Back to Journals » Integrated Blood Pressure Control » Volume 16
Blood Pressure Examination Habit and Its Determinants Among Civil Servants in Arba Minch Town: A Cross-Sectional Study – Using Hurdle Poisson Regression Model
Authors Legisso TZ , Mamo BG, Bimrew AM, Fikadu T
Received 16 December 2022
Accepted for publication 2 March 2023
Published 11 March 2023 Volume 2023:16 Pages 1—9
DOI https://doi.org/10.2147/IBPC.S397760
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Professor Turgay Celik
Tesfahun Zewde Legisso,1 Bereket Getachew Mamo,1 Abebaw Miskir Bimrew,1 Teshale Fikadu2,3
1Department of Statistics, College of Natural Sciences, Arba Minch University, Arba Minch, Ethiopia; 2Department of Public Health, College of Medicine and Health Science, Arba Minch University, Arba Minch, Ethiopia; 3Department of Nutrition and Dietetics, Faculty of Public Health, Institute of Health, Jimma University, Jimma, Ethiopia
Correspondence: Tesfahun Zewde Legisso, Email [email protected]
Background: Hypertension is a common non-communicable disease detected through blood pressure measurement that makes periodic health examinations crucial for the detection, prevention, and timely treatment.
Objective: To assess the frequency of blood pressure examination and its determinant among civil servants in Arba Minch Town, south Ethiopia.
Methods: From February to March 2020 an organization-based cross-sectional study design was employed among civil servants in Arba Minch town. Data were collected from 580 randomly selected civil servants using a well-structured questionnaire. Hurdle Poisson regression model was conducted to identify determinants of frequency of blood pressure examination using R version 4.0.2.
Results: A total of 407 (70.2%) civil servants had never examined their blood pressure within a year before the study time. The mean frequency of blood pressure examination was 0.71 with a standard deviation of 1.46. The hurdle Poisson regression analysis indicates age above 40 years (IRR = 6.11, p < 0.001), elevated blood pressure (IRR = 1.48, p < 0.001), no family history of hypertension (IRR = 0.59, p < 0.001) had significant effects on the expected number of non-zero counts blood pressure examination. And education status (OR; 2.39, p < 0.05), poor knowledge about hypertension, not getting advice from health professionals (OR = 8.93, p < 0.001), and age above 40 years had significant effects on not taking blood pressure examination.
Conclusion: The frequency of blood pressure examinations among civil servants was found to be low. This study reveals age, elevated blood pressure, family history of hypertension, getting advice, and knowledge on hypertension were found to be determinants of the frequency of blood pressure examination. Thus, concerned health authorities and medical workers should work on these factors to prevent and detect hypertension among apparently healthy civil servants.
Keywords: Arba Minch, blood pressure examination, Ethiopia, hurdle Poisson regression, hypertension
Background
Hypertension is a major public health problem that causes heart disease, stroke, renal failure, premature death, and disability.1 And maintaining blood pressure in the normal range reduces 50% risk of heart failure, 40% risk of cerebrovascular accidents, and 25% risk of myocardial infarction.2 Approximately 17 million people die each year worldwide as a result of cardiovascular disease. Of these, 9.4 million die from complications of hypertension.3
Globally, diagnosed hypertension in 2019 was 59% in women and 49% in men, with less than half receiving treatment, 47% in women and 38% in men. Of these, only 23% of women and 18% of men controlled their blood pressure.4 This means that significant proportions of the world’s population were not diagnosed, were not treated after diagnosis, and did not control their blood pressure during treatment. Due to difference in risk factors such as unhealthy diet, lack of exercise, and obesity, the prevalence of hypertension varies among regions of the world. It is lower in high-income countries (28.5%) than in low- and middle-income countries (31.5%). It was also slightly higher in men (31.9%) than in women (30.1%).5
Hypertension is a growing problem in developing countries, including Africa, and is the leading cause of morbidity and mortality from non-communicable diseases, accounting for 13% of all deaths worldwide.6 In many developing countries, more and more people are suffering from heart attack and stroke due to undiagnosed and uncontrolled risk factors such as high blood pressure.1 The staggering rise in hypertension and cardiovascular disease in Africa will have significant economic implications as there are many productive age groups affected by hypertension and its complications.7
Hypertension is a public health problem in Ethiopia and was the country’s seventh leading cause of death in 2000–2001, accounting for 1.4% of all deaths.8 A study indicates about one in four people in Ethiopia suffered from hypertension, and this was higher in the urban population (23.7%) than in the urban-rural population (14.7%). It was slightly higher in men (20.6%) than in women (19.2%).9 Despite this, about 37–78% of hypertensive patients were unaware of their blood pressure situation,10 and 12.3% to 40% of the population affected by undiagnosed hypertension.11–16 This evidence suggests the importance of blood pressure screening for preventive, control and timely treatment of hypertension.
