Back to Journals » Journal of Experimental Pharmacology » Volume 15
Anti-Hyperglycemic and Hypoglycemic Activities of 80% Methanol Extract and Solvent Fractions of Ocimum lamiifolium Hochst Ex Benth. (Lamiaceae) Leaves in Mice
Authors Tesfaye T , Teka F, Duga G , Obsa T , Dereje B , Makonnen E
Received 24 February 2023
Accepted for publication 1 June 2023
Published 6 June 2023 Volume 2023:15 Pages 255—266
DOI https://doi.org/10.2147/JEP.S409997
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Roger Pinder
Tilahun Tesfaye,1,2 Firehiwot Teka,3 Gudeta Duga,2 Temesgen Obsa,4 Beyene Dereje,5 Eyasu Makonnen1,6
1Department of Pharmacology and Clinical Pharmacy, School of Pharmacy, College of Health Science, Addis Ababa University, Addis Ababa, Ethiopia; 2Department of Pharmacy, College of Medicine and Health Science, Ambo University, Ambo, Ethiopia; 3Department of Traditional and Modern Medicine Research Directorate, Ethiopian Public Health Institute, Addis Ababa, Ethiopia; 4Department of Pharmacology, School of Pharmacy, College of Medicine and Health Science, Jigjiga University, Jigjiga, Ethiopia; 5Department of Pharmacology, School of Medicine, College of Medicine and Health Science, Dire Dawa University, Dire Dawa, Ethiopia; 6Center for Innovative Drug Development and Therapeutic Trials for Africa (CDT-Africa), Addis Ababa University, Addis Ababa, Ethiopia
Correspondence: Tilahun Tesfaye, Email [email protected]
Background: Globally, the prevalence of diabetes mellitus is rising. Due to the scarcity, high cost, and many adverse effects of modern treatments, traditional medicine is commonly used in rural areas to treat a variety of illnesses, including diabetes mellitus. The aim of this study was to assess the antihyperglycemic and hypoglycemic effects of Ocimum lamiifolium Hochst ex Benth leaves.
Methods: A crude methanol 80% extract’s and its solvent fractions’ effects on healthy, oral glucose-given, and STZ-induced diabetic mice were examined. Swiss albino mice of either sex were assigned into sixteen groups, each containing six mice, for the OGTT and hypoglycemia tests. Male mice were used in the study, and they were divided into groups for the negative control (citrate buffer for diabetic mice), the normal control (Tween 2%), the test groups, and a positive control (glibenclamide) for the antihyperglycemic test in STZ (200 mg/kg body weight)-induced diabetic mice.
Results: A crude 80% methanol extract of 200 mg/kg effectively lowered blood glucose levels (p < 0.05) and none of the fractions extracts caused hypoglycemia shock in norma mice. The aqueous residue at 100, 200, and 400 mg/kg, the n-butanol fraction at 100 and 200 mg/kg, and the chloroform fraction at 200 mg/kg demonstrated higher glucose tolerance in orally glucose-loaded mice (p < 0.05). The crude 400 mg/kg of an 80% methanol extract, 100 and 200 mg/kg of the n-butanol fraction, 200 and 400 mg/kg of the chloroform fraction, and 5 mg/kg of glibenclamide significantly reduced blood glucose levels in STZ-induced diabetic mice (p < 0.05).
Conclusion: The current research demonstrates that a crude 80% methanol extract of Ocimum lamiifolium Hochst ex Benth leaves, as well as its solvent fractions, significantly reduce blood sugar levels in mice that are healthy, loaded with glucose, and streptozotocin induced diabetic mice.
