Back to Journals » Patient Preference and Adherence » Volume 18
Adherence to Anti-Retroviral Therapy (ART) and Its Determinants Among People Living with HIV/AIDS at Bonga, Kaffa, South-West Ethiopia
Authors Tekle A, Tsegaye A , Ketema T
Received 18 October 2023
Accepted for publication 20 February 2024
Published 5 March 2024 Volume 2024:18 Pages 543—554
DOI https://doi.org/10.2147/PPA.S445164
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 5
Editor who approved publication: Dr Jongwha Chang
Asrat Tekle, Arega Tsegaye, Tsige Ketema
Jimma University, College of Natural Sciences, Department of Biology, Jimma, Ethiopia
Correspondence: Tsige Ketema, Email [email protected]
Background: The scaling-up of antiretroviral therapy (ART) is the greatest accomplishment to reduce the burden of acquired immunodeficiency syndromes (AIDS) to date. However, it requires optimal adherence to be effective. Thus, this study was designed to assess the level of adherence of people living with HIV (PLWH) to ART and its determinants in one of the hardest-hit areas with HIV in Ethiopia.
Methods: A health facility-based cross-sectional study design was conducted among adult PLWH, age > 18 years, and receiving ART in southwest Ethiopia. Data was collected by face-to-face interviews following the Self-Rating Scale Item for drug adherence and from participants’ medical cards. The effects of variables related to socio-demographic and socio-economic factors, disease and medication, health facilities, and patients’ behavior on ART adherence were analyzed using a binary logistic regression model. The data was analyzed using R software.
Results: Self-reported good adherence to ART recorded in this study was 73.1% (n =301/412). The risk of poor adherence was significantly higher among those who were divorced, merchants, used ART for longer durationsand were found in stage IV WHO pathogenesis. Contrarily, those who had a positive perception of the effectiveness of ART had significantly better adherence to ART. Longer duration on ART and frequency of pills taken, ≥ 3 pills per day, were significantly associated with a low CD4+ cell count (< 500 cells/mm3). For each unit increase in medication frequency per day, the likelihood of having a high viral load of > 1000 copies/mL was 5.35 times higher.
Conclusion: The ART adherence documented in this study was graded as moderately low. Some variables, such as clinical, medical, and behavioral, were found to affect the adherence of people living with HIV to ART. Hence, care providers should be aware of such variables in the process of treatment, follow-up, and monitoring of people living with HIV in the study area.
Keywords: Adult, ART, adherence, hospital, HIV/AIDS
Introduction
Human immunodeficiency virus (HIV) is one of the globally emerging viruses and is posing a complex threat to humankind. The virus infects cells of the immune system, impairs their function, and increases susceptibility to various opportunistic infectious agents.1 Up to 2022 worldwide, the number of people who died since the emergence of this virus was estimated to be 40.4 million; those living with HIV were 39.9 million, and those accessing ART were only 29 million.2 The incidence rate in 2022 was only 1.3 million globally.2 Sub-Saharan Africa remains among the hardest hit regions by HIV, with nearly 4.2% of people living with HIV, contributing to about two-thirds of the global total of people living with HIV.3 Totally, this region contributes about 76% of total HIV infection to the globe.3
Ethiopia is the second-highest-populated country in Africa. Like any other country in the sub-Saharan region, in Ethiopia, the number of people infected with HIV over the last two decades was estimated to be 943,040.4,5 However, the country has significantly reduced the HIV burden in the last few years, with overall reduced incidence from 3.3% in 2002 to 0.9% in 2017, and AIDS-related deaths also reduced from 83,000 deaths in 2000 to 15,600 in 2017,6 following the scaling-up of ART dispensation in almost all regions of the country.4 In Ethiopia, the highest prevalence was reported from Gambella (4.8%), while the lowest was from Somalia (0.1%).7,8 Among those aware of their serostatus and diagnosed positive, only 59% were receiving antiretroviral therapy (ART). While a significant proportion of people living with HIV were not using the treatment.9 However, unlike other chronic conditions, people living with HIV (PLWH) need to be highly adhered (>80% to 95% adherence) to their therapy for the drug to be effective for a long period and to prevent the emergence of resistant viral strains.10 Hence, poor medication adherence is linked to the development of drug resistance, higher death rates, lower rates of CD4+ cell count, lower therapeutic success, and increased hospitalization.11 Nonetheless, adherence is a complex health behavior that is influenced by the drug regimen itself, patient and family-related factors, and the patient-health provider relationship.12 In Ethiopia, different studies have shown that the level of people living with HIV adherence to their treatment varies (between 70% and 95%) in different regions,13–16 and there are also diverse factors contributing to the observed poor adherence. Likewise, many similar studies were conducted at regional and global levels using a population of diverse cultures, customs, beliefs, livelihoods, societal perceptions toward the HIV infection, demographic characteristics, the magnitude of the HIV burden, the health system, and geographical settings, which could determine the variables identified to influence people’s adherence to ART.17 Variables identified to affect ART adherence in one region might not have a similar effect in another region or locality. Hence, it urges regular monitoring of medication adherence by PLWH residing in such high HIV burden regions to help improve adherence in those particular areas, besides consistent surveillance of the incidence. Therefore, the current study is aimed at assessing the level of ART adherence among adult people living with HIV/AIDS at Gebretsadik Shawo General Hospital, Bonga, Kaffa, southwest Ethiopia.
