Back to Journals » International Journal of Women's Health » Volume 16
Antenatal Care Practices: A Population-Based Multicenter Study from Saudi Arabia
Authors Alqifari SF
Received 2 December 2023
Accepted for publication 25 February 2024
Published 1 March 2024 Volume 2024:16 Pages 331—343
DOI https://doi.org/10.2147/IJWH.S452934
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Professor Elie Al-Chaer
Saleh F Alqifari
Pharmacy Practice Department, Faculty of Pharmacy, University of Tabuk, Tabuk, 47512, Saudi Arabia
Correspondence: Saleh F Alqifari, Pharmacy Practice Department, College of Pharmacy, University of Tabuk, Tabuk, Saudi Arabia, Tel +966532544334, Email [email protected]
Background: Antenatal care (ANC) is the care women receive during pregnancy before birth and represents a cornerstone of maternal and child health. Previously, Saudi women faced various barriers to practicing ANC, including challenges related to transportation, low maternal education, poor communication with healthcare centers, and incorrect maternal beliefs. In line with Saudi Vision 2030, this multicenter cross-sectional study aimed to investigate the timing of ANC contact, coverage of service utilization in public hospitals among Saudi mothers, sociodemographic factors and antenatal health care utilization, and beliefs about prenatal vitamins, and supplement use among pregnant Saudi women.
Methods: Data was collected from 1230 pregnant women across 11 Ministry of Health (MOH) facilities. The study assessed the timing of ANC initiation, beliefs about prenatal vitamins, and the use of folic acid, calcium, and iron during pregnancy. Chi-square tests were employed to analyze associations between variables.
Results: The findings revealed that 14.55% of participants initiated ANC within the first 8 weeks of pregnancy, with 85.44% starting later. However, the majority 88.78% received prenatal care during pregnancy, regardless of the timing of ANC initiation. Beliefs about prenatal vitamins varied, with 20.08% agreeing that prenatal vitamins were only indicated for malnourished mothers, 72.35% disagreeing, and 7.56% uncertain. Moreover, 51.30% believed ANC should begin before pregnancy, 29.83% after pregnancy confirmation, and 13.57% during the first trimester, with no significant correlation between beliefs and ANC timing. Regarding prenatal care, 95.20% would recommend starting prenatal care with every pregnancy, regardless of the timing of their own ANC initiation.
Conclusion: This study offers a comprehensive analysis of factors impacting late ANC contact and inadequate ANC contacts among pregnant Saudi women. These findings contribute to the broader understanding of ANC practices among Saudi women and underscore the importance of considering various determinants for tailored interventions and health education programs.
Keywords: antenatal care, pregnancy complications, inadequate ANC, late ANC, prenatal care
Introduction
It is widely recognized that high quality antenatal care (ANC) is a crucial element towards maternal healthcare. ANC is crucial for several reasons. It significantly contributes to reducing perinatal and maternal mortality and morbidity by identifying high-risk pregnancies and intervening early in cases of complications like preeclampsia.1 In 2016, the World Health Organization (WHO) updated its guidelines for ANC, shifting from recommending at least four ANC visits to a model that emphasizes “antenatal contacts” and raises the minimum required number to at least eight.2,3 Research indicates a strong correlation between substandard prenatal, intrapartum, and postnatal care and unfavorable pregnancy outcomes.4 Maternal health, nutrition, the availability, and utilization of healthcare services all contribute to the risk factors for perinatal death.5 Inadequate ANC, which means having fewer than the recommended number of visits, and late ANC, which begins after 12 weeks of pregnancy, can have significant implications for the health of both mothers and newborns.6,7 Inadequate antenatal care, defined as starting after the 12th week of pregnancy or having fewer than the recommended number of visits, has significant consequences for the health of mothers, fetuses, and newborns.8–12
