Back to Journals » Integrated Pharmacy Research and Practice » Volume 12
Assessment of Dispensing Malpractice in Community Drug Retail Outlets in South Gondar Zone, Northwest Ethiopia: A Simulated Patient Experience
Authors Bogale Kassie A , Mengie Ayele T , Mekonnen Agidew M
Received 2 May 2023
Accepted for publication 18 July 2023
Published 25 July 2023 Volume 2023:12 Pages 171—183
DOI https://doi.org/10.2147/IPRP.S416830
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Professor Jonathan Ling
Achenef Bogale Kassie,1 Teklie Mengie Ayele,1 Melaku Mekonnen Agidew2
1Department of Pharmacy, College of Health Sciences, Debre Tabore University, Debre Tabore, Amhara Regional State, Ethiopia; 2Department of Biomedical Science, College of Health Sciences, Debre Tabore University, Debre Tabore, Amhara Regional State, Ethiopia
Correspondence: Achenef Bogale Kassie, Email [email protected]
Background: Pharmacy professionals in community drug retail outlets, as the most accessible personnel for the community, are engaged in consultation and responding to health problems in addition to filling prescriptions. In doing so, different dispensing malpractices are observed and much is not known on the issue in Ethiopia.
Objective: The study aimed at assessing dispensing malpractice at pharmacies, drug stores and drug vendors in South Gondar zone.
Methodology: A cross-sectional study design with a descriptive approach was applied from April 1 to June 30. The data was collected using the simulated patient method. Seven prescription-only medicines and a diarrheal case were requested during visit. All drug retail outlets in South Gondar zone that were in service during data collection were visited.
Results: Almost all prescription-only medications were dispensed without prescription at all community drug retail outlets. Of all the dispensaries, 19 (82.6%) provided a partial dosage regimen of amoxicillin. Presence of fever and pregnancy status were asked about by dispensers in only 8% and 20% of visits for diarrhea, respectively. Medication history was also rarely requested. Medication was dispensed in 80% of visits for diarrhea, all of which included antimicrobials. Oral rehydration salt was considered in only two (10%) dispensaries.
Conclusion: Dispensing medications without a prescription is common in community drug retail outlets in South Gondar zone in Amhara Regional State. Our findings also showed that detailed assessments of patients’ signs and symptoms are not performed properly by the dispensers to understand the diarrheal case. Training of pharmacy professionals and strict regulatory control are needed.
Keywords: dispensing malpractice, simulated patient survey, community drug retail outlets
Background
The primary concern of good pharmacy practice in each section of the health care facility is the welfare of patients that can be achieved through the best use of medicines and medical products.1 Good dispensing practice is one way to attain this objective. Such a practice is important in realizing rational drug therapy, and pharmacy professionals can play a huge role in this regard, although rational drug therapy requires the rigorous efforts of all health care professionals towards that goal.1,2
Dispensing embraces all activities that are addressed between the time the prescription or oral request of the patient or care provider is presented and the drug or other items are dispensed to them.2 Dispensing is normally considered a simple, routine process that cannot go wrong. All resources used for patient care and the efforts invested in process may be considered as useless if there is a problem during dispensing.3
Public health institutions and community drug retail outlets (CDROs) are the main sites to obtain medications. This is because medicines at CDROs are easily accessible, widely available, with acceptable waiting times and longer hours of opening.4 In addition to filling prescriptions, dispensers in such settings are involved in self-care. CDROs are commonly involved in the provision of both prescription-only medicines (POMs) and over-the-counter medication (OTC) based on a specific drug request and a disease manifestation explained by the client. During this time, the main task of the pharmacy professional is to distinguish a minor illness from a more serious condition since this helps to provide better recommendations. Doing this may be important to provide other options such as non-drug treatment, visiting a practitioner for full investigation and also management of illnesses using an appropriate non-prescription medicine.5,6 By doing this, pharmacy professional can adhere to professional ethics and need to be in line with standards of good pharmacy practice.1
However, there are different malpractices related to this issue. Dispensers often decide on and recommend unsuitable treatment due to inadequate assessment of the client’s condition prior to medication provision.7–9 Drug shops stock medicines which are illegally obtained from the public sector and sell them when requested without prescription.10 Throughout the world, POMs such as antimicrobials can be accessed without prescription from various CDROs.10–17 The commonly proposed reasons for dispensing malpractice, especially in developing countries, include poor regulation, failing health systems, lack of professional ethics with poor subject matter knowledge, lack of financial incentives for those in public health institutions and business orientation of pharmacists in community CDROs, pharmacists’ familiarity with the management protocol and their belief that the same medication will be prescribed by the practitioners.18