Methods
Description of the Study Area, and Period
The study was conducted at Gebretsadik Shawo General Hospital, Bonga Town. The hospital is situated in Bonga town, about 449 km southwest of Addis Ababa, the capital of Ethiopia. Geographically, the town is located at a latitude and longitude of 7°16′ 0″N, 36°14′ 0″E, with an elevation of 1714 m. According to the projection made by the National Central Statistical Agency (CSA), the total population of the town is estimated to be 56,045 in 2022.18 In the town, there was one public hospital, one public health center, and many other private health facilities. The hospital provides multi-dimensional services to its visiting clients. The study was conducted from January to August2019.
Study Design and Study Population
A health facility-based descriptive cross-sectional study design was employed. The study population was adult people living with HIV/AIDS (APLWHA) (age above 18 years), those receiving ART at least for five months or more, and those willing to participate in the study. Those people on ART who followed up and resided in the study area for a shorter period of time who were taking pills by a representative, critically ill or mentally unfit, or unwilling to participate in the study were excluded (Figure 1).
 |
Figure 1 Study diagram. |
Data Collection Method
Data were collected through face-to-face interviews using a predesigned and pretested questionnaire prepared in English, which was later translated into the local language (Kafa). For the sake of consistency, all interviews were conducted by the same nurse professional working in the ART clinic of the hospital in the presence of the principal investigator of this study. The factors influencing ART adherence were analyzed across the five dimensions of adherence suggested by the WHO.17 These variables were socio-demographic, and socio-economic factors [ethnicity, educational status, marital status, occupational status, sex, residence, monthly income, age, and living condition], disease-related variables [duration of antiretroviral therapy, the serological status of sex partners, previous history of hospitalization after antiretroviral therapy, experiencing stigma, average CD4+ cells count, and use of treatment other than highly active antiretroviral therapy (HAART), knowledge of adverse effects of ART drug, level of adherence, perception toward the effectiveness of the HAART], and medication and facility related variables [type of 1st line ART regimens, type of 2nd line ART regimens, number of pills take per day, frequency of dose per day and other concurrent medication], and people living with HIV related variables [tuberculosis, fungal infections, depression, heart failure, and others] were considered in the study.17 In addition, the research teams collected immunological data (CD4+ cell count), clinical data (viral load), and length of ART from each person living with HIV and on their ART medical card.
Data Processing and Management
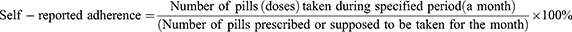
To measure PLWH adherence to ART, a self-reported instrument of missing pills over 30 days was used. Missed pills were further confirmed through pill counting by nurse professionals working in the health facility during participants visited the clinic for their regular follow-up to increase the accuracy of the measurement and reduce potential recall bias. Since there is no standard guideline for estimation of ART adherence, self-reported adherence was classified as being “good adherent” when people living with HIV were asked about their medication (pills) use in the last month and they have taken ≥95% of prescribed pills (more than one dose per day) missed, while those who reported taking <95% of prescribed pills were considered as “poor-adherent” by National AIDS Control Organization (NACO) guidelines.19 Therefore, the percentage of self-reported adherence was determined by calculating the number of pills taken of the number of pills prescribed:
An adherence measurement of 95% or more is classified as good adherent and less than 95% is classified as having poor adherence as per the Ethiopian Federal Ministry of Health Guideline for Comprehensive HIV Prevention, Care and Treatment.19 The overall good adherence of the study participants to ART was computed by dividing the number of self-reported adherence the total participants (n = 412) and multiplying by 100.