Studies have shown varying rates of antenatal care attendance, with some countries reporting high coverage, while others have lower rates.13–22 Access to quality ANC has far-reaching sociodemographic effects, impacting communities’ health and socio-economic status. In developed countries, comprehensive antenatal services are readily available, contributing to reduced maternal and neonatal mortality rates and better overall maternal health. Conversely, in many low- and middle-income nations, access to such care remains a challenge due to various sociodemographic factors, including poverty, limited education, and inadequate healthcare infrastructure. By analyzing data on ANC coverage over the last five years23 across various countries from different continents and varying sociodemographic indices, it becomes evident that there is considerable variability in ANC coverage. Some countries, such as Finland, the USA, Czechia, Estonia, Australia, and Italy, have consistently achieved high ANC coverage rates, exceeding 90%. These nations have managed to provide comprehensive ANC services to a substantial proportion of their pregnant population (Figure 1). In contrast, other countries, like Nigeria with a coverage rate of 60.4%, and Senegal at 55.4%, struggle with relatively low ANC coverage. These discrepancies can be attributed to several factors, including the availability of public healthcare facilities and the sociodemographic index of the respective countries. It is essential to recognize that the success of ANC programs is closely linked to the capacity of a country’s healthcare infrastructure to provide these services and the sociodemographic characteristics of the population. Countries with higher sociodemographic indices tend to have better healthcare access and, consequently, higher ANC coverage rates.
In Saudi Arabia, there has been a scarcity of research conducted on antenatal care, with the majority of studies involving small sample sizes.24–26 Therefore, this study aimed to assess the proportion and potential determinants of inadequate and late antenatal care and update the prevalence of ANC utilization among pregnant women in 11 Ministry of Health (MOH) pregnancy follow-up centers in Saudi Arabia. This information is crucial for preventing maternal and newborn mortality and guiding healthcare policy in the region.
 |
Figure 1 Heatmap depicting the ANC coverage for at least 5 consecutive years for 16 countries from different continents. Notes: Data from World Health Organization. GHO | By category | Antenatal care coverage - Data by country. 2023. Available at: https://apps.who.int/gho/data/node.main.ANTENATALCARECOVERAGE4.23 |
Materials and Methods
Study Design, Period, and Setting
This is a cross-sectional study of pregnant mothers who followed up at 11 MOH pregnancy follow-up centers across Saudi Arabia between September 2022 through July 2023. Patients are offered periodic pregnancy follow-ups throughout their pregnancy with the frequency depending on the pregnancy status.25 Follow-up for uncomplicated pregnancies is initiated at one of the aforementioned centers with 8 antenatal contacts offered, at minimum, to pregnant mothers. Follow-up appointments are typically booked through the Sehhaty smartphone application from anywhere in Saudi Arabia.27 This study data was collected by trained medical and pharmacy interns with the assistance of trained registered nurses in each of the centers.
Terms and Definitions
Participants: Refers to mothers who followed up at 11 MOH pregnancy follow-up centers between September 2022 through July 2023. The sample was collected systemically by targeting every other pregnancy follow-up appointment scheduled to capture 1230 women out of approximately 3600 scheduled appointments in these centers during the study duration.
Inadequate ANC: This term refers to receiving fewer than eight antenatal contacts, as defined by the World Health Organization (WHO).
Late ANC: This phrase indicates that the first antenatal contact occurred after 12 weeks into pregnancy, which is beyond the first trimester.
Interpregnancy interval: This concept pertains to the duration between the conclusion of one pregnancy and the commencement of the subsequent pregnancy. The WHO recommends that this interval should be at least 24 months.
Questionnaire and Data Collection
The validated questionnaire tool used in this study was adapted from previously published protocols.14,19,24,28,29 An additional construct was added to assess the perception and utilization of prenatal care. The questionnaire was then reviewed by two experts for face and content validity.
