Back to Journals » Infection and Drug Resistance » Volume 17
Birth Outcomes of Pregnant Women Infected with COVID-19 in Highland Areas of China from 2020 to 2022: A Retrospective Analysis
Authors Lv A, Ma BBZ, Qiong D, Ma DWZ, Ma PBZ, Yao D, Zhen D, Tang C, Ma BBZ, Lu Y, Cai L, Zhang Y, Yin J, Ding T, Zhen LJQ, Cang DW, Wu M, Chen Y, Li Y
Received 16 August 2023
Accepted for publication 4 March 2024
Published 8 March 2024 Volume 2024:17 Pages 927—934
DOI https://doi.org/10.2147/IDR.S435751
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Professor Suresh Antony
Aiming Lv,1,2 Bian Ba Zhuo Ma,3 De Qiong,2 Da Wa Zhuo Ma,2 Pu Bu Zhuo Ma,3 Donghua Yao,4 Da Zhen,2 Chunxiu Tang,2 Bian Ba Zhuo Ma,2 Youzhi Lu,2 Long Cai,2 Yutong Zhang,2 Jinyu Yin,2 Tong Ding,2 Lang Ji Qu Zhen,2 Da Wa Cang,5 Meng Wu,5 Yulan Chen,5 Ye Li1
1Department of Obstetrics and Gynecology, Beijing Hospital, National Center of Gerontology, Institute of Geriatric Medicine, Chinese Academy of Medical Sciences, Beijing, People’s Republic of China; 2Department of Obstetrics and Gynecology, Women and Children’s Hospital of Tibet Autonomous Region, Lhasa City, TB, People’s Republic of China; 3Department of Obstetrics and Gynecology, Lhasa People’s Hospital, Lhasa, TB, 850000, People’s Republic of China; 4Department of Obstetrics and Gynecology, Nyingchi People’s Hospital, Nyingchi City, TB, People’s Republic of China; 5Department of Obstetrics and Gynecology, Tibet University Medical School, Lhasa City, TB, People’s Republic of China
Correspondence: Ye Li, Department of Obstetrics and Gynecology, Beijing Hospital, National center of Gerontology, Institute of Geriatric Medicine, Chinese Academy of Medical Sciences, China, No. 1 DaHua Road, Dong Dan, Beijing, 100730, People’s Republic of China, Tel +86 13611118475, Fax +86 10 85136220, Email [email protected]
Purpose: To explore the effect of coronavirus disease 2019 (COVID-19) infection on neonates in plateau regions.
Methods: Cases of newborns born to pregnant women infected with COVID-19 who received prenatal care or treatment at the Women and Children’s Hospital of the Tibet Autonomous Region and the Lhasa People’s Hospital between January 2020 and December 2022 (infected group) and newborns born to healthy pregnant women (non-infected group) who were included by age, underlying disease and length of hospital stay were retrospectively collected. According to the inclusion and exclusion criteria, 381 patients in the infected group and 314 patients in the non-infected group were included in the study.
Results: The results of multivariate analysis showed that admission to the neonatal intensive care unit (OR = 3.342, 95% CI = 1.564– 6.764), shortness of breath (OR = 2.853, 95% CI = 1.789– 3.154), irregular breathing (OR = 2.465, 95% CI = 1.879– 4.112) and neonatal jaundice (OR = 2.324, 95% CI = 1.989– 2.445) were the factors influencing the low Apgar scores of neonates in the infected group (all P < 0.05).
Conclusion: Neonates born to pregnant women infected with COVID-19 had lower Apgar scores and higher incidences of complications, such as shortness of breath, groaning, irregular breathing and neonatal jaundice, than newborns born to pregnant women not infected with COVID-19.
