Back to Journals » Orthopedic Research and Reviews » Volume 15
Arthroscopic Minced Cartilage Repair in the Glenohumeral Joint – Short Term Clinical Outcome in a 33-Year-Old Handyman: A Case Report
Authors Karkosch RF, Smith T, Jensen G, Tuecking LR, Horstmann H
Received 26 April 2023
Accepted for publication 4 October 2023
Published 23 November 2023 Volume 2023:15 Pages 245—251
DOI https://doi.org/10.2147/ORR.S418032
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Professor Clark Hung
Roman Frederik Karkosch, Tomas Smith, Gunnar Jensen, Lars Rene Tuecking, Hauke Horstmann
Orthopedic Surgery Department, Hannover Medical School (MHH), Hannover, D-30625, Germany
Correspondence: Hauke Horstmann, Email [email protected]
Objective: Clinical outcome data for the novel minced cartilage procedure are sparse. While good results have been shown for the knee joint, this is the first report in the current literature regarding this increasingly important procedure in the glenohumeral joint.
Case Description: A 33-year-old handyman with a cartilage defect in the humeral head underwent an all arthroscopic one-stage cartilage repair with the AutoCartTM procedure (Arthrex GmbH, Munich, Germany). A senior specialist examined the patient before surgery, five-, 12-and 24-weeks post-surgery. Outcome parameters (Constant-Murley Score, UCLA Shoulder Score and ASES Score) and radiographic imaging were recorded.
Results: At six months, follow-up the outcome parameter showed excellent results, the joint pain decreased to numeric rating scale (NRS) 0. The postoperative magnetic resonance imaging (MRI) revealed a thin cartilage layer in the treated area with sufficient integration to the surrounding tissue. The cartilage in the former defect zone presented a homogeneous signal, which was comparable to the intact cartilage.
Conclusion: This case report underlines the growing interest in single-stage arthroscopic minced cartilage procedures and shows promising results in the glenohumeral joint. Yet, larger investigations with long-term follow-up are necessary to provide reliable clinical data to determine if comparable results can be achieved over time.
Keywords: cartilage repair, shoulder, minced cartilage
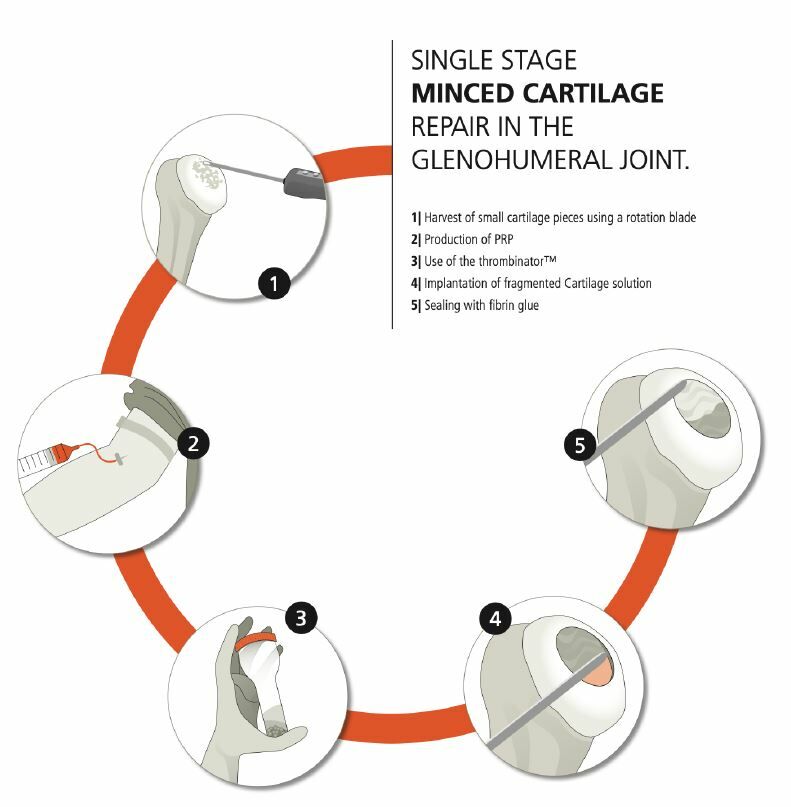
Graphical Abstract:
Introduction
The treatment of full thickness cartilage defects in the glenohumeral joint remains a challenge and often leads to osteoarthritis in the long term.1,2 Its origin is usually associated with several pathologies such as chronic or acute trauma, instability, rotator cuff injuries, inflammatory processes and osteonecrosis.3 Consequently, the overall incidence of cartilage defects in the shoulder varies between 6% and 17% in patients undergoing shoulder arthroscopies for other injuries.3–7 In the absence of concomitant structural injuries, it is difficult to detect chondral defects in the glenohumeral joint early on as even extensive lesions are often overlooked in the MRI examination.1,8 In addition, due to limited load bearing compared to the lower extremity these defects are characterized by a longer asymptomatic period.9,10
