Back to Journals » Patient Preference and Adherence » Volume 18
Adherence to Background Antipsychotic and Pimavanserin in Patients with Schizophrenia: Post Hoc Analyses from the ENHANCE and ADVANCE Studies
Authors Bugarski-Kirola D, Abbs B, Odetalla R, Liu IY, Darwish M, DeKarske D
Received 14 September 2023
Accepted for publication 11 January 2024
Published 19 January 2024 Volume 2024:18 Pages 207—216
DOI https://doi.org/10.2147/PPA.S436041
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Johnny Chen
Dragana Bugarski-Kirola,1,2 Brandon Abbs,2 Ramzey Odetalla,2 I-Yuan Liu,2 Mona Darwish,2 Daryl DeKarske3
1Acadia Pharmaceuticals GmbH, Basel, Switzerland; 2Acadia Pharmaceuticals Inc, Princeton, NJ, USA; 3Acadia Pharmaceuticals Inc, San Diego, CA, USA
Correspondence: Dragana Bugarski-Kirola, Acadia Pharmaceuticals GmbH, Barfüẞerplatz 3, Basel, Switzerland, 4051, Tel +41798658317, Email [email protected]
Background: In patients with schizophrenia, study design to optimize adherence and objective measurement of adherence is critical for interpreting results. Two randomized, double-blind studies evaluating adjunctive pimavanserin in patients with schizophrenia who received stable antipsychotic treatment included measures to encourage and assess treatment adherence.
Objective: This post hoc analysis evaluated adherence levels achieved in the Phase III ENHANCE study (NCT02970292) and the Phase II ADVANCE study (NCT02970305).
Methods: Blood levels of participants receiving adjunctive treatment with pimavanserin or placebo added to their ongoing antipsychotic medication were tested and evaluated regularly throughout both studies. For both the background antipsychotic and pimavanserin, treatment adherence was defined as a blood sample test result above the lower limit of quantification.
Results: Overall, 392 of 633 screened patients and 403 of 608 screened patients were in the safety populations in ENHANCE and ADVANCE, respectively. In ENHANCE, at weeks 1, 3, and 6/early termination (ET), the adherence rates remained ≥ 95.1% for the background antipsychotic in both pimavanserin and placebo treatment groups and ≥ 96.8% for pimavanserin. In ADVANCE, high adherence rates (≥ 90.6%) with the background antipsychotic (for both treatment groups) and pimavanserin (≥ 95.0%) were observed at weeks 2, 8, 14, and 26/ET.
Conclusion: Rigorous screening was performed to exclude patients not adherent to their background antipsychotic before enrollment and to pimavanserin during study visits by using regular blood sampling. Mandatory caregiver participation further supported adherence to study treatment and procedures. These efforts may have contributed to the high levels of adherence to both background antipsychotic and pimavanserin reported in ENHANCE and ADVANCE.
Keywords: adjunctive therapy, treatment compliance, pharmacokinetic drug levels, blood sampling, negative symptoms, caregiver participation
Introduction
Many individuals with schizophrenia experience an inadequate response to antipsychotic treatment,1 which may reflect subtherapeutic exposure to the drug or medication ineffectiveness. Treatment nonadherence should be considered first in patients who experience inadequate treatment response despite therapeutic doses by evaluating subtherapeutic antipsychotic blood levels.2 Patients who do not adhere to their prescribed regimen accrue higher costs of care and experience worse clinical outcomes compared with patients who adhere to their prescribed regimen.3
Failure to achieve therapeutic levels of the study treatment as a result of poor adherence may also complicate the interpretation of clinical study outcomes4 and hinder the development of a potentially effective treatment. Confirming adherence among patients in a clinical study is necessary to ensure that the results of the study are an accurate reflection of the therapeutic potential of the agent under investigation.2 Moreover, this practice is consistent with US Food and Drug Administration guidance on enrichment strategies to support approval of human drugs and biologic products, in which identifying and selecting patients likely to adhere to treatment is a “useful and generally accepted” strategy to decrease variability.5 Conversely, high rates of adherence in a clinical study can complement positive efficacy and safety results, providing additional evidence that the investigational agent can improve a patient’s symptoms without burdensome or treatment-limiting adverse effects. Therefore, it is important to test for adherence when determining eligibility for a study, measure adherence during the study, and review the adherence results after study completion, regardless of the study outcome.