Keywords: COVID-19, pregnant women, newborn
Introduction
The pathogen of coronavirus disease 2019 (COVID-19) is severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), belonging to the group of betacoronaviruses that includes other members, such as the severe acute respiratory syndrome coronavirus (SARS-CoV) and the Middle East respiratory syndrome coronavirus (MERS-CoV) that became widespread across the globe with high morbidity and mortality.1–3 The SARS-CoV-2 invades cells by binding the spike protein (S protein) with the angiotensin-converting enzyme 2 (ACE2).4 The SARS-CoV-2 and the SARS-CoV have a similar affinity to the ACE2, but the former has a high incidence of infection due to its mutability.5–7
The physiological changes in immune, respiratory and circulatory systems during pregnancy make pregnant women susceptible to pathogens and intolerant to hypoxia.8–10 Pregnant women have a higher risk of viral infections, complications and adverse clinical and pregnancy outcomes compared with the general population.11 Controversy exists about whether a novel coronavirus infection impacts neonatal outcomes.12–16 Some studies have found no significant increase in the incidence of adverse neonatal outcomes in pregnant women who tested positive for COVID-19 compared with pregnant women who tested negative.17,18 Conversely, some studies have shown an increased risk of adverse neonatal outcomes in pregnant women who tested positive for COVID-19.19,20 The COVID-19 vaccination effectively reduces the incidence of critical and fatal cases. However, neonates cannot be vaccinated against COVID-19, have low immunity21 and, as a consequence, are vulnerable to epidemics. Infected newborns may die,22 and COVID-19 may also cause systemic diseases accompanied by multiple internal organ involvement.23 Therefore, our understanding of COVID-19 should be deepened, and scientific countermeasures should be implemented to protect neonates.
Pregnant women are a high-risk group for COVID-19. Currently, studies on the effect of SARS-CoV-2 on neonatal outcomes are conflicting, and studies of COVID-19 in pregnancy are mostly limited to a single site with a small sample size and no appropriate control group.24 Most studies have been carried out in urban areas, such as Wuhan and Shanghai, and studies focusing on newborns at high altitudes are scarce. The population in plateau regions lives in a chronic hypoxic environment, and previous studies show that a low-pressure and hypoxic environment affects foetal and neonatal health.25 The oxygen concentration in the air has a significant effect on neonates infected with COVID-19, which may cause neonatal asphyxia, and critical patients with COVID-19 may rapidly progress to acute respiratory distress syndrome, septic shock, organ failure and even death.26
Therefore, by focusing on neonates born to pregnant women infected with COVID-19, this study aims to deepen the understanding of the effect of pregnancy combined with COVID-19 on neonates and provide scientific evidence for early warning, prevention and treatment. The study is of great applicative significance for formulating disease prevention and control strategies and long-term birth plans for patients in the post-COVID era.
Research Participants and Methods
Research Participants
Cases of newborns born to pregnant women infected with COVID-19 who received prenatal care or treatment in the hospital between January 2020 and December 2022 were retrospectively collected (infected group) as well as newborns born to healthy pregnant women (non-infected group) included by age, underlying disease, and length of hospital stay. The above cases were from women and children in Tibet Autonomous Region Hospital and Lhasa People’s Hospital. All eligible participants were included in chronological order according to the inclusion and exclusion criteria. All participants included in the infected group met the diagnostic criteria for laboratory and clinically confirmed cases of COVID-19 according to the Guidelines on the diagnosis and treatment of novel coronavirus pneumonia (trial version 5).27 Inclusion criteria: pregnant women with or without COVID-19 aged 20–45 years. Exclusion criteria: patients with chromosomal abnormalities or congenital malformations of their reproductive organs. This study was conducted in accordance with the Declaration of Helsinki and approved by the Ethics Committee of the Women and Children’s Hospital of the Tibet Autonomous Region (qfeyy-2023001). Written informed consent was obtained from all parents and local guardians.
Birth malformations are defined as morphological or functional abnormalities in one or more parts of the body that appear during fetal development or after birth and are present at birth. For example, an organ or tissue is abnormal in shape, size or location, or something is present that impacts the normal functioning of the organ or system. Birth anomalies vary from mild (no significant impact on life) to severe (requiring immediate medical intervention or long-term treatment). These malformations can affect various aspects of the body, including the heart, brain, limbs and face.28
The diagnostic criteria for a pneumonia diagnosis and the treatment protocol for novel coronavirus infection (trial version 5) were: (1) a real-time fluorescent reverse transcription polymerase chain reaction detection of novel coronavirus nucleic acid positivity in respiratory specimens or blood specimens or (2) viral gene sequencing in respiratory specimens or blood specimens, highly homologous to known novel coronavirus. Those with one of the above etiological pieces of evidence were included as confirmed cases.
