Back to Journals » Infection and Drug Resistance » Volume 15
Bioassay-Guided Phytochemical Analyses and Antimicrobial Potentials of the Leaf Extract of Clematis hirsuta Perr. and Guill. Against Some Pathogenic Bacteria and Fungi
Authors Ameya G, Manilal A, Sabu KR, Aragie S
Received 13 September 2022
Accepted for publication 5 November 2022
Published 10 November 2022 Volume 2022:15 Pages 6577—6588
DOI https://doi.org/10.2147/IDR.S389699
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Prof. Dr. Héctor Mora-Montes
Gemechu Ameya,1,2 Aseer Manilal,3 Kuzhunellil Raghavanpillai Sabu,4 Solomon Aragie2
1Department of Medical Laboratory Sciences, College of Medicine and Health Sciences, Kotebe Metropolitan University, Addis Ababa, Ethiopia; 2Department of Cellular, Microbial, and Molecular Biology, College of Natural and Computational Sciences, Addis Ababa University, Addis Ababa, Ethiopia; 3Department of Medical Laboratory Sciences, College of Medicine and Health Sciences, Arba Minch University, Arba Minch, Ethiopia; 4Department of Chemistry, College of Natural and Computational Sciences, Arba Minch University, Arba Minch, Ethiopia
Correspondence: Gemechu Ameya, Email [email protected]
Background: In spite of the great advances in modern medicine in recent decades, medicines of plant origin are still in use for several ailments in different parts of the world. There is always an urge to develop novel, effective and inexpensive antimicrobials. This study was aimed to evaluate the antimicrobial activity and phytochemical composition of the leaf extract of Clematis hirsuta against selected human bacterial and fungal pathogens.
Methods: The crude extracts of C. hirsuta leaves were prepared with five different solvents of varying polarity. Agar well diffusion assay on five different species of ATCC organisms, four clinical bacterial isolates, and four clinically isolated fungi were performed. The tube dilution method was used to determine the minimum inhibitory concentrations and the selected extract was subjected to bio-assay-guided fractionation using column chromatography and the active fraction obtained were pooled and GC-MS, FT-IR, and CHN analysis were conducted, and this study is actually bioassay-guided research.
Results: A varying patterns of antimicrobial activity against tested microorganism was observed. Acetone extract showed the highest spectrum of activity (17– 32mm) in the well diffusion assay against bacteria and 16– 23mm in the case of fungi. The MIC ranged from 7.5– 60 mg/mL in the case of bacteria and 15– 60 mg/mL against fungi. The bioassay-guided column chromatography of the acetone extract followed by GC-MS showed the presence of three major compounds, specifically O-ethylhydroxylamine (43%), 2-ethyl heptanoic acid (20.6%), and 1-nonyl cycloheptane (19.5%). The finding was confirmed by FT-IR and elemental analysis of TLC-separated fractions.
Conclusion: The acetone extract showed better antimicrobial activity and the least minimum inhibition concentrations against bacteria compared to fungi. The observed antibacterial can be assigned to the presence of alkoxy amine, alkyl aliphatic acids, and cycloalkane. The overall findings substantiate the traditional usages of the parts of this plant, especially the leaves, in managing infectious diseases.
Keywords: antimicrobial analysis, Clematis hirsuta, pathogenic organisms, phytochemical analysis
Introduction
Infectious diseases are causing significant morbidity and mortality worldwide, and epidemiological data show that six of the ten top causes of the overall disease burden among children correspond to infectious diseases.1 Drug-resistant microbe are becoming a severe problem in both the developing and developed countries; WHO lists antimicrobial resistance as one of the top ten global public health threats to humanity.2 The alarming incidence of antibiotic resistance exhibited by bacteria and fungi create a constant need for introducing new and effective therapeutic agents. However, most of the available antibiotics have some sort of adverse effects; some are immuno-suppressants, and many end up in allergic reactions.3 Despite the increasing drug resistance to common pathogens, the non-availability of modern medicines in developing countries, particularly in many African nations is challenging. Moreover, the cost factor is escalating, resulting in heavier hospital bills. There are several contributing factors, including the fast population growth.4
The demand for plant-derived isolable components which are medicinally is ever-increasing due to the adverse side effects associated with purely synthetic antibiotics and the high prevalence of drug-resistant microbial strains.5,6 In addition, the increase in the number of cases of opportunistic infections related to AIDS, and immunosuppressive chemotherapy, clubbed with the toxicity of many antibacterial and antifungal drugs, have imposed severe pressure on clinicians to look for alternative and novel therapeutic agents.7,8 Notwithstanding the global decline in the magnitude of contagious diseases, six of the top ten causes of mortality in low-income countries, even today, are associated with severe infections.1,4
Several types of mechanisms can be proposed to correlate the efficacy of phytochemicals in curing infections with their diverse molecular structures and functional identities. They may subjugate the growth of microorganisms by interfering with some of the microbial metabolic processes or may even modulate the gene expressions and signal transduction pathways.9–11 Secondary metabolites contained in plants may exhibit different modes of action against a number of fungi and bacterial strains and are probably linked to the alteration of the cytoplasmic membrane, disruption of proton motive force, electron flow, active transport, and even the coagulation of cell contents.12–14
In Ethiopia, several plant species continue to be the most affordable and easily accessible sources of medicines for treating different infectious diseases in humans and livestock. In most cases, medicines extracted from traditionally identified plants are utilised.15,16 However, many medicinal plants are not well studied or systematically evaluated in terms of their antimicrobial and phytochemical potentials. Ethno-botanical studies proved that there are about 6500 to 7000 promising medicinal plant species in Ethiopia, of which approximately 12% are endemic.17–20
Clematis hirsuta family of Ranunculaceae has a local name of “Yeazo Areg” in Amharic and “Hidafeti” in the Afan Oromo region of Ethiopia. It is a woody climber, several meters long; young stems are densely hairy, but usually they become glabrous later. The leaves are pinnate with five leaflets; rarely bi-pinnate; well-developed leaves are often associated with inflorescence. The leaflets are sub-orbicular to ovate, more or less acuminate to sub-obtuse at the apex, cordate to rounded at the base and are often found with a central lobe and shorter lateral lobes on each side.21,22
Earlier ethnobotanical studies revealed that different parts of this plant are used to treat swellings and wounds.23 Crushed leaves are applied on swellings as a bandage, and sometimes, the chopped stem is also used for this purpose, whereas the latex can be applied over wounds.23 Several species of the genus Clematis have been widely used in folk medicines in many countries. For instance, the decoction made from the fruits and leaves of C. vitalba is used for treating oral inflammation and rheumatic pain24,25 and the leaves of another species, C. drummondi are used as a disinfectant and antibiotic.26 There exists, however, a shortage of information on the antimicrobial activity of the title plant, particularly in Ethiopia. Therefore, this study is aimed to assess the phytochemical compositions and antimicrobial activity of C. hirsuta leaf extracts against a battery of pathogenic bacteria and fungi.