Periodic health examination (PHE) is a common component of preventive medicine that helps to detect risk factors and early signs of disease, used as a tool for early case finding, preventing illness through early intervention, and includes physical examination and screening tests.2 Also, it is essential to increase health-seeking behavior of the population.17 Hypertension is a common non-communicable disease that detects commonly through unexpected blood pressure measurements which makes PHE crucial for the detection, prevention, and timely treatment.2 And BP is widely measured during PHE.18
There are various blood pressure screening methods around the world. Among them, office blood pressure measurement (OBP) is commonly and widely used to detect hypertension. The second commonly used method is ambulatory blood pressure monitoring (ABPM). This type of blood pressure screening method provides information about mean 24-hour blood pressure, means daily blood pressure, means nighttime blood pressure, and calculated nighttime blood pressure drop rate, and is the best way to diagnose hypertension. A third method is home blood pressure monitoring (HBPM). It is widely used in many countries and is the best method for long-term hypertension tracking. Others include blood pressure measurement in pharmacies and public places (kiosks), cuffless wearable blood pressure measurement, and blood pressure measurement using mobile technology.19–21 In the United States, a combination of office blood pressure (OBP), ambulatory blood pressure monitoring (ABPM), and home blood pressure monitoring (HBPM) screening methods is recommended.22 But in our study only office blood pressure measurement (OBP) is used in government and private clinical settings screening for hypertension because other methods are not available.
To reduce the consequence of hypertension periodic blood pressure examination is mandatory. But there is limited evidence on periodic blood pressure examination in Ethiopia; hence, the objective of this study was to identify the determinants of periodic blood pressure examination among civil servants in Arba Minch town hypothesizing that there are factors associated with periodic blood pressure examination.
Materials and Methods
Study Design and Sources of Data
A cross-sectional study design was conducted in February–March among civil servants in the town of Arba Minch, Gamo Zone, Southern Ethiopia. Primary data were collected using a structured questionnaire administered by a personal interviewer that addressed the frequency of 12-month blood pressure assessments and related factors. Civil servants who had worked in the town of Arba Minch for at least 12 months and on work during the data collection were included, but those who had regular medical visits and already diagnosed as hypertension were excluded from the study.
Knowledge about hypertension was measured using 19 standard questions.23 The collected data were coded “1” for correct answers and “0” for incorrect answers. We then summed up the correct answers and categorized those who scored above average as “know good” and “not good otherwise”.
Study Variables
The dependent and independent variables with their description are discussed in Table 1.
 |
Table 1 Coding and Variable Description for the Analyzed Blood Pressure Examination |
Sample Size Determination
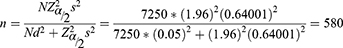
A sample size of 580 was determined using a formula in [i]1 with the assumption of 5% level of significance, 0.05 margin of error, and standard deviation of 0.64001 from pilot study conducted in the study area.24
Sample size n = 580 were determined as shown below
where N is the total number of civil servants which is 7250, d is the margin of error, s is the standard deviation of blood pressure examination per year and  = 1.96.
= 1.96.
Sampling Technique
To get the sampling frame, we used secondary data from all civil service organizations found in Arba Minch town. Information from the government offices showed that there were 7250 civil servants. The respondents of this study were selected using single stage simple random sampling technique.