Data Collection
The pregnancy outcome data, including basic neonatal information, the Apgar score at 1, 5 and 10 min, the neonatal intensive care unit (NICU) admission rate, neonatal mortality and neonatal complications, were collected from the two groups of pregnant women by consulting the electronic medical record information system or prenatal examination records. Specially trained attending physicians, obstetricians and gynaecologists with professional titles collected the above data, and all collected data were entered and verified by two individuals to ensure the validity of the data.
The basic information included sex, birth weight and length.
Apgar scoring was used to evaluate neonatal asphyxia.29 After birth, newborns were scored according to five signs: skin colour, heart rate, respiration, muscle tone and movement and reflexes. Pale skin colour was scored 0, cyanotic skin 1 and ruddy skin 2. A score of 2 was given for a heart rate of more than 100 beats per min, 1 for less than 100 beats per min and 0 for no heart rate. Regarding respiration, irregular breathing or an “unloud” cry was scored 1, regular breathing and a loud cry 2 and no breathing 0. Good muscle tone was scored 2, decreased muscle tone 1 and floppy or no muscle tone 0. After the baby ‘s soles of the feet or nasal cannula were rubbed by hand, the baby developed crying, sneezing or coughing with a score of 2, and only slight reactions such as frowning with a score of 1 and no reactions with a score of 0. A total score of 8–10 was normal; 4–7 indicated mild asphyxia, also clinically known as asphyxia, requiring measures such as airway clearance, artificial respiration, oxygen inhalation and drug therapy; and 0–3 indicated severe asphyxia, also known as pale asphyxia, pointing to severe hypoxia requiring emergency treatment, such as laryngoscopic endotracheal intubation and oxygen inhalation under direct vision.
Neonatal complications included birth deformity, shortness of breath, moaning, irregular breathing and neonatal jaundice.
Evaluation Indicators
Primary outcome measures: the Apgar score at 1, 5 and 10 min.
Secondary outcome measures: the NICU admission rate, neonatal mortality and neonatal complications.
Statistical Analysis
Excel 2019 was applied for data compilation, and SPSS 26.00 for statistical analysis. Normally distributed or approximately normally distributed data were presented as , comparisons between the groups were performed with t–tests, and repeated-measures data were analysed using repeated-measures analysis of variance (separate effects were required if there was an interaction between time and group, indicating that neonatal outcomes had changed automatically over time in both groups, and the main effects were analysed if there was no interaction). The enumeration data were described by the number of cases and rate, and comparisons between the groups were performed using the x2 test. Multivariate analysis was performed using binary logistic regression. Significant suspected risk factors identified in the univariate analysis were coded by whether the Apgar score was >8 min at 1 min after birth as the dependent variable (yes = 1, no = 0), and logistic regression analysis was performed. Table 1 presents the grouping and coding information, and raw values were entered for the quantitative data. A backward approach using partial maximum likelihood estimation techniques (the inclusion criterion was P ≤ 0.05, and the exclusion criterion was P ≥ 0.10) was applied to include or exclude these factors, and logistic regression analysis models were then constructed. The inspection level was α = 0.05, and all tests were two-sided.
, comparisons between the groups were performed with t–tests, and repeated-measures data were analysed using repeated-measures analysis of variance (separate effects were required if there was an interaction between time and group, indicating that neonatal outcomes had changed automatically over time in both groups, and the main effects were analysed if there was no interaction). The enumeration data were described by the number of cases and rate, and comparisons between the groups were performed using the x2 test. Multivariate analysis was performed using binary logistic regression. Significant suspected risk factors identified in the univariate analysis were coded by whether the Apgar score was >8 min at 1 min after birth as the dependent variable (yes = 1, no = 0), and logistic regression analysis was performed. Table 1 presents the grouping and coding information, and raw values were entered for the quantitative data. A backward approach using partial maximum likelihood estimation techniques (the inclusion criterion was P ≤ 0.05, and the exclusion criterion was P ≥ 0.10) was applied to include or exclude these factors, and logistic regression analysis models were then constructed. The inspection level was α = 0.05, and all tests were two-sided.
 |
Table 1 Variable Grouping and Encoding |
Results
Comparison of the Clinical Data of the Neonates from the Two Groups
A total of 178 women and 203 men were included in the infected group compared with 163 women and 151 men in the non-infected group. In the infected group, birth weight was 3,201 ± 532 g and body length was 48.61 ± 2.31 cm; in the non-infected group, birth weight was 3,195 ± 622 g and body length was 49.36 ± 1.47 cm.