Dispensing malpractice has various impacts on the community as well as on the individual patient, including medical and economic-related problems. The most common consequence is the risk of antibiotic resistance. A larger percentage of antimicrobial resistance, adverse drug reactions and masking of infectious disease diagnosis is commonly associated with frequent use of non-prescription antimicrobial drugs.19
Although much is not known regarding the overall practices of CDROs, some studies in Ethiopia showed that dispensing of partial doses of POMs medicines without prescription is a common practice when consulted for treatment with minimal symptomatic complaints.20,21
In Ethiopia, studies which disclosed some contraventions of pharmacy practice regulations by CDROs were conducted over ten years ago. Additionally, studies conducted in Ethiopia on dispensing malpractice of pharmacy professionals, using a simulated client method which helps to see the actual behavior, are limited in number and most of these are focused on assessment of antibiotics.22,23 So, this study was conducted to assess the current picture of dispensing practice by using selected POMs for various diagnosese and a diarrheal case. The findings of the study will definitely sensitize concerned stakeholders, including the regulatory authority of the country.
Methodology
Study Area
This study was conducted in South Gondar zone in Amhara region. According to the 2007 census conducted by the Central Statistical Agency of Ethiopia (CSA), South Gondar zone has a total population of 2,651,350 people, of whom 1,345,306 are men and 1,306,044 are women, which is an increase of 16% over the 1994 census. With an area of 14,095.19 square kilometers, South Gondar has a population density of 188.10; 252,674 people (9.53%) are urban inhabitants.24 Debre Tabor town, the administrative town for this zone, is located 659 km from Addis Ababa, the capital of Ethiopia. The zone consisted of 10 hospitals (one comprehensive specialized referral hospital and nine primary hospitals), 10 health centers, and 96 health posts. All are public institutions. In addition to these, the zone also consists of 105 private clinics (28 medium clinics, 74 primary clinics and 3 specialty clinics) and 64 private drug retail outlets (8 pharmacies, 54 drug stores, and 2 drug vendors).
Study Design and Period
The data was collected from October 1 to February 30, 2023 using a descriptive cross-sectional study design and the data were collected using the simulated patient method. This method is nowadays becoming popular in the research arena since it is important to assess the real behavior of health care workers in the actual setting. In this method, a trained individual who could pretend to be a regular consumer is used to assess a health care setting with a standardized or non-standardized written or non-written request. If being cognizant of being observed is a means to ensure practitioners’ behavioral change, using this method must be the best methodological tool for pharmacy practice.25,26 Eight tracer POMs which are indicated for various cases and with a commonly dispensed profile for the top ten communicable and non-communicable diseases in Ethiopia were selected for direct drug requests without prescriptions.27 These include amoxicillin capsule, amoxicillin + clavulanic acid (augmentin) oral suspension, artemether + lumefantrine (coartem), ketoconazole cream, omeprazole capsule, sildenafil citrate (Viagra), glibenclamide and enalapril. A diarrhea case was used to evaluate patient assessment and response to symptoms. So, a given dispensary was visited for a total of nine times by different investigators with an interval of a few day. The role of asking for medication was done verbally for amoxicillin capsule, Viagra and coartem; in written form on a piece of paper for augmentin, omeprazole, and ketoconazole cream and by providing an empty pack for glibenclamide; and by pointing to the shelf for enalapril. For a particular drug, a predetermined and similar scenario was presented by all investigators in all CDROs whenever further information was requested by pharmacy professionals. Community pharmacy professionals who were willing to issue amoxicillin without prescription were further requested for one strip (partial dose). Seeking care for diarrhea was based on a female patient (sister) who is a dweller in each selected town, South Gondar zone. She is 30 years old and two months pregnant. She has had mucoid and bloody diarrhea since the day before. She also has fever and severe abdominal cramps. She had had a meal in a restaurant the night before yesterday. She did not try any medication for her illness and is not taking medication for other purposes.