Methods
Study Design
An in-vitro bioassay-guided study was done to determine the phytochemical compositions and antimicrobial activity of C. hirsuta leaves extracted in six different solvents.
Collection and Extraction of C. hirsuta Leaves
Leaves of C. hirsuta were selected for this study based on the ethnobotanical details and information linked to its traditional utilisation in the cure of infectious diseases. Leaves of matured plants were collected from Nekemte in the western part of Ethiopia (latitude and longitude of 95’N and 36 33’E). The plant was taxonomically identified with the aid of an eminent plant taxonomist (Dr Garuma Gerbaba, Addis Ababa University, Ethiopia), and specimens were deposited in the Department of Medical Laboratory Sciences, College of Medicine and Health Sciences, Arba Minch University (Voucher No. GAP 015) for future reference. Before solvent extraction, leaves were washed to remove dust and other associated debris and were chopped into small pieces and dried under shade to prevent photolysis and thermal degradation and finally ground to convert to coarser powder.
The secondary metabolites were isolated employing an immersion extraction process using appropriate solvents as described in detail previously.27–32 In a typical experiment, fifty grams of coarsely powdered dry leafy material was pulverised in a ceramic mortar carrying heavy round-ended pestle using six different solvents separately (200 mL each) (chloroform, ethyl acetate, acetone, absolute ethanol, methanol, and distilled water) of increasing polarity, at room temperature. The extracts were kept in an orbital shaker at 100 rotations per min for 24 hours at room temperature and were then filtered using a sterilised Whatman No. 1 filter paper and were evaporated to remove the excess solvent in a rotary vacuum evaporator at 40°C (Yamato RE 801, Japan); residues devoid of solvents were stored at a temperature of −20°C until further use. All solvents and chemicals used were of analytical reagent grade procured from Fisher Scientific co.
Culture and Maintenance of Test Microorganisms
The antimicrobial assay was carried out on a panel of three groups of microorganisms, such as ATCC standards (Staphylococcus aureus (ATCC-25923), Salmonella enterica (ATCC-10708), Klebsiella pneumoniae (ATCC-700603), and Escherichia coli (ATCC-25922)); clinical bacterial isolates (Pseudomonas aeruginosa, Shigella sp., E. coli, and S. aureus) and clinical fungal isolates (Candida albicans, Penicillium spp. Aspergillus flavus, and A. niger). They were obtained from the Ethiopian Public Health Institute and Arba Minch General Hospital. All bacterial strains were maintained on nutrient agar slants (Hi-Media) at 37°C±0.1°C. Sabouraud Dextrose agar slant (Hi-Media) was used for the routine propagation of fungi.30–34
Agar Well Diffusion Assay
Aliquots of the crude leaf extracts in respective solvents (10 mg/mL) were prepared and tested to find their antibacterial activity against human pathogens mentioned above, as per the agar well diffusion assay described previously.29,30 Sterile Mueller-Hinton agar (Hi-Media) was the medium used. Inoculums were prepared from overnight cultures and suspended in nutrient broth, and the turbidity was adjusted to 0.5 Mc Farland standard. Afterwards, the test organisms were uniformly swabbed, and a six-millimetre diameter well was made using a sterile cork borer. About 50 µL of the extract in each solvent separately (10 mg/mL) was added to the wells; Petri plates were then incubated for 24 hours at 37°C, and the inhibitory activity was measured by calculating the diameter (millimetre) of the inhibition zone around the wells. The antifungal assay was performed on Sabouraud dextrose agar (Hi-media). The cell suspensions of respective fungal isolates were evenly inoculated; wells were prepared and carefully filled with 50 μL of the leaf extract. Each solvent used for the respective extraction and dilution was considered as the negative control to validate inferences. All the assays were performed in duplicates. The diameter of the zone of inhibition after 48 hours, corresponding to the activity, was calculated.30–34
Determination of MIC
The tube dilution method was employed to determine the MIC of bacteria, whereas the agar dilution method was applied to determine the MIC of fungal isolates. For the latter test, the crude leaf extract was converted into a stock solution of in respective solvents (200 mg/mL) and was dispensed into a double-strength sterilised molten SDA at 45°C in a water bath. A dosing range corresponding to a factor of 2 (antilog 0.3) (100, 50, 25, 12.50, 6.25, 3.125, 1.56 and 0.78 mg/mL) was applied. These diluted extracts were then mixed with agar and poured aseptically into a sterile Petri dish. A suspension (equal to 0.5 McFarland standard) of each fungal isolate was added, and the dishes were kept at 27°C for 48 hours. The minimum dilution of the extract that completely inhibited the growth of each test organism corresponds to MIC. The positive and negative controls comprised sterilised SDA plates, inoculated with each test organisms with and without the solvent used for extraction, respectively.30–34