The two groups of neonates showed no statistically significant differences in sex, birth weight, body length, rates of NICU admission, neonatal mortality and birth deformity (P > 0.05). The differences in the neonatal Apgar scores (Ftreatment = 231.351, P < 0.05), rates of shortness of breath (χ2 = 10.181, P < 0.05), moaning (χ2 = 6.132, P < 0.05), irregular breathing (χ2 = 8.346, P < 0.05) and neonatal jaundice (χ2 = 5.521, P < 0.05) between the two groups were statistically significant, as shown in Table 2.
 |
Table 2 Comparison of Clinical Data of Neonates from the Two Groups |
The interaction between the time*treatment of the neonatal Apgar scores of the two groups was not statistically significant (Finteraction = 11.231, P > 0.05), and, hence, the main effect was directly analysed. The neonatal Apgar scores of the two groups increased over time (Ftime = 112.471, P < 0.05). Furthermore, the impact of whether a pregnant woman was infected with COVID-19 on the neonatal Apgar score varied (Ftreatment = 231.351, P < 0.05). A further comparison of the magnitudes of the Apgar scores of the two groups of neonates at 1, 5 and 10 min showed that the non-infected group had a larger Apgar score at 1 min (t = 3.478, P < 0.05), 5 min (t = 4.553, P < 0.05) and 10 min (t = 4.536, P < 0.05).
Multivariate Analysis of Factors Influencing Neonatal Apgar Scores of the Two Groups
To further explore the factors influencing the Apgar scores, meaningful suspected risk factors were identified using binary logistic regression. The results showed that admission to NICU (OR = 3.342, 95% CI = 1.564–6.764, P < 0.05), shortness of breath (OR = 2.853, 95% CI = 1.789–3.154, P < 0.05), irregular breathing (OR = 2.465, 95% CI = 1.879–4.112, P < 0.05) and neonatal jaundice (OR = 2.324, 95% CI = 1.989–2.445, P < 0.05) were the factors influencing the low Apgar score in the infected group, as shown in Table 3.
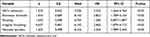 |
Table 3 Multivariate Analysis of Factors Influencing Neonatal Apgar Scores of the Two Groups |
Discussion
The results showed that the Apgar scores of newborns in the group of pregnant women infected with COVID-19 were lower than that of newborns in the non-infected group, and the incidence of complications, such as shortness of breath, groaning, irregular breathing and neonatal jaundice, was higher. Admission to the NICU, shortness of breath, irregular breathing and neonatal jaundice were the factors influencing the low Apgar scores of the neonates in the infected group. In this study, we investigated newborns living at high altitudes and proposed new findings to help improve the prognosis of newborns born to pregnant women infected with COVID-19. However, this study only looked at the short-term adverse effects of COVID-19 on pregnant women and newborns, and long-term follow-up and monitoring are necessary to further explore the long-term effects of SARS-CoV-2 on pregnant women and their offspring.
In this study, the group of pregnant women infected with COVID-19 had lower neonatal scores than the non-infected group, consistent with previous studies.30 However, no differences in the lengths and weights of neonates were found. A study on perinatal and neonatal outcomes in pregnant women30 showed that pregnant women with viral pneumonia were more likely to deliver newborns small for their gestational ages with low birth weights, foetal growth restrictions, preterm deliveries and low neonatal Apgar scores. This may be because women’s unique hormonal and physiological alterations during pregnancy render their bodies more susceptible to respiratory pathogens and severe pneumonia.8,31 Possible mechanisms of action include changes in the maternal immune system during pregnancy (eg changes in Cd4 + T cells from a Th1 phenotype to a Th2 phenotype, decreases in circulating natural killer cells, increases in circulating progesterone levels and changes in the innate immune system),32 physiological changes in the respiratory system (uterine changes during pregnancy lead to diaphragmatic elevations and respiratory changes that increase susceptibility to respiratory infections)33 and changes in coagulation (a hypercoagulable state during pregnancy).34 Compared with previous studies of pregnant women infected with SARS, MERS and influenza A virus subtype, H1N1,13 pregnant women infected with COVID-19 had a higher incidence of neonatal outcomes. Therefore, the pathogenic mechanisms responsible for the adverse neonatal outcomes caused by SARS-CoV-2 in pregnant women and newborns should be investigated further to identify targeted prevention and treatment strategies.
