Back to Journals » Journal of Asthma and Allergy » Volume 17
A Retrospective Claims Database Study to Clarify Treatment Reality of Asthma Patients Before and After Referral to a Specialist
Authors Hozawa S, Ono K, Makita N, Uchimura H, Arita Y, Hirai T, Tashiro N
Received 30 August 2023
Accepted for publication 21 December 2023
Published 18 January 2024 Volume 2024:17 Pages 9—19
DOI https://doi.org/10.2147/JAA.S437944
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Luis Garcia-Marcos
Soichiro Hozawa,1 Keita Ono,2 Naoyuki Makita,3 Hitomi Uchimura,3 Yoshifumi Arita,3 Takehiro Hirai,2 Naoki Tashiro3
1Hiroshima Allergy and Respiratory Clinic, Hiroshima, Japan; 2AstraZeneca K.K., Tokyo, Japan; 3AstraZeneca K.K., Osaka, Japan
Correspondence: Soichiro Hozawa, Hiroshima Allergy and Respiratory Clinic, 6F, 1-9-28 Hikari-machi, Higashi-ku, Hiroshima, 732-0052, Japan, Tel +81-82-568-1167, Fax +81-82-568-1239, Email [email protected]
Purpose: Japanese guidelines recommend that patients with uncontrolled asthma be referred by non-specialists to specialists (allergists and/or pulmonologists). This study investigated the reality of clinical practice in asthma patients referred to specialists in Japan.
Patients and Methods: This was a retrospective, observational cohort study of asthma patients in a health insurance claim database (Cross Fact) referred from facilities with non-specialists to those with specialists from January 2016 to December 2018. The referred asthma patients were defined as patients with ≥ 4 inhaled corticosteroid (ICS)-containing prescriptions during a 1-year baseline period, with an asthma diagnosis, and who had visited a facility with specialists. Asthma exacerbation, maintenance treatment, laboratory tests, and medical procedures before and after referral were analyzed.
Results: Data for 2135 patients were extracted, of which 420 with referral codes were analyzed. The proportion of patients with asthma exacerbations was 50.2% (95% confidence interval [CI]: 45.4– 55.1%) before referral and 37.4% (95% CI: 32.7– 42.2%) after, a significant decrease (P< 0.001; McNemar test). The proportions of patients prescribed ICS alone, long-acting beta-agonists (LABA), and ICS/LABA were lower after referral than before, but the proportions of patients prescribed long-acting muscarinic antagonists (LAMA), ICS/LABA/LAMA, and biologics increased after referral. More asthma-related laboratory tests were performed after referral, and spirometry incidence increased from 16.4% before referral to 51.4% after referral.
Conclusion: This study shows a decrease in asthma exacerbations, change in asthma treatments, and increase in laboratory tests after referral to a specialist, suggesting that referrals to specialists lead to better management of asthma.
Keywords: asthma, database, referral, specialist, symptom exacerbation
Introduction
Asthma is a chronic heterogeneous disease that affects the airways.1 Patients with asthma have a history of respiratory symptoms that vary over time, including wheezing, shortness of breath, coughing, and chest tightness, along with variable limitations in expiratory airflow.1 Worldwide, 0.9–29% of the population suffer from asthma at some point in their lives.2 In Japan, asthma symptoms are recognized as a highly prevalent health problem affecting 9–10% of the adult population.3
Asthma treatment aims to control the symptoms and reduce the risk of exacerbations, asthma-related mortality, persistent airflow limitations, and treatment side-effects.1 Various treatments, including inhaled corticosteroid (ICS) monotherapy or ICS/long-acting beta-agonists (LABA) combinations, are available and known to reduce the frequency of asthma exacerbations; however, they may not fully prevent them.4 Patients with asthma exacerbations have an increased risk of future exacerbations, which may contribute to worsening respiratory function and increasing medical expenditure.5–7 Therefore, patients with uncontrolled asthma need better management to prevent asthma exacerbations, which may include referral to specialists.