Rigorous assessment of adherence through pharmacokinetic levels of exposure was part of the study design of 2 randomized, double-blind, placebo-controlled studies of pimavanserin in patients with schizophrenia who had been stable while receiving current antipsychotic treatment: ENHANCE (NCT02970292) and ADVANCE (NCT02970305). The phase III ENHANCE study evaluated the efficacy and safety of adjunctive pimavanserin in adult patients with schizophrenia and the inadequate response to their current antipsychotic treatment over 6 weeks of treatment. On the primary efficacy endpoint, change in the Positive and Negative Syndrome Scale (PANSS) total score from baseline to week 6 was numerically greater in the pimavanserin group than in the placebo group, though the difference was not statistically significant. Improvements in negative symptoms with pimavanserin versus placebo were observed in prespecified analyses of the PANSS negative symptoms subscale score and Marder negative symptoms factor score.6 The phase II ADVANCE study evaluated the efficacy and safety of pimavanserin as an adjunctive treatment for the negative symptoms of schizophrenia in patients with stabilized positive symptoms. ADVANCE met its primary efficacy endpoint, demonstrating a statistically significant difference in change in the 16-item Negative Symptom Assessment (NSA-16) total score from baseline to week 26 between pimavanserin and placebo.7
Here, we present a post hoc analysis of treatment adherence to a current antipsychotic and pimavanserin for patients meeting stringent selection criteria from the ENHANCE and ADVANCE studies. We highlight key elements of the study design that promoted adherence and enabled the evaluation of adherence data.
Methods
The design and methodology of the ENHANCE and ADVANCE studies have been reported previously.6,7 Study protocols were reviewed and approved by independent ethics committees or institutional review boards at each study site. Both studies were conducted in accordance with the principles of Good Clinical Practice derived from the Declaration of Helsinki, and in accordance with local regulations and International Council of Harmonization guidelines. All patients provided written informed consent prior to enrolling in the study. This retrospective analysis utilized anonymized patient data to maintain patient privacy. Both studies were registered with ClinicalTrials.gov (Identifiers: NCT02970292 and NCT02970305). Patients enrolled in ENHANCE and ADVANCE were randomly assigned to receive either pimavanserin (flexible dosing of 10, 20, or 34 mg) or placebo added to ongoing antipsychotic therapy. Several eligibility and testing requirements were specifically included in the design of both studies to enable the assessment of treatment adherence among participants (Figure 1).
Eligibility Criteria
To participate in either study, patients must have been receiving a stable dose of aripiprazole (or long-acting injectable [LAI]), asenapine, brexpiprazole, cariprazine, lurasidone, olanzapine, or risperidone (or LAI) before enrollment. Patients were required to have received documented (eg, a copy of the prescription) treatment with an adequate dose of an antipsychotic within the dose range recommended according to the local prescribing information for ≥ 8 weeks before screening. Dose changes within 4 weeks before screening for oral or 16 weeks before screening for LAI were not permitted. In ENHANCE, if the patient was taking 2 antipsychotics at screening, the investigator determined which antipsychotic was the main antipsychotic and discontinued the other antipsychotic at least 5 half-lives before randomization, if medically justified. In ADVANCE, patients must have been taking only 1 antipsychotic, which was continued throughout the patient’s participation in the study. The patient’s caregiver was also required to agree to participate alongside the patient to support the patient’s adherence to treatment and study procedures.