In this study, most neonates had evident jaundice symptoms. Studies35,36 show that COVID-19 affects the liver and gastrointestinal system, possibly causing neonatal isoerythrolysis and excessive bilirubin generation, which requires further research. The physiological basis of children’s low susceptibility also plays a role. The main target sites37 of SARS-CoV-2 when infecting humans are ACE2 receptors. Most neonatal cases had mild symptoms, which may be attributed to their low function or expression of ACE2 receptors that limit the virus entry pathways.38
In this study, newborns born to pregnant women in the group infected with COVID-19 had a higher incidence of shortness of breath, groaning and irregular breathing. Multivariate analysis also showed that admission to the NICU, shortness of breath and irregular breathing were risk factors for low Apgar scores. Li Zewu et al39 reported that the mortality rate of pregnant women and their foetuses infected with the novel coronavirus was low but that the adverse pregnancy outcome or pregnancy complication rate was significantly increased, including premature delivery, low birth weight, premature rupture of membranes and foetal distress. This suggests that we should give timely individualised intervention to pregnant women infected with SARS-CoV-2 according to the severity of the disease and pregnancy progression, with more attention paid to pregnant women infected with SARS-CoV-2 in the first and second trimesters to prevent the occurrence of adverse outcomes.
This study has some limitations. First, this is a retrospective study with patients from multiple research centres, with the differences in electronic record systems resulting in a loss of clinical data for some of the patients. Second, patients’ willingness to undergo prenatal examinations was low during the pandemic, and some of the patients were lost to follow-up, which resulted in a failure to obtain continuous data. Third, some neonates born in the early stage of the epidemic did not receive SARS-CoV-2 nucleic acid and antibody tests. Fourth, the number of patients in early and mid-term pregnancy was small, and a larger number of samples are needed to explore the effect of SARS-CoV-2 on pregnant women in these stages. Fifth, this study failed to collect and test the breast milk, vaginal fluid and intrauterine tissue samples of some of the patients, making it difficult to confirm the presence of mother-to-child transmission. Sixth, most patients with mild symptoms were treated at mobile cabin hospitals or other public facilities, whereas pregnant women infected with COVID-19 were hospitalised in designated institutions, which may have caused selection bias in the incorporation of the group of pregnant women infected with COVID-19.
Conclusion
Neonates born to pregnant women infected with COVID-19 had lower Apgar scores and a higher incidence of complications, such as shortness of breath, groaning, irregular breathing and neonatal jaundice than newborns born to pregnant women in the non-infected group. Clinically, attention should be given to the physical condition of newborns born to women infected with COVID-19, and monitoring should be strengthened, with particular attention paid to the respiratory status of newborns, timely optimisation of treatment options and improvement in prognosis.
Data Sharing Statement
All data generated or analyzed during this study are included in this published article.
Ethics Approval and Consent to Participate
This study was conducted in accordance with the Declaration of Helsinki and approved by the Ethics Committee of Women and Children’s Hospital of Tibet Autonomous Region (qfeyy-202300). Written informed consent was obtained from all parents/local guardians.
Funding
Tibet Autonomous Region Key R&D Project (XZ202201ZY0044G).
Disclosure
None of the authors have any personal, financial, commercial, or academic conflicts of interest to report for this work.
