Back to Journals » Journal of Asthma and Allergy » Volume 17
Assessment of the Implementation of Global Initiative for Asthma (GINA) 2019 Guidelines for Treatment of Mild Asthma Among Pediatric Registrars: A Quasi-Interventional Study
Authors Abashar IBH, Salih OAMM, Joda TAA , Alsedig MFA, Omer AT , Ahmed HA, Hemmeda L , Esmaeel MAM , Mohamed Ahmed KAH
Received 21 October 2023
Accepted for publication 12 March 2024
Published 5 April 2024 Volume 2024:17 Pages 339—347
DOI https://doi.org/10.2147/JAA.S442573
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Luis Garcia-Marcos
Iman Bashir Hamid Abashar,1,* Omaima Abdel Majeed Mohamed Salih,2,* Tarteel Abbas Abaker Joda,3,* Mai Fathi Awadalla Alsedig,3,* Alaa T Omer,3,* Hayat A Ahmed,3,* Lina Hemmeda,3,* Mariam Alazraa M Esmaeel,3,* Khabab Abbasher Hussien Mohamed Ahmed3,*
1Asthma Clinic Mohammed Alamin Hamid Pediatric Hospital, Omdurman, Sudan; 2Departments of Pediatrics and Child Health, Faculty of Medicine and Health Sciences, Omdurman Islamic University, Omdurman, Sudan; 3Faculty of Medicine, University of Khartoum, Khartoum, Sudan
*These authors contributed equally to this work
Correspondence: Mariam Alazraa M Esmaeel, Faculty of Medicine, University of Khartoum, ElQasr Avenue, Khartoum, Khartoum State, 11111, Sudan, Tel +249915077027, Email [email protected]
Background and Aims: It is essential to have proper treatment and management for asthma in order to minimise symptoms, lessen the burden, and lower the chance of exacerbations. To better control asthma, the purpose of this study was to evaluate and enhance paediatric registrars’ understanding and application of asthma treatment.
Methods: The Sudan Medical Specialisation Board (SMSB) paediatric registrars provided data for this quasi-interventional study between April and September of 2021. Twice, both before to and following the intervention education sessions, the questionnaire was delivered. SPSS version 28 was used to analyse the data after it had been cleaned up in an Excel document.
Results: 203 (or 77.8%) of the 261 were women. A substantial rise from 8.1 ± 4.12 SD to 18 ± 5.03 SD in the mean overall knowledge score of registrars between the pre-and post-intervention periods. A significant difference (p=0.001) was observed in the post-intervention phase, with first-year registrars (R1) demonstrating higher scores than their senior colleagues. The registrars’ total knowledge scores did not differ significantly from one another during the pre-intervention period. The Global Initiative of Asthma (GINA) guidelines of management were implemented to a certain extent, according to the study. Of the registrars, 148 (56.7%) and 203 (77.8%) evaluated step one management in children ages 5 and under; 66 (25.3%) and 213 (81.6%) evaluated step one management in children ages 6 to 11; and 66 (25.3%) and 213 (81.6%) evaluated step one management in children ages 6 to 11 in pre- and post-intervention, respectively.
Conclusion: Given that the intervention in this study greatly increased registrars’ knowledge, doctors should obtain training on the GINA 2019 recommendations through conferences, workshops, and academic programmes. To find out why R1 outperforms their older counterparts, more investigation has to be done.
Keywords: asthma, GINA, management of asthma, Sudan
Introduction
According to the definition, asthma is “a heterogeneous disease, usually characterised by chronic airway inflammation”. The respiratory symptoms, which include coughing, chest tightness, wheezing, and fluctuating expiratory airflow restriction, are what characterise it. These symptoms can change over time and in intensity.1 It is becoming more widely accepted that genetic predisposition, host characteristics, and environmental exposures combine to cause asthma, a complex multifactorial condition. These comprise environmental factors (pollens, mould and other aeroallergens, weather), host factors (obesity, nutritional factors, infections, and allergic sensitization), and genetic factors. Although the underlying mechanisms of asthma are still poorly understood, they may involve airway inflammation, tone regulation, and reactivity.