The data was collected through face-to-face interviews and includes information related to the timing of antenatal care (ANC) contact, age, education level, number of pregnancies, number of births, history of abortions, planned pregnancies, inter-pregnancy intervals, pre-existing medical conditions, history of premature deliveries, placenta problems during pregnancy, type of delivery, prenatal care perception and utilization, and the frequency of prenatal care.
Sample Size Estimation and Data Statistical Analysis
For sample size estimation, we utilized the Raosoft Sample Size Calculator30 (accessed on 20 April 2022) based on a margin of error of 5%, a response distribution of 50%, and a confidence level of 90%. The population size is 6673 based on the latest pregnancy and delivery consensus data by the MOH in Saudi Arabia for these centers. The calculated sample size was 364 participants.
Logistic regression was used to analyze the association of time of ANC contacts with the characteristics of the study population. The adjusted model included all potential characteristics and the unadjusted model included only one potential characteristic to calculate the odd ratios and 95% confidence interval. Chi-square statistics was used to analyze the categorical variables of patient response and supportive care with time of ANC contact. A two-tailed p-value less than 0.05 was considered a statistically significant association between the characteristics and time of ANC contact. Statistical Package for Social Sciences (SPSS version 26.0) was used in statistical analysis.
Ethical Approval
The study protocol (Reference No. 00–20211310) was approved by the MOH Research Ethics Committee on October 13, 2021. Participants were briefed on the purpose of the study and the expected duration of the interview, and those who consented to participate were included in the study.
Results
Sociodemographic Factors and Antenatal Health Care Among Pregnant Women
We collected data from 1230 participants (Recent and old mothers) in the age group of 18–50 years. The mean (standard deviation) age was 31.48 (6.52) years. Approximately 14.55% of the participants initiated early ANC contact within the first 8 weeks of pregnancy, while the majority, 85.44%, contacted ANC services after 8 weeks. Furthermore, 64.55% of the pregnant women had adequate ANC contacts, while 35.44% had fewer than 8 ANC contacts. When examining demographic factors, it was observed that 445 pregnant women were under the age of 30, with 117 of them having adequate ANC contacts, whereas 785 women aged 30 or older included 375 with adequate ANC contacts. In terms of education level, 273 women had completed high school education or less, with 42 of them having timely ANC contact. In contrast, among the 957 women who completed undergraduate degrees or higher, only 120 had adequate ANC contacts. Additionally, the analysis considered the number of pregnancies, births, and abortions. A substantial proportion of women, 924, had been pregnant less than five times, with 745 of them having adequate ANC contacts. Conversely, all 306 women with more than five pregnancies had adequate ANC contacts. A similar pattern was observed for the number of births and abortions where 598 women with planned pregnancies had adequate ANC contacts, while 436 of those with unplanned pregnancies had fewer than 8 ANC contacts. Inter-pregnancy intervals played a role as well, with 258 women reporting more than 24 months between pregnancies and 184 of them having adequate ANC contacts (Table 1).
 |
Table 1 Sociodemographic Characteristics of Participants (n=1230) and ANC Contact Frequency |
Analysis of Factors Associated with Late Antenatal Care (ANC) Contact and Inadequate ANC Contacts Among Pregnant Women
Age initially revealed a significant impact, with pregnant women under 30 having a lower risk of late ANC contact (14.55%) and inadequate ANC contacts (64.55%), but these associations became non-significant after adjusting for other factors (adjusted OR for late ANC: 1.275, p-value: 0.555; adjusted OR for inadequate ANC: 0.478, p-value: 0.260). Education level did not significantly affect late ANC contact (unadjusted OR: 1.088, p-value: 0.659). Still, it was significantly associated with inadequate ANC contacts (42.24%), with graduates showing a lower risk, and this association remained significant after adjustment (adjusted OR: 0.010, p-value: 0.000).