Screening Procedures
Screening procedures included laboratory testing of blood samples to confirm the presence or absence of the identified ongoing antipsychotic treatment as part of a comprehensive review of patient eligibility before any study procedure. Patients also undertook a structured telemedicine interview with an independent clinician to confirm they had a partial but inadequate response to their ongoing antipsychotic treatment (ENHANCE) and that they were not treatment-resistant. Treatment resistance was defined as either failing to demonstrate even a minimal response to ≥2 adequate antipsychotic medications prescribed at adequate doses and durations or based on clozapine treatment, which included clozapine treatment for refractory psychosis or use of clozapine within the past 12 weeks prior to screening. As part of the criteria, the failure to tolerate a medication did not constitute failure to respond. In ADVANCE, the interview was used to confirm patients had predominant negative symptoms of schizophrenia while taking their ongoing antipsychotic. Predominant negative symptoms were defined by a score of at least 20 on the sum of the seven PANSS Marder negative factor items (and scores ≥4 on at least three of the seven PANSS items or ≥5 on at least two of the seven PANSS items), and a score of no more than 22 on the sum of the eight PANSS Marder positive factor items (of which no more than two selected items were rated 4, and none ≥5, at screening and baseline). There were three selected PANSS Marder positive factor items (P1 delusions, P3 hallucinatory behavior, and P6 suspiciousness or persecution). The severity of negative symptoms required a score of ≥4 (moderately ill or worse) at screening and baseline on the negative symptoms subscale of the Clinical Global Impression of Schizophrenia Scale-Severity (CGI-SCH-S).
Measures of Adherence to Study Treatment
Regular testing and the evaluation of blood samples of patients undergoing ongoing antipsychotic treatment were conducted throughout both studies. The same methods were used for all antipsychotics (including LAI formulations of aripiprazole and risperidone). Blood samples were collected at baseline and weeks 1, 3, and 6 (or early termination [ET]) for ENHANCE and at baseline and weeks 2, 8, 14, and 26 (or ET) for ADVANCE to confirm the presence or absence of the ongoing background antipsychotic treatment and to assess the pharmacokinetics of pimavanserin.
Study Outcomes and Statistical Analyses
Reasons for screen failure were evaluated. Adherence was assessed in the safety population, which included all randomly assigned patients who received at least 1 dose of the study drug.
Descriptive statistics were used throughout to examine the proportion of patients who were adherent to their ongoing antipsychotic treatment at screening and to the ongoing antipsychotic and pimavanserin during each study. Patients were considered adherent to their medication at a certain time point if a blood sample test result was above the lower limit of quantification (LLOQ) for pimavanserin or the background antipsychotic. Additional analyses were performed using other adherence definitions, including complete nonadherence for both the antipsychotic and pimavanserin (all postbaseline samples <LLOQ).
Results
Patient Population
Overall, 633 and 608 patients were screened for eligibility to participate in the ENHANCE and ADVANCE studies, respectively.
Reasons for screen failure for both studies are summarized in Table 1. Failure to confirm the ongoing antipsychotic in the screening blood sample was a common reason for screen failure (ENHANCE, 16.9% [n = 46]; ADVANCE, 13.3% [n = 32]). A rescreening was permitted under exceptional circumstances, such as when a temporary condition may have contributed to nonadherence detected during an initial screening. In the ENHANCE study, 3 patients were deemed eligible to participate and be randomly assigned to treatment following an initial screen failure for nonadherence. These patients were receiving olanzapine as a background antipsychotic, and rescreening was permitted owing to technical issues, with the assay leading to failed testing. In the ADVANCE study, 1 patient was deemed eligible to participate and be randomly assigned to treatment following an initial screen failure for nonadherence. This patient was switched to a different generic version of their ongoing antipsychotic after no antipsychotic was detected in blood samples drawn while the patient was receiving the previous generic. The background antipsychotics were not detected in an additional 10 patients who had failed screening for participation in the ENHANCE study for a reason other than nonadherence before antipsychotic blood level results were known. Other common reasons for screen failure in the ADVANCE study included patients not meeting study inclusion criteria for the presence of predominant negative symptoms of schizophrenia and withdrawal of consent. In both studies, withdrawal of consent frequently resulted from the rigorous screening process required for the study.