It is increasingly acknowledged that asthma may really consist of a collection of diverse phenotypes with various aetiologies and prognoses rather than being a single illness.2 The prevalence of asthma is estimated to have affected 339.4 million people worldwide, a 3.6% increase in age-standardized prevalence since 2006. Asthma ranks 16th among the top causes of years lived with disability and 28th among the top causes of disease burden globally.3
Reducing risk and managing symptoms are the long-term objectives of asthma treatment. By reducing airway inflammation by minimising pro-inflammatory environmental exposures, using daily controller anti-inflammatory medications, and managing coexisting conditions that can exacerbate asthma, the goal is to lessen the burden on the patient as well as their risk of exacerbations, airway damage, and medication side effects. Better asthma control is usually associated with less inflammation, which also means fewer exacerbations and lower demand for quick-relief asthma drugs.4
In addition to improving prevention and management, the Global Initiative for Asthma (GINA) was created to raise awareness of the disease among medical professionals, public health officials, and the general public. It offers a thorough and integrated approach to asthma management that can be customised for unique patient circumstances and local conditions.5 Through the creation of recommendations suitable for local, regional, or national situations, GINA offers the basis necessary to raise awareness of asthma and enhance asthma treatment globally. GINA was created to promote the development of guidelines and knowledge translation on a global scale, taking into account the needs and resources of local communities, with the shared goal of reducing asthma morbidity and mortality by bridging the knowledge gap between what is known and how asthma management is practised.6
Related earlier research was conducted in Nigeria on the use of GINA principles in paediatric residents’ asthma care. Evaluating paediatric residents’ clinical use of GINA guidelines was the goal. The results of this study showed that paediatric residents did not make good use of the GINA recommendations.7 Apart from the economic hardship, Sudan has other challenges in managing asthma. The combination of these multifaceted issues—which might include physicians, patients, or health services—leads to inadequate asthma management.8
Since following management principles significantly alters the outcome, optimising management is the key to the answer. Although there are no governmental guidelines for the care of asthma, doctors in Sudan practice addressing the condition.6 The purpose of this study is to evaluate and enhance paediatric registrars’ understanding and practice of managing asthma in order to better control asthma, reduce the need for numerous medications, minimise adverse effects, and minimise hospitalisation and worsening of the condition.
Materials and Methods
Study Design and Study Setting
A quasi-experimental study was conducted, where a pre- and post-intervention assessment was done.
The study was conducted at the Sudan Medical Specialization Board SMSB, which is the sole professional training body in the Republic of Sudan mandated to manage and deliver medical and health speciality programs in the country.
The study was conducted in the period between April –September 2021.
Study Population
All Pediatric registrars of the Sudan Medical Specialization Board who registered in the period of 2017–2021 included residents from other states and out-of-service registrars who agreed to be part of the study. Those who refused or did not respond were excluded from the study.
Sample Size and Sampling Technique
The sample was calculated using the Yamane formula:
Where the n=minimum sample size
N=total population number as taken from the pediatric council secretary.
e= degree of accuracy, set as 5%
Thus:
n=746/1+746(0.0025) =260.8=261 participants
Sample selection was done by systematic sampling technique.
Data Collection Tool
Two parts made up the Google form survey. The first part consisted of 12 questions regarding the GINA2019 classification of asthma severity, and the second part consisted of 8 questions about the GINA2019 therapy recommendations for mild asthma. An Arabic translation and an English translation of the questionnaire were performed. A second time, prior to the interventional education sessions, the questionnaire was given to study participants in order to assess the improvement in registrars’ knowledge 24 hours following the educational intervention (due to registrar availability).