The number of pregnancies significantly impacted late ANC contact (14.55%), with women having fewer than 5 pregnancies showing a lower risk (unadjusted OR: 0.806, p-value: 0.000), which remained unaffected by adjustment. Additionally, the number of pregnancies had a dramatic effect on inadequate ANC contacts, with women having more than 5 pregnancies at a substantially higher risk (unadjusted OR: 3732.019, p-value: 0.000), and this association remained significant after adjustment (adjusted OR: 0.000, p-value: 0.998). The number of births significantly influenced late ANC contact (14.55%), with women having fewer than 5 births exhibiting a lower risk (unadjusted OR: 0.020, p-value: 0.000), and this association was not influenced by adjustment. Moreover, the number of births significantly affected inadequate ANC contacts (14.55%), with women having more than 5 births at higher risk (unadjusted OR: 0.003, p-value: 0.000). After adjustment, this association remained significant (adjusted OR: 0.402, p-value: 1.000). Regarding abortions, women with one abortion had a significantly higher risk of late ANC contact (2.47%) compared to those with no abortions (unadjusted OR: 2.065, p-value: 0.000), and this association remained significant after adjustment (adjusted OR: 4.906E6, p-value: 0.992). A similar pattern was observed for inadequate ANC contacts (2.47%), with women having one abortion at higher risk (unadjusted OR: 2.972, p-value: 0.000), and this association remained significant after adjustment (adjusted OR: 0.538, p-value: 0.489) (Table 2).
 |
Table 2 Unadjusted and Adjusted Odds Ratios for Various Sociodemographic Factors Affecting ANC Contacts Among Participants |
Prenatal Care, Prenatal Vitamins, and Attitudes Towards Prenatal Care Among Surveyed Women
Approximately 14.55% of the total respondents-initiated ANC within the first 8 weeks of pregnancy, while 85.44% started ANC after 8 weeks. - 64.55% of the participants had eight or more ANC contacts, whereas 35.44% had less than eight ANC contacts. The majority of respondents (88.78%) reported receiving prenatal care during pregnancy, while 11.21% did not. - Interestingly, the timing of ANC contact did not significantly impact the receipt of prenatal care, as indicated by a non-significant Chi-square value of 0.055. - A larger proportion of those who initiated ANC within 8 weeks reported receiving prenatal care (88.86%), compared to those who started later (11.13%). Regarding beliefs about prenatal vitamins, 20.08% agreed that prenatal vitamins are only indicated for malnourished mothers, while 72.35% disagreed, and 7.56% had no idea. - The Chi-square value of 0.996 indicates that there is no significant association between beliefs about prenatal vitamins and the timing of ANC contact. - Among those who agreed that prenatal vitamins are only for malnourished mothers, 24.54% initiated ANC within 8 weeks, while 66.51% started later (Table 3).
 |
Table 3 Descriptive Statistics and Regression Analysis Between Timing and Frequency of ANC Contacts and Beliefs Regarding the Use of Various Supplements During Pregnancy |
Supplement Usage and Prenatal Vitamin Adoption Among Surveyed Women
Most respondents reported using folic acid (88.13%), calcium (64.63%), iron (77.39%), and prenatal vitamins (25.77%) supplements. The timing of ANC contact did show significant associations with supplement usage, except for folic acid supplements, where those initiating ANC within 8 weeks were slightly more likely to use them (88.39%). In summary, while there are variations in the timing of ANC contact and beliefs about prenatal vitamins and the right time to start prenatal care, the majority of pregnant women received prenatal care and used supplements regardless of when they initiated ANC. However, there are important nuances to consider when promoting early ANC and educating about supplement use during pregnancy (Table 4).