Source Population
All CDROs in South Gondar zone were the source population for the study.
Study Population
The study population was all CDROs in South Gondar zone which were serving clients when the data was collected.
Sampling
Sample Size
All dispensaries from each category of CDROs that were providing services during the study period were studied. A total of 8 pharmacies, 54 drug stores, and 2 rural drug vendors were addressed. So, the total number of CDROs included in our study was 64.
Sampling Technique
Even though CDROs were stratified as pharmacies, drug stores/shops and rural drug vendors for analysis purposes, all categories of CDROs from each stratum were included in the study.
Study Variables
Dependent Variables
Dispensing malpractice.
Independent Variables
Category of CDROs.
Type of Drug Requested.
Patient assessment.
Data Collection and Analysis
Data Collection Instruments
The data collection tool was developed after deeply searching previously conducted studies to include all necessary variables and was validated by the social and public health department after taking into account the purpose, objective and methodology of our study. Then, the data collection tool was used tested before the actual data collection. The data collection tool included two components. The first part is on dispensing a specific drug request and the second part is assessment of patient and reply to a diarrheal case.
Data Collectors
Ten 5th year pharmacy students were trained to collect the data. The training tried to make them a good simulator. During their training, each expected scenario was discussed and rehearsed in detail. They were told to approach the dispenser as a lay individual and they were told not to use a medical term that is indicative of a professional. In case the dispenser does not agree to issue the requested drug, the data collectors were told not to pressure the dispenser to provide the requested drug. In addition to this, the investigators were told to give information only if asked by the dispenser to do so. The assigned investigators recorded what happened during their communication in the data collection tool instantly after each CDRO visit, making sure that the dispenser did not see them.
Pretesting the data collection tool was priorly done before actual data collection started to be sure that it could enable an appropriate data collection process. Pretesting was done on 15 CDROs in Bahr Dar town, which were not part of South Gondar zone. In case of diarrheal case assessment, additional information was added based on data from pretest to make the tool clearer and more direct.
In order to ensure data quality, discussion was done in detail and a simulated practice was performed on the process of data collection between the investigators. Any misunderstandings and challenges that happened during the real data collection were solved through discussion and strategies were developed for succeeding visits. To reduce the chance of data omissions, collecting incomplete data, and to avoid significant illegible writing, the investigators were thoroughly checked each data at the end of each day.
Data Analysis and Interpretation
Data analysis was done using SPSS version 20 and descriptive statistics were used for data summarization with proportions; most of the data was presented using tables and figures.
Ethical Considerations
During development of the data collection tools and during the data collection period, data that identified the actual dispensaries were not collected. The confidentiality of the data obtained was further assured by keeping secured the data filled in in the tools. Three months before the data collection, the principal investigator of this work explained that we plan to collect data from dispensaries using a simulated client without disclosing the exact time and the respondents agreed to give their consent so long as their privacy is protected.
Operational Definitions
Pharmacy: a drug retail outlet run by a pharmacist
Drug store/shop: a drug retail outlet run by a druggist
Rural drug vendor: a drug retail outlet run by a health assistant
Dispensing malpractice: dispensing incorrect dosage and frequency of the right medication, dispensing the wrong medication, dispensing prescription-only medicines without prescription, and failing to assess signs and symptoms before dispensing the drug or referring to physicians
Results
General Information
The study was conducted on 64 CDROs in total: 8 pharmacies, 54 drug stores, and 2 rural drug vendors, headed pharmacist, druggist, and health assistant, respectively. A total of 576 covert visits were done.
Dispensing Drug Request
In all 64 CDROs, a request for amoxicillin was done orally without provision of a prescription. The drug was available in all dispensaries during visits. All 64 dispensaries agreed to dispense the full dose medication without prescription. Out of 64 dispensaries where the drug was available, 53 (82.81%) of the CDROs provided a partial dosage regimen when requested. Out of which, 24 (45.28%) CDROs took time to explain the danger of taking partial dosage regimen and advised to take additional dose. In 11 (17.19%) of the CDROs, while willing to dispense the drug without prescription, they resisted dispensing one strip (10 capsules) of amoxicillin, insisting that it should be taken three times a day for a minimum of 5 days. Professionals in 47 (73.44%) of the CDROs asked who will take the drug and only in 12 (18.75%) did they enquire about the symptoms indicating that the requested drug was needed (Table 1).