Following their completion of the pre-intervention assessment, the chosen registrars received phone calls to confirm their participation. Following this, they received an invitation to participate in an online WhatsApp session discussing the management of mild asthma and asthma classification in accordance with the guidelines set forth by the Global Initiative for Asthma 2019. A specialist physician led the session, and participants acknowledged their participation by sending texts. Following the talk, there was an open, interactive conversation during which the speaker responded to questions by voice or text messaging.
Data Entry and Analysis
The most recent version of SPSS 28 was used to clean, input, and analyse data into a Microsoft Excel datasheet. Proportions and frequencies are used to represent categorical data. Using an independent sample, a comparison of mean knowledge and practice was conducted before and after the education intervention. Mann–Whitney T-test for the relationship between total knowledge and gender; Kruskal–Wallis test for the relationship between total knowledge and age; and degree of training for the relationship between total knowledge and age. Assuming compliance with all statistical test regulations and a certain degree of confidence, a p-value of less than 0.05 was deemed statistically significant. Following analysis, the data were shown as figures, narrative illustrations, cross-tabulation (bi-variable tables), and uni-variable tables.
Results
Demographics and Level of Training
The study included 261 paediatrics registrars who registered at the Sudan Medical Specialization Board SMSB. The age of 141 (54%) of the residents ranged from 20 to 30 years old and most of the registrars 203 (77.8%) were females. The majority of the pediatric registrars in our study were found to be in year four of the training program R4 (Table 1).
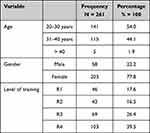 |
Table 1 The Demographical Data and Level of Training of the Pediatric Residents Participating in This Study (N=261) |
Assessment of the Knowledge of the Pediatric Registrars About Asthma Classification and Management
Following the intervention, the mean total registrars’ knowledge score increased statistically significantly from 8.1 ± 4.12 SD in the pre-intervention phase to 16.18 ± 5.03 SD in the post-intervention phase, according to a Wilcoxon signed-rank test. There is a statistically significant increase in the registrars’ score of knowledge about Asthma classification and treatment following the intervention. The pre-intervention phase mean for each was (5.76 ± 2.76 SD and 2.33 ± 1.97 SD when P-value 0.001), and the post-intervention phase mean was (10.10 ± 2.79 SD and 6.07 ± 2.44 SD when P-value 0.001) for asthma classification and treatment respectively.
Between the registrars’ overall knowledge scores in the pre-intervention and post-intervention phases, there was no significant difference in terms of gender or age groups. There was no significant difference between the residents’ total knowledge scores and the various levels of training during the pre-intervention period. Although there was a significant difference in the post-intervention phase (p=0.001), R1 registrars had the greatest scores, followed by R4 and R3, and R2 registrars had the lowest scores (Table 2).
 |
Table 2 The Residents’ Total Knowledge Scores in the Pre-Intervention and Post-Intervention Phases in Terms of Their Gender, Age and Level of Training (N=261) |
Assessment of the Knowledge of Pediatric Registrars About the Mild Asthma Classification
In the assessment of the clinical scenario of 5 years old or younger asthmatic patients who managed by step one: 251 (96.2%) of the residents correctly classified the asthma in the pre-intervention phase compared to 257 (98.5%) in the post-intervention phase while in the clinical scenario of 5 years old or younger asthma patient who managed by step two: 72 (27.6%) of the registrars chose the correct classification in the pre-intervention phase compared to 204 (78.2%) in post-intervention phase (Table 3).
In the assessment of the clinical scenario of asthmatic children aged 6 to 11 years who managed by step one: 135 (51.7%) of the residents correctly classified asthma in the pre-intervention phase compared to 233 (89.3%) in the post-intervention phase while in the clinical scenario of asthmatic children aged 6 to 11 years who managed by step two:80 (30.7%) of the registrars chose the correct classification in the pre-intervention phase compared to 216 (82.8%) in post-intervention phase (Table 3).