 |
Table 1 Most Common Reasons for Screening Failures (Randomized Population) |
Patient demographics, disease characteristics, and background antipsychotic have been previously reported6,7 and were generally similar in the pimavanserin and placebo groups for each study. The percentage of the most frequent antipsychotics in ENHANCE and ADVANCE were oral and LAI aripiprazole (17.4% [n = 69] and 3.5% [n = 14]; 26.1% [n = 105] and 6.5% [n = 26]), olanzapine (35.9% [n = 142]; 27.8% [n = 112]), and oral and LAI risperidone (33.3% [n = 132] and 6.1% [n = 24]; 30.0% [n = 121] and 8.4% [n = 34]), respectively.
Adherence Rates
Among the randomly assigned patients, blood samples were available at baseline for 392 of 396 patients participating in the ENHANCE study and for all 403 patients participating in the ADVANCE study. The missing baseline blood samples in ENHANCE were either inadvertently not collected (n = 2) or not analyzed (n = 2).
At baseline, 94.9% (372 of 392) and 95.0% (383 of 403) of patients with available samples were considered adherent to their current antipsychotic in the ENHANCE and ADVANCE studies, respectively. If patients who were nonadherent to their current antipsychotic at screening had been included in the study, adherence rates would have been 83.2% (326 of 392) in ENHANCE and 87.1% (351 of 403) in ADVANCE.
In ENHANCE, adherence rates for either the antipsychotic or pimavanserin were all at or above 95.1% at any given time point (weeks 1, 3, and 6/ET) (Table 2). More than 93% of patients in both treatment groups were adherent to their current antipsychotic at all time points, and > 96% were adherent to adjunctive pimavanserin treatment at all time points (Figure 2a).
 |
Table 2 Adherence to Background Antipsychotic and Pimavanserin During Treatment by Study Visit (ENHANCE; Safety Population) |
In ADVANCE, adherence rates for either the antipsychotic or pimavanserin were all at or above 90.6% at any given time point (weeks 2, 8, 14, and 26/ET) (Table 3). More than 85% of patients in both treatment groups were adherent to their current antipsychotic at all time points, and > 92% were adherent to adjunctive pimavanserin treatment at all time points (Figure 2b). Of the measured postbaseline pimavanserin concentrations, 91.7% were at or above the lower end of the 90% prediction interval of the model-predicted median expected level.
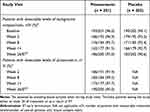 |
Table 3 Adherence to Background Antipsychotic and Pimavanserin During Treatment by Study Visit (ADVANCE; Safety Population) |
Nonadherence Rates in ENHANCE
Because the primary efficacy endpoint of ENHANCE was not met, characteristics of patients with nonadherence (ie, adherence at 0 time points) in ENHANCE were analyzed to gain insight into these patients and to understand the potential role of nonadherence in the results. Of patients who were treated with pimavanserin but who were nonadherent to their background antipsychotic (n = 5), the mean change from baseline in the PANSS total score was −20.8 and −13.4 for all patients (both adherent and nonadherent to background antipsychotic) in the placebo group (n = 189). Clinical profiles of individual patients with complete nonadherence showed some questionable but not exclusionary disease characteristics (eg, late age of onset, no history of hospitalization), but no consistent findings were observed at a group level. Patients from the United States constituted 55.6% of those with complete nonadherence and 30.8% with any nonadherence, compared with 18.4% of all randomly assigned patients. Three of 21 total US sites had ≥ 1 patient with complete nonadherence. Risperidone was the most frequent main antipsychotic treatment in nonadherent patients (66%) and was more common in these patients than in the population of all randomly assigned patients (33%).
Discussion
Adherence to treatment among patients with schizophrenia is typically poor, with an estimated 30% of patients exhibiting some level of nonadherence to their prescribed medication in the clinical study setting.8 Patients in both the 6-week ENHANCE study and the 26-week ADVANCE study achieved a high level of treatment adherence (ENHANCE: > 95%; ADVANCE: > 82%) to both the background antipsychotic and adjunctive pimavanserin at all time points. In both studies, adherence was reliably assessed using pharmacokinetic assessments of the medication in the blood. Confirmation of adherence throughout these studies allowed confidence in the findings related to the efficacy and safety of the studied dosing regimen.