Keywords: blood glucose, diabetes mellitus, glibenclamide, hyperglycemia, Ocimum lamiifolium, oral glucose tolerance test, streptozotocin
Introduction
Diabetes mellitus is a serious, complex, and heterogeneous metabolic disorder that has been proved to be a non-curable but controllable chronic burden, with its prevalence increasing worldwide. It is characterized by periods of hyperglycemia and glucose intolerance that impair the ability of cells to secrete insulin or cause tissues to become less sensitive to insulin.1–3 An absolute or relative lack of the hormone Insulin causes the illness to show symptoms and signs of osmotic diuresis, such as polyuria, polydipsia, weight loss, calorie loss, generalized weakness, and polyphagia.4,5
Over long-term diabetes, Mellitus progresses to micro- and macrovascular complications, which damage both small and large blood vessels, respectively.6 According to the American Diabetes Association,7 Type 1 diabetes, Type 2 diabetes, gestational diabetes mellitus, and specific types of diabetes resulting from other causes are the four different types or classifications of diabetes mellitus. According to the International Diabetes Federation (IDF), there were 415 million cases of diabetes among individuals’ aged 20 to 79 in 220 countries in 2015. The number of cases is predicted to rise to 693 million by the year 2045, from 642 million in 2040 G.C.8,9 Ethiopia has the highest diabetes prevalence in sub-Saharan Africa, with 2.57 million (5.2% of adults aged 20 to 79) having the disease, according to the IDF’s 2017 estimate. About 1.96 million (76%) of them do not even realize they have diabetes.10
The etiologies of diabetes mellitus are a composite of immunologic, environmental, and genetic factors.11,12 With no known cure and a steadily growing worldwide prevalence, there are conventional anti-diabetic drugs. However, studies showed these drugs have problems associated with adverse effects, availability, and affordability, which calls for looking for new alternatives from medicinal plants, one of which is the Ocimum species.13–15
Ocimum is one of the largest genera in the Lamiaceae family, with over 150 species.16 It has been reported that O. campechianum has an antidiabetic effect in Trinidad and Tobago; O. canum, O. gratissimum, O. sanctum, and O. tenuiflorum have antihyperglycemic activity.17 Ocimum lamiifolium Hochst ex Benth is native to Ethiopia, where it is known as “dama-kassie” (in Amharic) and “anchabi” (in Afan Oromo). It is a 0.7 to 3 meter tall erect, highly branching subshrub or shrub with an indumentum of simple hairs. It is an evergreen perennial shrub with oppositely oriented, pubescent petiolate leaves (0.5–5 mm), thin at the base, and highly serrated leaf surfaces. Pinkish blooms are borne in racemes. It grows in gardens, along roads and streams, on bush area, on the edges of woods, and on grassland between 1200 and 2900 meters above sea level.16,18
Terpenoids, flavonoids, saponins, tannins, and steroids were found in ethanol extracts of Ocimum lamiifolium leaves during phytochemical study. O. lamiifolium is a common aroma-containing genus (family Lamiaceae) with a wide range of essential oils known for their therapeutic properties. Anti-stress, diaphoretic, diuretic, anti-pyretic, stomachache, anti-microbial, insecticidal, fungicidal, mosquito repellent, anti-aging, anti-cancer, anti-inflammatory, anti-atherosclerosis, anti-apoptosis, anti-oxidants, hypoglycemia, and other properties have been demonstrated for essential oils. It is found throughout the tropics.19,20 The current study sought to assess the antihyperglycemic and hypoglycemic properties in mice of a crude 80% methanol extract of Ocimum lamiifolium Hochst ex Benth leaf and its solvent fractions.
Materials and Methods
Animals
Swiss albino mice, males (20–35 g, 6–8 weeks old), were used for pharmacologic evaluations, while either sexes of the same weight and age were used for hypoglycemic effect and OGT tests. Mice were obtained from the animal house of the School of Pharmacy, the College of Health Sciences, Addis Ababa University, and the Ethiopian Public Health Institute (EPHI). Each animal utilized in this study received a regular pellet diet in addition to unlimited access to water. Animals were kept and cared for in a lab environment with a temperature of 22 ± 3 °C, the optimum humidity level, and a 12 hour dark and 12 hour light cycle.21
Plant Materials
Fresh leaves of Ocimum lamiifolium were collected in January 2020 from Ejere district, West Shoa zone, Oromia region, and EPHI. Samples of plant material were deposited in the national herbarium at the College of Natural and Computational Science, Addis Ababa University, after the leaves were identified and voucher number TT-001 was given by a botanist. Green leaves were then dried in the room at room temperature, away from direct sunlight. The dried leaves were ground manually into a fine powder using a traditional mortar and pestle called Mawkecha in Amharic. The powdered plant components were weighed before being stored at room temperature in dry, airtight plastic bags.
Equipment
Rotary vapor (BUCHI rotary vapor R-200 Switzerland), vacuum (BUCHI vac®-500 Switzerland), Erlenmeyer conical round-bottomed flask, biker, Separatory funnel, funnel (Griffin Germany), oven, analytical balance, refrigerator, Insulin syringe, gloves, plastic container, filter paper, lyophilizer (OPERON OPR-FDU-5012 KOREA), cotton cloth, nylon cloth, Whatman No. 1 filter paper, aluminum foil, mortar and pestle, measuring cylinder, stirrer, one touch A glucometer and blood glucose strip (Precisa) were employed for the experiments.
Drugs and Chemicals
Streptozotocin (Sigma Aldrich Germany), Chloroform (99.8%, Carlo Erba Reagent), n-Butanol (99%, Loba Chemistry Pvt. Ltd.), Citric acid anhydrous C6H8O7 (Sigma Aldrich Germany), and Sodium Citrate (C6H5Na3O7.2H2O) are used. In this investigation, distilled water, Tween 80% (Sigma Aldrich Germany), glucose powder, and Glibenclamide 5 mg (Reyoung Pharmaceutical Co., Ltd.) were also used.