Statistical Models
The outcome variable of this study is the number of blood pressure examinations of a person within the last 12 months which is a count data. Count regression models are often used to model count data and analysis of count data can be done in various fields, including health science. The most commonly used are Poisson and negative binomial regression models. One of the assumptions of the Poisson model is that the variance equals the mean. However, count data often deviate from the Poisson distribution. This is because the variance of the observed variable, known as over-dispersion, becomes larger than the mean as the percentage of zeros increases. In other words, excessive zeros in count responses can cause over-dispersion and lead to biased inferences. Negative binomial (NB) regression models, the most popular alternative to Poisson regression, address over dispersion by explicitly modeling correlated and sparse events via latent variables. Although the NB regression model can deal with over scattering, it is not appropriate to model data with a high percentage of zero counts. As a result, the regression model zero-inflated Poisson, zero-inflated negative binomial, and hurdle Poisson or hurdle negative binomial are used.25,26
When multiple maximum likelihood counting models are available, the Akaike Information Criterion (AIC) and the Bayesian Schwartz Information Criterion (BIC) can be used to compare the performance of alternative models based on multiple probability measures.27,28
In this study, hurdle Poisson regression models were used to model the number of blood pressure examination of a person within a year after comparing with Poisson, negative binomial, zero-inflated Poisson, zero-inflated negative binomial, hurdle Poisson, and hurdle negative binomial regression models (Table 2).
 |
Table 2 Socio Demographic and Health-Related Factors of Civil Servants in Arba Minch Town |
Hurdle Poisson Model
The hurdle model is a binary mixed model consisting of a probability of zero counts and a truncated Poisson distribution.12 Unlike the zero-inflated model which assumes that zero observations have two distinct origins namely structural and sampling, a hurdle model assumes that all zero observations only have one origin namely “structural”. Let the response variables of the ith count data Yi, i = 1, 2, 3, …, n, where n indicates the total number of count data. If the count data is distributed Poisson, the probability distribution for the Hurdle Poisson is given as follows:
For this study, P (i) is the probability of not taking blood pressure examination. The most natural choice for modeling the probability of zero is the logistic regression model
where  is the ith row of covariate matrix Z and are unknown q-dimensional column vector of parameters.
is the ith row of covariate matrix Z and are unknown q-dimensional column vector of parameters.
Count data (truncated at zero) are modeled using Poisson regression model:
Where  is the ith row of covariate matrix X and
is the ith row of covariate matrix X and  are unknown p-dimensional column vector of parameters. The Maximum Likelihood Estimation (MLE) method is used to estimate parameters in the count models.26
are unknown p-dimensional column vector of parameters. The Maximum Likelihood Estimation (MLE) method is used to estimate parameters in the count models.26
Model Compressions of Count Data Analysis
The predictable power of the count models Poisson, NB, ZIP, ZINB, HP, and HNB were compared for the zero counts. Poisson and Negative Binomial models underestimated zero counts, the zero-inflated models overestimated zero counts and the hurdle models captured all zero values. The AIC and BIC test statistics suggest that the Poisson hurdle Regression model is a significant improvement over the other count models since the value of AIC and BIC are smaller than the other models. Consequently, the analysis is done by applying this model only (Table 2).
Ethical Consideration
Ethical approval and clearance were obtained from the College of medicine and health Sciences, Arba Minch University. Written informed consent was obtained from the study participant after informing the purpose of the study. The study conducted corresponds to the Declaration of Helsinki.
Results
A total of 580 civil servants with a mean age of 36 years participated in the study. The majority of respondents were male 331 (57.1%), married 302 (52.1%), had at least a first degree 367 (63.3%), and had a normal body mass index 447 (77.1%). Less than 1 in 5 had elevated blood pressure and a family history of hypertension (Table 3).
 |
Table 3 Model Comparison Using AIC, BIC and Number of Zeros |
Frequency of Blood Pressure Examination
More than seven out of ten civil servants 407 (70.2%) never examined their blood pressure for the last 12 months. The minimum frequency of examination was 0 and the maximum frequency of examination was 8 with 0.71 mean and 1.458 variances. This indicated that the distribution was extremely skewed right with a spike at zero Figure 1.