International guidelines suggest that referrals to specialists may be appropriate in cases of difficult to confirm diagnosis, suspected occupational asthma, difficult to control, frequent exacerbations, asthma-related death risk, treatment side-effects, sub-types of asthma, complications or for various other reasons in children aged 6–11 years.1
To prevent asthma exacerbations and provide better asthma management in Japan, local treatment guidelines for physicians have also been developed. The Japanese Guidelines for Adult Asthma 2021 recommend referral to a specialist, such as an allergist and/or pulmonologist, if step-up treatment fails to improve asthma control.8 The Practical Guidelines for Asthma Management 2022 suggest referral to a specialist if: a) asthma is difficult to diagnose because of non-response to initial asthma treatment; b) there is poor asthma control despite treatment for severe asthma during the long-term management of asthma; or c) repeated exacerbations or severe acute exacerbations are occurring.9 Specialists commonly evaluate asthma control status, asthma treatment adherence, inhalation technique, comorbidities, and asthma phenotype/endotype in referred asthma patients and provide appropriate maintenance treatment as recommended in treatment guidelines.8,9
In the United States and Israel, studies found that referrals to specialists reduced asthma exacerbations and the use of systemic steroids.10,11 However, it is difficult to extrapolate overseas results directly to the clinical setting in Japan, particularly as there are differences in the medical and insurance systems between Japan and other countries.12 While there are clear recommendations for which groups of patients should be referred to specialists, there is still little evidence of the results of referral in the general asthma population. Thus, the reality of clinical practice in asthma patients referred to specialists in Japan has not been well elucidated.
This study aimed to clarify the reality of asthma exacerbations, asthma treatment, and the asthma-related laboratory tests of asthma patients who were referred by a physician or self-referred to a facility with specialists in Japan. These results may confirm the significant benefits of being referred or self-referred for asthma management in patients with uncontrolled or inadequately controlled asthma.
Materials and Methods
Study Design
This study was a retrospective, observational cohort study using a health insurance claim database (Cross Fact; Intage Real World Inc., Japan) of asthma patients referred from non-specialists to specialists. Cross Fact is an administrative database comprising medical and pharmacy claims data for salaried workers and their family members. This database included around 7 million or more insured persons as of December 2019. In this database, a unique identifier is assigned to each individual; thus, individuals can be followed up even if they transfer to another institution. The health insurance claim database used data from employees’ national health insurance, and covers all institutions including diagnosis procedure combination (DPC) hospitals, which is the claims-based payment system used by numerous large acute care hospitals in Japan. DPC is a comprehensive daily payment system based on the diagnosis group classification for acute hospitalization.
The dataset was completely anonymized and contained patient demographic information, inpatient and outpatient medical and pharmacy claims data, with clinical diagnoses coded under the International Classification of Diseases, 10th revision (ICD-10) classification, drug prescriptions information coded according to the Anatomical Therapeutic Chemical (ATC) classification, as well as healthcare procedures. In addition, the facility with which the respiratory specialist and/or allergist was associated was recorded by the database vendor, with confirmation of the anonymity of individuals, using information from the website of the Japanese Society of Allergology and the Japanese Respiratory Society, with permission.13,14
The study protocol and its amendment were approved by the NPO-MINS Institutional Review Board (Approval No. 220217 in July 2022). This observational study was performed in accordance with ethical principles consistent with the Ethical Guidelines for Biomedical Research Involving Human Subjects, the Declaration of Helsinki, and the Japanese Act on the Protection of Personal Information. Informed consent was waived because the data were anonymized.
Patients
Data from January 1, 2015, to December 31, 2019, were analyzed. The index date was defined as the first visit date at a facility with a specialist. Adult asthma patients with visits to a facility with specialists were included if they met all of the inclusion criteria and did not meet any of the exclusion criteria (Figure 1). Inclusion criteria were: 1) asthma patients aged ≥17 years at the index date; 2) patients that could be followed up for 1 year (365 days) before and after the index date; 3) patients with ≥4 records of ICS-containing prescriptions ATC code: R03D1, R03F1) with an asthma diagnosis from a facility without specialists during the baseline period; and 4) patients with a visit to a facility with specialists. Patients were excluded if they had been diagnosed with autoimmune disease, multiple sclerosis, or nephrotic syndrome (see Supplementary Table 1).
 |
Figure 1 Study design. Abbreviations: ATC, Anatomical Therapeutic Chemical; ICD-10, International Classification of Diseases, 10th revision; ICS, inhaled corticosteroid. |
Among those asthma patients with a visit to a facility with specialists, physician-referred asthma patients were defined as those with a referral code (180016110). For each patient, asthma diagnosis and referral were confirmed based on ICD-10 codes (J45 and J46) and the referral code.