The tube dilution method was carried out on nutrient broth in the case of bacterial isolates and the dosing range remained the same as in the case of fungi. Tubes were aseptically inoculated with suspensions (equivalent to 0.5 McFarland standard) of each bacterial isolate and were incubated at 37°C for 24 hours; the minimum dilution of the extract without turbidity corresponds to MIC. The positive and negative controls comprised broth inoculated with each test organism with and without the extraction solvent, respectively.30–34
Bioassay-Guided Column Fractionation
An aliquot of the solvent free crude Me2CO extract (5 gm), the most bioactive one was chromatographed on a silica gel (60–120 mesh) (Merck) column packed using hexane and was eluted with a mixture of hexane and ethyl acetate of varying volume ratio (9:1 of hexane and ethyl acetate and 100% ethyl acetate) yielding ten fractions. Individual fractions were collected and subjected to the antimicrobial assay, after carefully evaporating the solvent off and then preparing a solution of concentration 1 mg/mL, in EtOAc. The three fractions eluted using hexane and ethyl acetate (eluent mixtures rich in EtOAc, ie, 80, 90, and also 100% EtOAc) were found to retain consistent activities against the tested microorganism and were further pooled and subjected to gas chromatography-mass spectroscopy.31 The remaining seven fractions were discarded from analysis due to inconsistent and marginal activities.
Gas Chromatographic and Mass Spectroscopic Analysis (GC-MS)
The pooling of fractions was done by blending the obtained volumes (ie, 70, 60 and 100 mL) of the three consistently bioactive fractions collected as it is (as described above). After mixing (pooling), the solvents (hexane + EtOAc) were completely removed by means rotavap. The pooled active column fraction was then subjected to gas chromatographic and mass spectroscopic analysis, after proper dilution prior to injection in EtOAc. The concentration remained approximately 5 µg/mL. Shimadzu QP-2010 GC-MS system equipped with a capillary column, Rtx 30 m and 0.53 mm internal diameter (RESTEK, USA) and flame ionization detector was used. The temperature of the GC oven was kept at 100°C for two minutes and was further programmed to 280°C at the rate of 10°C/min and then kept at 280°C for 13 min. The split ratio was 1:25, and the injection volume was 2 μL of sample and linear velocity of 30 cm−1. The injection port and detector port temperatures were 260°C and 250°C, respectively. The helium, 5.0 Pas was the carrier gas with a flow rate of 40 mL/min. The GC-MS electron ionisation mode was 150 eV. The mass scanned ranged between m/z 20–500 amu (70 ms accumulation time), and the eluted components from GC were subsequently subjected to mass spectral analysis. Active constituents were identified based on the retention indices and by comparing the mass spectra with the National Institute of Standards and Technology Library of mass spectral data.31,32
Preparative TLC
The highly active pooled column fractions were further fractionated using thin layer chromatographic (TLC) plates (Merck TLC plates (20 × 20 cm, aluminium plates, silica gel 60 f254)) with a 1:9 mixture of hexane and EtOAc. After the development of the chromatogram, the three resolved spots (F1, F2 and F3) were scraped out and extracted in EtOAc. The process was repeated to several times obtain sufficient quantities of individual components, which were further subjected to FT-IR analysis after evaporating the solvent.31,32
FT-IR Analysis
The functional groups in the isolated individual components present in the TLC fractions. ie, F1, F2 and F3 were analysed and identified by recording the spectra between 400 and 4000 cm−1 (FT-IR spectrometer; Thermo Fisher).31
Elemental Analysis
Elemental analyses were done in a 5 E- series C/H/N elemental analyser (5 E-CHN 2200) and determined the carbon, hydrogen, and nitrogen contents in individual samples obtained from the preparative TLC.31
Statistical Analysis
Descriptive statistics were used to summarise the data; a one-way analysis of variance was used to compare the influence of solvents used for extraction and the differences in susceptibility of the test microorganisms. It was carried out using the SPSS version 25; P-values <0.05 were considered statistically significant.
Ethical Considerations
Prior to data collection, ethical clearance was obtained from Arba Minch University, College of medicine and public health ethical review committee. All important ethical issue was considered while collecting the medicinal plant and determining antibacterial and antifungal activity of the medicinal plants the test pathogenic organisms were handled with great care.
