardner J, et al. Modeled state-level estimates of hypertension prevalence and undiagnosed hypertension among US adults during 2013–2015. J Clin Hypertens. 2018;20(10):1395–1410. doi:10.1111/jch.13388
10. Merai R, Siegel C, Rakotz M, et al. Morbidity and Mortality Weekly Report CDC Grand Rounds: a Public Health Approach to Detect and Control Hypertension. MMWR. 2016;65(45):1261–1264. doi:10.15585/mmwr.mm6545a3
11. Jiapeng L, Yuan L, Xiaochen Wang BS, Xinyue L. Prevalence, awareness, treatment, and control of hypertension in China: data from 1·7 million adults in a population-based screening study (China PEACE Million Persons Project). Lancet. 2017;390(10112):2549–2558.
12. Anto EO, Owiredu WKBA, Adua E, et al. Prevalence and lifestyle-related risk factors of obesity and unrecognized hypertension among bus drivers in Ghana. Heliyon. 2020;6(1):e03147. doi:10.1016/j.heliyon.2019.e03147
13. Vincent GO, Adaji JO, Umeonwuka CI. Prevalence of undiagnosed hypertension among traders at a regional market in Nigeria. Ann Med Heal Serv Res. 2017;7(2):97–101.
14. Ataklte F, Erqou S, Kaptoge S, Taye B, Echouffo-Tcheugui JB, Kengne AP. Burden of undiagnosed hypertension in sub-saharan africa: a systematic review and meta-analysis. Hypertension. 2015;65(2):291–298. doi:10.1161/HYPERTENSIONAHA.114.04394
15. Addo J, Smeeth L, Leon DA. Hypertension in sub-Saharan Africa: a systematic review. Hypertension. 2007;50(6):1012–1018. doi:10.1161/HYPERTENSIONAHA.107.093336
16. Cappuccio FP, Micah FB, Emmett L, et al. Prevalence, detection, management, and control of hypertension in ashanti, West Africa. Hypertension. 2004;43(5):1017–1022. doi:10.1161/01.HYP.0000126176.03319.d8
17. Zhou J, Fang S. Association between undiagnosed hypertension and health factors among middle-aged and elderly chinese population. Int J Environ Res Public Health. 2019;16:7.
18. Kibret KT, Mesfin YM. Prevalence of hypertension in Ethiopia: a systematic meta-analysis. Public Health Rev. 2015;36(1):. doi:10.1186/s40985-015-0014-z
19. Getachew F, Dirar A, Solomon D. Prevalence of undiagnosed hypertension and associated factors among residents in Gulele Sub-City, Addis Ababa, Ethiopia. J Community Med Health Educ. 2018;08(01):6–10.
20. Bonita R, Winkelmann R, Douglas KA, de Courten M. The WHO stepwise approach to surveillance (steps) of non-communicable disease risk factors. Glob Behav Risk Factor Surveill. 2003:9–22.
21. Yunka TT, Mogas SB, Zawdie B, et al. The hidden burden of diabetes mellitus in an urban community of southwest ethiopia. Diabetes, Metab Syndr Obes Targets Ther. 2020;13:2925–2933. doi:10.2147/DMSO.S269386
22. World Health Organization. Waist circumference and waist–hip ratio. Report of a WHO Expert Consultation. Geneva.
23. Frese EM, Fick ASS. Blood pressure measurement guidelines for physical therapists. Cardiopulm Phys Ther J. 2011;22(2):5–12. doi:10.1097/01823246-201122020-00002
24. Chobanian AV, Bakris GL, Black HR, et al. The seventh report of the joint national committee on prevention, detection, evaluation, and treatment of high blood pressure: the JNC 7 report. J Am Med Assoc. 2003;289(19):2560–2572. doi:10.1001/jama.289.19.2560
25. Hata Y. Application of Friedewald’s LDL-cholesterol estimation formula to serum lipids in the Japanese population. Jpn Circ J. 1986;50(12):1191–2000. doi:10.1253/jcj.50.1191
26. American Diabetes Association. Diagnosis and classification of diabetes mellitus. Diabetes Care. 2014;37(1):S81–90. doi:10.2337/dc14-S081
27. International Diabetes Federation. IDF clinical practice recommendations for managing type 2 diabetes in primary care. international diabetes federation – 2017. 2017:1–32.
28. (ATP-IV) TLR. National cholesterol education program expert panel on detection, evaluation, and treatment of high blood cholesterol in adults; 2012. Available from: https://connect.springerpub.com/content/reference-book/978-0-8261-7934-0/back-matter/part02/back-matter/bmatter4https://connect.springerpub.com/content/reference-book/978-%0A0-8261-7934-0/back-matter/part02/back-matter/bmatter4.
29. Association AH. Consequences of high blood pressure [Internet]; 2020. Available from: https://www.heart.org/en/health-topics/high-blood-pressure/health-threats-from-high-blood-pressure.
30. Singh S, Shankar R, Singh GP. Prevalence and Associated risk factors of hypertension: a cross-sectional study in urban varanasi. Int J Hypertension. 2017;2017:1–10. doi:10.1155/2017/5491838
31. Gudina K, Bonsa F, Gudina EK, Hajito KW. Original article prevalence of hypertension and associated factors in Bedele Town, Southwest Ethiopia. Ethiopian Journal of Health Science. 2014.DOI: http://dx.doi.org/10.4314/ejhs.v24i1.3
 © 2021 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2021 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
