Back to Journals » Breast Cancer: Targets and Therapy » Volume 15
A Review on the Management of Peripheral Neuropathic Pain Following Breast Cancer
Authors Avila F, Torres-Guzman R, Maita K, Garcia JP, De Sario GD, Borna S, Ho OA, Forte AJ
Received 22 April 2023
Accepted for publication 9 October 2023
Published 30 October 2023 Volume 2023:15 Pages 761—772
DOI https://doi.org/10.2147/BCTT.S386803
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Professor Robert Clarke
Francisco Avila, Ricardo Torres-Guzman, Karla Maita, John P Garcia, Gioacchino D De Sario, Sahar Borna, Olivia A Ho, Antonio J Forte
Division of Plastic Surgery, Department of Surgery, Mayo Clinic, Jacksonville, FL, USA
Correspondence: Antonio J Forte, Mayo Clinic Florida, 4500 San Pablo Roads, Jacksonville, FL, 32224, USA, Tel +1 904-953-2073, Email [email protected]
Abstract: Postmastectomy pain syndrome (PMPS) is a common and debilitating form of postsurgical pain with neuropathic characteristics, presenting as burning, stabbing, or pulling sensations after mastectomy, lumpectomy, or other breast procedures. With a prevalence of 31%, the risk factors for PMPS include younger age, psychosocial factors, radiotherapy, axillary lymph node dissection, and a history of chronic pain. This review evaluates the pharmacological and surgical options for managing PMPS. Pharmacological treatment options include antidepressants, gabapentinoids, levetiracetam, capsaicin, and topical lidocaine. Procedural and surgical options include fat grafting, nerve blocks, radiofrequency ablation, peripheral nerve surgery, serratus plane block, and botulinum toxin injections. Despite the variety of therapeutic options available for patients, further randomized trials are required to conclude whether these treatments reduce the intensity of neuropathic pain in patients with PMPS. In particular, comparative studies and the inclusion of patients across a range of pain intensities will be essential to developing a treatment algorithm for PMPS. In conclusion, current management for these patients should be tailored to their individual requirements.
Keywords: postmastectomy pain syndrome, postsurgical pain, neuropathic pain, neuralgia, breast neoplasms, Mastectomy
Introduction
Postmastectomy pain syndrome is a debilitating form of chronic persistent postsurgical pain (PPSP) with neuropathic characteristics. Patients often describe this pain as burning, stabbing, or pulling sensations localized in the anterior thorax, axilla, or upper medial arm, generally ensuing after mastectomy, lumpectomy, or other breast-related surgical procedures.1–3 Several authors have advocated for a broader term, post-breast surgery pain syndrome (PBSPS).3 The most recent modifications to this definition, dating from more than five years ago, include its presence for at least 6 months, occurring at least 50% of the time, and exacerbated by shoulder girdle movements.3
Postmastectomy pain syndrome is widely attributed to local nerve damage, most commonly to the intercostobrachial nerve (ICBN).4 Other theorized origins include intraoperative damage to pathways of the axillary nerve, neuroma formation, and nerve entrapment due to scar fibrosis.5 Furthermore, studies have observed a diminished density of intraepidermal nerve fibers in mastectomy scars, suggesting the presence of small fiber neuropathy.6
Prevalence rates can be as high as 31.3% among all patients treated for breast cancer and surge to 57.1% among those experiencing postoperative pain, depending on the evaluation method.7 Certain risk factors such as younger age, psychosocial factors, radiotherapy, axillary lymph node dissection, increasing acute postoperative pain, and a history of chronic pain, among others, have been identified.8–12 Recent findings also indicate that a history of opioid or alcohol use was recently found to be associated with increased pain in patients with PMPS.13
There is no definitive treatment standard for treating PMPS. This review aims to explore the range of available pharmacological and surgical options for those grappling with this condition. While a comprehensive understanding of PMPS may also include pain stemming from the musculoskeletal system and lymphedema-related pain,14 the focus of this review will remain on managing the neuropathic aspect of pain following breast cancer surgery.
Types of Treatment
Pharmacological
A summary of the results is available in Table 1.
 |
Table 1 Pharmacological Management |
Antidepressants
Amitriptyline is a tricyclic antidepressant that has been used to treat a variety of neuropathic chronic pain conditions, including PMPS. This drug’s mechanism of action, which involves the inhibition of serotonin and norepinephrine reuptake, increases neurotransmitter availability and improves brain pain regulation. Amitriptyline is frequently one of the drugs of choice for chronic neuropathic pain syndromes.15 To the best of our knowledge, Eija et al were the first to investigate the use of amitriptyline in patients with PMPS.16 Theirs was a randomized, double-blind, placebo-controlled crossover study enrolling 15 patients. The initial dose was 25 mg and escalated to 100 mg daily in 4 weeks.16 The drug substantially improved neuropathic pain in the arm and breast scar, with 8 patients having at least a 50% decrease in pain intensity.16 As with other pathologies requiring this medication, it is typically administered in low doses initially and gradually increased as needed to achieve a therapeutic effect. Therefore, optimal dosage and treatment duration may vary. Possible amitriptyline adverse effects include drowsiness, dry mouth, constipation, blurred vision, and weight gain.17 Since high doses might harm cardiovascular health, it is vital to titrate to the lowest possible dose that provides satisfactory pain relief.