 |
Table 4 The Associations Between the Timing of ANC Contact, the Number of ANC Contacts, and the Use of Different Supplements |
Discussion
Adequate and early antenatal care is essential because it increases the likelihood of pregnant women undergoing crucial screening tests, detecting non-communicable diseases, and modifying lifestyle risk factors like malnutrition and smoking, which are most effectively addressed in early pregnancy.29,31–34
ANC coverage in Arabic countries, spanning from the 1990s to the most recent available data in 2019 reveals a diverse landscape of ANC services in the region. Some countries, such as Bahrain and the United Arab Emirates (UAE), stand out with exceptional ANC coverage, consistently nearing 100% (Figure 2). These nations have established highly effective ANC programs that provide crucial care to a vast majority of pregnant women. In contrast, several other countries in the Arabic region grapple with lower ANC coverage rates. For instance, Mauritania reported a coverage rate of 52.4%, and Morocco’s coverage stood at 60.9%. These data indicate a need for these countries to enhance their ANC services and expand access to reach more expectant mothers (Figure 2). Saudi Arabia, with an ANC coverage rate of 79.9% in 2019, falls in between the countries with outstanding ANC coverage and those with lower rates. While Saudi Arabia has made significant progress in providing ANC services. We decided to conduct a comprehensive study aimed at updating and assessing the coverage of ANC in Saudi Arabia.
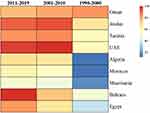 |
Figure 2 Heatmap depicting the ANC coverage for 9 Arabic countries from Africa and Asia. Notes: Data from World Health Organization. GHO | By category | Antenatal care coverage - Data by country. 2023. Available at: https://apps.who.int/gho/data/node.main.ANTENATALCARECOVERAGE4.23 |
Previous studies identified various barriers in Saudi Arabia to attend ANC visits.35 These barriers were categorized into three themes: physical obstacles (such as transportation issues), low maternal education, and inadequacies in healthcare facilities, including negative staff attitudes and poor communication.
In our study, we investigated ANC initiation and utilization among 1230 pregnant women aged 18 to 50. Our findings shed light on factors related to ANC initiation and contact adequacy, providing a comprehensive view of prenatal healthcare in Saudi Arabia.
Our study unveiled that 14.55% of pregnant women initiated ANC within the first 8 weeks, while the majority (85.44%) started later. Remarkably, a significant proportion (88.78%) received prenatal care, regardless of ANC initiation timing. These findings demonstrate an improvement in ANC coverage compared to previous national studies across various regions of Saudi Arabia.36,37 In a 2020 study, 34% of participants had inadequate or late ANC.26
Regarding perceptions of prenatal care commencement, approximately 51.30% believed it should begin before pregnancy, 29.83% after confirmation, 13.57% during the first trimester, and 5.28% uncertain. Interestingly, these beliefs did not significantly correlate with ANC initiation timing. A noteworthy 95.20% were willing to advise others to start prenatal care with every pregnancy, regardless of their own ANC initiation timing.
Regarding supplement usage, most respondents took folic acid (88.13%), iron (77.39%), calcium (64.63%), and prenatal vitamins (25.77%). ANC initiation timing generally did not significantly affect supplement usage, except for calcium (57.54%) among early initiators. The majority of participants in our study received complementary supplements during pregnancy, which aligns with findings from studies in other countries that have shown significant usage of complementary supplements during pregnancy.38–41
In comparison to earlier studies in the Kingdom of Saudi Arabia,42 which reported that 81.8% of pregnant women received folic acid during antenatal care, our study indicated a notable advancement, with 88.13% of participants receiving folic acid. This suggests a rising level of awareness among pregnant Saudi women and a satisfactory provision of information by healthcare centers.
The study by Al-Wutayd26 found a significant percentage of participants with inadequate and late antenatal care, where high parity and employment status played a substantial role. Similarly, another study24 in 2009 explored the impact of employment on prenatal care initiation and visits, indicating that working mothers often initiated care late and attended fewer visits.
Conclusions
The analysis of factors influencing ANC among pregnant Saudi women reveals several key determinants. While age and education were not significant predictors of delayed ANC initiation, higher education levels correlated with improved ANC adequacy. Lower numbers of pregnancies and births were associated with more timely and adequate ANC, while a history of abortions significantly influenced both tardiness and insufficiency of ANC contacts. Planned pregnancies and extended inter-pregnancy intervals were linked to better ANC outcomes. Pre-existing health conditions, a history of premature deliveries, and placental problems during pregnancy were critical predictors of late and inadequate ANC. The study emphasizes the complex interplay of sociodemographic and health-related factors influencing ANC utilization.