Methanol 80% Extract Preparation
Techniques of cold method (maceration) extraction were used for the preparation of an 80% methanol crude extract. The 911.39 g of powdered leaves of Ocimum lamiifolium were soaked in 80% methanol (v/v) (air-dried leaf mixed with 80% methanol) for three consecutive days in an Erlenmeyer conical flask with occasional manual shaking every 30 minutes during the day. A one-to-five (1:5) solid-to-solvent ratio was used for maceration. The filtrates were then combined and filtered using Whatman No. 1 filter paper using a vacuum-pressurized suction filtration system after being filtered by folded cotton and nylon fabric. To effectively extract the plant material, the marc was re-macerated twice using extra-fresh 80% methanol. The methanol was then recovered from the extract by evaporating it under vacuum using Rota Vapor at 40 °C. The filtrates were then maintained in a deep freezer and lyophilized to remove the water.21,22
Solvent Fractionation
The crude 80% methanol extract of dried leaves of Ocimum lamiifolium was fractionated with different solvents based on polarity index using a separatory funnel, resulting in chloroform and n-butanol fractions as well as aqueous residue. One hundred grams (100g) of crude methanol extract were taken and dissolved in 150 mL of distilled water. Then an equal amount of chloroform (150 mL) was added to it and shook gently, and pressure was released intermittently. This formed two layers; as chloroform is denser, it remained at the bottom and eluded first. The process was repeated over and over until a clear layer was obtained between chloroform and aqueous residue. The extract was then sequentially fractionated using the same volume (150 mL) of n-butanol until the extracting solvents were colorless. The solvents were recovered by Rota Vapor from the chloroform and butanol fractions after the fractionation process was complete. The n-butanol fraction and aqueous residue are separated and dried using a lyophilizer, while the chloroform fraction is dried in an oven at a low temperature. The dried extracts were then placed in different vials and kept in the refrigerator until used.21,23
Induction of Diabetes
A highly selective pancreatic beta cell cytotoxic drug called streptozotocin (STZ) results in full beta cell necrosis and induces diabetes within 48 hours. On day 1, 4 hours prior to STZ administration, ad libitum was removed from all cages and only water was provided. STZ was dissolved in sodium citrate buffer, adjusted at pH 4.5, to a final concentration of 0.1M. Immediately after preparation, the STZ solution was injected i.p. into the mice at a dose of 200 mg/kg. Mice were then provided with food and a 5% glucose solution 6 hours after the administration of STZ for the next 24 hours to prevent death secondary to hypoglycemic shock. After 72 hours, mice with a fasting blood glucose level >200 mg/dL were considered diabetic and included in the study. Then they were randomly divided into different groups, and the bedding of the cages was changed every day to maintain the dryness of the cages for polyuric diabetic mice.24,25
Grouping and Dosing of Animals
A hypoglycemic and oral glucose tolerance test study was done on ninety-six mice. For hypoglycemic and oral glucose tolerance tests, mice of either sex were divided into sixteen groups (each group contains six mice). Male mice were used for diabetic models as female mice are less sensitive to streptozotocin and insulin compared to male animals. Diabetic mice were randomly divided into eighteen groups (six mice per group). Group I (diabetic mice as a negative control) received 10 mL/kg of citrate buffer, Group II received Tween 2% in 10 mL/kg, and Group III (as a positive control) received 5 mg/kg of glibenclamide. Group IV–XVIII was treated with different doses of crude extract and fractions (aqueous residue, n-butanol, and chloroform). Controls were separate for all models. Extracts and fractions were administered at doses of 100, 200, and 400 mg/kg, respectively.
Blood Collection and Blood Glucose Level Determination
A mouse tail vein was punctured aseptically with scissors to obtain a blood sample, and the glucose levels were assessed by a blood glucose meter (Precisa), and results are expressed as mg/dL.21,25
Hypoglycemic Effect of Methanol Extracts of O. lamiifolium Leaves and Fractions
Animals were weighed and sorted into sixteen groups, and their respective doses were computed. In comparison to the negative and positive groups, the hypoglycemic effects of plant extracts such as crude 80% methanol (v/v), chloroform fraction, n-butanol fraction, and aqueous residual delivered orally after fasting for six hours were studied in groups of normoglycemic mice. Blood was extracted from the mouse tail veins using a blood glucose strip after an aseptic cut was made with scissors. Blood sugar levels were measured using a glucometer prior to treatments (0 minutes), as well as 1, 2, 3, and 4 hours afterwards.