We also recorded the rate of reverse-referred patients in all groups, defined as patients referred from a facility with specialists to a former facility with non-specialists.
Definitions of Asthma Exacerbation-Related Events
The primary objective was to investigate the proportions of asthma patients with asthma exacerbations before and after referral in the physician-referred population (Figure 2). The secondary objectives were to investigate the number of asthma exacerbations, the proportions of patients taking asthma-related treatments by treatment type, and the proportions of patients with related laboratory tests or medical procedures before and after referral.
 |
Figure 2 Analysis populations. Abbreviations: ICD-10, International Classification of Diseases, 10th revision; ICS, inhaled corticosteroid. |
Patients were considered to have asthma exacerbation if they met at least one of the following criteria: 1) having experienced asthma-related hospitalization, defined as any hospitalization with asthma as the main disease; 2) having received injectable steroids, defined as a record of an injectable steroid prescription with coexistence of an asthma diagnosis; and/or 3) having received an oral corticosteroid (OCS) burst, defined as a record of an OCS prescription with a dose of ≥20 mg/day or a record of an OCS prescription with a dose increase of ≥10 mg/day compared with the previous OCS prescription, with coexistence of an asthma diagnosis.
Patient Demographics and Clinical Variables
The demographic characteristics recorded included age, sex, comorbidities (Quan–Charlson comorbidity index score, respiratory infection, allergic rhinitis, gastroesophageal reflux disease [GERD], chronic obstructive pulmonary disease [COPD], diabetes mellitus, chronic paranasal sinusitis, atopic dermatitis, osteoporosis, sleep apnea, pneumonia, psychiatric disorder, and cardiovascular disease), facility for asthma treatment (with or without specialist), asthma-related prescriptions (short-acting beta-agonists [SABA], ICS alone, LABA, long-acting muscarinic antagonists [LAMA], ICS/LABA, ICS/LABA/LAMA, OCS, LT receptor antagonist [LTRA], theophylline, and biologics), and asthma-related laboratory tests and medical procedures (spirometry, eosinophil count, total immunoglobulin E [IgE], radioallergosorbent test [RAST], fractional exhaled nitric oxide [FeNO], and C-reactive protein [CRP]). High, middle, and low doses of any ICS were defined as ≥1600, 800–<1600, and <800 µg per day budesonide equivalent dosage, respectively, in accordance with both global and Japanese guidelines.1,8
Statistical Analysis
The patient demographics and characteristics are summarized descriptively. For categorical variables, the number and the proportion of patients were calculated. For quantitative variables, the number of patients, mean, and standard deviation (SD) were calculated.
Patients who met all of the inclusion criteria and did not meet the exclusion criteria were defined as the full analysis population (FAP) (Figure 2). The physician-referred population consisted of asthma patients in the FAP with a referral code within 1 month before the index date. Patients in the physician-referred frequent exacerbators population were defined as those with referral codes and ≥2 asthma exacerbations, while patients in the FAP who presented independently to specialists (ie, with no referral code) were defined as the self-referred population.
The proportions of patients with asthma exacerbations, laboratory tests, and medical procedures before and after referral were tested by McNemar’s method. For each component of asthma exacerbation, proportions of asthma patients before and after referral were calculated along with 95% confidence intervals (CIs). The number of asthma exacerbations before referral was compared with that after referral using the Wilcoxon signed-rank test. The statistical tests were exploratory and, therefore, were not adjusted for multiplicity. Statistical significance was assessed by two-sided α=0.05 type I error. All analyses were conducted in SAS Viya version 3.5 (SAS Institute Inc., Cary, North Carolina).