Considering the adverse events observed with amitriptyline, another antidepressant, venlafaxine, was studied by the same group of authors.18 Venlafaxine belongs to a group of medications known as serotonin-norepinephrine reuptake inhibitors, and therefore its direct effect is increasing the levels of these neurotransmitters in the brain. Preclinical studies show that the analgesic effect of venlafaxine might differ depending on the type of neuropathic pain, with different adrenergic and serotoninergic receptors involved.19 The side effects of venlafaxine include nausea, dry mouth, dizziness, and drowsiness.20 As with the past study, this was a randomized, double-blind, crossover comparison of venlafaxine and placebo in 13 patients lasting 10 weeks.18 The authors increased the dose by one tablet (18.75 mg) weekly.18 Pain relief was significantly better, and pain intensity was significantly lower in the venlafaxine group.18 Higher blood venlafaxine concentrations were observed in patients with improved pain relief.18 Thus, the authors conclude that higher doses of the drug could be used to improve neuropathic pain.18 A recent review by Aiyer, Barin, and Bhatia on using venlafaxine for neuropathic pain, regardless of the cause, also found that higher drug doses showed significantly higher pain relief.21 However, they also state that venlafaxine did not perform better when compared with other neuropathic medications.21 Considering its widespread use for neuropathic pain, further research is required to elucidate this drug’s appropriate dosage and uses.21
Anticonvulsants
This class of drugs includes gabapentin and pregabalin, anticonvulsant drugs that are now commonly prescribed for neuropathic pain and PMPS. Their mechanism of action involves binding to voltage-gated calcium channels in the central nervous system, reducing the release of neurotransmitters involved in pain signaling.22 In a systematic review by Rai et al, both drugs were found to decrease opioid consumption after mastectomy when administered perioperatively, but only gabapentin reduced pain 24 hours after the surgery.23 Furthermore, gabapentin was also observed to produce improved pain relief compared to stellate ganglion block (SGB).24 However, these patients also had a lower quality of life.24 Additionally, the combination of gabapentin, NSAIDs, and morphine led to significantly lower pain intensity compared to groups receiving gabapentin and NSAIDs or gabapentin alone three weeks after initiating treatment.25 Of note, the latter study included patients with neuropathic pain after any treatment for breast cancer, including surgery, chemotherapy, and radiotherapy.25 Despite showing positive results regarding pain intensity, further studies are needed to elucidate whether gabapentin leads to sustained pain relief and the appropriate dosage.
Regarding pregabalin, recent evidence has shown that 75 mg of the drug taken twice daily for one week, starting the day of the surgery, could reduce the frequency of PMPS.26 Moreover, Kaur et al found that pregabalin significantly reduced pain intensity in patients with an established diagnosis of PMPS after one month of treatment with 75 mg of the drug twice daily.27 Considering the scarcity of evidence on the use of pregabalin for PMPS, research on the efficacy of this drug in reducing neuropathic pain in patients with PMPS is warranted. Currently, in the setting of widespread gabapentinoid use for PMPS, the available evidence shows that gabapentin, either alone or in combination with other drugs, could have better symptomatology relief in these patients.
Although incompletely understood, levetiracetam’s primary mechanism of action is believed to involve binding to the synaptic vesicle protein 2A, decreasing the release of certain excitatory neurotransmitters like glutamate in the central nervous system.28 Vilholm et al conducted a randomized, double-blind, placebo-controlled, crossover study on using levetiracetam for PMPS.29 The treatment schedule consisted of two treatment phases of 4 weeks each with either 1500 mg of levetiracetam twice daily or a placebo.29 The authors found no difference in pain intensity scoring between the two groups.29 Therefore, levetiracetam cannot be recommended for treating PMPS with the available evidence.
Capsaicin
Capsaicin, a compound found in chili peppers,30 has been used to treat neuropathic pain following breast cancer treatment. This compound is thought to bind to vanilloid receptors on pain-sensing nerve cells, inhibiting the transmission of pain signals to the central nervous system. Several studies have applied capsaicin topically to treat post-mastectomy pain syndrome (PMPS), using different concentrations and application frequencies.
One study used a 0.025% capsaicin solution, applied four times a day for four weeks, leading to significant pain relief in most of the participants.31 Another study used a 0.075% capsaicin solution, also applied four times daily for six weeks, which significantly reduced jabbing pain and pain severity scores.32 A third study used a 0.025% capsaicin solution applied three times daily for two months, leading to complete pain relief in 10.5% of patients, and substantial pain improvement in 57.9% of patients.33 A more recent case report described the use of 8% capsaicin patches for 30 minutes, applied after a 30-minute treatment with a topical anesthetic.34 High-concentration patches (179 mg) have also been used, resulting in significant pain release.35
However, these treatments are associated with a burning sensation, which can compromise patient comfort. Despite the frequent recommendation to use local anesthetics to prevent this sensation, a recent study has shown that cooling the skin might be better at preventing it.36 While lower concentrations of capsaicin (in cream form) might be better tolerated,37 higher concentrations seem to provide longer-lasting effects.38 Further high-quality clinical trials are necessary to determine the optimal dosage and delivery method for treating PMPS with capsaicin.
Topical Lidocaine
Although lidocaine patches are part of the treatment guidelines for neuropathic pain of different etiologies,39 evidence is scarce regarding its use in patients with PMPS. Garzon-Rodriguez et al conducted a prospective, descriptive, non-controlled, non-randomized study on using lidocaine 5% patches as co-analgesic in patients with cancer pain.40 The study showed that these patches were effective in the short-term management of cancer pain accompanied by allodynia deriving from a scar or a chest wall tumor.40 The study does not provide specific details on which patients had PMPS.40 Studies should be performed on patients with a diagnosis of PMPS to determine the efficacy and safety of these patches in this population and increase the available topical management options.