Oral Glucose Tolerance Test
On mice that had fasted the night before, an oral glucose tolerance test was performed. Mice of either sex were randomly divided into sixteen groups. Tween 2%, glibenclamide, and extracts/fractions were administered to the negative control, positive control, and test groups, respectively. 30 minutes after each treatment, 2 g/kg of glucose solution was administered orally. At 30, 60, and 120 minutes, blood samples were obtained aseptically from the mouse tails.25
Antihyperglycemic Activity of O. lamiifolium Leaf in Diabetic Mice
After 14 hours of overnight fasting, blood was obtained from STZ-induced diabetic mice at 0 hours (immediately before treatment), 1, 2, 3, and 4 hours of therapy.26
Ethical Consideration
Prior to its execution, the study obtained ethical approval from the Ethiopian Public Health Institute and School of Pharmacy, College of Health Sciences, Addis Ababa University, IRB (P.N.: ERB/SOP/200/12/2019). The animals were housed in cages in an animal home that had a 12-hour light/dark cycle. They were fed normal pellets and water on an ad libitum basis. Prior to the experiments, the mice were acclimatized to the laboratory environment for one week. All investigations were conducted in a quiet laboratory setting. The investigations were carried out in line with the Laboratory Animal Care and Use Handbook.
Statistical Analysis
The results were presented as a mean ± S.E.M. The statistical differences between the treatments and the controls were analyzed using one-way analysis of variance (ANOVA), followed by multiple comparison posthoc tests using SPSS version 25. A difference between the mean values (p<0.05) was considered to be statistically significant.
Results
Crude Extracts and Fraction Yields
The yield from 910.39 g of O. lamiifolium leaf powder was 171.49 g (18.82%). Aqueous residue, n-butanol fractions, and chloroform fractions yielded yields of 57.14%, 28.41%, and 12.34%, respectively, from the 100 g fractionated.
Hypoglycemic Effect of Crude 80% Methanol Extract of O. lamiifolium Leaves
At 1 hour, glibenclamide 5 mg/kg significantly (p<0.05) reduced blood glucose levels compared to a crude 80% methanolic extract of 400 mg/kg, as shown in Table 1. During the second and third hours, the crude 80% methanol extract at 200 mg/kg showed a significant reduction in blood glucose level comparable to that of the 400 mg/kg crude 80% methanol extract (p<0.05). The crude 80% methanol extract at 400 mg/kg reduced blood glucose levels the most (34.19%), followed by glibenclamide 5 mg (27.25%) (Figure 1).
 |
Table 1 Hypoglycemic Effect of Crude 80% Methanol Extract of Ocimum lamiifolium Leaves in Normoglycemic Mice |
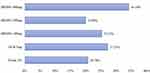 |
Figure 1 % reduction of blood glucose level by 80% methanol extract of Ocimum lamiifolium leaves in normoglycemic mice. |
Hypoglycemic Effect of Fractions of Methanolic Extracts of O. lamiifolium Leaves
The results of the hypoglycemic evaluation of solvent fractions are summarized in Table 2. One hour after treatment with aqueous residue (200–400 mg/kg) and n-butanol fraction (100–400 mg/kg), blood glucose levels were significantly reduced (p<0.01). At 2 hours, the n-butanol fraction of 100 mg/kg reduced blood glucose levels more significantly than the aqueous residue (p<0.01). Aqueous residue (200 mg/kg, 400 mg/kg) and n-butanol fraction (200 mg/kg) showed a significant reduction in blood glucose level at the third hour after treatment (p<0.01). Glibenclamide had the greatest effect on blood glucose levels (47.71%), followed by aqueous residue 400 mg/kg (29.32%) (Figure 2).
 |
Table 2 Hypoglycemic Effect of Fractions of 80% Methanol Extract of Ocimum lamiifolium Leaves in Normoglycemic Mice |
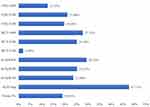 |
Figure 2 % reduction of blood glucose level by solvent fractions of Ocimum lamiifolium leaves in normoglycemic mice. |
Antihyperglycemic Effect of Crude O. lamiifolium Extracts in Glucose Loaded Mice
Peak blood glucose levels were detected 30 minutes after orally loading glucose, indicating the induction of hyperglycemia. In 0.5 hours, 400 mg/kg of methanol 80% extract produced the highest blood glucose level. At all times after therapy, glibenclamide 5 mg/kg significantly (p<0.05) reduced hyperglycemia. At 2 hours, 200 mg/kg of an 80% methanol extract produced the highest glucose tolerance. Blood glucose levels were lowered the highest by standard medications (63.95%), followed by 80% methanol 200 mg/kg extracts (46.82%) (Figure 3).
 |
Figure 3 % reduction of blood glucose level by 80% methanol extracts of Ocimum lamiifolium leaves in glucose loaded mice. |
Antihyperglycemic Effects of Solvent Fractions in Glucose Loaded Mice
At 0.5 hours, 200 mg/kg aqueous residue and 400 mg/kg chloroform fraction showed significant glucose tolerance (p<0.05). At 1 hour, aqueous residue (100, 200 mg/kg) resisted glucose loading significantly (p<0.05). Aqueous residues (100 and 400 mg/kg), butanol fractions (100 and 200 mg/kg), and chloroform fractions (200 mg/kg) tolerated glucose loading significantly at 2 hours (p<0.05) (Figure 4).