Results
Cohorts and Patient Characteristics
Approximately 1.7 million asthma patients were included in the database between 2015 and 2019 (Figure 2). The FAP included 2135 asthma patients, of whom 420 were physician-referred to specialists and 1715 were self-referred. A total of 148 patients in the physician-referred population had ≥2 asthma exacerbations (physician-referred frequent exacerbators).
In the physician-referred population, 226 patients (53.8%) were female and the mean (SD) age was 47.8 (12.4) years (Table 1). The mean (SD) Quan–Charlson comorbidity index score was 3.0 (2.3). The common comorbidities (≥10% in prevalence) were allergic rhinitis (79.3%), respiratory infection (60.7%), pneumonia (46.9%), GERD (35.2%), diabetes mellitus (34.1%), COPD (30.7%), chronic paranasal sinusitis (29.8%), cardiovascular disease (23.8%), psychiatric disorder (20.5%), and sleep apnea (20.2%). Patient characteristics of the FAP and subpopulations are shown in Supplementary Table 2.
 |
Table 1 Patient Demographics and Characteristics of the Physician-Referred Population |
Asthma Exacerbations Before and After Referral
In the physician-referred population, significantly fewer patients had asthma exacerbations in the outcome period (37.4% [95% CI: 32.7–42.2%] than in the baseline period (50.2% [95% CI: 45.4–55.1%]; P<0.001; McNemar test) (Figure 3).
In the physician-referred population, there was a numerical decrease from before to after referral to specialists in the proportion of patients with asthma-related hospitalization (8.3% [95% CI: 5.9–11.4%] vs 6.7% [95% CI: 4.5–9.5%]; P=0.354) and receiving OCS bursts (25.0% [95% CI: 20.9–29.4%] vs 21.4% [95% CI: 17.6–25.7%]; P=0.158); however, this difference was only significant for those receiving injectable steroids (35.2% [95% CI: 30.7–40.0%] vs 26.7% [95% CI: 22.5–31.2%]; P=0.002; McNemar test) (Figure 3).
The respective proportions of patients with 0, 1, 2, 3, or ≥4 asthma exacerbations were 49.8%, 26.7%, 9.5%, 4.5%, and 9.5% in the baseline period, and 62.6%, 17.4%, 7.1%, 3.8%, and 9.1% in the outcome period in the physician-referred population (Supplementary Table 3). This represented a significant decrease in the number of exacerbations between the two periods (P=0.012; Wilcoxon signed-rank test).
Asthma-Related Treatment, Laboratory Tests, and Medical Procedures Before and After Referral
In the physician-referred population, significantly fewer patients were prescribed ICS alone (baseline period vs outcome period: 21.0% vs 14.5%), LABA (19.3% vs 9.8%), ICS/LABA (92.9% vs 82.4%), LTRA (75.2% vs 65.5%), or theophylline (42.1% vs 26.0%; all P<0.001; McNemar test) in the outcome period (Table 2) compared with the baseline period. Conversely, significantly more patients were prescribed LAMA (9.5% vs 14.1%; P=0.004), ICS/LABA/LAMA (0.0% vs 1.2%; P=0.025), and biologics (0.7% vs 2.1%; P=0.014; McNemar test) in the outcome period compared with the baseline period. In the physician-referred population, prescription of any ICS (high dose 56.7% vs 42.9%, middle dose 28.8% vs 23.3%, low dose 11.3% vs 19.3%) was not significantly changed in the outcome period (Table 2) compared with the baseline period. However, patients with no ICS prescription comprised 11.3% of the population in the outcome period.
 |
Table 2 Prescription of Asthma Treatment Before/After Referral in Asthma Patients Referred from Non-Specialist to Specialist in the Physician-Referred Population |
SABA (46.7% vs 31.4%) and OCS (43.3% vs 32.6%) were prescribed to fewer physician-referred patients in the outcome period compared with the baseline period (all P<0.001; McNemar test) (Table 2). The proportion of patients receiving maintenance OCS was 1.2% in the baseline period and 2.4% in the outcome period in the physician-referred population (P=0.025; McNemar test) (Table 2). The increase in the proportion of patients receiving maintenance OCS was not consistent with the decrease in the proportion of patients with exacerbations. Furthermore, the proportion of patients receiving a biologic was extraordinarily low in the baseline period.