Results
Antimicrobial Activity of C. hirsuta Leaf Extracts
The leaf extract of C. hirsuta showed broad and high antimicrobial activities against the tested pathogenic bacteria and fungi. The highest zone of inhibition was observed against the reference isolate, E. coli, in the case of the acetone extract (32 mm), followed by ethanolic extract (30 mm). The chloroform extract also showed some antimicrobial activity (P = 0.019), whereas the aqueous extract was found to be ineffective in most of the cases, except against Shigella sp. and C. albicans. There is no considerable difference among the test microorganisms in terms of their susceptibility to the extracts, except in the case of Salmonella and the standard strain, E. coli, irrespective of the solvent used for extraction (P = 0.043) (Table 1).
 |
Table 1 Antimicrobial Activity of C. Hirsuta Leaf Extracts Against Test Organisms by Agar Well Diffusion Assay |
Minimum Inhibitory Concentrations
The MIC values of crude extracts ranged from 7.5 to 60 mg/mL for all tested microorganisms. Comparatively, ethanolic and methanolic extracts required only minimum concentrations to inhibit the growth of tested fungal isolates (15 to 30 mg/mL); however, all the other three non-aquos extract showed higher MIC values (15 to 60 mg/mL) (Table 2).
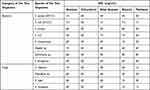 |
Table 2 Minimum Inhibitory Concentrations of C. Hirsuta Leaf Extracts Against Test Organisms |
Bacterial isolates were found to be more susceptible with regard to the level of minimum inhibitory concentrations, compared to the fungal isolates. Among the tested bacteria, the standard strain, E. coli, was inhibited by a relatively lower concentration of the leaf extract (7.5 to 30 mg/mL). In contrast, the concentrations of extracts required to inhibit Salmonella (30 to 60 mg/mL) and Shigella (15 to 60 mg/mL) were comparatively higher (Table 2).
Activity of Column Fractions
The crude Me2CO extract was fractionated using column chromatography with a number of mixtures of hexane and EtOAc of varying volume ratios. The fractions obtained were subjected to antimicrobial assay. As mentioned earlier, the residual antimicrobial activities of fractions were determined against a particular Gram-positive and Gram-negative bacteria, they are S. aureus and E. coli, respectively. In the agar well diffusion assay, fractions obtained by using eluents such as mixtures of 1:8 and 1:9 (v/v) of hexane, EtOAc as well as 100% EtOAc showed remarkable activity against both the tested pathogens S. aureus (18 ± 2.1 mm) and E. coli (26 ± 2.5 mm). The activity of the remaining fractions were found to be inconsistent and only marginal and therefore were discarded from further evaluation and analysis, since this is a bioassay-guided study.
Identification of Chemical Constituents
The chromatogram of chemical constituents of the pooled active column fractions identified by GC-MS analysis is shown in Figure 1. Three main components contained in the pooled active fractions were found to be O-ethylhydroxylamine (43%), 2-ethyl heptanoic acid (20.6%), and 1-nonyl cycloheptane (19.5%) as per the NIST library, which comprise the base peaks, molecular ion peaks, and the typical fragmentation patterns. Several minor compounds also exist, as shown in Table 3. The highly active pooled column fractions were further purified by preparative TLC, which yielded only three fractions with diverse Rf values, ie, F1-0.92, F2- 0.69, and F3- 0.41. The procedure was repeated to accumulate sufficient amounts of these three fractions to obtain the FT-IR spectrum.
 |
Table 3 GC-MS Analysis of Pooled Active Column Fractions |
 |
Figure 1 Chromatogram obtained from the GCMS analysis of pooled active column fraction. |
As per the FT-IR spectra of the three fractions obtained (Table 4) from the preparatory TLC, three individual components were identified corresponding to F1, F2 and F3; F1 was found to be an alkyl-substituted cycloalkane, with specific IR bands at 2850–3000, 1440–1470, and 1380 cm−1 corresponding to C-H stretching, C-H bending and -CH3 scissoring, respectively, as described in Table 2. At the same time, the fraction F2 has shown several IR bands such as 3400 (broad), 2971, 1721, 1419, 1296, and 948 cm−1 matching with O-H stretching, C-H stretching, C=O stretching, O-H bending, C-O stretching, O-H bending (out of plane) vibrations, respectively, and hence the compound could be an alkyl substituted aliphatic acid.
 |
Table 4 FT-IR Analysis of TLC Fractions |
The third fraction, F3 showed IR bands such as 3250–3330 (well-defined), 3350–3400 (well-defined), 650–850 (broad), 1580 to 1600, and 851–840 cm−1 corresponding to N-H stretching (symmetric), N-H stretching (asymmetric), -NH2 out of plane wagging, -NH2 scissoring and -CON stretching vibrations (very typical of alkoxyamines), respectively. Results from the elemental analysis of F1, F2 and F3 perfectly match the theoretical values for 1-nonyl cycloheptane, 2-ethyl heptanoic acid, and O-ethyl hydroxylamine, as given in Table 5.
 |
Table 5 CHN Analysis of F1, F2 and F3 Fractions from the Preparative Analysis |
Discussion
All the five non-aqueous leaf extracts of C. hirsuta showed promising antimicrobial activity in agar well diffusion assay. The values of minimum inhibitory concentrations obtained are impressive. Only lower concentrations of the leaf extracts were needed to inhibit test microorganisms. In a previous study, methanol (80%) and chloroform extracts of C. hirsuta showed antimicrobial activity against some pathogenic bacteria.35
In our current study, the aqueous extract of C. hirsuta showed only a weak antimicrobial activity; only Shigella sp. and C. albicans were susceptible to this extract at a concentration of 60 mg/mL. All the other five extracts showed significant antimicrobial activities against the tested microorganisms. Salmonella and the standard culture, E. coli, showed significantly varying susceptibility profiles, and other test microorganisms had no notable differences in a pair-wise comparative analysis done among them. Antimicrobial activities of chloroform and 80% methanol extracts of C. hirsuta were determined in an earlier study in Ethiopia and the highest zone of inhibition was 12.33 mm;35 the zone of inhibition obtained in our study was, however, higher (at 60 mg/mL concentration). This variation could be attributed to the difference in the method of antimicrobial analysis employed, ie, agar well diffusion and disc diffusion assays.