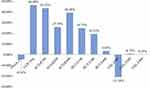 |
Figure 4 % reduction of blood glucose level by solvent fractions of Ocimum lamiifolium leaves in glucose loaded mice. |
Ant Hyperglycemic Effect of 80% Methanol Extract of O. lamiifolium Leaves in STZ Induced Diabetic Mice
At zero hour, the blood glucose level of all STZ groups was significantly higher than that of the normal control group. The results are summarized in Table 3. At 1 hour, standard drug controlled blood glucose level significantly compared to crude methanol 80% 200 mg/kg and negative control (p<0.05), while 80% methanol extract 400 mg/kg reduced blood glucose level significantly at the 2nd, 3rd, and 4th hours (p<0.05). Maximum reduction in blood glucose level was observed with the standard drug Glibenclamide at 5 mg/kg, accounting for a 68.47% reduction, followed by 400 mg/kg of 80% methanol extract (63.53%) and 100 mg/kg (55.58%) (Figure 5).
 |
Table 3 Crude Ocimum lamiifolium Leaf Extracts Effect in STZ-Induced Diabetic Mice |
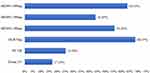 |
Figure 5 % reduction of blood glucose level by 80% methanol extracts of Ocimum lamiifolium leaves in STZ-induced diabetic mice. |
Antihyperglycemic Effect of Solvent Fractions of Ocimum lamiifolium Extracts in STZ Induced Diabetic Mice
At the 1st hour, 200 and 400 mg/kg of chloroform fractions and 5 mg/kg of glibenclamide significantly reduced the blood glucose level (p<0.01) and continued to reduce the blood glucose level at the 2nd hour (p<0.05). At the 3rd hour, glibenclamide, chloroform fractions (200 and 400 mg/kg), and n-butanol fractions (100 and 200 mg/kg) significantly (p<0.05) reduced the blood glucose level. At the final 4th hour, glibenclamide and chloroform fraction at 200 mg/kg significantly (p<0.01) controlled blood glucose levels. Glibenclamide reduced blood glucose levels the most (76.75%), followed by 200 mg/kg chloroform fraction (51.67%) (Table 4 and Figure 6).
 |
Table 4 Effect of Solvent Fractions of Ocimum lamiifolium Leaves on Blood Glucose Level in STZ-Induced Diabetic Mice |
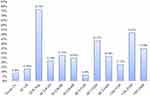 |
Figure 6 Percentage reduction of blood glucose level by solvent fraction of Ocimum lamiifolium leaves in STZ-induced diabetic mice. |
Discussion
This study investigated at the antihyperglycemic and hypoglycemic effects of an 80% methanol extract of O. lamiifolium leaves and its solvent fraction in mice. In normoglycemic, glucose-loaded, and diabetic mice, both the 80% methanol extracts and the solvent fractions shown promising efficacy. STZ-induced diabetic mice had significantly higher blood glucose levels (>200 mg/dl) than normal control mice 72 hours after receiving a single high dose (200 mg/kg) of STZ. Some investigations found that intraperitoneal treatment of STZ at a dose of 150–200 mg/kg permanently produced type I diabetic mellitus in mice.25 To test hypoglycemic activity, normoglycemic mice of both sexes were given different doses (100 mg/kg, 200 mg/kg, and 400 mg/kg) of 80% methanol extracts of O. lamiifolium leaves and its solvent fractions (aqueous residue, butanol fraction, and chloroform fraction) orally for 0, 1, 2, 3, and 4 hours.