The proportions of patients (baseline period vs outcome period) receiving laboratory tests and medical procedures were as follows: spirometry, 16.4% vs 51.4%; eosinophil count, 40.5% vs 60.7%; total IgE, 16.0% vs 43.1%; RAST, 13.8% vs 31.2%; FeNO, 10.0% vs 38.6%; and CRP, 48.1% vs 74.3% (Table 3). These were all significantly higher in the outcome period than in the baseline period (all P<0.001; McNemar test).
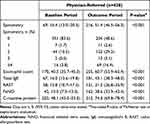 |
Table 3 Presence of Laboratory Tests and Medical Procedures Before/After Referral in Asthma Patients Referred from Non-Specialist to Specialist in the Physician-Referred Population |
Asthma Exacerbations
In the physician-referred frequent exacerbators population, the proportion of patients with asthma exacerbations was 100% in the baseline period and 59.5% in the outcome period (Supplementary Table 4). In this group, the occurrence of hospitalization, receiving injectable steroids, and receiving an OCS burst were numerically low after referral to a specialist, and the relative difference (baseline period vs outcome period) was greater than that in the physician-referred population.
In the patient population who self-referred, the proportion of patients with asthma exacerbations was 41.3% in the baseline period and 30.4% in the outcome period (Supplementary Table 5). The proportions of patients with asthma-related hospitalization, receiving injectable steroids, and receiving OCS bursts were lower in the outcome period.
In all subpopulations, the proportions of patients with laboratory tests were higher in the outcome period and the treatment drugs were changed similarly (Supplementary Tables 6–9).
Reverse Referral
The proportions of reverse-referred patients were 62.9% in the physician-referred population, 55.4% in physician-referred frequent exacerbators, and 39.5% in self-referred patients (Supplementary Table 10). In the physician-referred population, there were more reverse referrals from DPC system hospitals15 than non-DPC hospitals (67.2% vs 47.9%) and from hospitals with ≥20 beds than those with <20 beds (67.3% vs 35.2%).
Discussion
To the best of our knowledge, this is the first study to clarify asthma exacerbations, asthma-related treatment, and laboratory tests before and after specialist referral in Japan. In the physician-referred population, the proportion of patients with asthma exacerbation was significantly lower after referral to a specialist (37.4%) than before (50.2%). Referral to specialists led to improvements in asthma exacerbation-related outcomes in this study. Moreover, a change of asthma-related treatment and greater execution of asthma-related laboratory tests were observed after referral. These findings may indicate the benefit of referring Japanese asthma patients to specialists.
Overall, the sex and age distribution of patients in this study were generally consistent with previous reports.16,17 However, the distribution of comorbidities of the referred patients in this study was higher than in those previous reports.16,17 It is possible that these patients were referred not only for managing asthma but also for managing complications. The proportion of asthma exacerbations (composite) was significantly decreased (P<0.001) after referral. Similarly, real-world studies in the United States10 and Israel11 also showed that the proportion of patients with asthma exacerbations decreased after referral to specialists. In each component of asthma exacerbation, injectable steroid use was significantly decreased in this study (P=0.002). The administration of OCS burst and frequency of asthma-related hospitalization decreased numerically but not significantly (P=0.158 and P=0.354, respectively) in this study. It may be surmised that an OCS burst may be associated with decreased asthma-related hospitalization.
In addition to the proportions of patients with asthma exacerbations, the proportions of patients stratified by the number of asthma exacerbations (composite; 0, 1, 2, 3, or ≥4) also were significantly different after referral (P=0.012). Consistent results were shown in this study population for a decrease in the proportion of patients experiencing asthma exacerbations and the number of asthma exacerbations after referral. The number of asthma exacerbations decreased significantly after referral to a specialist; in particular, the proportion of patients with 1 asthma exacerbation decreased numerically. However, the proportion of patients with ≥4 asthma exacerbations was similar before and after referral, suggesting that some patients could not decrease their exacerbations even after being referred to a specialist. This may be because the asthma was difficult to control during the 1-year outcome period after referral because of the severity, the characteristics of the patient, treatment adherence, or complications.