Treatment adherence is important for multiple conditions, including neurodegenerative disorders such as Alzheimer’s disease and psychiatric conditions such as schizophrenia (Velligan et al 2020). The ENHANCE and ADVANCE trials of schizophrenia confirmed adherence using the direct, objective pharmacokinetic assessment of antipsychotic concentration in patient blood. In addition to using direct measures, guidelines and studies have proposed using multiple measures of adherence within a study, including the use of indirect measures such as individual reports (ie, patient, caregiver, or provider) or electronic medication bottle monitoring (Velligan et al 2020).
The high rates of adherence in the ENHANCE and ADVANCE studies might be attributed to specific design elements that encouraged adherence throughout both studies. First, screening procedures included testing for measurable levels of the patient’s current antipsychotic, indicating adherence to their treatment regimen. Because a lack of adherence is a known prognostic factor for future poor adherence and poor outcomes,9,10 this screening measure may have excluded patients who were less likely to be adherent to medication during the studies. Second, additional regular blood testing throughout treatment was mandatory in both studies. The knowledge that adherence was being quantified may have indirectly encouraged adherence. Finally, the designation of a caregiver was mandatory in both studies. These individuals were responsible for providing support to the patient to ensure adherence to the study treatment, study visits, and protocol procedures. Caregiver and familial support is an established factor in achieving adherence to medication among patients with severe psychiatric disorders such as schizophrenia11 and can help compensate for the lack of insight or cognitive issues of patients who do not take their medication as prescribed.12
The high levels of adherence achieved complement the positive efficacy and safety results previously reported in the ADVANCE study.7 Indeed, the a priori presence of treatment adherence measurements in any study can strongly suggest that monitoring medication adherence reveals the presence of an efficacy signal.13 Moreover, because the rate of adherence was high, reliable detection of a treatment effect was possible. ADVANCE met its primary efficacy endpoint, demonstrating a significant improvement in negative symptoms over 26 weeks as measured by a change in the 16-item Negative Symptom Assessment total score. As previously reported, few patients were discontinued in ADVANCE owing to nonadherence to either pimavanserin or placebo (both n = 2 [1.0%]),7 which complements the efficacy results by indicating that the treatment regimen was generally well tolerated. In 2 phase III clinical studies evaluating encenicline for cognitive impairment in schizophrenia, only 4% to 5% of patients who had 0% adherence (at all times) contributed to failure; 17% to 18% of patients were not adherent at some point during the study, emphasizing the importance of high adherence rates in longer-term schizophrenia studies.14
Nonadherence was likely driven by a combination of antipsychotic drug pharmacokinetics (ie, short drug half-life) and environmental factors (eg, forgetting to take a dose).15 A review of the clinical profiles of individual patients considered eligible to participate in the ENHANCE study, which demonstrated complete nonadherence, revealed disease characteristics that, although not considered criteria for exclusion, may have indicated a higher likelihood for nonadherence, including a late age of onset and no history of hospitalization. Adherence may also be affected by geographic differences in treatment paradigms, including long-term relationships with treatment teams and continuity of care support from family that actively promote patient adherence to their treatment.16,17 Many of the patients with complete nonadherence were located in the United States. In fact, 3 of the 21 US study sites reported complete nonadherence, suggesting both US recruitment and treatment practices may not be as supportive of adherence as those in Europe.
Strengths of our study included the rigorous screening methods, caregiver participation requirements, and large percentage of patients (91.7%) with plasma pimavanserin concentrations at or above the lower limit of a model-predicted median expected level. Limitations of the study include the post hoc design and use of a descriptive statistical approach to summarize nonpooled data from 2 studies. Although during screening, most patients exhibited prior antipsychotic plasma levels above the minimum expected level, some concentrations may have been on the lower end (ie, 90% prediction interval) due to the timing of the blood draw during the study visit as different antipsychotics can have significantly different elimination half-lives. In addition, given our stringent inclusion criteria, our high rates of adherence are most relevant to clinical studies and may not reflect rates in real-world settings where patients may lack a caregiver. This lack of caregiver support in the real-world setting underlies the great unmet need in this patient population for reliable caregivers and real-world studies. Future work could help address this by implementing programs to facilitate caregiver education on treatment adherence and the importance of real-world studies for these patients.