Statistical Data Analysis
Data was analyzed using R-software version 4.2.0. Both descriptive (ie frequency, percent, and crosstabs) and inferential (ie logistic regression) statistics were used for the data analysis. Multiple logistic regressions were used in this investigation to find traits associated with adherence to ART. For all analyses significance levels were considered at 95% CI.
Results
Socio-demographic and Clinical Variables
Among the 739 registered people living with HIV/AIDS, 80 of them were excluded at the initial phase of the study due to their age below 18 years. Of the remaining 659 targeted population, 240 were refused to participate in the study. Lastly, complete data was obtained for 412 adult people living with HIV and on ART (Figure 1). Nearly 60% of the people living with HIV were married and two-thirds (68.7%) of them were females. The majority of them (44.9%) were found to be between 26 and 35 years old. Around 76.5% of the people living with HIV were urban inhabitants, lived alone (68.4%), had no history of co-morbidity (65%), and with ≥500 cells/mm3 CD4+ cells count (54.4%), found in stage III WHO category (43.2%), had received less than three pills per day (79.4%) and found with good adherence to their ART regimen (73.1%) (Table 1).
 |
Table 1 Descriptive Summary of Socio-Demographic and Clinical Variables Among Adult People Living with HIV/AIDS at Gebiretsadik Shawo General Hospital. Southwest of Ethiopia |
Findings from the multiple logistic regression analysis revealed that marital status, occupational status, substance use (khat chewing), time since treatment started, status of WHO stage of pathogenesis, perception towards ART, and facing stigma were found to be predictor variables for adherence to the ART among adult people living with HIV in the hospital. Sex, age, level of literacy, place of residence, living condition, CD4+ cells count, number of pills taken per day, and frequency of drug used per day were all found to be not significantly associated with adherence to ART (Table 2).
 |
Table 2 Two Effects of Socio-Demographic and Clinical Factors on the Adherence to ART Among Adult People Living with HIV/AIDS at Gebire Tsadik Shawo General Hospital, Southwest of Ethiopia |
The risk of poor adherence to ART was 5.56 times higher among divorced compared to those with single marital status (95% CI: 1.94,-15.91). Likewise, merchants had 18.18 times higher risk of being poor adherent compared to policemen (95% CI: 2.68–123.51). Those Khat users were 3.33 times more likely to have poor adherence to ART compared to non-khat users. Experiencing self-stigma was 0.44 (95% CI: 0.22–0.85) times less likely to have poor adherence to ART compared to stigma from others. Positive perception towards the effectiveness of ART was 0.33 (95% CI: 0.12–0.88) times less likely to have poor adherence to ART compared to those perceived as ART was ineffective in improving their health status. Those with negative perceptions were 3.03 times more likely to have poor adherence to ART.
In general longer duration (>1 year) of ART is significantly associated with poor adherence. Mainly those using ART for a duration of 6 to 10 years were 5.11 times more likely to have poor adherence to ART (95% CI: 1.76–14.9) than those using the drug for a shorter time (<1 year). Stage IV category of WHO pathogenesis was 3.94 [95% CI: 1.41–11.05] times more likely to have poor adherence to ART compared to stage I.