In the physician-referred frequent exacerbators population, the proportion of asthma exacerbations decreased from 100% to 59.5% after referral. This was consistent with the overall physician-referred population, and the extent of the asthma exacerbation decrease was more prominent.
The asthma-related medications used changed after referral to a specialist. Prescriptions for ICS alone, LABA, ICS/LABA, LTRA, and theophylline decreased, but prescriptions for medications often used in severe cases, including LAMA and biologics, increased. To improve treatment outcomes, specialists could take a “treatable traits” approach, wherein they focus on treatment adherence management, inhalation technique confirmation, treatment monitoring with asthma-related tests evaluating airflow limitation and type 2 inflammation, and management of comorbidities.8,9 This approach might lead to more appropriate drug selection and dosage. Specialists might cut back on some excessive treatments and add other treatments, including LAMA and biologics, for patients with more severe asthma. The proportions of patients with prescriptions for OCS and SABA for exacerbations also decreased after referral in this study, similar to a previous study.10 In clinical practice, referral to a specialist might result in a decrease in asthma attacks requiring OCS and SABA.
The proportions of patients receiving some laboratory assessments were significantly higher in the outcome period than in the baseline period. Spirometry, eosinophil count, and FeNO are important details for the management of asthma.1,8,9 Spirometry is an objective index for examining the degree of airflow limitation and is useful for monitoring asthma.17,18 Blood eosinophil and FeNO are important biomarkers for type 2 inflammation in asthma.19–22 Assessing and monitoring the treatable traits of airflow limitation and type 2 inflammation reduce exacerbation risk and improve asthma control.23 This assessment and monitoring could contribute to treatment adherence management, inhalation technique improvement, management of comorbidities, and improvement of outcomes. Nonetheless, laboratory tests were only conducted for 40–60% of referred patients. This may be attributable to the pre-referral test results being used as a reference. More asthma-related laboratory tests were performed after referral to a specialist compared with before referral, and these test results were checked to implement appropriate asthma management and asthma treatment necessary for severe asthma patients.
The proportions of reverse-referred patients were higher in DPC hospitals than in non-DPC hospitals and in facilities with ≥20 beds than facilities with <20 beds. In DPC hospitals and larger hospitals, reverse referral is generally recommended, which may be the reason more patients had reverse referrals.24 The advantage of referral to a specialist is that the patient is more likely to be reverse-referred, which may lead to optimization of medical resources in asthma treatment.24 These results suggest the importance of hospital collaboration through referrals.
The proportion of reverse-referred patients was higher in the overall physician-referred population than in the physician-referred frequent exacerbators population (Supplementary Table 10). It may be that the proportion of reverse referral in physician-referred frequent exacerbators was less than in the overall physician-referred population because the physician-referred frequent exacerbators population comprised less well-controlled asthma patients who might need continuous specialist care. In self-referred patients, the rate of reverse referral was lower than in the other groups. In these patients, visiting a facility with a specialist after attending a facility without a specialist was based on patient decision. The specialists may have difficulty reverse-referring a self-referred patient to a former facility with non-specialists with patients who are not adequately treated. To increase the rate of reverse referral, non-specialists should consider referring patients to a specialist via a referral letter.
This study had some limitations. First, there were no patient-reported or medical record data. Thus, the actual symptoms and asthma control status may have been inaccurate. Second, the majority of patients included in this claims database were working-age individuals, and elderly patients may be under-represented. Therefore, our results cannot be applied to the elderly population. Third, there was a gap between the period when specialists were flagged, and the period used for analysis. Fourth, the reason for referral might not have necessarily been asthma. In this study, to increase the accuracy for referral by asthma, referred patients were defined as those with a visit to a facility with a specialist and with an asthma diagnosis.