Recommendations
Our study recommends the establishment of public communication teams dedicated to announcing and promoting antenatal care in primary health care centers, targeting both educators and non-educators. Healthcare providers should prioritize the early initiation of antenatal care within the first 8 weeks and address diverse beliefs about prenatal vitamins to optimize maternal and child health outcomes. These insights serve as valuable guidance for interventions aimed at enhancing antenatal health practices among pregnant women in Saudi healthcare centers.
Data Sharing Statement
Data are available upon request from the corresponding author.
Acknowledgments
The author would like to extend appreciation to the Ministry of Health in Saudi Arabia for their support and facilitation of this study.
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Disclosure
The author declares no relevant conflicts of interest or financial relationship in this work.
References
1. Alhashem A, Alotaiby BA, Al Thobaiti RB, et al. Adoption of antenatal care conversation mapping among health care providers in Saudi Arabia: application of the diffusion innovation theory. PLoS One. 2023;18(6):e0286656. doi:10.1371/journal.pone.0286656
2. New guidelines on antenatal care for a positive pregnancy experience; 2023. Available from: https://www.who.int/news/item/07-11-2016-new-guidelines-on-antenatal-care-for-a-positive-pregnancy-experience.
3. World Health Organization. WHO Recommendations on Antenatal Care for a Positive Pregnancy Experience. Geneva: World Health Organization; 2016.
4. Yirgu R, Molla M, Sibley L, Gebremariam A. Perinatal mortality magnitude, determinants and causes in West Gojam: population-based nested case-control study. PLoS One. 2016;11(7):e0159390. doi:10.1371/journal.pone.0159390
5. Al-Ani ZR, Al-Hiali SJ, Al-Mashhadani WS. Perinatal mortality rate in Al-Ramadi Maternity and Children’s Hospital, western Iraq. Saudi Med J. 2009;30(10):1296–1300.
6. Benova L, Ö T, Moran AC, Campbell OMR. Not just a number: examining coverage and content of antenatal care in low-income and middle-income countries. BMJ Global Health. 2018;3(2):e000779. doi:10.1136/bmjgh-2018-000779
7. Berhan Y, Berhan A. Antenatal care as a means of increasing birth in the health facility and reducing maternal mortality: a systematic review. Ethiop J Health Sci. 2014;24:93–104. doi:10.4314/ejhs.v24i0.9S
8. 1 in 10 babies worldwide are born early, with major impacts on health and survival; 2023. Available from: https://www.who.int/news/item/06-10-2023-1-in-10-babies-worldwide-are-born-early--with-major-impacts-on-health-and-survival.