References
1. Wong SF, Chow KM, Leung TN, et al. Pregnancy and perinatal outcomes of women with severe acute respiratory syndrome. Am J Obstet Gynecol. 2004;191(1):292–297. doi:10.1016/j.ajog.2003.11.019
2. Alfaraj SH, Al-Tawfiq JA, Memish ZA. Middle east respiratory syndrome coronavirus (MERS-CoV) infection during pregnancy: report of two cases & review of the literature. J Microbiol Immunol Infect. 2019;52(3):501–503. doi:10.1016/j.jmii.2018.04.005
3. Lu R, Zhao X, Li J, et al. Genomic characterisation and epidemiology of 2019 novel coronavirus: implications for virus origins and receptor binding. Lancet. 2020;395(10224):565–574. doi:10.1016/S0140-6736(20)30251-8
4. Zhou P, Yang XL, Wang XG, et al. A pneumonia outbreak associated with a new coronavirus of probable bat origin. Nature. 2020;579(7798):270–273. doi:10.1038/s41586-020-2012-7
5. Huang C, Wang Y, Li X, et al. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet. 2020;395(10223):497–506. doi:10.1016/S0140-6736(20)30183-5
6. Walls AC, Park YJ, Tortorici MA, et al. Structure, function, and antigenicity of the SARS-CoV-2 Spike Glycoprotein. Cell. 2020;181(2):281–292.e6. doi:10.1016/j.cell.2020.02.058
7. Wu A, Peng Y, Huang B, et al. Genome composition and divergence of the novel coronavirus originating in China. Cell Host Microbe. 2020;27(3):325–328. doi:10.1016/j.chom.2020.02.001
8. Vojtek I, Dieussaert I, Doherty TM, et al. Maternal immunization: where are we now and how to move forward? Ann Med. 2018;50(3):193–208. doi:10.1080/07853890.2017.1421320
9. Chaouat G, Petitbarat M, Dubanchet S, et al. Tolerance to the foetal allograft? Am J Reprod Immunol. 2010;63(6):624–636. doi:10.1111/j.1600-0897.2010.00832.x
10. Cunningham FG, Leveno KJ, Bloom SL, et al. Williams obstetrics, 25th. McGraw Hill Professional; 2018.
11. Siston AM. Pandemic 2009 influenza A(H1N1) virus illness among pregnant women in the United States. JAMA. 2010;303(15):1517–1525. doi:10.1001/jama.2010.479
12. Adhikari EH, Moreno W, Zofkie AC, et al. Pregnancy outcomes among women with and without severe acute respiratory syndrome coronavirus 2 infection. JAMA Network Open. 2020;3(11):e2029256. doi:10.1001/jamanetworkopen.2020.29256
13. Huntley BJF, Huntley ES, Di Mascio D, et al. Rates of maternal and perinatal mortality and vertical transmission in pregnancies complicated by severe acute respiratory syndrome coronavirus 2 (SARS-Co-V-2) infection: a systematic review. Obstet Gynecol. 2020;136(2):303–312. doi:10.1097/AOG.0000000000004010
14. Jering KS, Claggett BL, Cunningham JW, et al. Clinical characteristics and outcomes of hospitalized women giving birth with and without COVID-19. JAMA Intern Med. 2021;181(5):714–717. doi:10.1001/jamainternmed.2020.9241
15. The American College of Obstetricians and Gynecologists. Vaccinating pregnant and lactating patients against COVID-19; 2020.
16. Centers for Disease Control and Prevention COVID-19. People with certain medical conditions. 2021.
17. Yang H, Sun G, Tang F, et al. Clinical features and outcomes of pregnant women suspected of coronavirus disease 2019. J Infect. 2020;81(1):e40–e44. doi:10.1016/j.jinf.2020.04.003
18. Chen H, Guo J, Wang C, et al. Clinical characteristics and intrauterine vertical transmission potential of COVID-19 infection in nine pregnant women: a retrospective review of medical records. Lancet. 2020;395(10226):809–815. doi:10.1016/S0140-6736(20)30360-3
19. Schwartz DA. An analysis of 38 pregnant women with covid-19, their newborn infants, and maternal-fetal transmission of SARS-CoV-2: maternal coronavirus infections and pregnancy outcomes. Arch Pathol Lab Med. 2020;144(7):799–805. doi:10.5858/arpa.2020-0901-SA
20. Flaherman VJ, Afshar Y, Boscardin WJ, et al. Infant outcomes following maternal infection with severe acute respiratory syndrome coronavirus 2 (sars-cov-2): first report from the pregnancy coronavirus outcomes registry (PRIORITY) study. Clin Infect Dis. 2021;73(9):e2810–e2813. doi:10.1093/cid/ciaa1411
21. Mehraeen E, Dadras O, Afsahi AM, et al. Vaccines for COVID-19: a systematic review of feasibility and effectiveness. Infect Disord Drug Targets. 2022;22(2):e230921196758. doi:10.2174/1871526521666210923144837
22. Zhang K, Jiang SY, Yan K, et al. Clinical characteristics of 16 neonates infected with SARS-CoV-2 during omicron variant outbreak. Zhonghua Er Ke Za Zhi. 2022;60(11):1158–1162. doi:10.3760/cma.j.cn112140-20220617-00561 Chinese.