Effect of Good ART Adherence on Clinical Outcomes
The majority of people living with HIV whose CD4+ cells count <500 cells/mm3 and viral load of >1000 copies/mL were females, found in age range from 26 to 35 years, the serological status of their sex partner was unknown, they were found in stage III WHO pathogenesis, taking less than 3 pills per day, do not have a habit of smoking, chewing khat, drink alcohol, and they were those without comorbidity. Most of the patients with CD4+ cells count <500 cells/mm3 had been on ART therapy for 6 to 10 years, while those with viral loads >1000 copies/mL were on treatment for 11 to 15 years. Longer duration on ART had shown an association with lower mean CD4+ cells count and higher viral load (Table 3).
 |
Table 3 CD4+ Cells Count and Viral Load Status of Among Adult People Living with HIV/AIDS at Gebre Tsadik Shawo General Hospital Southwest of Ethiopia |
To find the effect of good adherence on CD4+ cell count and viral load response, the whole binary logistic regression model was evaluated and predictors were tested for goodness of fit. Relative risk factors with mean CD4+ cells count and viral load outcomes of HIV/AIDS patients with good adherence were identified. Although self-reported good adherence did not show significant association with overall CD4+ cells count (0.92, 95% CI: 0.68 −1.2, p = 0.58), significant reduction of viral load, <1000 copies/mL (1.6, 95% CI: 1.03–2.25, p = 0.037) was observed. People living with HIV with good adherence were 0.29 (95% CI: 0.16–0.52) times less likely to have high viral load than patients with poor adherence (which have 3.5 times more likely to have high viral load), while people living with HIV with high CD4+ cells count (≥500 cells/mm3) were 0.2 (95% CI: 0.18–0.39) times less likely to have high viral load (lower CD4+ cells count were 5.13 times more likely to have high viral load). A unit increase in drug frequency in a day increased the risk of having a high level of viral load in the blood by 3.15 (95% CI: 1.8–5.52). For treatment time from 6 to 10 years, the patients were 2.78 (95% CI: 1.27–6.1) times more likely to have <500 CD4+ cells count when compared to those who had received less than a year of treatment. For each unit increase in medication frequency in a day, CD4+ cells count <500 cells/mm3 was 8.88 (95% CI: 4.12–19.15) times higher. People who took less than three pills per day were 2.69 (95% CI: 1.13–6.4) times more likely to have a CD4+ cells count of <500 cells/mm3 compared to people living with HIV who took three to five pills per day. Three or more pills reduced the likelihood of having a CD4+ cells count of <500. For each unit increase in medication frequency in a day, the viral load of >1000 was 5.35 (95% CI: 2.6–11.2) times higher. In HIV/AIDS patients on ART at Gebre Tsadik Shawo General Hospital, Bonga town, time since treatment started, number of pills taken per day, and drug frequency per day were found to be associated with ART adherence and CD4+ cells count, while drug frequency in a day was found to be affected current viral load. Age, gender, WHO stage of pathogenesis, existing comorbidity, partner’s serological status, khat use, smoking, and alcohol use were not influenced by ART adherence and impacted CD4+ cells count (Table 4).
 |
Table 4 Effect of Good Adherence on Mean CD4+ Cell Count and Viral Load Response Among Adult People Living with HIV/AIDS at GebreTsadik Shawo General Hospital, Southwest of Ethiopia |
Discussion
To adequately suppress the viral replication, produce long long-lasting response and stop the disease progression, ensuring >95% ART adherence was suggested a long ago.17 However, in this study, only 73.1% (301/412) self-reported adherence was documented, which is lower than the set reference (>95%). Also, the level of ART adherence observed in this study was lower than reports from selected Hospitals in West Wollega, Ethiopia (87.5%), Western Ethiopia (78.2%) and North-west Ethiopia (80.9%).14–16 While it was better ART adherence than reports from Pakistan (55%), USA (60%) and India (68%).20–22 The heterogeneity observed in these different studies might be accountable to the measurement methods used since there is no gold standard measurement of ART adherence or time of study, study setting/geographical location, differences in culture and tradition of the community, differences in the study designs, and definitions of adherence referred and contexts of the patients. There is also evidence demonstrating the difficulty of measuring adherence in the outpatient setting with absolute precision and accuracy as it may result in recall biases due to its dependence on only the use of patients’ self-reports or pill count.1
Further, in line with prior reports, socio-demographic factors such as marital status, occupational status, substance use (khat, natural stimulant, use), clinical status and treatment-related factors were highly interlinked and were found to contribute to the poor adherence to ART.16,23 The aftermath of this poor adherence to ART could speed up the emergence of drug-resistant viral strains, increase mortality rates, less effective viral suppression, poor treatment outcomes, increased susceptibility to other opportunistic infections, and different comorbidities.10,11,24,25 This was further evidenced in the study through the fact that there was a significant positive association between the advanced WHO clinical stage (stage IV WHO pathogenesis when the severely symptomatic stage appears) and poor adherence to ART. Also, according to the World Health Organization suggestion when the ART adherence rate fails to the level between 50% and 85%, the probability of the emergence of drug resistance could become very high.26