The MIC values corresponding to the leaf extracts of the title plant in different solvents are more or less at par with the results of the qualitative agar well diffusion assay. Our findings indicate that extractions done using acetone and ethanol are worthy because of the lower MIC values obtained corresponding to several bacterial and fungal pathogens tested using these extracts. The least value of inhibitory concentration was observed in the case of the standard strain, E. coli (7.5 mg/mL for acetone and ethanol extract each), whereas both acetone and methanol extracts were equally effective against C. albicans with the same value, which is also the lowest. Similar is the case of A. fumigatus, where methanol and ethanol extracts showed an identical performance (15 mg/mL).
Extensive research on the phytochemical and biological aspects of some Clematis sp., including C. hirsuta grown in Saudi Arabia, revealed their antimicrobial and anti-inflammatory activities.36 Especially, the volatile constituents contained in C. hirsuta showed remarkable antimicrobial activities against Gram-positive and negative bacteria and the fungus C. albicans. For instance, in the case of B. subtilis, S. aureus and C. albicans the MIC corresponded to a concentration of 0.2 mg/mL of the plant extract. However, in the case of E. coli, the MIC value was 0.45 mg/mL.36 This great disparity in MIC values can be correlated to several factors, such as the nature of the crude extract, fluctuations in concentrations of metabolites, cytoplasmic permeability, and virulence factors associated with different types of bacteria.36
Various members coming under this species contain a diverse array of chemical constituents, such as carbohydrates, flavonoids, tannins, triterpenes/sterols, and fatty acids having multiple functionalities.36 Important drug leads for a number of infectious diseases have long been known, and many of them are constituents of secondary metabolites obtained from several species. Depending on GC-MS, FT-IR and elemental analysis, three major secondary metabolites from the C. hirsuta leaf extract were identified in our study; these three major compounds are O-ethyl hydroxylamine, 2-ethyl heptanoic acid and 1-nonyl cycloheptane. The minor compounds include 3-hexene, 2.4-dimethyl-, propanoic acid, 2-methyl-, 2-ethyl-1-propyl-1,3-propanediyl ester, and (2S,3S)-(-)-3-propyloxirane methanol. Surprisingly, C. hirsuta has not yet been shown to contain these three compounds in much greater proportions in earlier studies as seen in this work.
The most prominent compound, as per the peak area in GC-MS analysis and FT-IR of TLC fraction, is O-ethyl hydroxylamine, which is an aliphatic primary amine. The hydroxylamine derivatives, especially N-substituted hydroxylamine compounds, have antimicrobial activity, and they act as radical scavengers and inhibit the ribonucleotide reductase enzyme.37 However, similar properties of O-ethyl hydroxylamine are not much described in the open literature. As per Duke’s Phytochemical and Ethnobotanical databases, O-ethyl hydroxylamine has anti-tumour and anticancer activities.38 Amine compounds found in some plant cells are responsible for the high responsivity of plants to the development and also to environmental signals. Also, amines are needed for the growth of the plant and the smooth cellular metabolism in them. In other words, phytochemicals containing amine functionality fulfil a series of roles in cellular metabolism and also they integrate the micro-evolutionary signals.39
The second most predominant compound identified is 2-ethyl heptanoic acid, an aliphatic monocarboxylic acid (short-chain fatty acid); short and medium-chain fatty acids possess some antimicrobial activity.40 Search results from Duke’s phytochemical and ethnobotanical databases showed that 2-ethyl heptanoic acid had been detected in plant species such as Sarcostemma acidum, Hymenocardia acida, Cicca acida, Rumex acetosella, Phyllanthus acidus, Citrus acida and Uncaria acida.38
The third most abundant compound found in the analysis of the extract is nonyl cyclo-heptane, which is an alkyl-substituted alicyclic compound. It is a hydrocarbon contained in flowers and leaves of plants such Thevetia peruvian and Plumeria rubra;41 essential oils from these plants have shown antimicrobial activity against S. aureus, E. coli, P. aeruginosa and C. albicans.41 Cycloheptane has also been detected in other plants, such as Piper guineense and Cnidoscolus quercifolius.42,43
According to an extensive literature survey conducted as part of this study, we found that protoanemonin is the major volatile compound in plants belonging to the Ranunculaceae family, along with thirty-five other components. Those involve butylated hydroxytoluene, phenyl ethyl alcohol, carvacrol, benzyl alcohol, and lipoxy linalool.36 When extracted using butanol, the aerial parts of the title plant gave protoanemonin in large excess. However, in our study, we could not find the presence of this compound; variations in the type and the concentration of individual compounds found during such phytochemical analysis could be attributed mainly to the specific plant part extracted and solvent systems used.