Procedural
A summary of the results is available in Table 2.
 |
Table 2 Procedural Management |
Fat Grafting
To our knowledge, Caviggioli et al were the first to describe autologous fat grafting for treating PMPS under the hypothesis that the fat graft could improve tissue differentiation, alleviate nerve entrapment by scar softening, and promote an anti-inflammatory effect.5 In their trials in patients undergoing mastectomy or lumpectomy with subsequent radiotherapy, the authors found a significant decrease in pain intensities as evaluated using the Visual Analog Scale (VAS) one year after treatment.5,41,42 Further trials showed smoking status, axillary dissection, and aromatase inhibitors could be associated with a reduced therapeutic effect.43 Despite these initial findings, a recent randomized clinical trial (RCT) showed that autologous fat grafting was not superior to a placebo in reducing pain, including the neuropathic characteristics or quality of life in patients with PMPS.44 As the authors of the RCT state, pain areas differed in size in their study; however, all patients received the same amount of fat.44
One of the key differences between these and previous studies is the fat processing technique. While the initial studies used aspiration with a 3.5-mm cannula and fat centrifugation, Sollie et al used a 2-mm cannula and fat decantation.5,41–44 As stated by Minghao, the first author group’s graft was highly purified but with more damaged adipocytes.45 Simultaneously, the second was characterized by lower purification with a more preserved adipocyte integrity.45 The scarcity of data on this topic makes it impossible to state which method is better for fat grafting in PMPS. A meaningful discussion was presented by Lisa et al on the effect of “needleotomy”, where the surgeons break fibrotic tissue using the injection needle, thus releasing tension in the tissue underneath the scar.46 The authors argue that the tension release inherently alleviates pain,46 and can therefore be considered a confounding factor. However, the effect of this action might be negligible.47
Ultimately, the studies proving a positive effect of fat grafting for PMPS were smaller, non-randomized studies with less rigorous methods, except that by Juhl et al.6 The latter was an RCT that, despite showing positive results, did not include a control intervention group.6 Furthermore, the two RCTs in the literature contain contrasting results. Considering the previous information and that Sollie et al’s methodology was more robust and had a control intervention group receiving normal saline instead of a fat graft, fat grafting cannot be currently recommended with the available data. More RCTs are required to conclude whether this treatment reduces neuropathic pain in patients with PMPS.
Nerve Blocks
Nerve blocks are most commonly performed in the perioperative setting to decrease the risk of PMPS. Thoracic paravertebral blocks (PVB) consist of injecting local anesthetic medication into the paravertebral space adjacent to the thoracic vertebrae and have long been proven effective at improving postoperative pain control.48 There are few cases described in the literature where authors used nerve blocks as a form of treatment instead of a prevention method when the patients had already developed chronic neuropathic pain. Among the first reports of using these procedures for PMPS is that by Miller, Johnston, and Hosobuchi in 1975.49 The authors performed a series of injections using 10% ammonium sulfate in a group of patients with intercostal neuralgia, out of which six of them were postmastectomy patients.49 Despite being highly efficient for post-thoracotomy patients, only three postmastectomy patients had moderate to maximum pain relief 72 hours after injection, and one had relief lasting more than 90 days.49
Another relevant blocking procedure is the SGB, which has been used therapeutically in patients with an established diagnosis of PMPS and for those with cancer-related neuropathic pain.50 This procedure is performed under imaging guidance to ensure accurate needle placement and injection of the local anesthetic, thus decreasing the risk of complications.51 The imaging methods to perform this procedure can be divided into fluoroscopic and non-fluoroscopic.51 Non-fluoroscopic approaches include magnetic resonance imaging, computerized tomography, and ultrasound.51 Despite being simpler, exposing the patient to less radiation, and not needing contrast dye, they might sometimes be time-consuming and impractical.52 As with other types of nerve blocks, the duration of pain relief often varies, with some patients requiring multiple injections or trialing of other pain management strategies. The anatomy and composition of the stellate ganglion can also predispose patients to uncomfortable side effects, such as Horner syndrome.52 Another critical disadvantage of the SGB is the fact that an incomplete sympathetic block can lead the patients to still require pain medication after the procedure.52
Two different anatomical approaches exist for SGB, the anterior and oblique approaches. Although both were found to be effective at reducing PMPS using the VAS, Nabil Abbas et al’s cohort consisted of patients with neuropathic symptoms lasting less than 8 weeks.52 Considering that the IASP’s definition of chronic neuropathic pain states that pain should last more than 6 months to be categorized as such, it is crucial to develop homogenized protocols including patients with long-lasting pain to accurately evaluate the effectiveness of these approaches. Additionally, the anatomical plane in relation to the cervical prevertebral fascia in which the anesthetic is injected might influence the patient’s improvement, as observed by Elramely et al.53 In their clinical trial, the authors found a higher degree of pain relief when performing an ultrasound-guided injection of anesthetic subfascially than extrafascially, therefore concluding that a subfascial approach with a lower amount of anesthetic could provide positive results for patients with PMPS.53
Radiofrequency Ablation
Radiofrequency (RF) ablation is a technique that involves using an electrical current to heat and destroy nerve tissue. There are multiple radiofrequency procedures, including the thermal, pulsed, water-cooled, and cryoneurolysis approaches.54 The complications associated with RF ablation are nerve damage, infection, bleeding, and even increased pain.54 The most widely used methods in PMPS are thermal and pulsed RF. Thermal RF consists of delivering a continuous electrical current, achieving higher temperatures and more predictable tissue lysis.54 This method has been previously tested by Hetta et al, who described its successful use for ablation of the thoracic sympathetic ganglia at the level of T2, T3, and T4 for the treatment of neuropathic pain in patients with PMPS.55 Pulsed RF consists of delivering the electrical current in short bursts.54 Although this method does not achieve the same high temperatures as thermal RF and does not entirely provide tissue lysis, it can alter tissue function to create a neuromodulatory effect. However, it usually provides more temporary pain relief than thermal RF. Abbas and Reyad observed this in stellate ganglion ablations, where they found that although there was no significant difference in the patients’ quality of life or their functional capacity, patients that underwent thermal RF of the stellate ganglion had a more successful and sustained response compared to those in the pulsed RF group.56 Importantly, as considered by Hetta et al in their inclusion criteria, this treatment should be considered in patients who have had a failed course of medical treatment and a positive response to nerve blocks.55 Moreover, the studies considered patients with a VAS score of at least 4, pointing to the limited use of this procedure for patients with moderate to severe pain.