 |
Table 1 Response to Amoxicillin Request in Community Drug Retail Outlets in South Gondar Zone, Northwest Ethiopia, June 2022 |
Requests for amoxicillin + clavulanic acid (Augmentin) revealed that the drug was unavailable in the two rural drug vendors, three pharmacies and twenty-four drug stores. Most dispensers where the drug was available (82.86%) did not ask why the drug was needed and all dispensed the medication without asking for a prescription (100%) (Table 2).
 |
Table 2 Response to Amoxicillin + Clavulanic Acid Request in Community Drug Retail Outlets in Gondar Town, Northwest Ethiopia, June, 2022 |
As shown in Figure 1, mystery clients found that artemether + lumefantrine (coartem) was stocked in only 29 (45.31%) of the CDROs. All dispensaries which stocked the drug dispensed it without prescription. Before dispensing, pharmacy professionals in 11 (37.93) dispensaries asked for detail information from clients regarding medical and past medication history.
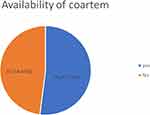 |
Figure 1 Availability of artemether + lumefantrine (coartem) in community drug retail outlets in South Gondar zone, Northwest Ethiopia, collected using the simulated patient method, April 2022. |
Ketoconazole was available in all CDROs. A request for ketoconazole cream written on a non-prescription paper was followed by dispensing of the drug in all CDROs. The intended use of the medication was enquired about in only two pharmacies and five drug stores (Table 3).
 |
Table 3 Response to Ketoconazole Cream Request in Community Drug Retail Outlets in South Gondar Zone, Northwest Ethiopia, June 2022 |
The only question from the dispenser to the client during omeprazole request was the number of strips the client wanted. Otherwise, they issued the drug without even knowing for whom the drug was wanted (Table 4).
 |
Table 4 Response to Omeprazole Request in Community Drug Retail Outlets in South Gondar Zone, Northwest Ethiopia, June 2022 |
Sildenafil citrate was available in all eight pharmacies (Figure 2), and none of the dispensers asked for additional information before issuing the requested number of tablets. No one can get sildenafil citrate from the drugs list for drug shops in Ethiopia. But it was stocked in most of the drug shops, all of which dispensed without prescription.
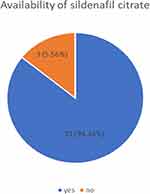 |
Figure 2 Availability of sildenafil citrate in community drug retail outlets/stores in South Gondar zone, Northwest Ethiopia, collected using the simulated patient method, June 2022. |
Glibenclamide was available in 53 CDROs (8 pharmacies and 45 drug stores) when visited and no professional hesitated to dispense the drug upon provision of an empty package. Dispensers asked no questions before dispensing (Table 5).
 |
Table 5 Response to Glibenclamide Request in Community Drug Retail Outlets in South Gondar Zone, Northwest Ethiopia, June 2022 |
Diarrheal Case Assessment and Response
Patient Assessment
From the total 64 CDRO who were asked to supply antidiarrheal drugs, 44 (68.75%) asked a minimum of one question. Whether the requested help is for self or for someone else (37, 57.81%), whether the diarrhea looks watery or bloody (40, 62.50%), whether the medication is required for male or female patient (31, 48.44%), and whether the patient is an adult or child (27, 42.19%) were the most commonly asked questions. A very important question, whether the patient is taking any medication for other health conditions, was not asked by any one of the dispensaries and only one CDRO asked whether the patient in need had taken any medication for management of the existing case. Pregnancy status was enquired about in 21 (32.81%) of the CDROs (Table 6).
 |
Table 6 Questions Asked by Providers in Response to a Diarrheal Case in Community Drug Retail Outlets in South Gondar Zone, Northwest, Ethiopia, June 2022 |
Outcome of Visit
In 59 (92.19%) of the visits, the required medication was provided. Referral to a clinic to be assessed further by an appropriate practitioner were recommended in five of the consultations. These referrals were from three pharmacies and two drug stores, all because the case involved a pregnant woman. In one dispensary, the provider was unwilling to be consultated, stating that there is no medication for diarrhea. Providers in one CDRO preferred to advise to come back again without providing any remedy for a reported pregnant diarrhea case (Table 7).