Viral load and CD4+ cell count are the two surrogate markers of antiretroviral therapy responses and HIV disease progression used to manage and monitor HIV infection.27 Accordingly, good adherence to ART is required to consistently suppress the viral load, sustain high CD4+ cell count, prevent the onset of AIDS, prolong survival, and reduce the risk of opportunistic infections and HIV transmission.28,29 In agreement with this scenario, although significant improvement of CD4+ cell count was not observed among self-reported good ART adherent participants, viral load was significantly suppressed. This is supported by similar studies from Ethiopia, where high CD4+ cell count (≥500 cells/mm3) was positively associated with good ART drug adherence30 and a comprehensive systematic review and meta-analysis by Peter et al,31 which revealed the majority of studies included in the review were found no differences on the odds of adherence when comparing CD4+ cells count strata.32 However, CD4+ cell count remains the best monitor of a patient’s immunity and clinical status, the risk of opportunistic infections, and supports diagnostic decision-making, particularly for patients with advanced HIV disease. Besides improving the health status of HIV patients, sustainable adherence to ART could improve the durability of antiretroviral agents, reduce the development of drug-resistant HIV, and help long-term control of HIV infection.28,29 Likewise, another study revealed that the optimum level of adherence to ART was associated with significant viral load reduction.30 Thus, the observed significant association between ART good adherence and lower viral load is an indication of improved clinical outcomes for HIV/AIDS patients.
Another variable found to be strongly associated with improved CD4+ cells count was number of pills taken per day. As the number of pills taken per day decreased (<3 pills), significantly better adherence to ART and lower risk of hospitalization were reported.31 As ART adherence improves, the count of CD4+ cells will be improved.32 In addition, adherence was affected by the frequency of pills taken per day, as more frequent use of pills per day is associated with poor ART adherence.33 Therefore, those HIV/AIDS patients on ART and taking pills frequently (twice or three times a day) and take it in higher doses (>3 pills) require regular check-ups and monitoring of their condition, to take appropriate measures before the disease progression and ultimately leading to hospitalization or death.
Limitation of the Study
As this study is primarily based on the response rate of the study participants, their willingness to participate in the study as well as genuine responses is essential. However, a substantial number of the study participants were not willing to take part in the study, which could limit the generalizability of the findings to the study setting.
Conclusion
The overall self-reported ART adherence observed in this study can be referred to as moderately low ART adherence, and it is very far from the recommended adherence. Some socio-demographic and clinical variables were found to be significantly associated with ART adherence. This should signal concerned health authorities to relook into the current ART delivery service, and they should urgently work on enhancing awareness of these PLWH, mainly in light of the consequences of their negligence. Therefore, care providers should do proper follow-up, monitoring the clinical conditions and infection status of PLWH on ART, to improve their health status and disease outcomes.
Data Sharing Statement
The authors confirm that data supporting the results of this study are available in the article. Raw data supporting the results of this study are available from the corresponding author upon reasonable request.
Ethical Approval and Consideration
The study was ethically approved by Research and Ethical Review Board members of the College of Natural Sciences, Jimma University, dated 23 Oct 2019, Ref. No. RPG/18/2019. Initially, an official letter was sent to the hospital for the study cooperation. Data was collected after permission was obtained from the officials, and consent was earned from each participant. The participants were informed about the purpose of the study before data collection. Data was collected only from those who were willing to participate and confidentiality was maintained. The study fulfills the Declaration of Helsinki.
Acknowledgments
The authors would like to thank health authorities at all levels for permitting to conduct of the study and the study participants for their willingness to be recruited and their genuine responses. The authors would also like to thank Jimma University for the financial support of this study.
Disclosure
The authors declare that they have no conflicts of interest in this work.