Peripheral Nerve Surgery
After postoperative complications have been excluded and conservative therapy has failed to provide pain relief to the patient, the possibility of peripheral nerve injury, and therefore PMPS, should be strongly considered.57 To confirm the diagnosis and to assess the patient’s candidacy for surgery, many authors propose using the Tinel’s sign to identify the painful area, followed by performing a series of consecutive nerve blocks in the distribution of the intercostobrachial nerve to identify the compromised structure.57,58 Peripheral nerve surgery is indicated if the patient has a pain reduction of 5 points on self-evaluation scales.57 Among the surgical procedures used to treat PMPS due to nerve injury or neuroma formation, the most important are resection of the neuroma, neurorrhaphy, and neurectomy with stump transposition.59
Neurectomy aims to interrupt the abnormal discharge from the distal pain receptor to the central nervous system by proximally transecting the affected nerve.60 This procedure has been used for thoracic pain secondary to intercostal nerve surgery or trauma with positive results.61,62 In the specific subset of patients that develop PMPS, recent retrospective studies showed that one or more neurectomies significantly reduced pain intensity in these patients from a median of 9 in the VAS to a median of 1, four months after the procedure.63 Although other authors have also described positive results with this type of procedure,57 neuropathic pain might recur, in some cases, even one month after the surgery.57 Therefore, long-term follow-up of these patients is required to evaluate the effectiveness of this procedure.
Although scarce, the literature points to neuromas as the cause of PMPS in many patients with damaged ICBN. Kim and Spiess describe a case of a patient who was found to have a surgical clip and an associated neuroma on the ICBN branch causing the pain.64 Furthermore, case series have described observational associations between PMPS and neuroma formation, with pain receding after neuroma excision and nerve transposition.58 Importantly, neuromas can also present as a consequence of traumatic injury during surgery and might cause pain when localized over the surgical scar with a positive Tinel sign.58,59
Serratus Plane Block
The serratus plane block (SPB) is a type of regional anesthesia that involves the ultrasound-guided injection of local anesthetic into one of the potential spaces between the serratus anterior muscle, the latissimus dorsi (superficial plane), and the parietal pleura and ribcage (deep plane) (see Figure 1).65 Although this block primarily targets the intercostal nerves, it can also affect the ICBN.66 Thus, it provides analgesia to the chest wall, axilla, and upper arm, relieving patients with PMPS. Most importantly, this procedure can be performed in an outpatient setting without increasing patient risk.67
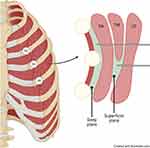 |
Figure 1 Serratus plane blocks. Superficial and deep planes for serratus plane blocks, as described by Blanco et al.65 Created with biorender.com. Abbreviations: SA, serratus anterior; TM, teres minor; LD, latissimus dorsi. |
A recent case series by Zocca et al provides insight into the authors’ experience using the superficial plane block with lidocaine and methylprednisolone in patients with PMPS.66 Theirs was a retrospective study of eight women with postmastectomy pain who, although not with a specific diagnosis of PMPS, all had pain of neuropathic characteristics without a precise duration.66 The authors found that improvement initially varied from 25% to almost complete pain relief and lasted from two days to 12 weeks.66 Considering it was a heterogeneous group of women regarding cancer treatment and previous pain management strategies were not available,66 there is not a specific group of patients for which this procedure could be recommended. However, patients with a second anesthetic injection had more sustained pain relief; therefore, the authors advocate for repeating the block as needed with a minimum interval between the procedures of two months.66
In a different SPB case series of four patients, Liu et al achieved adequate pain relief in three patients using a combination of bupivacaine and triamcinolone.68 Only two patients reported classic symptomatology associated with neuropathic pain.68 Both patients had been on neuropathic pain medication regimens without success.68 The first case achieved pain improvement of 90%, after which she could resume activities of daily living.68 The second was initially treated with an ICBN block, after which she developed tightness in the area.68 For this, the authors performed a series of three SPBs, after which the feeling improved substantially.68 Considering this and that the rest of the patients had an improvement in feelings of tightness in the surgical area, the authors concluded this procedure could be ideally performed in patients with complaints of these characteristics.68
Piracha et al report four cases in which a deep SPB was used in patients with PMPS.69 All patients had severe pain of neuropathic characteristics and had either had a previous unsuccessful superficial SPB or the superficial SPB was not possible due to scarring of the plane.69 All patients achieved pain relief but, as with the superficial SPB described by other authors, required more than one block.69 It is possible that no plane is superior to the other but that specific subsets of patients benefit from a block in these different areas.69