When nonoperative treatment fails, several surgical treatment options are available. Thus, total shoulder arthroplasty and partial resurfacing provide good results in pain relief and mobility, they may not be a suitable option for young patients due to a limited life span of the prosthesis.11 Joint-preserving options such as arthroscopic debridement with or without microfracture, CAM Procedure, autologous matrix-induced chondrogenesis (AMIC), autologous chondrocyte implantation (ACI), and osteochondral transplantation (OATS) have been described as successful treatment options.3,12,13 Yet, there is no consensus in the literature which treatment option is the most suitable one and in contrast to other major joints clinical evidence is extremely limited.9 Minced cartilage treatments for cartilage defects have been reported for nearly 4 decades,14 but have regained popularity lately. The modern minced cartilage procedure uses ultra-small cartilage particles in combination with thrombin and platelet-rich-plasma (PRP).15 In contrast to the gold standard ACI, it can be performed in a single surgery and is rather cost efficient. For deeper defects, a membrane augmentation is also possible.
This case report is an attempt to provide technical insights and much needed clinical outcome data into an all-arthroscopic minced cartilage procedure on the humeral head.
Case Presentation
Medical History
A 32-year-old handyman reported severe shoulder pain (NRS 6) for a duration of 6 months prior surgery. Several microtrauma had occurred in the past. No previous surgeries were reported. Nonoperative treatment included nonsteroidal anti-inflammatory drugs (NSAiDs), physical therapy and joint infiltrations. The patient regularly smoked ten cigarettes per day.
Clinical Evaluation and Radiographic Findings
The patient was examined before surgery, 5-, 12- and 24-weeks post-surgery by a senior specialist who was not the surgeon. Outcome parameters (Constant-Murley Score, UCLA Shoulder Score and ASES Score), active and passive range of motion (ROM), as well as strength testing of the rotator cuff were recorded. Pain level was determined at rest and in motion according to the numeric rating scale (NRS). To determine the location of the defect and concomitant injuries standard X-ray, MRI and a CT scan were conducted.
The patient showed an 18.5×21.9 mm measuring Grade IV chondral lesion to the center of the humeral head with an intact subchondral layer. There was no evident damage to the glenoid. With an inferior humeral osteophyte of 3 mm, this case was classified as a Grade 1 osteoarthritis (Samilson and Prieto classification).16
Decision Making
At the age of 32, an occupation that includes heavy lifting as well as forceful use of the right arm and the presence of a unipolar cartilage defect, an arthroplasty was not a suitable option for this patient. As a salvage operation, the arthroscopic minced cartilage procedure was discussed as an option. Smoking and grade 1 osteoarthritis were discussed as limiting factors beforehand.