References
1. Koyra HC. Adherence to Antiretroviral Therapy among Adult Persons Living with HIV/AIDS in Southern Ethiopia. Inter J Virology and AIDS. 2018;5(1):2469–2567.
2. UNAIDS. Global HIV & AIDS statistics — fact sheet. Global HIV & AIDS statistics — fact sheet. UNAIDS; 2023.
3. Rosenberg NE, Shook-Sa BE, Liu M, et al. Adult HIV-1 incidence across 15 high-burden countries in sub-Saharan Africa from 2015 to 2019: a pooled analysis of nationally representative data. Lancet. 2023;10(3):175–185. doi:10.1016/S2352-3018(22)00328-9
4. FHAPCO. HIV/AIDS national strategic plan for Ethiopia, 2021-2025; 2020.
5. Center for Disease Control and Prevention (CDC) Ethiopia. Global HIV and TB. Ethiopia Country Profile (cdc.gov); 2021.
6. HAPCO. HIV prevention in Ethiopia National Road map. 2018.
7. Federal Ministry of Health (FMOH). HIV Prevention in Ethiopia National Road Map 2018 – 2020. Addis Ababa, Ethiopia: Federal HIV/AIDS Prevention and Control Office: Federal Ministry of Health, Ethiopia; 2018.
8. Kibret GD, Ferede A, Leshargie CT, et al. Trends and spatial distributions of HIV prevalence in Ethiopia. Infect Dis Poverty. 2019;8(1):90. doi:10.1186/s40249-019-0594-9
9. Ethiopian public health institute (EPHI). HIV related estimates and projections for Ethiopia–2017. Addis Ababa: Ethiopian public health institute; 2017.
10. Cevik M, Orkin C, Sax PE. Emergent resistance to dolutegravir among INSTI-naive patients on first-line or second-line antiretroviral therapy: a review of published cases. Open Forum Infect Dis. 2020;7(6):ofaa202. doi:10.1093/ofid/ofaa202
11. Benson C, Wang X, Dunn KJ, et al. Antiretroviral Adherence, Drug Resistance, and the Impact of Social Determinants of Health in HIV-1 Patients in the US. AIDS Behav. 2020;24(12):3562–3573. doi:10.1007/s10461-020-02937-8
12. Villiera JB, Katsabola H, Bvumbwe M, et al. Factors associated with antiretroviral therapy adherence among adolescents living with HIV in the era of isoniazid preventive therapy as part of HIV care. PLOS Glob Public Health. 2022;2(6):e0000418. doi:10.1371/journal.pgph.0000418
13. Fite RO. Association between adherence to Antiretroviral Therapy and place of residence among adult HIV infected patients in Ethiopia: a systematic review and meta-analysis. PLoS One. 2021;16(9):e0256948. doi:10.1371/journal.pone.0256948
14. Dibaba D, Kajela G, Chego M, et al. Antiretroviral Treatment Adherence Level and Associated Factors Among Adult HIV-Positive Patients on Both HIV/AIDS Care Models: comparative Study in Selected Hospitals of Western Ethiopia, 2019. HIV AIDS. 2021;13:1067–1078.
15. GebreEyesus F, Mitku D, Tarekegn T, et al. Levels of Adherence and Associated Factors Among Children on ART Over Time in Northwest, Ethiopia: evidence from a Multicenter Follow-Up Study. HIV AIDS. 2021;13:829–838. doi:10.2147/HIV.S323090;.
16. Tolossa T, Wakuma B, Mulisa D, et al. ART Adherence Among People Living with HIV Seeking Services from Public Health Facilities in Western Ethiopia. HIV/AIDS Res Palliative Care. 2021;13:1149–1158.
17. Alvi Y, Khalique N, Ahmad A, et al. World Health Organization dimensions of adherence to antiretroviral therapy: a study at antiretroviral therapy center, Aligarh. Indian J Community Med. 2019;44:118–124. doi:10.4103/ijcm.IJCM_164_18
18. Central Statistical agency (CSA). Population Statistics, Charts, Map & Location. Bonga Town, Ethiopia; 2022. Available from: https://www.citypopulation.de/en/ethiopia/admin/south.west/ET070911_bonga.