Maranto, Strickland, and Goree describe the case of a 42-year-old woman with a 16-month history of postmastectomy pain with some neuropathic characteristics such as allodynia and hyperalgesia.67 Previous management with lidocaine patches, naproxen, gabapentin, and ketamin did not relieve pain.67 The reported patient also had temporary relief with intercostal nerve blocks (T2 through T5) and a pectoralis nerve block type 1 (PEC-1), after which she experienced severe pain exacerbation.67 The authors decided to perform a combined superficial and deep SPB with bupivacaine, dexamethasone, and clonidine.67 She had complete pain relief until after eight weeks, when she reported pain intensity of 5/10.67 A second block was performed at 12 weeks, providing complete symptom relief.67 The authors of this case report highlight that performing a block of both planes provided successful results without increasing risks.67
Although there are studies evaluating differences between types of nerve blocks and SPB, these focus on using them as a preventive method.70,71 There was only one randomized clinical trial by Fuji et al comparing pain outcomes between SPB and pectoral nerve-2 (PEC-2) block.72 However, the authors included patients with chronic pain after mastectomy, without specifying if they had been diagnosed with PMPS.72 Therefore, it is unclear if the patients’ pain had neuropathic characteristics.72 In this study, 80 patients were divided into two groups, those receiving an SPB and those receiving a PEC-2 block.72 All patients received the same amount of ropivacaine and were followed for six months after surgery.72 The authors found the PEC-2 block to be more effective at reducing the rate of moderate to severe chronic pain at six months.72 The fact that the patients’ symptomatology is unclear, there is no control group, it is a single-center experience, and patients were limited to ASA physical status 1 or 2 highlights the need for further comparisons in patients with an established diagnosis of PMPS.72
Lastly, it is worth noting the retrospective analysis by Yang et al, in which the authors examined the pain outcomes after different types of blocks of 169 female patients with a mean age of 58 years and a diagnosis of PMPS.73 In 350 blocks, there were 13 different types, including combinations of them, of which the most common were the deep SPB, superficial SPB, and a combination of both.73 Blocks with less than 25 patients included the parasternal, PEC-1, PEC-2, a combination of PEC-1 and PEC-2, thoracic sympathetic, erector spinae, stellate ganglion, intercostobrachial, paravertebral, and thoracic intercostal nerve.73 The analyzed patients had a mean baseline pain score of 7 and a statistically significant decrease to 3.73 The mean pain relief duration was 45 days, and opioid medication was reduced by 11% from baseline.73 All patients received either 20 or 40 mg of triamcinolone, with those receiving the higher dose having a longer duration of pain relief and a lower pain intensity after treatment.73 Although the study did not provide a specific comparison between the different blocks, it corroborates the effectiveness of nerve blocks and shows that using a higher dose of steroids in addition to the local anesthetic provides improved results.73
Botulinum Toxin
Although the botulinum toxin’s mechanism of action for pain relief has not been elucidated, preclinical data suggest it affects pain modulators and neurotransmitters, peripherally and centrally, in addition to acetylcholine presynaptic vesicles.74–76 It has been previously tested in humans for treating chronic pain disorders with variable success.77 Rostami et al describe a case series of 12 patients with postsurgical and post-radiation pain after cancer, of which four patients presented with chronic pain after mastectomy.78 Out of these patients, two presented with severe pain of neuropathic characteristics, and therefore botulinum toxin injections were performed in a grid-like pattern.78 One of these patients had minimal improvement after 6 and 12 weeks, while the other presented complete pain remission.78 This information is currently inconclusive, and thus, large multi-center clinical trials are required to appropriately evaluate whether botulinum toxin is an appropriate management for the neuropathic symptoms of PMPS.
Future Directions
Current research on treating the neuropathic characteristics of pain in patients with PMPS is limited by a lack of standardized definitions, short-term evaluations, and overrepresentation of more severe cases. To improve the outcomes in future studies, researchers and the medical community must agree upon a standard definition of PMPS so that results can be comparable. Additionally, clinical studies should include patients with differing pain intensity levels to identify the best treatment option that relieves neuropathic pain. Finally, although treatment algorithms exist for neuropathic pain and several authors propose guidelines to treat PMPS, a treatment algorithm will be necessary for escalating pain management if initial pain is not adequately controlled.
Conclusion
Effective management of PMPS might require a comprehensive multimodal approach that considers the individual needs and preferences of the patient. Pharmacological interventions, such as those described in this review, have shown promising results. If pharmacological management is unsuccessful, procedural interventions may become necessary. Therefore, creating a comprehensive guideline to treat neuropathic pain specifically in patients with PMPS is becoming increasingly relevant, as appropriate pain management in breast cancer survivors who have undergone surgical management can substantially improve their quality of life.