Surgical Technique
The patient underwent an all arthroscopic one-stage cartilage repair with the AutoCartTM procedure (Arthrex GmbH, Munich, Germany). This was performed according to the technique described by Lorenz et al2 (graphical abstract). In brief, PRP is collected at the beginning of the surgery by the anesthetist. The patient was placed in a beach-chair position. Standard anterior inferior, posterior and lateral portal were used to access the glenohumeral joint and confirm the indication. Arthroscopic cannulas were placed in the anterior inferior and posterior portal. No concomitant procedures needed to be performed. With an intact subchondral layer, no bony augmentation was indicated. The cartilage from the defect was harvested with a 3.8 mm shaver in combination with a graft-net device (Arthrex GmbH, Munich, Germany). The vertical rim of the lesion was created by using a curette. It was not necessary to harvest additional cartilage. Diagnostic arthroscopy and cartilage harvesting were performed using wet arthroscopy. The following reimplantation of the cartilage was performed in a dry manner (Figures 1 and 2).
 |
Figure 1 Display of arthroscopic minced cartilage implantation. |
 |
Figure 2 Minced cartilage fixation with thrombin. |
This was achieved by extensive suction and the careful use of a swab. At reimplantation, the cartilage fragments were fixed with autologous conditioned plasma and thrombin, which were produced according to the guidelines for this procedure (AutoCartTM procedure, Arthrex GmbH, Munich, Germany).
Postoperative Care
Postoperative management included the application of a brace for 4 weeks to limit weight bearing and range of motion. Passive assisted motion was limited by pain only. Continuous passive motion was applied for four weeks postoperatively.
Results
Clinical Results
The demonstrated case shows excellent clinical results six months post-surgery. Significant increases among the Constant-Murley Score (50 vs 98), UCLA Shoulder (16 vs 35) Score and ASES Score (40 vs 98.3) were reported (Figure 3).
 |
Figure 3 Display of outcome measures. |
Moreover, pain was reduced from NRS 6 to NRS 0 at six months with full range of motion. Consequently, the use of NSAiDs was not necessary anymore. In spite of recurrent admonitions, the patient continued smoking (10 cigarettes/day).
Radiological Results
The postoperative MRI revealed a thin cartilage layer in the treated area with sufficient integration to the surrounding tissue (Figures 4 and 5).
 |
Figure 4 Preoperative MRI scan. |
 |
Figure 5 MRI scan at three-months post-surgery. Note slight chondral layer. |
The cartilage in the former defect zone presented a homogeneous signal, which was comparable to the intact cartilage. The subchondral bone showed decreasing signal enhancement compared to the preoperative MRI scan. Signs of osteoarthritis grade 1 (Samilson and Prieto) were still present.
Discussion
This is the first case report to provide clinical outcome data and a postoperative MRI scan for an all-arthroscopic minced cartilage repair in the glenohumeral joint. While cartilage repair in the lower limb is performed frequently, evidence in the glenohumeral joint is sparse.9 Despite a comparably thin layer of cartilage, defects are rarely discovered early on in the absence of concomitant injuries.17 Among a variety of treatment options, minced cartilage with PRP has gained popularity especially in the knee joint.15
The use of current state minced cartilage therapy has been enhanced by promising animal studies performed by Domínguez Perez et al.18 This study group was able to show a “near to normal” cartilage repair 6 months after inflicting an 8 mm defect to the femoral condyle in a sheep model. No animal studies have examined glenohumeral cartilage repair using this technique. Moreover, there is a single report in the literature describing a modern minced cartilage technique in the shoulder by Lorenz et al.2 Yet, no clinical data has been reported.
While debridement and microfracture of the glenohumeral joint fail to prevent the progression of osteoarthritis,6,19 ACI has shown promising results in some studies.20 Nevertheless, convincing data for high quality and volume studies is not available. In contrast to ACI minced cartilage can be performed in a single surgery with the opportunity to reduce costs. It offers a quick, modern membrane-free procedure.