It is reported that the amount, composition, and proportions of phytochemicals in many plant species are influenced by a variety of internal and external factors, such as the age of the plant, extent of pollution, evolution, climate, type and pH of the soil, plant materials studied (leaves, flowers, etc.), altitude, precipitation, or even stress conditions that can inhibit or trigger the occurrence of specific compounds within the plants.44,45 Other factors influencing the presence or absence of compounds with particular bioactivities are the timing of harvest, storage temperatures, the type of solvent used, extraction methods, and several other procedural factors involved.46 In the present study, the factors mentioned above would have contributed a lot, and there can be some variations in terms of the type of phytochemical constituents and the therapeutic activity. We have not studied the activity of individual compounds; there can be a synergistic effect exerted by all the major and minor compounds in the plant extract. Nevertheless, as per an extensive literature survey conducted and to the best of our knowledge, this is the first report describing the phytochemical analysis of the Ethiopian C. hirsuta leaf extract and its antimicrobial activity. The GC-MS, FT-IR, and elemental analysis of leaf extracts in the solvent acetone revealed the presence of three major compounds such as O-ethyl hydroxylamine, 2-ethylheptanoic acid, and 1-nonyl cyclo-heptane, along with certain minor compounds viz., 3-hexene, 2.4-dimethyl-, propanoic acid, 2-methyl-, 2-ethyl-1-propyl-1,3-propanediyl ester and (2S,3S)-(-)-3-propyloxiranemethanol. This study is significant in providing inspiring leads for future research, especially in the background of the emergence of drug-resistant bacteria. Further in-depth studies related to the mode of bioactivity and in vivo toxicity may bring forth new drug leads helping the control of human bacterial and fungal pathogens.
Other than the existing pathogens (bacteria and fungi), various newly emerging and remerging variants impart detrimental effects on human health and economy. For instance, SARS CoV-2, Zika, Nipah, dengue, and chikungunya have resulted in severe damages to millions.46–50 In addition, numerous human oncogenic viruses, such as HBV, HCV, EBV, and HPV, are responsible for 18% of cancers. Several antiviral drugs or vaccines are available to manage them effectively, however emerging drug resistance pose serious threats. Therefore, physical scientists and medical researchers are interested in the diverse applications of secondary metabolites from terrestrial and marine flora. Ethnomedicines are gaining popularity due to their safe and broad-spectrum activity over synthetic drugs. Herpes Simplex Viruses, Dengue, and Chikungunya are just a few examples of infections controlled by medicinal plants.51–53 The results of the present study point towards the fact that C. hirsuta is a rich and novel source of drug leads for antimicrobials. Further comprehensive studies on the in vivo medicinal properties of this plant are warranted.
Disclosure
The authors report no conflicts of interest in relation to this work.
References
1. Murray CJ, Aravkin AY, Zheng P., et al. Global burden of 87 risk factors in 204 countries and territories, 1990–2019: a systematic analysis for the Global Burden of Disease Study 2019. Lancet. 2020;396(10258):1223–1249.
2. WHO. Antimicrobial resistance. WHO Fact sheet; 2021. Available from: https://www.who.int/news-room/fact-sheets/detail/antimicrobial-resistance.
3. LeDuc JW. World Health Organization strategy for emerging infectious diseases. JAMA. 1996;275(4):318–320. doi:10.1001/jama.1996.03530280070040
4. Zaman SB, Hussain MA, Nye R, Mehta V, Mamun KT, Hossain N. A review on antibiotic resistance: alarm bells are ringing. Cureus. 2017;9(6):e1403. doi:10.7759/cureus.1403
5. Saleem M, Nazir M, Ali MS, et al. Antimicrobial natural products: an update on future antibiotic drug candidates. Nat Prod Rep. 2010;27(2):238–254. doi:10.1039/B916096E
6. Wright GD. Opportunities for natural products in 21st century antibiotic discovery. Nat Prod Rep. 2017;34(7):694–701. doi:10.1039/C7NP00019G
7. Bicanic T, Bottomley C, Loyse A, et al. Toxicity of amphotericin B deoxycholate-based induction therapy in patients with HIV-associated cryptococcal meningitis. Antimicrob Agents Chemother. 2015;59(12):7224–7231. doi:10.1128/AAC.01698-15
8. Morales-Alvarez MC. Nephrotoxicity of antimicrobials and antibiotics. Adv Chronic Kidney Dis. 2020;27(1):31–37. doi:10.1053/j.ackd.2019.08.001
9. Ancheeva E, Daletos G, Proksch P. Bioactive secondary metabolites from endophytic fungi. Curr Med Chem. 2020;27(11):1836–1854. doi:10.2174/0929867326666190916144709
10. Sohn SI, Rathinapriya P, Balaji S, et al. Phytosterols in seaweeds: an overview on biosynthesis to biomedical applications. Int J Mol Sci. 2021;22(23):12691. doi:10.3390/ijms222312691
11. Shen J, Hu M, Tan W, et al. Traditional uses, phytochemistry, pharmacology, and toxicology of Coreopsis tinctoria Nutt. J Ethnopharmacol. 2021;6(269):113690. doi:10.1016/j.jep.2020.113690
12. Rabia A, Taher A, Ahmed I, Esra Z. Bioactive properties of some selected Libyan plants. J Med Plants Res. 2016;10(6):67–76. doi:10.5897/JMPR2015.5955
13. Puupponen-Pimiä R, Nohynek L, Alakomi HL, Oksman-Caldentey KM. Bioactive berry compounds—novel tools against human pathogens. Appl Microbiol Biotechnol. 2005;67(1):8–18. doi:10.1007/s00253-004-1817-x
14. Roy R, Tiwari M, Donelli G, Tiwari V. Strategies for combating bacterial biofilms: a focus on anti-biofilm agents and their mechanisms of action. Virulence. 2019;9(1):522–554. doi:10.1080/21505594.2017.;1313372
15. Yebirzaf Y, Esubalew T, Workinesh T. The dynamics of medicinal plants utilisation practice nexus its health and economic role in Ethiopia: a review paper. Int J Biodiversity Conservation. 2019;11(1):31–47. doi:10.5897/IJBC2018.1201
16. Mengistu M, Kebede D, Atomsa D, Abebe A, Alemnie D. Status and utilisation of medicinal and aromatic plants in Eastern Hararghe, Ethiopia. Cogent Food Agriculture. 2019;5(1):1701349. doi:10.1080/23311932.2019.1701349
17. Aragaw TJ, Afework DT, Getahun KA. Assessment of knowledge, attitude, and utilisation of traditional medicine among the communities of Debre Tabor Town, Amhara Regional State, North Central Ethiopia: a cross-sectional study. Evid Based Complementary Alternative Med. 2020;10:458.