Ethics Approval and Informed Consent
Since there was no human participation in this study, no ethics approval or informed consents were required.
Funding
This study was funded in part by the Center for Regenerative Medicine and the Clinical Practice Committee of Mayo Clinic Florida.
Disclosure
The authors report no conflicts of interest in this work.
References
1. Classification of chronic pain. Descriptions of chronic pain syndromes and definitions of pain terms. Prepared by the international association for the study of pain, subcommittee on taxonomy. Pain Suppl. 1986;3:S1–226.
2. Stubblefield MD, Custodio CM. Upper-extremity pain disorders in breast cancer. Arch Phys Med Rehabil. 2006;87(3):S96. doi:10.1016/j.apmr.2005.12.017
3. Waltho D, Rockwell G. Post-breast surgery pain syndrome: establishing a consensus for the definition of post-mastectomy pain syndrome to provide a standardized clinical and research approach - a review of the literature and discussion. Can J Surg. 2016;59(5):342–350. doi:10.1503/cjs.000716
4. Vecht CJ, Van de Brand HJ, Wajer OJM. Post-axillary dissection pain in breast cancer due to a lesion of the intercostobrachial nerve. Pain. 1989;38(2):171–176. doi:10.1016/0304-3959(89)90235-2
5. Caviggioli F, Maione L, Forcellini D, Klinger F, Klinger M. Autologous fat graft in postmastectomy pain syndrome. Plast Reconstr Surg. 2011;128(2):349–352. doi:10.1097/PRS.0b013e31821e70e7
6. Juhl AA, Karlsson P, Damsgaard TE. Fat grafting for alleviating persistent pain after breast cancer treatment: a randomized controlled trial. J Plast Reconstr Aesthet Surg. 2016;69(9):1192–1202. doi:10.1016/j.bjps.2016.07.003
7. Ilhan E, Chee E, Hush J, Moloney N. The prevalence of neuropathic pain is high after treatment for breast cancer: a systematic review. Pain. 2017;158(11):2082–2091. doi:10.1097/j.pain.0000000000001004
8. Cui L, Fan P, Qiu C, Hong Y. Single institution analysis of incidence and risk factors for post-mastectomy pain syndrome. Sci Rep. 2018;8(1):11494. doi:10.1038/s41598-018-29946-x
9. Alves Nogueira Fabro E, Bergmann A, Do Amaral ESB, et al. Post-mastectomy pain syndrome: incidence and risks. Breast. 2012;21(3):321–325. doi:10.1016/j.breast.2012.01.019
10. Wang L, Guyatt GH, Kennedy SA, et al. Predictors of persistent pain after breast cancer surgery: a systematic review and meta-analysis of observational studies. Cmaj. 2016;188(14):E352–e361. doi:10.1503/cmaj.151276
11. Miaskowski C, Cooper B, Paul SM, et al. Identification of patient subgroups and risk factors for persistent breast pain following breast cancer surgery. J Pain. 2012;13(12):1172–1187. doi:10.1016/j.jpain.2012.09.013
12. Gärtner R, Jensen MB, Nielsen J, Ewertz M, Kroman N, Kehlet H. Prevalence of and factors associated with persistent pain following breast cancer surgery. JAMA. 2009;302(18):1985–1992. doi:10.1001/jama.2009.1568
13. Berger JM, Longhitano Y, Zanza C, Sener SF. Factors affecting the incidence of chronic pain following breast cancer surgery: preoperative history, anesthetic management, and surgical technique. J Surg Oncol. 2020;122(7):1307–1314. doi:10.1002/jso.26176
14. Tait RC, Zoberi K, Ferguson M, et al. Persistent post-mastectomy pain: risk factors and current approaches to treatment. J Pain. 2018;19(12):1367–1383. doi:10.1016/j.jpain.2018.06.002
15. Moore RA, Derry S, Aldington D, Cole P, Wiffen PJ. Amitriptyline for neuropathic pain in adults. Cochrane Database Syst Rev. 2015;2015(7):Cd008242. doi:10.1002/14651858.CD008242.pub3
16. Eija K, Tiina T. Amitriptyline effectively relieves neuropathic pain following treatment of breast cancer. Pain. 1996;64(2):293–302. doi:10.1016/0304-3959(95)00138-7
17. Anderson IM, Ferrier IN, Baldwin RC, et al. Evidence-based guidelines for treating depressive disorders with antidepressants: a revision of the 2000 British association for psychopharmacology guidelines. J Psychopharmacol. 2008;22(4):343–396. doi:10.1177/0269881107088441
18. Tasmuth T, Härtel B, Kalso E. Venlafaxine in neuropathic pain following treatment of breast cancer. Eur J Pain. 2002;6(1):17–24. doi:10.1053/eujp.2001.0266
19. Li D, Lee JH, Choi CW, Kim J, Kim SK, Kim W. The analgesic effect of venlafaxine and its mechanism on oxaliplatin-induced neuropathic pain in mice. Int J Mol Sci. 2019;20:7.
20. Gallagher HC, Gallagher RM, Butler M, Buggy DJ, Henman MC. Venlafaxine for neuropathic pain in adults. Cochrane Database Syst Rev. 2015;2015(8):Cd011091. doi:10.1002/14651858.CD011091.pub2
21. Aiyer R, Barkin RL, Bhatia A. Treatment of neuropathic pain with venlafaxine: a systematic review. Pain Med. 2017;18(10):1999–2012. doi:10.1093/pm/pnw261
22. Taylor CP. Mechanisms of action of gabapentin. Rev Neurol. 1997;153:S39–45.
23. Rai AS, Khan JS, Dhaliwal J, et al. Preoperative pregabalin or gabapentin for acute and chronic postoperative pain among patients undergoing breast cancer surgery: a systematic review and meta-analysis of randomized controlled trials. J Plast Reconstr Aesthet Surg. 2017;70(10):1317–1328. doi:10.1016/j.bjps.2017.05.054
24. Hoseinzade H, Mahmoodpoor A, Agamohammadi D, Sanaie S. Comparing the effect of stellate ganglion block and gabapentin on the post mastectomy pain syndrome. Shiraz E Med J. 2008;9(2):88–96.
25. Patarica-Huber E, Boskov N, Pjevic M. Multimodal approach to therapy-related neuropathic pain in breast cancer. J buon. 2011;16(1):40–45.
26. Reyad RM, Omran AF, Abbas DN, et al. The possible preventive role of pregabalin in postmastectomy pain syndrome: a double-blinded randomized controlled trial. J Pain Symptom Manage. 2019;57(1):1–9. doi:10.1016/j.jpainsymman.2018.10.496