In the assessment of the clinical scenario of asthmatic adolescents (12 years or more) who managed by step one: 64 (24.5%) of the residents correctly classified asthma in the pre-intervention phase compared to 229 (87.7%) in the post-intervention phase while in the clinical scenario of asthmatic adolescent (12 years or more) who managed by step two: 104 (39.8%) of the registrars chose the correct classification in the pre-intervention phase compared to 222 (85.1%) in post-intervention phase (Table 3).
Assessment of the Knowledge of Paediatric Registrars About the Moderate and the Severe Asthma Classification
In the assessment of the evaluation of the clinical scenario of moderate asthma in children aged five years or younger: 169 (64.8%) of the registrars correctly classified the asthma in the pre-intervention phase compared to 227 (87%) in the post-intervention phase. However, in the clinical scenario of severe asthma in children aged five years or younger: 142 (54.4%) of the registrars correctly classified the asthma in the pre-intervention phase compared to 218 (83.5%) in the post-intervention phase (Table 4).
When determining the classification of the clinical scenario of moderate asthma in patients aged 6–11 years, in the management by the preferred option: 127 (48.7%) registrars chose the correct classification in the pre-intervention phase compared to 214 (82%) in the post-intervention phase. In the same scenario, in the management by true alternative option: 109 (41.8%) registrars chose the correct classification in the pre-intervention phase, compared to 206 (78.9%) registrars in the post-intervention phase (Table 4).
Regarding the assessment of moderate asthma classification in adolescents 12 years and older: 137 (52.5%) of the registrars chose the correct classification in the pre-intervention phase compared to 201 (77%) in the post-intervention phase. On the other side, in the assessment of severe asthma in adolescents 12 years and more: the registrars that chose the correct classification were 114 (43.7%) and 210 (80.5%) in the pre - and post-intervention phase respectively (Table 4).
Implementation Level of Global Initiative of Asthma (GINA) Guidelines of Management
As for the assessment of step one management in children aged 5 and younger, 148 (56.7%) and 203 (77.8%) of the registrars did so in the pre- and post-intervention phases respectively, whereas 66 (25.3%) and 213 (81.6%) of the registrars did so in the pre- and post-intervention phases for step one management in children aged 6 to 11 years. On the other hand, when it came to the evaluation of step one management for adolescents 12 years and older, 34 (13%) and 198 (75.9%) of the registrars, respectively, selected the right response before and after the intervention (Table 5).
 |
Table 5 The Implementation Level of Global Initiative of Asthma (GINA) Guidelines of Management Among the Paediatric Residents Participating in This Study (N = 216) |
In the pre-and post-intervention phases, 67 (25.7%) and 182 (69.7%) of the registrars, respectively, selected the right response for the evaluation of step 2 management for children aged 5 and under. Regarding the comparison of step 2 management for children aged 6 to 11 years and adolescents aged 12 and older, respectively, 72 (27.6%) and 65 (24.9%) of the registrars chose the right answer in the pre-intervention and post-intervention phases, while 192 (73.6%) and 193 (73.9%) did so in the post-intervention phase (Table 5).
In terms of the evaluation of the management of virally induced wheeze, 96 registrars (36.8%) made the right treatment choice in the pre-intervention phase compared to 222 residents (85.1%) in the post-intervention phase. When exercise-induced wheeze management was evaluated, 56 (21.5%) registrars chose the appropriate course of action in the pre-intervention period compared to 183 (70.1%) in the post-intervention phase (Table 6).