In the described case excellent results could be achieved after six months. Three months after the intervention, the patient was able to continue with his profession. Pain or limitations in ROM were not reported at six months. Yet, cartilage tends to show a healing response over several months and therefore the long-term result might differ from the outcome after six months.
This being a case report, limitations have to be addressed. Due to its nature this study does not include a control group or reference data. In addition, no quantification of pain to detect hyperalgesia has been used.21
Several important lessons were learned from this case. At first sight, this patient does not seem promising for a successful cartilage repair. This is due to prearthrotic deformities, such as inferior osteophytes on the humeral side as well as subchondral cysts. Furthermore, the patient is a constant smoker and manual worker with high load weight bearing during his daily activities. In spite of this, a very satisfactory result was achieved. Therefore, we should also be able to have quick and easy access to this procedure in doubtful cases, when a CAM procedure is planned.
The demonstrated procedure is fairly easy to perform for the surgeon but requires trained staff that is familiar with the technical processes. If possible, the blood sampling should be completed before the beginning of the operation in order to not prolong the surgery itself. The use of a separate butterfly needle for this step is crucial and can otherwise lead to clotted PRP, when blood is taken from larger intravenous catheter.
We anticipated problems during the “dry” part of the arthroscopy, when implanting the cartilage, but due to a separate suction (and gravity) inserted through the posterior portal, this was not an issue. The fact that the described patient had a large shoulder might have worked in our favor. Since the cartilage layer in the glenohumeral joint is comparably thin, it can be challenging to harvest enough “defect cartilage” to cover the treated area. Yet, this was not the case in this patient.
Last, as mentioned above, many shoulder patients present concomitant injuries, such as biceps tendinits, subacromial impingement or bursitis. These additional procedures have to be performed before addressing the cartilage lesion, because necessary movements in the shoulder might impair or dislocate the reconstructed area.
To summarize, single-stage arthroscopic minced cartilage procedure in the glenohumeral joint can yield excellent clinical results in the short term. Yet, larger investigations with long-term follow-up are necessary to provide reliable and extensive clinical data. So far, our knowledge on this novel surgical approach is extremely limited in general. Age limitation as well as long-term effects and benefits remain unclear for the foreseeable future.
Ethics and Consent Statements
The patient gave his written informed consent to the study and publication of this paper including all images.
No ethical approval was required. No further institutional permission was required to publish this case report and images.
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Disclosure
The authors declare that they have no conflicts of interest in this work.
References
1. Ruckstuhl H, de Bruin ED, Stussi E, Vanwanseele B. Post-traumatic glenohumeral cartilage lesions: a systematic review. BMC Musculoskelet Disord. 2008;9(1):107. doi:10.1186/1471-2474-9-107
2. Lorenz CJ, Freislederer F, Salzmann GM, Scheibel M. Minced cartilage procedure for one-stage arthroscopic repair of chondral defects at the glenohumeral joint. Arthrosc Tech. 2021;10(7):e1677–e1684. doi:10.1016/j.eats.2021.03.012
3. Gross CE, Chalmers PN, Chahal J, et al. Operative treatment of chondral defects in the glenohumeral joint. Arthroscopy. 2012;28(12):1889–1901. doi:10.1016/j.arthro.2012.03.026