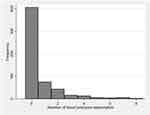 |
Figure 1 Frequency of blood pressure examination for the last 12 months among civil servants in Arba Minch town. |
Results of Hurdle Poisson Regression Analysis
From the count part of the hurdle Poisson regression model variables like age, family history of hypertension and elevated blood pressure had a significant effect on the expected number of non-zero frequencies of blood pressure examination. The expected number of non-zero frequencies of blood pressure examination of participants with age greater than or equal to 40 years was 6.11 times more examined than participants with age less than 40 years (Incidence Rate Ratios [IRR]: 6.11, p < 0.001). The expected numbers of non-zero frequencies of blood pressure examination of civil servants not having a family history of hypertension were 0.59 times less examined than civil servants having a family history of hypertension. The expected number of non-zero frequencies of blood pressure examination of civil servants with elevated blood pressure was 1.48 times more examined than civil servants with low blood pressure (Table 4).
 |
Table 4 Parameter Estimates of Hurdle Poisson Regression Model |
The odds of no blood pressure examination were 2.39 times higher among civil servants who had a first degree and above compared to those who had a diploma and less (OR: 2.39, p < 0.001). The odds of no blood pressure examination were 78.26 times higher among civil servants who had poor knowledge compared to their counterparts. Civil servants who did not receive advice from health professionals were 8.93 times more likely not examined than civil servants who receive advice (OR: 8.93, p < 0.001) and civil servants without a family history of hypertension were 62% less likely not to be blood pressure examined than civil servants with a family history of hypertension (Table 4).
Discussion
Blood pressure examination is an excellent mechanism for detecting and treating hypertension and controlling related diseases such as coronary artery disease, acute myocardial infarction, peripheral vascular disease, stroke, congestive heart failure, and renal failure, and premature death. The purpose of this study was to document the frequency and associated factors of blood pressure examination in civil servants. However, this study had certain limitations, including recall bias, lack of data on blood pressure self-measurement, and self-measurement challenges.
A previous study conducted in Ethiopia found a high level of hypertension among civil servants and recommend instructional-based blood pressure examination.29 But the frequency of blood pressure examination still has not improved. In this study, 70.2% of civil servants were never examined their blood pressure within a year before study time and the average number of blood pressure examinations was 0.71 with a variance of 1.458. It is a known fact that as age becomes older the elasticity of the blood vessels was reduced which increases the risk of hypertension. Also, evidence indicated that the incidence of hypertension was higher among older individuals.29 This evidence may encourage the older population to examine their blood pressure frequently. Our finding supports this idea that the frequency of blood pressure examination among participants with age greater than or equal to 40 years were 6.11 times more than participants with age less than 40 years. This may be due to participants’ fear of elevated blood pressure due to the significant association between age and hypertension, with the risk of hypertension increasing with age.29,30
In this study, a family history of hypertension has significant effects on the blood pressure examination. This may be because a family history of hypertension is one of the cause for elevated blood pressure,31,32 and those individuals who observe one of their family members suffering from hypertension had a better intention to check the blood pressure level. According to this study, elevated blood pressure was identified as another factor that affects the expected frequency of blood pressure examination. This is because civil servants with elevated blood pressure may want to control their blood pressure. One of the findings of this study showed that knowledge of hypertension had a significant effect on blood pressure examination. The probability of not making blood pressure examinations was high for those civil servants who did not have a good knowledge of hypertension. This may be because knowledge of hypertension has an association with self-care practice.33 Getting advice from a health professional was found significant association with blood pressure examination. The probability of not making blood pressure examinations was high for those civil servants who did not get advice from health professionals. This shows getting advice about blood pressure examination from health professionals is important.
Our results show that a significant proportion of civil servants are unaware of their blood pressure status despite being exposed to sedentary work habit. It also provides evidence that health professionals need to pay special attention to civil servants in order to achieve Sustainable Development Goals for non-communicable diseases by 2030.
Conclusion
Less than 3 out of 10 civil servants examined their blood pressure. Variables such as age, education, knowledge, advice from a medical professional, family history of hypertension, and elevated blood pressure had a significant impact on blood pressure testing. Relevant public health authorities and medical professionals should therefore consider these factors in their efforts to prevent and detect hypertension in civil servants.