Our analyses suggest that rigorous screening for adherence to ongoing treatment before study entry and compulsory participation of a caregiver with a specific role of ensuring patients take their medication can promote adherence to study treatment throughout active treatment in the clinical study setting. Ensuring a high level of adherence is particularly important when investigating adjunctive use of a new therapy because an accurate evaluation of any treatment effect requires that patients remain adherent to the study drug as well as to their ongoing background medication.
Conclusions
This post hoc analysis of 2 randomized, double-blind, placebo-controlled studies in patients with schizophrenia, a population known to be typically nonadherent, demonstrated a high level of short-term and long-term treatment adherence to current antipsychotic and adjunctive pimavanserin, as measured by blood levels. These observations indicate that high levels of adherence to treatment are achievable for patients with schizophrenia, particularly in the context of adjunctive therapy. These findings are most relevant for patients with schizophrenia in a clinical trial setting who have demonstrated prior treatment adherence and have access to a caregiver. The findings presented utilized direct measures of adherence, but indirect measures are also helpful in monitoring treatment adherence.
Key Points
- Because patients with schizophrenia are known to be nonadherent to their treatment plans, it can be difficult to discern whether poor outcomes are due to the treatment not working or to the patient’s low adherence to their regimen.
- For this reason, clinical studies with schizophrenia patients can be difficult and should be optimized for adherence, and measurement of adherence is necessary for interpreting results.
- In this study, we analyzed the adherence of schizophrenia patients taking a current antipsychotic in 2 completed clinical trials to show that high levels of treatment adherence are achievable for this patient population.
Data Sharing Statement
The research data collected for this ongoing phase III study on negative symptoms of schizophrenia, including individual participant data, will not be made available on request at this time because it is anticipated that these data may be part of future regulatory submissions.
Acknowledgments
Medical writing and editorial support, under the direction of the authors, were provided by Ashfield MedComms, an Ashfield Health company, and Nathan Hutcheson PhD (Citrus Health Group), in accordance with Good Publication Practices 2022 (GPP 2022).
Author Contributions
Dragana Bugarski-Kirola and Brandon Abbs contributed to the conception and design of the analysis. Dragana Bugarski-Kirola, Brandon Abbs, and Ramzey Odetalla performed data collection; Mona Darwish, Brandon Abbs, and I-Yuan Liu conducted analyses. All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising, or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Funding
The ENHANCE and ADVANCE studies and medical writing and editing support for the development of this manuscript were funded by Acadia Pharmaceuticals Inc.
Disclosure
Dragana Bugarski-Kirola, Mona Darwish, and I-Yuan Liu are employees of and stockholders in Acadia Pharmaceuticals Inc. Brandon Abbs, Daryl DeKarske, and Ramzey Odetalla are former employees of Acadia Pharmaceuticals Inc. The authors report no other conflicts of interest in this work.
References
1. Carbon M, Correll CU. Clinical predictors of therapeutic response to antipsychotics in schizophrenia. Dialogues Clin Neurosci. 2014;16(4):505–524. doi:10.31887/DCNS.2014.16.4/mcarbon
2. Howes OD, McCutcheon R, Agid O, et al. Treatment-resistant schizophrenia: treatment response and resistance in psychosis (TRRIP) working group consensus guidelines on diagnosis and terminology. Am J Psychiatry. 2017;174(3):216–229. doi:10.1176/appi.ajp.2016.16050503
3. Kane JM, Kishimoto T, Correll CU. Non-adherence to medication in patients with psychotic disorders: epidemiology, contributing factors and management strategies. World Psychiatry. 2013;12(3):216–226. doi:10.1002/wps.20060
4. Lam WY, Fresco P. Medication adherence measures: an overview. Biomed Res Int. 2015;2015:217047. doi:10.1155/2015/217047
5. US Food and Drug Administration. Enrichment Strategies for Clinical Trials to Support Demonstration of Effectiveness of Human Drugs and Biological Products. Silver Spring, Maryland: FDA; 2019.