 |
Table 7 Outcome of Visit for a Diarrheal Case in Community Drug Retail Outlets in South Gondar Zone, Northwest Ethiopia, June 2022 |
Medication Dispensed
From CDROs where the requested medication was given, a single drug was dispensed in 48 (75%) and two drugs were used in 16 (25%). Most of the dispensaries recommended tinidazole (31, 51.56%) and metronidazole (15, 23.44%). Oral rehydration salt was considered in only 3 (37.50%) pharmacies and 15 (27.78%) drug stores. In the case of a two-drug combination recommendation, ciprofloxacin with tinidazole was suggested on six occasions and cotrimoxazole + tinidazole was used in five occasions. After pregnancy status was confirmed, tinidazole with cotrimoxazole was dispensed on five occasions (Table 8).
 |
Table 8 Medications Dispensed for a Diarrheal Case in CDROs in South Gondar Zone, Northwest Ethiopia, June 2022 |
Discussion
Across all CDROs involved in this study, dispensing POMs without any formal order from authorized practitioners is a common practice. Various studies in different parts of the world revealed this type of malpractice.11,14,16,17,19 A study in Saudi Arabia showed that 100%, 97.9%, and 89.5% of requests for captopril, amoxicillin + clavulanic acid, and fluoxetine, respectively, were dispensed without a prescription.15 But our findings are even higher than those reported by Abdul et al.21 Another simulated patient study (2016) with a comparable sample size to ours, in Addis Ababa, went along with our findings in that 87.93% of the dispensaries were reported to provide POMs without prescription.25 Focusing on their business and competition between CDROs may explain this finding, which is associated with the increasing number of drug retail outlets.15 In this study, all dispensaries gave glibenclamide without prescription, which is similar to a study in Addis Ababa where all pharmacies and 80% of drug stores issued glibenclamide without prescription.28 On the other hand, a Gaza Strip study revealed that most pharmacists were unwilling to prescribe pharmacological agents for cardiovascular diseases and diabetes mellitus; 64.2% of respondents were never dispensed glibenclamide without prescription.13
In our study, only 11 (17.19%) CDROs which stocked amoxicillin resisted dispensing a partial dosage regimen when asked for one. Out of those which did dispense the partial dosage regimen, only 37.5% explained the disadvantage of taking a partial dosage and advised taking the additional dose at some future time without affecting the recommended time interval for the drug. This is in line with a simulated client approach study in Tanzania in which 71.43% of CDROs dispensed prescriptions with an incomplete dose.29 The current finding is much worse than a previous report in a study conducted in selected towns of Amhara region in which 60% of dispensers said they will not dispense a partial dose.20 This is one indication of the importance of the simulated client method to expose the actual behavior and hence get a real figure. A slightly higher figure (91%) of dispensed subtherapeutic doses of amoxicillin was reported in a Kenyan study.10 Other studies elsewhere also reported incomplete dose dispensing of antibiotics.12,16
Competition, fear of losing customers and inability of patients to pay for medical costs, including buying complete dosage regimens, may encourage pharmacy professionals to engage in such dispensing malpractices.13 However, by no means is it acceptable. In addition to dispensing a partial dosage regimen and prescribing following incomplete diagnosis, too frequent utilization of antimicrobials can cause extensive drug resistance. Since overutilization of sildenafil citrate is a confirmed cause of cardiovascular side effects, frequent and indiscriminate use in contraindicated patients may even result in death.30 Dispensing medications such as glibenclamide without refill instructions at scheduled appointments may encourage patients to simply collect drugs by avoiding going to a health facility at each check-up schedule (eg, glucose level). Patients’ glucose levels may vary to a large extent from the normal value and cause different complications, which makes periodic medical check-ups mandatory.
This study also indicated that questions are rarely asked following a specific drug request, although the level is different for different drug requests. Sildenafil citrate and glibenclamide were dispensed without any questioning. Ketoconazole and omeprazole were issued without any question in most CDROs. This is in support of a previously studied result in Addis Ababa in that more than 80% of CDROs failed to request prescriptions, tolled for visiting doctors, provided nonpharmacological advice, and gave instructions on side effects of medications.27 After coartem requests, details of symptoms to rule out other acute febrile illnesses were requested in only 58.6% of CDROs which stocked the drug and there were occasions on which amoxicillin and amoxicillin + clavulanic acid were dispensed without even knowing why and for whom the drugs were needed. Medication-related allergy history was not asked for at all. Similar studies in Saudi Arabia, Egypt and Tanzania revealed that pharmacists either ask further questions occasionally or not at all when being for a drug.12,14–16 This indicates that dispensers are focusing mainly on their business rather than patient safety. They are also not giving time to avoid drug–drug interactions= and related adverse drug reactions.