Conclusion
This is the first study in Japan to clarify asthma exacerbation, asthma-related treatments, and laboratory tests before and after physician- or self-referral to a specialist. Our findings showed a decrease in asthma exacerbations, change in asthma treatments, and increases in laboratory tests following referral or self-referral to a specialist, suggesting that both physician-referral and self-referral to a specialist lead to better management of asthma.
Abbreviations
ATC, Anatomical Therapeutic Chemical; COPD, chronic obstructive pulmonary disease; CRP, C-reactive protein; DPC, diagnosis procedure combination; FAP, full analysis population; FeNO, fractional exhaled nitric oxide; GERD, gastroesophageal reflux disease; ICD-10, International Classification of Diseases, 10th revision; ICS, inhaled corticosteroid; IgE, immunoglobulin E; LABA, long-acting beta-agonist; LAMA, long-acting muscarinic antagonist; LTRA, LT receptor antagonist; OCS, oral corticosteroid; RAST, radioallergosorbent test; SABA, short-acting beta-agonist; SD, standard deviation.
Data Sharing Statement
Data underlying the findings described in this manuscript may be obtained in accordance with AstraZeneca’s data sharing policy described at https://astrazenecagrouptrials.pharmacm.com/ST/Submission/Disclosure.
Acknowledgments
This work was supported by AstraZeneca K.K., Osaka, Japan. The study sponsor was involved in designing the study, analyzing and interpreting the data, and writing the report. The authors would like to thank EP Corporation for data analyses, EMC K.K. for medical writing services, and Edanz, Japan, for providing editorial support, all of which were funded by AstraZeneca K.K. The authors would also like to thank Kaori Oneda for their contribution in conducting the study.
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Funding
This research was funded by AstraZeneca K.K., Osaka, Japan.
Disclosure
SH has received honoraria from AstraZeneca, GlaxoSmithKline, Novartis Pharma, and Kyorin Pharmaceutical. KO, NM, HU, and YA are employees of AstraZeneca K.K. TH and NT are employees of and hold stock in AstraZeneca K.K. TH reports gain on sale of stocks (Daiichi Sankyo), outside the submitted work. The authors report no other conflicts of interest in this work.
References
1. Global Initiative for Asthma. Global strategy for asthma management and prevention; 2023. Available from: https://ginasthma.org/.
2. Mortimer K, Lesosky M, García-Marcos L, et al; Global Asthma Network Phase I Study Group. The burden of asthma, hay fever and eczema in adults in 17 countries: GAN Phase I study. Eur Respir J. 2022;60(3):2102865. doi:10.1183/13993003.02865-2021
3. Fukutomi Y, Nakamura H, Kobayashi F, et al. Nationwide cross-sectional population-based study on the prevalences of asthma and asthma symptoms among Japanese adults. Int Arch Allergy Immunol. 2010;153(3):280–287. doi:10.1159/000314369
4. Chung KF, Wenzel SE, Brozek JL, et al. International ERS/ATS guidelines on definition, evaluation and treatment of severe asthma. Eur Respir J. 2014;43(2):343–373. doi:10.1183/09031936.00202013
5. Zeiger RS, Schatz M, Li Q, Chen W, Khatry DB, Tran TN. Burden of chronic oral corticosteroid use by adults with persistent asthma. J Allergy Clin Immunol Pract. 2017;5(4):1050–1060.e9. doi:10.1016/j.jaip.2016.12.023
6. Matsunaga K, Hirano T, Oka A, et al. Progression of irreversible airflow limitation in asthma: correlation with severe exacerbations. J Allergy Clin Immunol Pract. 2015;3(5):759–764.e1. doi:10.1016/j.jaip.2015.05.005
7. Suruki RY, Daugherty JB, Boudiaf N, Albers FC. The frequency of asthma exacerbations and healthcare utilization in patients with asthma from the UK and USA. BMC Pulm Med. 2017;17(1):74. doi:10.1186/s12890-017-0409-3
8. Niimi A, Fukunaga K, Taniguchi M, et al. Executive summary: Japanese guidelines for adult asthma (JGL) 2021. Allergol Int. 2023;72(2):207–226. doi:10.1016/j.alit.2023.02.006