18. Mesfin F, Demissew S, Teklehaymanot T. An ethnobotanical study of medicinal plants in Wonago Woreda, SNNPR, Ethiopia. J Ethnobiol Ethnomed. 2009;5(1):1–8. doi:10.1186/1746-4269-5-28
19. Gonfa N, Tulu D, Hundera K, Raga D. Ethnobotanical study of medicinal plants, its utilisation, and conservation by indigenous people of Gera district, Ethiopia. Cogent Food Agriculture. 2020;6(1):1852716. doi:10.1080/23311932.2020.1852716
20. Seid MA, Aydagnehum SG. Medicinal plants biodiversity and local healthcare management system in Chencha district; Gamo Gofa, Ethiopia. J Pharmacognosy Phytochemistry. 2013;2(1):845.
21. Nuru A, Hepburn HR Pollen grains of some poisonous bee plants of Ethiopia. In
22. Raimondo D, Von Staden L, Foden W, et al. National Assessment: Red List of South African Plants, Version 2015.1. Pretoria, South Africa: South African National Biodiversity Institute; 2015.
23. Limenih Y, Umer S, Wolde-Mariam M. Ethnobotanical study on traditional medicinal plants in Dega Damot woreda, Amhara Region, North Ethiopia. Int J Res Pharm Chem. 2015;5(2):258–273.
24. Pieroni A, Quave CL, Santoro RF. Folk pharmaceutical knowledge in the territory of the Dolomiti Lucane, inland southern Italy. J Ethnopharmacol. 2004;95(2–3):373–384. doi:10.1016/j.jep.2004.08.012
25. Loi MC, Poli F, Sacchetti G, Selenu MB, Ballero M. Ethnopharmacology of ogliastra (villagrande strisaili, Sardinia, Italy). Fitoterapia. 2004;75(3–4):277–295. doi:10.1016/j.fitote.2004.01.008
26. Cantrell CL, Fischer NH, Urbatsch L, McGuire MS, Franzblau SG. Antimycobacterial crude plant extracts from South, Central, and North America. Phytomedicine. 1998;5(2):137–145. doi:10.1016/S0944-7113(98)80011-1
27. Handa SS, Khanuja SP, Longo G, Rakesh DD. Extraction Technologies for Medicinal and Aromatic Plants, No. 66. Italy: United Nations Industrial Development Organization and the International Centre for Science and High Technology. Trieste; 2008:21–25.
28. Jigna P, Rathish N, Sumitra C. Preliminary screening of some folklore medicinal plants from western India for potential antimicrobial activity. Indian J Pharmacol. 2005;37(6):408–409. doi:10.4103/0253-7613.19085
29. Salie F, Eagles PF, Leng HM. Preliminary antimicrobial screening of four South African Asteraceae species. J Ethnopharmacol. 1996;52(1):27–33. doi:10.1016/0378-8741(96)01381-5
30. Liu JW, Ko WC, Huang CH, et al. Agreement assessment of tigecycline susceptibilities determined by the disk diffusion and broth microdilution methods among commonly encountered resistant bacterial isolates: results from the Tigecycline In Vitro Surveillance in Taiwan (TIST) study, 2008 to 2010. Antimicrob Agents Chemother. 2012;56(3):1414–1417. doi:10.1128/AAC.05879-11
31. Ameya G, Manilal A, Idhayadhulla A. Phytochemical analysis and antimicrobial activity of bersama abyssinica fresen against multidrug-resistant bacterial uropathogens: picolinyl hydrazide is a major compound. J Herbs Spices Med Plants. 2019;25(4):389–400. doi:10.1080/10496475.2019.1635940
32. Ameya G, Manilal A, Merdekios B. In vitro antibacterial activity and phytochemical analysis of Nicotiana tabacum L. extracted in different organic solvents. Open Microbiol J. 2017;11(1):352–359. doi:10.2174/1874285801711010352
33. Manilal A, Sabu KR, Shewangizaw M, et al. In vitro antibacterial activity of medicinal plants against biofilm-forming methicillin-resistant Staphylococcus aureus: efficacy of Moringa stenopetala and Rosmarinus officinalis extracts. Heliyon. 2020;6(1):e03303. doi:10.1016/j.heliyon.2020.e03303
34. Ameya G, Gure A, Dessalegn E. Antimicrobial activity of Echinops kebericho against human pathogenic bacteria and fungi. Afr J Tradit Complement Altern Med. 2016;13(6):199–203. doi:10.21010/ajtcam.v13i6.29
35. Asmamaw H, Yalemtsehay M. Antibacterial potential of the 80% methanol and chloroform extracts of Clematis hirsuta. Af j Pharmacy Pharmacol. 2017;11(16):204–208.