Sildenafil citrate is not included in the list of drugs for drug shops in Ethiopia.31 In spite of this fact, it was stocked in 51 (94.44%) out of 54 drug stores. artemether + lumefantrine (coartem) was available in 29 (45.31%) CDROs. Even though the drug should be available through the legal pathways in public health institutions, the drug was stocked in most dispensaries illegally. Although we could not be sure, we suspect that a possibility exists for stocked coartem products in CDROs to be illegally obtained from public facilities, which was also the case in a study in Kenya.10
This study secondly focused on the assessment of dispensing practice using a diarrhea case scenario. A specific question was expected to be addressed: whether the patient is an adult or a child was requested in 42.19% of CDROs and only 23.44% requested the exact age of the client. In contrast to this, in a study conducted in Gondar town, the specific age of the patient was the most frequently asked question (98.35%).32 Similarly, a study in Pakistan showed that the patient’s age was enquired about in 83.3% of visits to pharmacies.8 Astonishingly, all CDROs failed to ask whether the patient who needed the medication was taking another medication for other health conditions and only one asked whether the patient was using medication for a current condition. A similar study assessing the situation in Gondar town supports our findings in that medication history concerned none of the CDROs investigated.32 Another study in Pakistan also is in line with the current study, in that only 7.8% of the pharmacy professionalsasked this question.8 This shows that dispensers are not committed enough to invest time to gather medication profiles and they barely link symptoms to drug-related adverse effects even though it should be their primary activity. An essential manifestation to distinguish the presence of infectious from non-infectious diarrhea, fever, was asked about in only 3 (4.69%) pharmacies. Although most drugs recommended for the management of diarrhea indicate a type of contraindication during pregnancy, professionals in most (82.81%) CDROs did not give weight to assessment of the presence or absence of pregnancy. This indicates that they are commonly ignoring this sensitive issue during drug selection, even though the presented case is one of the patient populations that needs special attention.33 Overall, the degree of patient assessment is unsatisfactory. Similar studies also found such inadequacies by pharmacists.9,17,32
The results of this study revealed that all dispensaries handed out medication. Similarly, Hussain and Ibrahim documented that antibiotics were dispensed in 77.1% of visits and Abdulhak et al documented that antibiotics were dispensed in 77.6% of visits involving different clinical scenarios. Both of these studies indicated that a substantial percent of pharmacies prefer not to refer patients for more medical evaluations.8,17
Tinidazole was the most frequently dispensed medication in the current study (51.56%) and ciprofloxacin (28.13%) was next. A study in Saudi Arabia revealed that metronidazole was the most frequently dispensed drug for similar case (89%).17 Another study in Pakistan also showed that metronidazole was commonly used (58.7%).8 The preference of tinidazole over metronidazole may be due to its short course of treatment.34 Basically, oral rehydration salt should be the mainstay of diarrhea management, especially when fluid loss is high, which is not the case in our study. In contrast to this, a study in Nigeria found much better oral rehydration salt use.9 The drug combination commonly used (ciprofloxacin + tinidazole and cotrimoxazole +tinidazole) indicated that dispensers are more likely using medications which treat a diarrheal case with either a protozoal or bacterial cause. This kind of practice, however, incurs unnecessary costs for the patient. After pregnancy status was confirmed, tinidazole and cotrimoxazole were dispensed in one visit. But these drugs are contraindicated in pregnancy. All medications dispensed except oral rehydration salt are POMs in Ethiopia.31
Although this study addressed many important issues, once the dispensers agreed to fill a drug request or give specific medication(s) for diarrhea, the simulated client left the CDRO by telling the provider that they needed to collect enough money to afford the medications requested. Because of this, we were unable to assess the extent and appropriateness of dosage instructions and other related-drug information provided by pharmacy professionals while dispensing a drug.