The hypoglycemic activity test in normoglycemic mice is intended to determine whether plant extracts cause hypoglycemia, a common side effect of diabetes medication, as well as whether the plants have blood glucose-lowering capabilities. Animals given a crude 80% methanol extract, aqueous residual, or the n-butanol fraction showed considerably decreased blood glucose levels over time. A blood glucose level of less than 70 mg/dL is considered hypoglycemia. Hence, when compared to other groups, Ocimum lamiifolium leaf extracts and fractions showed a modest hypoglycemic effect, with mild hypoglycemia defined as a blood glucose level in rodents between 60 and 80 mg/dL.27
At the studied dose, the plant extracts have a lower risk of hypoglycemic shock, since severe and marked hypoglycemia are characterized in rodents as blood glucose levels less than 40 mg/dL and 40 to 60 mg/dL, respectively.27,28 Because the 80% methanol extract contains a high concentration of tannins, saponins, steroids, terpenoids, flavonoids, and phenols, it may have antioxidant properties, hypoglycemic activity, and insulin-like effects that contribute to the significant reduction in blood glucose levels observed with these extracts.22 The hypoglycemic activity in fractions is caused by medium-polarity phytochemicals such tannins, saponins, phenols, and steroids, whereas the hypoglycemic activity in crude extracts is caused by flavonoids, tannins, and phenols.
The oral glucose tolerance test (OGTT) is a standard procedure that measures the clearance of an oral glucose load from the body or how quickly exogenous glucose can be cleared from the blood and is used in diagnosing diabetes mellitus.29,30 It is also used to track the temporal changes in blood glucose levels in response to an oral glucose challenge.31 In this study, crude methanol (80%, 400 mg/kg), aqueous residue (100, 200, 400 mg/kg), n-Butanol fraction (100, 200 mg/kg), and chloroform fraction (100, 200, 400 mg/kg) significantly tolerated glucose loading (P <0.05). A significant reduction in blood glucose level might be due to different secondary metabolites present in crude extract and fractions.
Secondary metabolites are thought to improve regulatory systems by an insulin-like action, most likely by increasing -cell glucose sensitivity or peripheral glucose consumption. Qualitative A phytochemical screening of an Ocimum lamiifolium aqueous leaf extract found that it included hypoglycemic sterols, terpenoids, flavonoids, tannins, and saponins that could act synergistically or independently to improve its efficiency.18 The methanol extract may also include the same secondary metabolites, though at different amounts.
STZ induces diabetes by entering pancreatic cells through the GLUT2 transporter and accumulates alkylating products intracellularly, causing beta cell death by alkylating DNA within these cells. STZ is a nitric oxide donor that generates free radicals like superoxide, which induces hydrogen peroxidase and hydroxyl-induced DNA damage by interfering with ATP synthesis in the mitochondria. This DNA damage decreases ATP, which causes beta cells to produce less insulin and secrete less insulin. As a result of the subsequent glucose overload, PKC pathways are activated, resulting in downstream glycation products that induce further oxidative stress, cell apoptosis, necrosis, and DNA damage.32,33
Increased free radical production and oxidative stress have been identified as crucial events in the development of diabetes and its effects. As a result, consuming antioxidants reduces oxidative stress and helps diabetics.34 Mice were fasted prior to receiving STZ injections because glucose can compete with STZ in a fed state, making fasted animals more sensitive to this chemical.32 Crude 80% methanol extract and its solvent fractions reduced blood glucose levels in STZ-induced animals in a manner comparable to those of normoglycemic mice. Ocimum lamiifolium leaves’ antihyperglycemic activity shows that STZ (200 mg/Kg) may not completely destroy the -cells, resulting in insulin release from undamaged -cells via active components present in Ocimum lamiifolium leaves.
Diabetes makes beta cells more vulnerable to free-radical or cytokine-induced damage.12,35 Leaf flavonoids suppress ROS synthesis by inhibiting enzymes or chelating trace elements involved in free radical formation, as well as by strengthening the antioxidant defense system.36 Saponins from Ocimum lamiifolium may also have regulated blood glucose levels in diabetic rats, either by stimulating beta cells or by suppressing glucose transfer from the stomach to the small intestine and blocking glucose transport over the brush border of the small intestine.37
Tannins, on the other hand, have an anti-diabetic effect by delaying intestinal glucose absorption and having an insulin-like effect on insulin-sensitive tissues, delaying the onset of insulin-dependent diabetes mellitus by regulating the pancreatic antioxidant environment and inhibiting amylase and glucose synthase activity.38 Low- and medium-polarity solvents like chloroform and n-butanol help extract phytochemical components like flavonoids, tannins, and steroids.22
Conclusion
The findings of the present study indicate that the crude 80% methanol extract of Ocimum lamiifolium Hochst ex Benth leaves and its solvent fractions have dose-dependent hypoglycemic and antihyperglycemic effects on normal, glucose-loaded, and streptozotocin-induced diabetic mice, which can be attributed to the secondary metabolites present in the extract and solvent fraction.
Abbreviations
DM, Diabetes Mellitus; DKA, Diabetic Keto Acidosis; GAD, Glutamic Acid Decarboxylase; GLP, Glucagon like Peptide; IDF, International Diabetic Federation; IGT, Impaired Glucose Tolerance; IR, Insulin Resistance; STZ, Streptozotocin; T1DM, Type one Diabetes Mellitus; T2DM, Type two Diabetes mellitus; GLUT2, Glucose Transport Two.