6. Bugarski-Kirola D, Bitter I, Liu IY, Abbs B, Stankovic S. ENHANCE: Phase 3, randomized, double-blind, placebo-controlled study of adjunctive pimavanserin for schizophrenia in patients with an inadequate response to antipsychotic treatment. Schizophr Bull Open. 2022;3(1). doi:10.1093/schizbullopen/sgac006
7. Bugarski-Kirola D, Arango C, Fava M, et al. Pimavanserin for negative symptoms of schizophrenia: results from the ADVANCE Phase 2 randomised, placebo-controlled trial in North America and Europe. Lancet Psychiatry. 2022;9(1):46–58. doi:10.1016/S2215-0366(21)00386-2
8. Yaegashi H, Kirino S, Remington G, Misawa F, Takeuchi H. Adherence to oral antipsychotics measured by electronic adherence monitoring in schizophrenia: a systematic review and meta-analysis. CNS Drugs. 2020;34(6):579–598. doi:10.1007/s40263-020-00713-9
9. Ascher-Svanum H, Zhu B, Faries D, Lacro JP, Dolder CR. A prospective study of risk factors for nonadherence with antipsychotic medication in the treatment of schizophrenia. J Clin Psychiatry. 2006;67(7):1114–1123. doi:10.4088/jcp.v67n0715
10. Lang K, Federico V, Muser E, Menzin J, Menzin J. Rates and predictors of antipsychotic non-adherence and hospitalization in medicaid and commercially-insured patients with schizophrenia. J Med Econ. 2013;16(8):997–1006. doi:10.3111/13696998.2013.816310
11. Rabinovitch M, Bechard-Evans L, Schmitz N, Joober R, Malla A. Early predictors of nonadherence to antipsychotic therapy in first-episode psychosis. Can J Psychiatry. 2009;54(1):28–35. doi:10.1177/070674370905400106
12. Stentzel U, van den Berg N, Schulze LN, et al. Predictors of medication adherence among patients with severe psychiatric disorders: findings from the baseline assessment of a randomized controlled trial (Tecla). BMC Psychiatry. 2018;18(1):155. doi:10.1186/s12888-018-1737-4
13. Baros AM, Latham PK, Moak DH, Voronin K, Anton RF. What role does measuring medication compliance play in evaluating the efficacy of naltrexone? Alcohol Clin Exp Res. 2007;31(4):596–603. doi:10.1111/j.1530-0277.2007.00343.x
14. Brannan S. 32.2 two global phase III trials of encenicline for cognitive impairment in chronic schizophrenia patients: red flags and lessons learned. Schizophr Bull. 2019;45(Suppl 2):S141–S2. doi:10.1093/schbul/sbz022.133
15. De Las Cuevas C, de Leon J. Self-report for measuring and predicting medication adherence: experts’ experience in predicting adherence in stable psychiatric outpatients and in pharmacokinetics. Patient Prefer Adherence. 2020;14:1823–1842. doi:10.2147/PPA.S242693
16. Higashi K, Medic G, Littlewood KJ, Diez T, Granström O, De Hert M. Medication adherence in schizophrenia: factors influencing adherence and consequences of nonadherence, a systematic literature review. Ther Adv Psychopharmacol. 2013;3(4):200–218. doi:10.1177/2045125312474019
17. Shahin W, Kennedy GA, Stupans I. The impact of personal and cultural beliefs on medication adherence of patients with chronic illnesses: a systematic review. Patient Prefer Adherence. 2019;13:1019–1035. doi:10.2147/PPA.S212046
 © 2024 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2024 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.