Abbreviations
AIC, Akaike Information Criterion; BIC, Bayesian Information Criterion; PHE, Periodic health examination; SSA, sub-Saharan Africa; NB, Negative Binomial; ZIP, Zero Inflated Poisson; ZINB, Zero Inflated Negative Binomials; HP, Hurdle Poisson; HNB, Hurdle Negative Binomial; IRR, Incidence Rate Ratios.
Acknowledgments
We sincerely thank Arba Minch University for funding this research. The authors would also like to thank all the participants who participated in the study.
Disclosure
The authors declare no conflicts of interest in this work.
References
1. World Health Organization. A Global Brief on Hypertension: Silent Killer, Global Public Health Crisis: World Health Day 2013. World Health Organization; 2013.
2. Virgini VS, Meindl-Fridez C, Battegay E, Zimmerli L. Check-up examination: recommendations in adults. Swiss Med Wkly. 2015;145:w14075. doi:10.4414/smw.2015.14075
3. Lim SS, Vos T, Flaxman AD, et al. A comparative risk assessment of burden of disease and injury attributable to 67 risk factors and risk factor clusters in 21 regions, 1990–2010: a systematic analysis for the global burden of disease study 2010. Lancet. 2012;380(9859):2224–2260. doi:10.1016/S0140-6736(12)61766-8
4. Zhou B, Carrillo-Larco RM, Danaei G, et al. Worldwide trends in hypertension prevalence and progress in treatment and control from 1990 to 2019: a pooled analysis of 1201 population-representative studies with 104 million participants. Lancet. 2021;398(10304):957–980.
5. Mills KT, Stefanescu A, He J. The global epidemiology of hypertension. Nat Rev Nephrol. 2020;16(4):223–237.
6. Egan BM, Zhao Y, Axon RN, Brzezinski WA, Ferdinand KC. Uncontrolled and apparent treatment resistant hypertension in the United States, 1988 to 2008. Circulation. 2011;124(9):1046–1058.
7. van de Vijver S, Akinyi H, Oti S, et al. Status report on hypertension in Africa-consultative review for the 6th session of the African union conference of ministers of health on NCD’s. Pan Afr Med J. 2014;16(1):1.
8. Getahun W, Gedif T, Tesfaye F. Regular Khat (Catha edulis) chewing is associated with elevated diastolic blood pressure among adults in Butajira, Ethiopia: a comparative study. BMC Public Health. 2010;10:1–8.
9. Kibret KT, Mesfin YM. Prevalence of hypertension in Ethiopia: a systematic meta-analysis. Public Health Rev. 2015;36(1):1–12.
10. Legese N, Tadiwos Y. Epidemiology of hypertension in Ethiopia: a systematic review. Integr Blood Press Control. 2020;135–143. doi:10.2147/IBPC.S276089
11. Haligamo D, Ayalew A, Genemo H, Yiriga N Undiagnosed hypertension and its associated factors among adult people living in Southern Ethiopia: discovery from Gunchire Woreda of Gurage Zone; 2021.