Data Sharing Statement
The datasets created and analyzed during the current investigation are available upon reasonable request from the corresponding author.
Acknowledgment
We would like to thank Addis Ababa University, the Center for Innovative Drug Development and Therapeutic Trials for Africa (CDT-Africa), and the Ethiopian Public Health Institute (EPHI) for supporting the present study.
Author Contributions
All authors contributed to data analysis, drafted or revised the article, agreed on the journal to which the article will be submitted, gave final approval of the version to be published, and agreed to be accountable for all aspects of the work. TT, EM, BD, GD and TO conceptualized the study and contributed to the original idea. TT, EM and FT carried out the experiments. TT, EM and BD, drafted the manuscript. GD, FT and TO participated in drafting the manuscript. TT, FT and EM recorded the data related experiments. TT, EM and BD, performed data analysis and drafted the results. BD, GD, FT and TO critically reviewed and edited the manuscript. TT and EM oversaw the entire project, from survey tool development to data analysis. The final manuscript was reviewed, read, and approved by all of the authors.
Funding
The study was funded by Department of Pharmacology and Clinical Pharmacy, School of Pharmacy, College of Health Science, Addis Ababa University.
Disclosure
The authors declare that they do not have any conflicts of interest.
References
1. Sapra A, Bhandari P. Diabetes Mellitus - StatPearls - NCBI Bookshelf. StarPearls Publication; 2022.
2. Eberle C, Stichling S. Effect of telemetric interventions on glycated hemoglobin A1c and management of type 2 diabetes mellitus: systematic meta-review. J Med Internet Res. 2021;23:1–14.
3. Iatcu CO, Steen A, Covasa M. Gut microbiota and complications of type-2 diabetes. Nutrients. 2022;14. doi:10.3390/nu14010166
4. Meresa A, Gemechu W, Basha H, et al. Herbal medicines for the management of diabetic mellitus in Ethiopia and Eritrea including their phytochemical constituents. Am J Adv Drug Deliv. 2017;01:040–058.
5. Piero MN. Diabetes mellitus – a devastating metabolic disorder. Asian J Biomed Pharm Sci. 2015;4:1–7. doi:10.15272/ajbps.v4i40.645
6. Saberzadeh-Ardestani B, Karamzadeh R, Basiri M, et al. Type 1 diabetes mellitus: cellular and molecular pathophysiology at a glance. Cell J. 2018;20:294–301. doi:10.22074/cellj.2018.5513
7. American Diabetes Association. 2. Classification and diagnosis of diabetes: standards of medical care in diabetes-2021. Diabetes Care. 2021;44:S15–S33.
8. Cho NH, Shaw JE, Karuranga S, et al. IDF Diabetes Atlas: global estimates of diabetes prevalence for 2017 and projections for 2045. Diabetes Res Clin Pract. 2018;138:271–281. doi:10.1016/j.diabres.2018.02.023
9. Ogurtsova K, da Rocha Fernandes JD, Huang Y, et al. IDF diabetes atlas: global estimates for the prevalence of diabetes for 2015 and 2040. Diabetes Res Clin Pract. 2017;128:40–50. doi:10.1016/j.diabres.2017.03.024
10. Bishu KG, Jenkins C, Yebyo HG, et al. Diabetes in Ethiopia: a systematic review of prevalence, risk factors, complications, and cost. Obes Med. 2019;15:100132. doi:10.1016/j.obmed.2019.100132
11. Paschou SA, Papadopoulou-Marketou N, Chrousos GP, et al. On type 1 diabetes mellitus pathogenesis. Endocr Connect. 2018;7:R38–R46. doi:10.1530/EC-17-0347
12. Thomassian B. Diabetes Mellitus: Pathophysiology and Clinical Guidelines. The Academy of Dental Learning and OSHA Training; 2017.
13. Ingle PV, Yin SB, Ying BJ, et al. Current trends in pharmacological treatment of type II diabetes mellitus. Int J Pharmacol Res Rev. 2018;7:1–15.