Conclusion
Dispensing POMs without amedical order is a common practice in CDROs in our study area. CDROs even dispensed a partial dosage regimens of amoxicillin. Further investigations of a patient’s condition during dispensing of a specific drug were not witnessed in most CDROs. CDROs also stocked drugs which they intended not to handle. In addition, CDROs are not interested and not capable of assessing whether they provide the right drug for the right patient.
Abbreviations
CDROs, community drug retail outlets; CSA, Central Statistical Agency of Ethiopia; OTCs, over-the-counter medicines; POMs, prescription-only medicines.
Data Sharing Statement
All data are contained within the manuscript.
Ethics Approval and Consent to Participate
The Debre Tabor University, College of Health Science’s research and ethical review committee reviewed the proposal before any attempt was made to collect data. Confidentiality of the data collected was secured starting from data collection tool development and design, with great care taken by removing direct provider information from gathered data and not allowing third party access.
Acknowledgments
The authors would like to acknowledge Debre Tabor University for providing ethical approval.
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Funding
The study was conducted by authors self-sponsored.
Disclosure
The authors declare that they have no competing interests.
References
1. World Health Organization. WHO Technical Report Series, No. 961, 48th Report, Annex 3. Geneva: World Health Organization; 2011.
2. Ministry of Health. Good Dispensing Practice and Pharmaceutical Supply Chain. Ethiopia: Addis Ababa; 2019.
3. Clark M. Management Sciences for Health. MDS-3: Managing Access to Medicines and Health Technologies. Arlington, VA: Management Science for Health Drug Supply; 2012.
4. Harding G, Taylor KM, editors. Pharmacy Practice. CRC Press; 2017.
5. Winfield AJ, Rees J, Smith I, editors. Pharmaceutical Practice E-Book. Elsevier health sciences; 2009.
6. Jon Waterfield W. Community Pharmacy Handbook. London, UK: Pharmaceutical press; 2020.
7. Chua SS, Ramachandran CD, Paraidathathu TT. Response of community pharmacists to the presentation of back pain: a simulated patient study. Int J Pharm Pract. 2006;14(3):171–178. doi:10.1211/ijpp.14.3.0003
8. Hussain A, Ibrahim MI. Management of diarrhoea cases by community pharmacies in 3 cities of Pakistan. East Mediterr Health J. 2012;18(6):635–640. doi:10.26719/2012.18.6.635
9. Ogbo PU, Aina BA, Aderemi-Williams RI. Management of acute diarrhea in children by community pharmacists in Lagos, Nigeria. Pharm Pract. 2014;12(1). doi:10.4321/S1886-36552014000100002
10. Wafula F, Abuya T, Amin A, Goodman C. Availability and dispensing practices for antimalarials and antimicrobials in western Kenyan pharmacies. Pharm Reg Affairs. 2013;2(1):1–8.
11. Basak SC, Sathyanarayana D. Evaluating medicines dispensing patterns at private community pharmacies in Tamilnadu, India. South Med Rev. 2010;3(2):27–31.
12. Minzi OM, Manyilizu VS. Application of basic pharmacology and dispensing practice of antibiotics in accredited drug-dispensing outlets in Tanzania. Drug Healthc Patient Saf. 2013;5:5. doi:10.2147/DHPS.S36409
13. Hammad J, Qusa H, Aljeesh Y. The dispensing practice of the over the counter drugs in the gaza strip. IUG J Nat Eng Stud. 2012;20(1):31–39.
14. Sabry NA, Farid SF, Dawoud DM. Antibiotic dispensing in Egyptian community pharmacies: an observational study. Res Social Adm Pharm. 2014;10(1):168–184. doi:10.1016/j.sapharm.2013.03.004
15. Al-Mohamadi A, Badr A, Mahfouz LB, Samargandi D, Al Ahdal A. Dispensing medications without prescription at Saudi community pharmacy: extent and perception. Saudi Pharm J. 2013;21(1):13–18. doi:10.1016/j.jsps.2011.11.003
16. Kagashe GA, Minzi O, Matowe L. An assessment of dispensing practices in private pharmacies in Dar-es-Salaam, Tanzania. Int J Pharm Pract. 2011;19(1):30–35. doi:10.1111/j.2042-7174.2010.00075.x
17. Abdulhak AA, Al Tannir MA, Almansor MA, et al. Non prescribed sale of antibiotics in Riyadh, Saudi Arabia: a cross sectional study. BMC Public Health. 2011;11(1):1–5. doi:10.1186/1471-2458-11-1
18. Dameh M, Norris P, Green J. New Zealand pharmacists’ experiences, practices and views regarding antibiotic use without prescription. J Prim Health Care. 2012;4(2):131–140. doi:10.1071/HC12131
19. Morgan DJ, Okeke IN, Laxminarayan R, Perencevich EN, Weisenberg S. Non-prescription antimicrobial use worldwide: a systematic review. Lancet Infect Dis. 2011;11(9):692–701. doi:10.1016/S1473-3099(11)70054-8
20. Abula T, Ashagrie G. Assessment of drug utilization from prescribers and dispensers perspectives in selected towns of Amhara region, Ethiopia. Ethiop J Health Dev. 2003;17(3):231–237.