23. Mehraeen E, Oliaei S, SeyedAlinaghi S, et al. COVID-19 in pediatrics: a systematic review of current knowledge and practice. Infect Disord Drug Targets. 2022;22(5):e290921196908. doi:10.2174/1871526521666210929121705
24. Khoury R, Bernstein PS, Debolt C, et al. Characteristics and outcomes of 241 births to women with severe acute respiratory syndrome coronavirus 2 (SARS-COV-2) infection at five new york city medical centers. Obstet Gynecol. 2020;136(2):273–282. doi:10.1097/AOG.0000000000004025
25. Julian CG. High altitude during pregnancy. Clin Chest Med. 2011;32(1):21–31. doi:10.1016/j.ccm.2010.10.008
26. Guo YR, Cao QD, Hong ZS, et al. The origin, transmission and clinical therapies on coronavirus disease 2019 (COVID-19) outbreak - an update on the status. Mil Med Res. 2020;7(1):11. doi:10.1186/s40779-020-00240-0
27. van Nieuwenhoven AL V. The immunology of successful pregnancy. Hum Reprod Update. 2003;9(4):347–357. doi:10.1093/humupd/dmg026
28. Park JS, Kim J, Ha Y, et al. Birth abnormalities in pregnant sows infected intranasally with porcine circovirus 2. J Comp Pathol. 2005;132(2–3):139–144. doi:10.1016/j.jcpa.2004.09.003
29. American academy of pediatrics committee on fetus and newborn; American college of obstetricians and gynecologists committee on obstetric practice. Apgar Score Pedi. 2015;136(4):819–822. doi:10.1542/peds.2015-2651
30. Chen YH, Keller J, Wang IT, et al. Pneumonia and pregnancy outcomes: a nationwide population-based study. Am J Obstet Gynecol. 2012;207(4):
31. Shirshev SV. Mechanisms of immune tolerance in physiological pregnancy. Usp Fiziol Nauk. 2010;41(1):75–93. Russian.
32. Zhou Y, Fu B, Zheng X, et al. Pathogenic T-cells and inflammatory monocytes incite inflammatory storms in severe COVID-19 patients. Natl Sci Rev. 2020;7(6):998–1002. doi:10.1093/nsr/nwaa041
33. Goodnight WH, Soper DE. Pneumonia in pregnancy. Crit Care Med. 2005;33(10 Suppl):S390–7. doi:10.1097/01.ccm.0000182483.24836.66
34. Di Renzo GC, Giardina I. Coronavirus disease 2019 in pregnancy: consider thromboembolic disorders and thromboprophylaxis. Am J Obstet Gynecol. 2020;223(1):135. doi:10.1016/j.ajog.2020.04.017
35. Zhang C, Shi L, Wang FS. Liver injury in COVID-19: management and challenges. Lancet Gastroenterol Hepatol. 2020;5(5):428–430. doi:10.1016/S2468-1253(20)30057-1
36. Xu L, Liu J, Lu M, et al. Liver injury during highly pathogenic human coronavirus infections. Liver Int. 2020;40(5):998–1004. doi:10.1111/liv.14435
37. Ciaglia E, Vecchione C, Puca AA. COVID-19 infection and circulating ACE2 Levels: protective role in women and children. Front Pediatr. 2020;8:206. doi:10.3389/fped.2020.00206
38. Liu J, Luo WJ, Deng ZH, et al. Clinical and epidemiological characteristics of 91 children confirmed with COVID-19. Chin J Nosocom. 2020;30(11):1625–1629.
39. Li ZW, Baike·Jiang Tuilu B, Ren MY, et al. Current research status of the relationship between novel coronavirus infection and adverse pregnancy outcomes in pregnant women. Chin J Reprod Heal. 2020;31(03):1.
 © 2024 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2024 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