27. Kaur N, Kumar A, Saxena AK, Grover RK. Pregabalin in the treatment of postmastectomy chronic pain: results of an open label, single-arm clinical study. Breast J. 2019;25(3):465–468. doi:10.1111/tbj.13242
28. Lynch BA, Lambeng N, Nocka K, et al. The synaptic vesicle protein SV2A is the binding site for the antiepileptic drug levetiracetam. Proc Natl Acad Sci USA. 2004;101(26):9861–9866. doi:10.1073/pnas.0308208101
29. Vilholm OJ, Cold S, Rasmussen L, Sindrup SH. Effect of levetiracetam on the postmastectomy pain syndrome. Eur J Neurol. 2008;15(8):851–857. doi:10.1111/j.1468-1331.2008.02206.x
30. Sharma SK, Vij AS, Sharma M. Mechanisms and clinical uses of capsaicin. Eur J Pharmacol. 2013;720(1–3):55–62. doi:10.1016/j.ejphar.2013.10.053
31. Watson CP, Evans RJ, Watt VR. The post-mastectomy pain syndrome and the effect of topical capsaicin. Pain. 1989;38(2):177–186. doi:10.1016/0304-3959(89)90236-4
32. Watson PNC, Evans RJ. The postmastectomy pain syndrome and topical capsaicin: a randomized trial. Pain. 1992;51(3):375–379. doi:10.1016/0304-3959(92)90223-x
33. Dini D, Bertelli G, Gozza A, Forno GG. Treatment of the post-mastectomy pain syndrome with topical capsaicin. Pain. 1993;54(2):223–226. doi:10.1016/0304-3959(93)90213-9
34. Flöther L, Avila-Castillo D, Burgdorff AM, Benndorf R. Capsaicin in the treatment of refractory neuropathic pain after mastectomy surgery: a case report. Case Rep Oncol. 2020;13(2):997–1001. doi:10.1159/000508948
35. Dupoiron D, Jubier-Hamon S, Seegers V, et al. Peripheral neuropathic pain following breast cancer: effectiveness and tolerability of high-concentration capsaicin patch. J Pain Res. 2022;15:241–255. doi:10.2147/jpr.S341378
36. Knolle E, Zadrazil M, Kovacs GG, Medwed S, Scharbert G, Schemper M. Comparison of cooling and EMLA to reduce the burning pain during capsaicin 8% patch application: a randomized, double-blind, placebo-controlled study. Pain. 2013;154(12):2729–2736. doi:10.1016/j.pain.2013.08.001
37. Watson CP. Topical capsaicin as an adjuvant analgesic. J Pain Symptom Manage. 1994;9(7):425–433. doi:10.1016/0885-3924(94)90198-8
38. Derry S, Rice AS, Cole P, Tan T, Moore RA. Topical capsaicin (high concentration) for chronic neuropathic pain in adults. Cochrane Database Syst Rev. 2017;1(1):Cd007393. doi:10.1002/14651858.CD007393.pub4
39. Colloca L, Ludman T, Bouhassira D, et al. Neuropathic pain. Natu Rev Dis Prim. 2017;3(1):17002. doi:10.1038/nrdp.2017.2
40. Garzón-Rodríguez C, Casals Merchan M, Calsina-Berna A, López-Rómboli E, Porta-Sales J. Lidocaine 5 % patches as an effective short-term co-analgesic in cancer pain. Preliminary results. Support Care Cancer. 2013;21(11):3153–3158. doi:10.1007/s00520-013-1948-7
41. Maione L, Vinci V, Caviggioli F, et al. Autologous fat graft in postmastectomy pain syndrome following breast conservative surgery and radiotherapy. Aesthetic Plast Surg. 2014;38(3):528–532. doi:10.1007/s00266-014-0311-9
42. Caviggioli F, Maione L, Klinger F, Lisa A, Klinger M. Autologous fat grafting reduces pain in irradiated breast: a review of our experience. Stem Cells Int. 2016;2016:2527349. doi:10.1155/2016/2527349
43. Lisa AVE, Murolo M, Maione L, et al. Autologous fat grafting efficacy in treating PostMastectomy pain syndrome: a prospective multicenter trial of two Senonetwork Italia breast centers. Breast J. 2020;26(9):1652–1658. doi:10.1111/tbj.13923
44. Sollie M, Toyserkani NM, Bille C, Thomsen JB, Sørensen JA. Autologous fat grafting as treatment of postmastectomy pain syndrome: a randomized controlled trial. Plast Reconstr Surg. 2022;149(2):295–305. doi:10.1097/prs.0000000000008705
45. Minghao L. The process of autologous fat grafting in treating postmastectomy pain syndrome: what should we do? J Plast Reconstr Aesthet Surg. 2022;75(6):2001–2018. doi:10.1016/j.bjps.2022.02.075
46. Lisa A, Vinci V, Battistini A, Klinger F, Klinger M. Autologous fat grafting as treatment of postmastectomy pain syndrome: a randomized controlled trial. Plast Reconstr Surg. 2023;151(3):520e–521e. doi:10.1097/prs.0000000000009940
47. Sollie M, Toyserkani N, Bille C, Thomsen JB, Sørensen JA. Reply: autologous fat grafting as treatment of postmastectomy pain syndrome: a randomized controlled trial. Plast Reconstr Surg. 2023;151(3):521e–522e. doi:10.1097/prs.0000000000009941
48. Schnabel A, Reichl SU, Kranke P, Pogatzki-Zahn EM, Zahn PK. Efficacy and safety of paravertebral blocks in breast surgery: a meta-analysis of randomized controlled trials. Br J Anaesth. 2010;105(6):842–852. doi:10.1093/bja/aeq265
49. Miller RD, Johnston RR, Hosobuchi Y. Treatment of intercostal neuralgia with 10 per cent ammonium sulfate. J Thorac Cardiovasc Surg. 1975;69(3):476–478. doi:10.1016/S0022-5223(19)41574-2
50. Mehrotra M, Reddy V, Singh P. Neuroanatomy, stellate ganglion. StatPearls. Available from: https://www.ncbi.nlm.nih.gov/books/NBK539807/.
51. Piraccini E, Munakomi S, Chang K-V. Stellate ganglion blocks. StatPearls. Available from: https://www.ncbi.nlm.nih.gov/books/NBK507798/.
52. Nabil Abbas D, El Ghafar EM A, Ibrahim WA, Omran AF. Fluoroscopic stellate ganglion block for postmastectomy pain: a comparison of the classic anterior approach and the oblique approach. Clin J Pain. 2011;27(3):207–213. doi:10.1097/AJP.0b013e3181fb1ef1
53. Elramely MA, Abdelaal Ahmed Mahmoud MAA, Hamza MK, et al. Subfascial versus extrafascial ultrasound-guided stellate ganglion block in patients with post-mastectomy sympathetically mediated pain: a randomized clinical trial. Br J Pain. 2022;16(6):610–618. doi:10.1177/20494637221109681
54. Wray JK, Dixon B, Przkora R. Radiofrequency Ablation. StatPearls. Available from: https://www.ncbi.nlm.nih.gov/books/NBK482387/.