9. Japan Asthma Society. Practical Guidelines for Asthma Management 2022. Tokyo: Kyowa Kikaku; 2022. Japanese.
10. Most JF, Ambrose CS, Chung Y, et al. Real-world assessment of asthma specialist visits among U.S. patients with severe asthma. J Allergy Clin Immunol Pract. 2021;9(10):3662–3671.e1. doi:10.1016/j.jaip.2021.05.003
11. Rosman Y, Hornik-Lurie T, Meir-Shafrir K, Lachover-Roth I, Cohen-Engler A, Confino-Cohen R. The effect of asthma specialist intervention on asthma control among adults. World Allergy Organ J. 2022;15(11):100712. doi:10.1016/j.waojou.2022.100712
12. Toyabe S, Kouhei A. Referral from secondary care and to aftercare in a tertiary care university hospital in Japan. BMC Health Serv Res. 2006;6(1):11. doi:10.1186/1472-6963-6-11
13. Japanese Society of Allergology. List of specialists and instructors, Japanese Society of Allergology (for general use). Available from: https://www.jsaweb.jp/modules/ninteilist_general/.
14. Japanese Respiratory Society. Specialist search. Available from: https://www.jrs.or.jp/search/specialist/index.php.
15. Wang K, Li P, Chen L, Kato K, Kobayashi M, Yamauchi K. Impact of the Japanese diagnosis procedure combination-based payment system in Japan. J Med Syst. 2010;34(1):95–100. doi:10.1007/s10916-008-9220-2
16. Nagase H, Adachi M, Matsunaga K, et al. Prevalence, disease burden, and treatment reality of patients with severe, uncontrolled asthma in Japan. Allergol Int. 2020;69(1):53–60. doi:10.1016/j.alit.2019.06.003
17. Inoue H, Kozawa M, Milligan KL, Funakubo M, Igarashi A, Loefroth E. A retrospective cohort study evaluating healthcare resource utilization in patients with asthma in Japan. NPJ Prim Care Respir Med. 2019;29(1):13. doi:10.1038/s41533-019-0128-8
18. Matsunaga K, Hamada K, Oishi K, Yano M, Yamaji Y, Hirano T. Factors associated with physician-patient discordance in the perception of asthma control. J Allergy Clin Immunol Pract. 2019;7(8):2634–2641. doi:10.1016/j.jaip.2019.04.046
19. Price DB, Rigazio A, Campbell JD, et al. Blood eosinophil count and prospective annual asthma disease burden: a UK cohort study. Lancet Respir Med. 2015;3(11):849–858. doi:10.1016/S2213-2600(15)00367-7
20. Belda J, Parameswaran K, Lemière C, Kamada D, O’Byrne PM, Hargreave FE. Predictors of loss of asthma control induced by corticosteroid withdrawal. Can Respir J. 2006;13(3):129–133. doi:10.1155/2006/189127
21. Dweik RA, Boggs PB, Erzurum SC, et al. An official ATS clinical practice guideline: interpretation of exhaled nitric oxide levels (FENO) for clinical applications. Am J Respir Crit Care Med. 2011;184(5):602–615. doi:10.1164/rccm.9120-11ST
22. Saito J, Gibeon D, Macedo P, Menzies-Gow A, Bhavsar PK, Chung KF. Domiciliary diurnal variation of exhaled nitric oxide fraction for asthma control. Eur Respir J. 2014;43(2):474–484. doi:10.1183/09031936.00048513
23. Pavord ID, Barnes PJ, Lemière C, Gibson PG. Diagnosis and assessment of the asthmas. J Allergy Clin Immunol Pract. 2023;11(1):1–8. doi:10.1016/j.jaip.2022.09.034
24. Health Insurance Bureau Medical Division, Ministry of Health, Labour and Welfare. Overview of FY2022 medical fee revision outpatient I. Available from: https://www.mhlw.go.jp/content/12400000/000920428.pdf.
 © 2024 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2024 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.