 |
Table 6 Assessment of Implementation of Management of Viral-Induced Wheeze and Exercise-Induced Wheeze Among the Paediatric Registrars: N=261 |
Discussion
Numerous studies in the literature have assessed asthma knowledge and management among health professionals, but very few of them conducted an assessment regarding the implementation of GINA guidelines for asthma management, especially here in Sudan. In this study, we aimed to assess and improve the knowledge and practice about Asthma management among pediatric registrars to achieve better control of Asthma. Moreover, we applied an educational intervention to assess the difference in the knowledge level of asthma management pre-and post-intervention. The main findings of our study showed that the mean total knowledge score among the registrars increased statistically significantly after the intervention. There is a statistically significant increase in the score of both knowledge about Asthma classification and treatment following the intervention. These findings are consistent with what has been proven that knowledge of and compliance with GINA guidelines enhances the treatment and results in the medical setting.9 Our results also indicated that there was no significant difference between the registrars’ total knowledge scores and the various levels of training during the pre-intervention period. This was not the case in a study conducted in Saudi Arabia among primary care physicians, as there were disparities in knowledge of the guidelines between junior versus their more senior colleagues. The greatest knowledge scores. It’s unclear why but this might be attributed to their great interest and eagerness to apply what they have learned throughout the interventional sessions more than the senior registrars. Emmanouil et al have reached a similar result in their study, he concluded that continued medical Education (CME) have positive outcomes on recent graduates more than senior ones.10 Moreover this finding is opposite to what has been shown in another study, that registrars’ level of training play no role in asthma treatment decisions.3 Nevertheless another study interestingly reported that senior registrars have higher knowledge scores which was in contrast to our observation.10 Furthermore regarding knowledge of registrars about mild asthma classification, the registrars exhibited a remarkable increase in the level of knowledge about the classification throughout different pediatric age groups such as; 5 years old or younger managed by step 1, asthmatic children aged 6 to 11 managed by step 1 or 2 and asthmatic adolescents aged 12 or above managed by step 1 or 2 in the post-intervention phase. This depicts how the interventional sessions were very successful in achieving their target by raising registrars’ self-reported knowledge and understanding of mild asthma. Concerning the implementation of GINA 2019 guidelines of step one and two management, registrars’ adherence to the guidelines increased dramatically in the post-intervention phase for the management of steps one and two in all paediatric age groups. Meanwhile, other studies where GINA guidelines were not implemented for example in a research done in south-west Nigeria, it revealed deficits in the application of GINA guidelines in dealing with asthma.11 Another study conducted among physicians treating asthma patients in a tertiary hospital in Nigeria, highlighted that there is inadequate knowledge about GINA guidelines.12 Additionally in a Nigerian state, more than 50٪ of the community pharmacist stated that lack of knowledge and training could constitute hurdles to complying with GINA guidelines.9 Our results and the previous studies’ results strongly emphasized that effective continuous medical education (CME) in terms of educational interventions that we did- or in any other form, leads to improvement in physician behaviour, clinical practice and healthcare outcomes.13,14 It’s now widely recognized that CME programs utilizing practice-enabling and reinforcing strategies have significantly enhanced clinicians’ performance and healthcare-related outcomes.15 The introduction of this educational intervention about GINA 2019 guidelines in pediatric training programs have proved to be useful in boosting the knowledge about asthma management among registrars. The sessions presented were 100% online, which makes its reproducibility possible. And we could include a wide range of physicians (from less experienced to more experienced ones) in this program to improve overall asthma care.
Limitation
There may be an overestimation of the effect of the educational intervention as a result of non-randomization.
Conclusion
After the educational intervention, registrars’ knowledge about asthma and asthma management increased significantly. Moreover, after applying the intervention first-year registrars (R1) have shown more positive results than their senior colleges. The results of this study indicate that the educational intervention has succeeded in raising the knowledge of the residents about the international guidelines in asthma management. Presenting such sessions to registrars and physicians, in general, may ensure an improvement in asthma care.
Recommendations
Data Sharing Statement
The datasets used and/or analysed during the current study are available from the corresponding author upon reasonable request.
Ethical Considerations
Written ethical clearance and approval for conducting this research were obtained from the institutional review board of the Sudan Medical Specialization Board and Educational Development Center (EDC). Written permission was obtained from the administrative authority of the Sudan Medical Specialization Board and the Council of Pediatrics and Child Health. Confidentiality is maintained by serial numbers and codes. Informed consent was obtained from all pediatric registrars who participated in this study.