4. Gartsman GM, Taverna E. The incidence of glenohumeral joint abnormalities associated with full-thickness, reparable rotator cuff tears. Arthroscopy. 1997;13(4):450–455. doi:10.1016/s0749-8063(97)90123-7
5. Paley KJ, Jobe FW, Pink MM, Kvitne RS, ElAttrache NS. Arthroscopic findings in the overhand throwing athlete: evidence for posterior internal impingement of the rotator cuff. Arthroscopy. 2000;16(1):35–40. doi:10.1016/s0749-8063(00)90125-7
6. Frank RM, Van Thiel GS, Slabaugh MA, Romeo AA, Cole BJ, Verma NN. Clinical outcomes after microfracture of the glenohumeral joint. Am J Sports Med. 2010;38(4):772–781. doi:10.1177/0363546509350304
7. Guntern DV, Pfirrmann CWA, Schmid MR, et al. Articular cartilage lesions of the glenohumeral joint: diagnostic effectiveness of MR arthrography and prevalence in patients with subacromial impingement syndrome. Radiology. 2003;226(1):165–170. doi:10.1148/radiol.2261012090
8. Carroll KW, Helms CA, Speer KP. Focal articular cartilage lesions of the superior humeral head: MR imaging findings in seven patients. AJR Am J Roentgenol. 2001;176(2):393–397. doi:10.2214/ajr.176.2.1760393
9. Bouaicha S. Shoulder cartilage regeneration: indications, possibilities, surgical implementation. Orthopade. 2017;46(11):914–918. doi:10.1007/s00132-017-3477-4
10. Cole BJ, Yanke A, Provencher MT. Nonarthroplasty alternatives for the treatment of glenohumeral arthritis. J Shoulder Elbow Surg. 2007;16(5):231. doi:10.1016/j.jse.2007.03.011
11. Green A, Norris TR. Shoulder arthroplasty for advanced glenohumeral arthritis after anterior instability repair. J Shoulder Elbow Surg. 2001;10(6):539–545. doi:10.1067/mse.2001.118007
12. Saltzman BM, Leroux T, Cole BJ. Management and surgical options for articular defects in the shoulder. Clin Sports Med. 2017;36(3):549–572. doi:10.1016/j.csm.2017.02.009
13. Millett PJ, Horan MP, Pennock AT, Rios D. Comprehensive Arthroscopic Management (CAM) procedure: clinical results of a joint-preserving arthroscopic treatment for young, active patients with advanced shoulder osteoarthritis. Arthroscopy. 2013;29(3):440–448. doi:10.1016/j.arthro.2012.10.028
14. Albrecht FH. Closure of joint cartilage defects using cartilage fragments and fibrin glue. Fortschr Med. 1983;101(37):1650–1652.
15. Salzmann GM, Ossendorff R, Gilat R, Cole BJ. Autologous minced cartilage implantation for treatment of chondral and osteochondral lesions in the knee joint: an overview. Cartilage. 2021;13(1_suppl):1124S–1136S. doi:10.1177/1947603520942952
16. Samilson RL, Prieto V. Dislocation arthropathy of the shoulder. J Bone Joint Surg Am. 1983;65(4):456–460.
17. Fox JA, Cole BJ, Romeo AA, et al. Articular cartilage thickness of the humeral head: an anatomic study. Orthopedics. 2008;31(3):216–311. doi:10.3928/01477447-20080301-11
18. Dominguez Perez JM, Fernandez-Sarmiento JA, Aguilar Garcia D, et al. Cartilage regeneration using a novel autologous growth factors-based matrix for full-thickness defects in sheep. Knee Surg Sports Traumatol Arthrosc. 2019;27(3):950–961. doi:10.1007/s00167-018-5107-z
19. Millett PJ, Huffard BH, Horan MP, Hawkins RJ, Steadman JR. Outcomes of full-thickness articular cartilage injuries of the shoulder treated with microfracture. Arthroscopy. 2009;25(8):856–863. doi:10.1016/j.arthro.2009.02.009
20. Boehm E, Minkus M, Scheibel M. Autologous chondrocyte implantation for treatment of focal articular cartilage defects of the humeral head. J Shoulder Elbow Surg. 2020;29(1):2–11. doi:10.1016/j.jse.2019.07.030
21. Calvo Lobo C, Romero Morales C, Rodriguez Sanz D, et al. Comparison of hand grip strength and upper limb pressure pain threshold between older adults with or without non-specific shoulder pain. PeerJ. 2017;5:e2995. doi:10.7717/peerj.2995
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