9. Neonatal Mortality Formative Research Working Group. Developing community-based intervention strategies to save newborn lives: lessons learned from formative research in five countries. J Perinatol. 2008;28:S2–8. doi:10.1038/jp.2008.166
10. Negese K, Belachew DZ. Maternal complications and associated factors among mothers who underwent a cesarean section at Gebretsadik Shewa general hospital: an institution based cross-sectional study. Front Global Women’s Health. 2023;4:1091863. doi:10.3389/fgwh.2023.1091863
11. Nagata C, Yang L, Yamamoto-Hanada K, et al. Complications and adverse outcomes in pregnancy and childbirth among women who conceived by assisted reproductive technologies: a nationwide birth cohort study of Japan environment and children’s study. BMC Pregnancy Childbirth. 2019;19(1):77. doi:10.1186/s12884-019-2213-y
12. Liu L, Oza S, Hogan D, et al. Global, regional, and national causes of child mortality in 2000-13, with projections to inform post-2015 priorities: an updated systematic analysis. Lancet. 2015;385:430–440. doi:10.1016/S0140-6736(14)61698-6
13. Debessai Y, Costanian C, Roy M, El-Sayed M, Tamim H. Inadequate prenatal care use among Canadian mothers: findings from the Maternity Experiences Survey. J Perinatol. 2016;36(6):420–426. doi:10.1038/jp.2015.218
14. Feijen-de Jong EI, Jansen DE, Baarveld F, van der Schans CP, Schellevis FG, Reijneveld SA. Determinants of late and/or inadequate use of prenatal healthcare in high-income countries: a systematic review. Europ J Public Health. 2012;22(6):904–913. doi:10.1093/eurpub/ckr164
15. Huda TM, Chowdhury M, El Arifeen S, Dibley MJ. Individual and community level factors associated with health facility delivery: a cross sectional multilevel analysis in Bangladesh. PLoS One. 2019;14(2):e0211113. doi:10.1371/journal.pone.0211113
16. Orwa J, Temmerman M, Nyaga L, Mulama K, Luchters S. Health facilities preparedness to deliver maternal and newborn health care in Kilifi and Kisii Counties, Kenya. BMC Health Serv Res. 2023;23(1):868. doi:10.1186/s12913-023-09884-9
17. Yeoh PL, Hornetz K, Ahmad Shauki NI, Dahlui M. Assessing the extent of adherence to the recommended antenatal care content in Malaysia: room for improvement. PLoS One. 2015;10(8):e0135301. doi:10.1371/journal.pone.0135301
18. Yoseph S, Dache A, Dona A. Prevalence of early postnatal-care service utilization and its associated factors among mothers in Hawassa Zuria District, sidama regional state, Ethiopia: a cross-sectional study. Obstet Gynecol Internat. 2021;2021:5596110. doi:10.1155/2021/5596110
19. Wolde F, Mulaw Z, Zena T, Biadgo B, Limenih MA. Determinants of late initiation for antenatal care follow up: the case of northern Ethiopian pregnant women. BMC Res Notes. 2018;11(1):837. doi:10.1186/s13104-018-3938-9
20. Salami KK, Yusuf OB, Akinyemi JO, et al. Individual and ecological analyses of antenatal care: prospects for delivery assistance and use of modern family planning in Nigeria. Afr J Reproduct Health. 2022;26:11.
21. Cresswell JA, Yu G, Hatherall B, et al. Predictors of the timing of initiation of antenatal care in an ethnically diverse urban cohort in the UK. BMC Pregnancy Childbirth. 2013;13:103. doi:10.1186/1471-2393-13-103
22. Asundep NN, Carson AP, Turpin CA, et al. Determinants of access to antenatal care and birth outcomes in Kumasi, Ghana. J Epidemiol Glob Health. 2013;3(4):279–288. doi:10.1016/j.jegh.2013.09.004
23. World Health Organization. GHO, by category, antenatal care coverage - Data by country; 2023. Available from: https://apps.who.int/gho/data/node.main.ANTENATALCARECOVERAGE4.
24. El-Gilany AH, El-Wehady A, El-Hawary A. Maternal employment and maternity care in Al-Hassa, Saudi Arabia. Europ J Contracep Reprod Health Care. 2008;13(3):304–312. doi:10.1080/13625180802185080
25. Alanazy W, Brown A. Individual and healthcare system factors influencing antenatal care attendance in Saudi Arabia. BMC Health Serv Res. 2020;20(1):49. doi:10.1186/s12913-020-4903-6
26. Al-Wutayd O. Inadequate and late antenatal contacts among Saudi mothers: a hospital-based cross-sectional study. Int J Women’s Health. 2020;12:731–738. doi:10.2147/IJWH.S265941
27. الصحة فبو. Ministry Of Health Saudi Arabia; 2023. Available from: https://www.moh.gov.sa/en/eServices/cards/Pages/Pregnancy-follow-up.aspx.