36. Al-Taweel AM Phytochemical and biological studies of some Clematis species growing in Saudi Arabia (Doctoral dissertation, PhD Thesis, King Saud University, College of Pharmacy, King Abdulaziz City, Saudi Arabia).
37. Miret-Casals L, Baelo A, Julián E, et al. Hydroxylamine derivatives as a new paradigm in the search of antibacterial agents. ACS omega. 2018;3(12):17057–17069. doi:10.1021/acsomega.8b01384
38. Duke J, Dr A Duke’s phytochemical and ethnobotanical database. Available from: https://phytochem.nal.usda.gov/phytochem/search.
39. Bouchereau A, Guénot P, Larher F. Analysis of amines in plant materials. J Chromatogr B Biomed Sci Appl. 2000;747(1–2):49–67. doi:10.1016/S0378-4347(00)00286-3
40. Huang CB, Alimova Y, Myers TM, Ebersole JL. Short-and medium-chain fatty acids exhibit antimicrobial activity for oral microorganisms. Arch Oral Biol. 2011;56(7):650–654. doi:10.1016/j.archoralbio.2011.01.011
41. ElZanaty SA, Seif Eldein NA, ElGebaly EA, ElGhaly EM, ElGizawy HA. Chemical composition and antimicrobial activity of the essential oils of Thevetia peruviana and Plumeria rubra cultivated in Egypt. Azhar Int J Pharmaceutical Med Sci. 2022;2(2):34–42.
42. Sulaimon LA, Anise EO, Obuotor EM, et al. In vitro antidiabetic potentials, antioxidant activities and phytochemical profile of African black pepper (Piper guineense). Clinical Phytosci. 2020;6(1):1–3. doi:10.1186/s40816-020-00236-2
43. de Oliveira-Júnior RG, Ferraz CA, de Oliveira AP, et al. Chemical constituents of non-polar fractions obtained from Cnidoscolus quercifolius Pohl (Euphorbiaceae), a Brazilian medicinal plant native to Caatinga biome Chemical constituents of non-polar fractions obtained from Cnidoscolus quercifolius Pohl (Euphorbiaceae), a Brazilian medicinal plant native to Caatinga biome. Revista Virtual de Química. 2019;11(2):498–516.
44. Figueiredo AC, Barroso JG, Pedro LG, Scheffer JJ. Factors affecting secondary metabolite production in plants: volatile components and essential oils. Flavour Fragrance j. 2008;23(4):213–226. doi:10.1002/ffj.1875
45. Gobezie S, Manilal A, Seid M, Lulekal E, Tsegaye Y. In vitro antibacterial activity of four plant species used in traditional medicine practices of south Omo zone, southern Ethiopia. Acta Microbioloica Hellenica. 2020;65(2):2020.
46. Manilal A, Sabu KR, Woldemariam M, et al. Antibacterial activity of Rosmarinus officinalis against multidrug-resistant clinical isolates and meat-borne pathogens. Evid Based Complementary Alternative Med. 2021. Apr;29:548.
47. Bos S, Gadea G, Despres P. Dengue: a growing threat requiring vaccine development for disease prevention. Pathog Glob Health. 2018;112:294–305. doi:10.1080/20477724.2018.1514136
48. Russo G, Subissi L, Rezza G. Chikungunya fever in Africa: a systematic review. Pathogens and Global Health. 2020;114(3):111–119. doi:10.1080/20477724.2020.1748965
49. Sharma V, Kaushik S, Kumar R, Yadav JP, Kaushik S. Emerging trends of Nipah virus: a review Pathog Glob Health. Int J Med. 2020;114:111–119.
50. Sharma V, Sharma M, Dhull D, Sharma Y, Kaushik S, Kaushik S. Zika virus: an emerging challenge to public health worldwide. Can J Microbiol. 2020;66(2):87–98. doi:10.1139/cjm-2019-0331
51. Kaushik S, Kaushik S, Sharma Y, Kumar R, Yadav JP. The Indian perspective of COVID-19 outbreak. Virus Dis. 2020;4:1–8.
52. Vachirayonstien T, Promkhatkaew D, Bunjob M, Chueyprom A, Chavalittumrong P, Sawanpanyalert P. Molecular evaluation of extracellular activity of medicinal herb Clinacanthus nutans against herpes simplex virus type-2. Nat Prod Res. 2010;24:236–245. doi:10.1080/14786410802393548
53. Kaushik S, Dar L, Kaushik S, Yadav JP. Identification and characterization of new potent inhibitors of dengue virus NS5 proteinase from Andrographis paniculata supercritical extracts on in animal cell culture and in silico approaches. J Ethnopharmacol. 2020;267:113541. doi:10.1016/j.jep.2020.113541
 © 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