19. Federal Ministry of Health (FMOH). Ethiopia. National Consolidated Guidelines for Comprehensive HIV Prevention, Care and Treatment. Addis Ababa: FMOH Ethiopia; 2018.
20. Iversen J, Qureshi SUH, Zafar M, et al. Adherence to antiretroviral therapy among HIV positive men who inject drugs in Pakistan. Int J Drug Policy. 2021;96:103281. doi:10.1016/j.drugpo.2021.103281
21. Piña C, Dange A, Rawat S, et al. Antiretroviral Treatment Uptake and Adherence Among Men Who Have Sex With Men and Transgender Women With HIV in Mumbai, India: a Cross-Sectional Study. J Assoc Nurses AIDS Care. 2018;29(2):310–316. doi:10.1016/j.jana.2017.10.001
22. McComsey GA, Lingohr-Smith M, Rogers R, Lin J, Donga P. Real-World Adherence to Antiretroviral Therapy Among HIV-1 Patients Across the United States. Adv Ther. 2021;38(9):4961–4974. doi:10.1007/s12325-021-01883-8
23. Addo MK, Aboagye RG, Tarkang EE. Factors influencing adherence to antiretroviral therapy among HIV/AIDS patients in the Ga West Municipality, Ghana. IJID Reg. 2022;3:218–225. doi:10.1016/j.ijregi.2022.04.009
24. Abadiga M, Hasen T, Mosisa G, Abdisa E. Adherence to antiretroviral therapy and associated factors among Human immunodeficiency virus positive patients accessing treatment at Nekemte referral hospital, west Ethiopia, 2019. PLoS One. 2020;15(5):e0232703. doi:10.1371/journal.pone.0232703
25. Carr A, Mackie NE, Paredes R, Ruxrungtham K. HIV drug resistance in the era of contemporary antiretroviral therapy: a clinical perspective. Antiviral Ther. 2023;28(5). doi:10.1177/13596535231201162
26. Angelo AT, Alemayehu DS. Adherence and Its Associated Factors among Adult HIV-Infected Patients on Antiretroviral Therapy in South Western Ethiopia, 2020. Patient Prefer Adherence. 2021;15:299–308. doi:10.2147/PPA.S298594
27. World Health Organizations. Guideline on When to Start Antiretroviral Therapy and on Pre-Exposure Prophylaxis for HIV. Geneva: World Health Organizations; 2015:978–992.
28. Panel on Antiretroviral Guidelines for Adults and Adolescents. Guidelines for the Use of Antiretroviral Agents in Adults and Adolescents with HIV. Department of Health and Human Services; 2022. Available from: https://clinicalinfo.hiv.gov/en/guidelines/adult-and-adolescent-arv.
29. Byrd KK, Hou JG, Bush T, et al. Adherence and viral suppression among participants of the patient-centered human immunodeficiency virus (HIV) care model project: a collaboration between community-based pharmacists and HIV clinical providers. Clin Infect Dis. 2020;70:789–797. doi:10.1093/cid/ciz276
30. Desta AA, Kidane KM, Woldegebriel AG, et al. Level of Adherence and Associated Factors Among HIV-Infected Patients on Antiretroviral Therapy in Northern Ethiopia: retrospective Analysis. Patient Prefer Adherence. 2020;14:1585–1594. doi:10.2147/PPA.S268395
31. Mohd Salleh NA, Richardson L, Kerr T, et al. A Longitudinal Analysis of Daily Pill Burden and Likelihood of Optimal Adherence to Antiretroviral Therapy Among People Living With HIV Who Use Drugs. J Addict Med. 2018;12(4):308–314. doi:10.1097/ADM.0000000000000403
32. Fiseha T, Ebrahim H, Ebrahim E, Gebreweld A. CD4+ cell count recovery after initiation of antiretroviral therapy in HIV-infected Ethiopian adults. PLoS One. 2022;17(3):e0265740. doi:10.1371/journal.pone.0265740
33. Mantell JE, Zech JM, Masvawure TB. Implementing six multi-month dispensing of antiretroviral therapy in Ethiopia: perspectives of clients and healthcare workers. BMC Health Serv Res. 2023;23(1):563. doi:10.1186/s12913-023-09549-7
 © 2024 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2024 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.