28. Guliani H, Sepehri A, Serieux J. Determinants of prenatal care use: evidence from 32 low-income countries across Asia, Sub-Saharan Africa and Latin America. Health Policy Plann. 2014;29(5):589–602. doi:10.1093/heapol/czt045
29. Wolde HF, Tsegaye AT, Sisay MM. Late initiation of antenatal care and associated factors among pregnant women in Addis Zemen primary hospital, South Gondar, Ethiopia. Reproductive Health. 2019;16(1):73. doi:10.1186/s12978-019-0745-2
30. Sample Size Calculator by Raosoft, Inc; 2023. Available from: http://www.raosoft.com/samplesize.html.
31. Mlotshwa PR, Sibiya MN. Pregnant women’s views regarding maternity facility-based delivery at primary health care facilities in the province of KwaZulu-Natal in South Africa. Int J Environ Res Public Health. 2023;20(15):6535. doi:10.3390/ijerph20156535
32. Magadi MA, Madise NJ, Rodrigues RN. Frequency and timing of antenatal care in Kenya: explaining the variations between women of different communities. Soc Sci Med. 2000;51(4):551–561. doi:10.1016/S0277-9536(99)00495-5
33. Powel JE, Chavan NR, Zantow EW, et al. Risk of adverse perinatal outcomes in pregnancies with ”small” fetuses not meeting Delphi consensus criteria for fetal growth restriction. Am J Clin Exp Obstet Gynecol. 2023;229(4):447.e1–447.e13. doi:10.1016/j.ajog.2023.04.037
34. Titaley CR, Dibley MJ, Roberts CL. Factors associated with underutilization of antenatal care services in Indonesia: results of Indonesia Demographic and Health Survey 2002/2003 and 2007. BMC Public Health. 2010;10:485. doi:10.1186/1471-2458-10-485
35. Alanazy W, Rance J, Brown A. Exploring maternal and health professional beliefs about the factors that affect whether women in Saudi Arabia attend antenatal care clinic appointments. Midwifery. 2019;76:36–44. doi:10.1016/j.midw.2019.05.012
36. Hazmi JA. Awareness of antenatal care importance among Saudi Pregnant Women in Madina. JGWH. 2017;4(5). doi:10.19080/JGWH.2017.04.555649
37. Al-Ateeq MA, Al-Rusaiess AA, Al-Dughaither AA. Perceptions and effects of antenatal education. Saudi Med J. 2013;34(12):1287–1293.
38. Barnes LAJ, Rolfe MI, Barclay L, McCaffery K, Aslani P. Demographics, health literacy and health locus of control beliefs of Australian women who take complementary medicine products during pregnancy and breastfeeding: a cross-sectional, online, national survey. Health Expect. 2022;25(2):667–683. doi:10.1111/hex.13414
39. Quzmar Y, Istiatieh Z, Nabulsi H, Zyoud SH, Al-Jabi SW. The use of complementary and alternative medicine during pregnancy: a cross-sectional study from Palestine. BMC Complement Med Therap. 2021;21(1):108. doi:10.1186/s12906-021-03280-8
40. Yazdi N, Salehi A, Vojoud M, Sharifi MH, Hoseinkhani A. Use of complementary and alternative medicine in pregnant women: a cross-sectional survey in the south of Iran. J Integr Med. 2019;17(6):392–395. doi:10.1016/j.joim.2019.09.003
41. Hall HG, Griffiths DL, McKenna LG. The use of complementary and alternative medicine by pregnant women: a literature review. Midwifery. 2011;27(6):817–824. doi:10.1016/j.midw.2010.08.007
42. AlAhmadi R. Use of folic acid among pregnant women attending antenatal care clinic at Al-Hejrah primary health care center, Makkah Al-Mokarramah, Saudi Arabia. Int J Med Sci Public Health. 2014;3(8):963. doi:10.5455/ijmsph.2014.020620141
 © 2024 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2024 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