12. Mogas SB, Tesfaye T, Zewde B, et al. Burden of undiagnosed hypertension among adults in urban communities of Southwest Ethiopia [Corrigendum]. Integr Blood Press Control. 2021;14:87–88. doi:10.2147/IBPC.S323336
13. Wachamo D, Geleta D, Woldesemayat EM. Undiagnosed hypertension and associated factors among adults in Hawela Tula sub-city, Hawassa, Southern Ethiopia: a community-based cross-sectional study. Risk Manag Healthc Policy. 2020;13:2169–2177. doi:10.2147/RMHP.S276955
14. Essa E, Shitie D, Yirsaw MT, Wale MZ. Undiagnosed hypertension and associated factors among adults in Debre Markos town, North-West Ethiopia: a community-based cross-sectional study. SAGE Open Med. 2022;10:20503121221094223. doi:10.1177/20503121221094223
15. Ayalew TL, Wale BG, Zewudie BT. Burden of undiagnosed hypertension and associated factors among adult populations in Wolaita Sodo Town, Wolaita Zone, Southern Ethiopia. BMC Cardiovasc Disord. 2022;22(1):293. doi:10.1186/s12872-022-02733-3
16. Dereje N, Earsido A, Temam L, Abebe A. Uncovering the high burden of hypertension and its predictors among adult population in Hosanna town, southern Ethiopia: a community-based cross-sectional study. BMJ open. 2020;10(10):e035823. doi:10.1136/bmjopen-2019-035823
17. Janus J, Kołton D, Kępowicz N, Kobos M, Jurkiewicz B. Periodic health examinations during a pandemic. Health Promot Phys Act. 2021;16(3):26–31. doi:10.5604/01.3001.0015.3311
18. Chen J-X, Zhou Y-F, Geng T, et al. Low concordance between blood pressures measured in periodic health examinations and in a workplace-based hypertension management program. Phenomics. 2022;2022;1–11.
19. Stergiou GS, Palatini P, Parati G, et al. 2021 European Society of Hypertension practice guidelines for office and out-of-office blood pressure measurement. J Hypertens. 2021;39(7):1293–1302. doi:10.1097/HJH.0000000000002843
20. Huang Q-F, Yang W-Y, Asayama K, et al. Ambulatory blood pressure monitoring to diagnose and manage hypertension. Hypertension. 2021;77(2):254–264. doi:10.1161/HYPERTENSIONAHA.120.14591
21. Pena-Hernandez C, Nugent K, Tuncel M. Twenty-four-hour ambulatory blood pressure monitoring. J Prim Care Community Health. 2020;11:2150132720940519. doi:10.1177/2150132720940519
22. Jin J. Screening for hypertension in adults. JAMA. 2021;325(16):1688. doi:10.1001/jama.2021.5288
23. Han HR, Chan K, Song H, Nguyen T, Lee JE, Kim MT. Development and evaluation of a hypertension knowledge test for Korean hypertensive patients. J Clin Hypertens. 2011;13(10):750–757. doi:10.1111/j.1751-7176.2011.00497.x
24. Cochran WG. Sampling Techniques. John Wiley & Sons; 1977.
25. Mullahy J. Specification and testing of some modified count data models. J Econom. 1986;33(3):341–365. doi:10.1016/0304-4076(86)90002-3
26. Cameron AC, Trivedi PK. Regression Analysis of Count Data. Cambridge university press; 2013.
27. Akaike H. Information theory and an extension of the maximum likelihood principle. In: Selected Papers of Hirotugu akaike. Springer; 1998:199–213.
28. McQuarrie A, Tsai C. Regression and Time Series Model Selection. New Jersey: World Scientific; 1998.
29. Angaw K, Dadi AF, Alene KA. Prevalence of hypertension among federal ministry civil servants in Addis Ababa, Ethiopia: a call for a workplace-screening program. BMC Cardiovasc Disord. 2015;15(1):1–6. doi:10.1186/s12872-015-0062-9
30. Abebe SM, Berhane Y, Worku A, Getachew A, Li Y. Prevalence and associated factors of hypertension: a crossectional community based study in Northwest Ethiopia. PLoS One. 2015;10(4):e0125210. doi:10.1371/journal.pone.0125210
31. Awoke A, Awoke T, Alemu S, Megabiaw B. Prevalence and associated factors of hypertension among adults in Gondar, Northwest Ethiopia: a community based cross-sectional study. BMC Cardiovasc Disord. 2012;12(1):1–6. doi:10.1186/1471-2261-12-113
32. Helelo TP, Gelaw YA, Adane AA, Fuchs FD. Prevalence and associated factors of hypertension among adults in Durame Town, Southern Ethiopia. PLoS One. 2014;9(11):e112790. doi:10.1371/journal.pone.0112790
33. Worku Kassahun C, Asasahegn A, Hagos D, et al. Knowledge on hypertension and self-care practice among adult hypertensive patients at university of Gondar comprehensive specialized hospital, Ethiopia, 2019. Int J Hypertens. 2020;2020:1.
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.