21. Abula T, Worku A, Thomas K. Assessment of the dispensing practices of drug retail outlets in selected towns, north west Ethiopia. Ethiop Med J. 2006;44(2):145–150.
22. Belachew SA, Hall L, Selvey LA. Magnitude of non-prescribed antibiotic dispensing in Ethiopia: a multicentre simulated client study with a focus on non-urban towns. J Antimicrob Chemother. 2022;77(12):3462–3465. doi:10.1093/jac/dkac341
23. Alemayehu T, Mekonnen E, Beedemariam G. Practice of over-the-counter dispensary of antibiotics for childhood illnesses in Addis Ababa, Ethiopia: a simulated patient encounter study. Int J Infect Dis. 2020;101:88. doi:10.1016/j.ijid.2020.09.257
24. Central Statistical Agency (CSA). The 2007 Population and Housing Census of Ethiopia. Statistical Report for Amhara Region; Part 1: Population Size and Characteristics. Ethiopia: Addis Ababa; 2007.
25. Watson MC, Skelton JR, Bond CM, et al. Simulated patients in the community pharmacy setting–Using simulated patients to measure practice in the community pharmacy setting. Pharm World Sci. 2004;26(1):32–37. doi:10.1023/B:PHAR.0000013467.61875.ce
26. Watson MC, Norris P, Granas AG. A systematic review of the use of simulated patients and pharmacy practice research. Int J Pharm Pract. 2006;14(2):83–93. doi:10.1211/ijpp.14.2.0002
27. Misganaw A, Naghavi M, Walker A, et al. Progress in health among regions of Ethiopia, 1990–2019: a subnational country analysis for the Global Burden of Disease Study 2019. The Lancet. 2022;399(10332):1322–1335. doi:10.1016/S0140-6736(21)02868-3
28. Erku DA, Mekuria AB, Surur AS, Gebresillassie BM. Extent of dispensing prescription-only medications without a prescription in community drug retail outlets in Addis Ababa, Ethiopia: a simulated-patient study. Drug Healthc Patient Saf. 2016;8:65–70. doi:10.2147/DHPS.S106948
29. Horumpende PG, Sonda TB, van Zwetselaar M, et al. Prescription and non-prescription antibiotic dispensing practices in part I and part II pharmacies in Moshi Municipality, Kilimanjaro Region in Tanzania: a simulated clients approach. PLoS One. 2018;13(11):e0207465. doi:10.1371/journal.pone.0207465
30. Koda-Kimble MA. Koda-Kimble and Young’s Applied Therapeutics: The Clinical Use of Drugs. Lippincott Williams & Wilkins; 2012.
31. EFMHACA. List of Medications for Drug Shop: 4th edition, Addis Ababa; 2012.
32. Wondimsigegn D, Woldegerima B, Taddese AA. History taking and response to an adult diarrheal case among community drug retail outlets in Gondar town, north-west Ethiopia: a simulated-client survey. J Pharm Policy Pract. 2021;14(1):1–8. doi:10.1186/s40545-021-00310-1
33. Luu BQ, Kayingo G, Hass VM, editors. Advanced Pharmacology for Prescribers. Springer Publishing Company; 2021.
34. Bakshi JS, Ghiara JM, Nanivadekar AS. How does tinidazole compare with metronidazole? A summary report of Indian trials in amoebiasis and giardiasis. Drugs. 1978;15(Suppl 1):33–42. doi:10.2165/00003495-197800151-00008
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