14. Padhi S, Nayak AK, Behera A. Type II diabetes mellitus: a review on recent drug based therapeutics. Biomed Pharmacother. 2020;131:110708. doi:10.1016/j.biopha.2020.110708
15. Model C. Standards of medical care in diabetes-2019. Diabetes Care. 2018;42:1–24.
16. Getasetegn M, Tefera Y. Biological activities and valuable compounds from five medicinal plants. Nat Prod Chem Res. 2016;4:220–230. doi:10.4172/2329-6836.1000220
17. Salehi B, Ata A, Anil Kumar NV, et al. Antidiabetic potential of medicinal plants and their active components. Biomolecules. 2019;9. doi:10.3390/biom9100551
18. Arika WM, Rachuonyo HO. Hypoglycemic effect of Ocimum lamiifolium in Alloxan induced diabetic mice. Med Aromat Plants. 2016;5:1–5. doi:10.4172/2167-0412.1000228
19. Bhasin M. Ocimum - Taxonomy, medicinal potentialities and economic value of essential oil. J Biosph. 2012;1:48–50.
20. Kifle H, Seyoum A, Asres K, et al. Composition, antimicrobial and free-radical scavenging properties of the essential oil of Damakese (Ocimum lamiifolium): a popular home remedy in Ethiopia. Int J Essent Oil Ther. 2007;1:110–116.
21. Nardos A, Makonnen E, Debella A. Effects of crude extracts and fractions of moringa stenopetala (Baker f) cufodontis leaves in normoglycemic and alloxan-induced diabetic mice. Afr J Pharm Pharmacol. 2011;5:2220–2225.
22. Sahalie NA, Abrha LH, Tolesa LD. Chemical composition and antimicrobial activity of leave extract of Ocimum lamiifolium (Damakese) as a treatment for urinary tract infection. Cogent Chem. 2018;4:1440894. doi:10.1080/23312009.2018.1440894
23. Dinku T, Tadesse S, Asres K. Antidiabetic activity of the leaf extracts of pentas schimperiana Subsp. schimperiana (A. Rich) Vatke on Alloxan-induced diabetic mice. Ethiop Pharm J. 2011;28:12–20.
24. Belayneh YM, Birru EM, Ambikar D. Evaluation of hypoglycemic, antihyperglycemic and antihyperlipidemic activities of 80% methanolic seed extract of Calpurnia aurea (Ait.) Benth. (Fabaceae) in mice. J Exp Pharmacol. 2019;11:73–83. doi:10.2147/JEP.S212206
25. Furman BL. Streptozotocin-induced diabetic models in mice and rats. Curr Protoc. 2021;1:1–21.
26. Ayele AG, Kumar P, Engidawork E. Antihyperglycemic and hypoglycemic activities of the aqueous leaf extract of Rubus Erlangeri Engl (Rosacea) in mice. Metab Open. 2021;11:100–118. doi:10.1016/j.metop.2021.100118
27. Grant CW, Duclos SK, Moran-Paul CM, et al. Comparative medicine development of standardized insulin treatment protocols for spontaneous rodent models of type 1 diabetes. Comp Med. 2012;62:381–390.
28. Kirilmaz OB, Salegaonkar AR, Shiau J, et al. Study of blood glucose and insulin infusion rate in real-time in diabetic rats using an artificial pancreas system. PLoS One. 2021;16:1–19. doi:10.1371/journal.pone.0254718
29. Müller-Wieland PD, Nauck M, Petersmann A, et al. Definition, classification and diagnosis of diabetes mellitus. Diabetologe. 2019;15:128–134. doi:10.1007/s11428-019-0460-1
30. Andrikopoulos S, Blair AR, Deluca N, et al. Evaluating the glucose tolerance test in mice. Am J Physiol. 2008;295:1323–1332.
31. Rozman J, Rathkolb B, Neschen S, et al. Glucose tolerance tests for systematic screening of glucose homeostasis in mice. Curr Protoc Mouse Biol. 2015;5:65–84. doi:10.1002/9780470942390.mo140111
32. Goyal SN, Reddy NM, Patil KR, et al. Challenges and issues with streptozotocin-induced diabetes - A clinically relevant animal model to understand the diabetes pathogenesis and evaluate therapeutics. Chem Biol Interact. 2016;244:49–63. doi:10.1016/j.cbi.2015.11.032
33. King A, Austin A. Animal Models of Type 1 and Type 2 Diabetes Mellitus.
34. Giacco F, Brownlee M. Oxidative stress and diabetic complications. Circ Res. 2010;107:1058–1070. doi:10.1161/CIRCRESAHA.110.223545
35. Skyler JS, Bakris GL, Bonifacio E, et al. Differentiation of diabetes by pathophysiology, natural history, and prognosis. Diabetes. 2017;66:241–255. doi:10.2337/db16-0806
36. Kumar S, Pandey AK. Chemistry and biological activities of flavonoids: an overview. Sci World J. 2013;2013:16. doi:10.1155/2013/162750
37. Desai SD, Desai DG, Kaur H. Saponins and their biological activities. Pharma Times. 2009;41:13–16.
38. Sieniawska E. Activities of tannins-from in vitro studies to clinical trials. Nat Prod Commun. 2015;10:1877–1884.
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