Funding
This study was funded independently by the authors.
Disclosure
The authors declare that they have no competing interests.
References
1. Tesse R, Borrelli G, Mongelli G, Mastrorilli V, Cardinale F. Treating pediatric asthma according guidelines. Front Pediatr. 2018;6. doi:10.3389/fped.2018.00234
2. Dharmage SC, Perret JL, Custovic A. Epidemiology of asthma in children and adults. Front Pediatr. 2019;7. doi:10.3389/fped.2019.00246
3. Global asthma network the global asthma report; 2018. Available from: www.globalasthmanetwork.org.
4. Marcdante KJ, Kliegman R. Nelson essentials of pediatrics; n.d.
5. Pocket guide for asthma management and prevention a pocket guide for health professionals updated 2018 (for adults and children older than 5 years) based on the global strategy for asthma management and prevention; 2018. Available from: www.ginasthma.org.
6. Elwarrag HM, Halay S, Awadalla H, Balla SA, Abdulhamid OH. Assessment of primary care doctors’ practice regarding asthma management in health centers in Khartoum State, Sudan, 2017. J Adv Med Med Res. 2018;27(7):1–8. doi:10.9734/jammr/2018/43617
7. Ayuk AC, Ubesie A, Odimegwu CL, Iloh K. Use of Global initiative for asthma (GINA) guidelines in asthma management among paediatric residents in a Sub Saharan African country: a cross-sectional descriptive study. Pan Afr Med J. 2017;27:1–6. doi:10.11604/pamj.2017.27.120.9260
8. Muneswarao J, Hassali MA, Ibrahim B, Saini B, Ali IAH, Verma AK. It is time to change the way we manage mild asthma: an update in GINA 2019. Respir Res. 2019;20. doi:10.1186/s12931-019-1159-y
9. Amorha KC, Idoko KE, Okonta MJ, Ukwe CV. Knowledge and practice of the global initiative for asthma report among community pharmacists in a Nigerian state. Pan Afr Med J. 2020;37(83):1–11. doi:10.11604/pamj.2020.37.83.18897
10. Rovithis E, Lionis C, Schiza SE, et al. Assessing the knowledge of bronchial asthma among primary health care physicians in Crete: a pre-and post-test following an educational course. BMC Med Educ. 2001;1(2). doi:10.1186/1472-6920-1-2
11. Adeniyi B, Ilesanmi O, Obaseki D, Desalu O, Betiku B, Erhabor G. Relationship between knowledge and quality of asthma care among physicians in South-West Nigeria. Niger J Clin Pract. 2017;20(5):566–572. doi:10.4103/1119-3077.206363
12. Umoh V, Ukpe I. Knowledge of the asthma guidelines among doctors in a tertiary hospital in Nigeria. Indian J Allergy Asthma Immunol. 2012;26(2):77. doi:10.4103/0972-6691.112552
13. O’Brien MA, Freemantle N, Oxman AD, Wolfe F, Davis D, Herrin J. Continuing education meetings and workshops: effects on professional practice and health care outcomes. Cochrane Database Syst Rev. 2001. doi:10.1002/14651858.cd003030
14. Clark N, Lachance L, Milanovich AF, Stoll S, Awad DF. Characteristics of successful asthma programs. Public Health Rep. n.d.;124(6):797–805. doi:10.1177/003335490912400606
15. Davis DA, Ann Thomson M, Oxman AD, Brian Haynes R, Epidemiology C, Oxman B. Evidence for the effectiveness of CME a review of 50 randomized controlled trials recognition of the importance of continuing medical education (CME) has been dogged by from the Departments of Family Medicine (Drs). JAMA. 1992;268(9):1111–1117.
 © 2024 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2024 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.