55. Hetta DF, Mohamed AA, Hetta HF, et al. Radiofrequency Thoracic sympathectomy for sympathetically maintained chronic post-mastectomy pain, a preliminary report: 6-month results. Pain Pract. 2021;21(1):54–63. doi:10.1111/papr.12933
56. Abbas DN, Reyad RM. Thermal versus super voltage pulsed radiofrequency of stellate ganglion in post-mastectomy neuropathic pain syndrome: a prospective randomized trial. Pain Physician. 2018;21(4):351–362. doi:10.36076/ppj.2018.4.351
57. Broyles JM, Tuffaha SH, Williams EH, Glickman L, George TA, Lee Dellon A. Pain after breast surgery: etiology, diagnosis, and definitive management. Microsurgery. 2016;36(7):535–538. doi:10.1002/micr.30055
58. Wong L. Intercostal neuromas: a treatable cause of postoperative breast surgery pain. Ann Plast Surg. 2001;46(5):481–484. doi:10.1097/00000637-200105000-00004
59. Salemis NS. Traumatic neuroma as a rare cause of intractable neuropathic breast pain following cancer surgery: management and review of the literature. Intractable Rare Dis Res. 2018;7(3):185–190. doi:10.5582/irdr.2018.01041
60. Dorsi MJ, Lenz FA. Neurosurgical approached to the treatment of pain. In: Wall & Melzack’s Textbook of Pain. Elsevier; 2013:563–569.
61. Ducic I, Larson EE. Outcomes of surgical treatment for chronic postoperative breast and abdominal pain attributed to the intercostal nerve. J Am Coll Surg. 2006;203(3):304–310. doi:10.1016/j.jamcollsurg.2006.05.018
62. Williams EH, Williams CG, Rosson GD, Heitmiller RF, Dellon AL. Neurectomy for treatment of intercostal neuralgia. Ann Thorac Surg. 2008;85(5):1766–1770. doi:10.1016/j.athoracsur.2007.11.058
63. Hart SE, Agarwal S, Hamill JB, Brown DL. Effective treatment of chronic mastectomy pain with intercostal sensory neurectomy. Plast Reconstr Surg. 2022;149(5):876e–880e. doi:10.1097/prs.0000000000008975
64. Kim JS, Spiess AM. Surgical treatment of intercostal brachial nerve pain after mastectomy and axillary dissection. Plast Reconstr Surg Glob Open. 2021;9(11):e3935. doi:10.1097/gox.0000000000003935
65. Blanco R, Parras T, McDonnell JG, Prats-Galino A. Serratus plane block: a novel ultrasound-guided thoracic wall nerve block. Anaesthesia. 2013;68(11):1107–1113. doi:10.1111/anae.12344
66. Zocca JA, Chen GH, Puttanniah VG, Hung JC, Gulati A. Ultrasound-guided serratus plane block for treatment of postmastectomy pain syndromes in breast cancer patients: a case series. Pain Pract. 2017;17(1):141–146. doi:10.1111/papr.12482
67. Maranto CJ, Strickland NR, Goree JH. Combined superficial and deep serratus plane block with bupivacaine, dexamethasone, and clonidine in the treatment of a patient with postmastectomy pain syndrome: a case report. A a Pract. 2018;11(9):236–237. doi:10.1213/xaa.0000000000000792
68. Liu Q, Khanna A, Stubblefield MD, Yue GH, Allexandre D. Ultrasound-guided superficial serratus plane block for persistent post-mastectomy pain: four case reports. Support Care Cancer. 2022;30(3):2787–2792. doi:10.1007/s00520-021-06696-7
69. Piracha MM, Thorp SL, Puttanniah V, Gulati A. “A Tale of two planes”: deep versus superficial serratus plane block for postmastectomy pain syndrome. Reg Anesth Pain Med. 2017;42(2):259–262. doi:10.1097/aap.0000000000000555
70. Arora S, Ovung R, Bharti N, Yaddanapudi S, Singh G. Efficacy of serratus anterior plane block versus thoracic paravertebral block for postoperative analgesia after breast cancer surgery - a randomized trial. Braz J Anesthesiol. 2022;72(5):587–592. doi:10.1016/j.bjane.2021.09.017
71. Yesiltas S, Türköz A, Çalım M, et al. Comparison of serratus plane block alone and in combination with pectoral type 1 block for breast cancer surgery: a randomized controlled study. Hippokratia. 2021;25(1):8–14.
72. Fujii T, Shibata Y, Akane A, et al. A randomised controlled trial of pectoral nerve-2 (PECS 2) block vs. serratus plane block for chronic pain after mastectomy. Anaesthesia. 2019;74(12):1558–1562. doi:10.1111/anae.14856
73. Yang A, Nadav D, Legler A, et al. An interventional pain algorithm for the treatment of postmastectomy pain syndrome: a single-center retrospective review. Pain Med. 2021;22(3):677–686. doi:10.1093/pm/pnaa343
74. Welch MJ, Purkiss JR, Foster KA. Sensitivity of embryonic rat dorsal root ganglia neurons to Clostridium botulinum neurotoxins. Toxicon. 2000;38(2):245–258. doi:10.1016/s0041-0101(99)00153-1
75. Meng J, Ovsepian SV, Wang J, et al. Activation of TRPV1 mediates calcitonin gene-related peptide release, which excites trigeminal sensory neurons and is attenuated by a retargeted botulinum toxin with anti-nociceptive potential. J Neurosci. 2009;29(15):4981–4992. doi:10.1523/jneurosci.5490-08.2009
76. Shin MC, Wakita M, Xie DJ, et al. Inhibition of membrane Na+ channels by A type botulinum toxin at femtomolar concentrations in central and peripheral neurons. J Pharmacol Sci. 2012;118(1):33–42. doi:10.1254/jphs.11060fp
77. Taylor SS, Noor N, Urits I, et al. Complex regional pain syndrome: a comprehensive review. Pain Ther. 2021;10(2):875–892. doi:10.1007/s40122-021-00279-4
78. Rostami R, Mittal SO, Radmand R, Jabbari B. Incobotulinum toxin-a improves post-surgical and post-radiation pain in cancer patients. Toxins. 2016;8(1):22. doi:10.3390/toxins8010022
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
