Back to Journals » Journal of Asthma and Allergy » Volume 17
A Longitudinal Study of a Selected Pediatric Asthmatic Population with Normal and Abnormal Spirometry at Baseline: An Emphasis on Treatment Outcomes
Authors Yimlamai S, Ruangnapa K , Anuntaseree W, Saelim K, Prasertsan P, Sirianansopa K
Received 9 October 2023
Accepted for publication 15 January 2024
Published 20 January 2024 Volume 2024:17 Pages 61—68
DOI https://doi.org/10.2147/JAA.S432648
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Dr Luis Garcia-Marcos
Sornsiri Yimlamai, Kanokpan Ruangnapa, Wanaporn Anuntaseree, Kantara Saelim, Pharsai Prasertsan, Kantisa Sirianansopa
Department of Pediatrics, Faculty of Medicine, Prince of Songkla University, Hat Yai, Songkhla, 90110, Thailand
Correspondence: Kanokpan Ruangnapa, Department of Pediatrics, Faculty of Medicine, Prince of Songkla University, Hat-Yai, Songkhla, 90110, Thailand, Tel +66-74-451250-1, Fax +66-74-451250-3, Email [email protected]
Purpose: It is still unclear whether considering abnormal spirometry as a marker for disease control can help physicians adjust asthma controllers in children because of the scarcity of pediatric studies. We aimed to investigate the prevalence of abnormal spirometry in a selected pediatric asthmatic population and its effect on longitudinal outcomes.
Patients and Methods: This retrospective cohort study was conducted at the Songklanagarind Hospital, Thailand. Children with asthma aged < 18 years were recruited for review if they attended the clinic and underwent acceptable spirometry with bronchodilator responsiveness (BDR) tests after receiving asthma treatment for at least 3 months between January 2011 and June 2022. Differences in baseline characteristics, atopic factors, asthma treatment, and outcomes were analyzed between the normal and abnormal spirometry groups over a 12-month post-spirometry period.
Results: The mean age of the 203 enrolled patients was 10.9 ± 2.6 years. Abnormal spirometry, defined as airflow limitation or the presence of BDR, was observed in 58.1% of patients. No significant differences were observed in baseline characteristics, atopic factors, asthma treatment, or outcomes between the normal and abnormal spirometry groups. Further analysis of 107 patients with abnormal spirometry with symptom control revealed that physicians adjusted the asthma controller based on spirometry and symptoms in 84 and 23 patients, respectively. There was no significant difference in the loss of disease control over the 12-month post-spirometry period between the two groups.
Conclusion: Abnormal spirometry was found in 58.1% of treated school-aged patients with asthma. Abnormal spirometry results were not associated with poor asthma outcomes during the 12-month follow-up. Both symptom-based and spirometry-based adjustments of asthma controllers resulted in comparable symptom control over a 12-month follow-up period in the selected population.
Keywords: pulmonary function test, lung function test, childhood asthma, bronchodilator responsiveness
Introduction
Asthma is the most prevalent non-communicable respiratory disease in childhood, affecting 11–13% of children worldwide.1 Besides symptom control and minimizing the future risk of exacerbations, preserving normal lung function is an important goal of long-term pediatric asthma care.2 Impaired lung function in children with asthma is associated with an increased risk of chronic airflow obstruction and chronic obstructive pulmonary disease development in early adulthood.2–4 Therefore, regular assessment of lung function is encouraged in monitoring children with asthma.2,5
Spirometry is currently the standard tool for assessing lung function in children with asthma. Abnormal spirometry parameters (such as low forced expiratory volume in 1 s [FEV1], low ratio of FEV1 to forced vital capacity [FEV1/FVC], or low forced expiratory flow between 25% and 75% of vital capacity [FEF25–75%], which represents airway dysfunction), are considered predictors of disease severity and long-term prognosis of respiratory health.3,4 Children with asthma with a lower FEV1 percentage are more likely to have more severe disease and are at a higher risk of exacerbation.6,7 However, a significant portion of symptom-controlled patients with asthma still have abnormal lung function.8–11
Airway reversibility is another characteristic feature of asthma that can be assessed via bronchodilator responsiveness (BDR) testing in children with asthma.2,5 Besides its diagnostic purpose, the persistence of BDR is a marker of poor asthma control and predictive of a good response to inhaled corticosteroids (ICS).12,13 Previous studies have reported evidence of airway reversibility in children with asthma with good asthma control or normal lung function.14,15 These controversial findings affect the role of spirometry and BDR testing in asthma management. However, because of the scarcity of pediatric studies, it is still unclear whether, besides symptom assessment, considering abnormal lung function or the presence of BDR as another marker for disease control can help physicians adjust asthma controllers in children.
Hence, we aimed to investigate the prevalence of abnormal spirometry results in school-aged children with asthma by exploring the longitudinal correlation between asthma control and spirometry results and its effect on asthma controller adjustment.
Materials and Methods
Study Design
This retrospective study was conducted at the Pediatric Pulmonology and Allergy Clinic of the Songklanagarind Hospital, Prince of Songkla University, Southern Thailand. Ethics committee approval from the Faculty of Medicine, Prince of Songkla University (REC-65-261-1-1, approved on August 15, 2022) was obtained prior to study initiation. The study was performed in accordance with the Declaration of Helsinki, and informed consent was obtained from the parent or legal guardian of all study participants (which aged <18 years) prior to study commencement. Children with asthma aged <18 years who attended the clinic and underwent spirometry testing between January 2011 and June 2022 were recruited for the initial review. Based on the initial review, children who met the following criteria were enrolled as study participants: 1) received asthma treatment for at least 3 months before spirometry 2) had acceptable spirometry and 3) underwent BDR testing. Children were excluded from the study if they met the following criteria: 1) any underlying diseases, congenital heart, chronic lung, neuromuscular diseases, or immunodeficiency disorders and 2) incomplete follow-up data after spirometry.
Data Collection
Patient information was collected from medical records, including demographic data, atopic history, allergen sensitization, asthma comorbidities, current asthma controller used, symptom control status, and healthcare utilization because of acute asthma (systemic steroid use, emergency visits, and hospital and intensive care admission) prior to and at 3, 6, and 12 months post spirometry. Spirometry parameters were also collected from electronic records.
Definition and Measurement Methods
Asthma Characteristics
Atopic history and asthma comorbidities, including food allergy, atopic dermatitis, allergic rhinitis, gastroesophageal reflux, and obstructive sleep apnea, were defined based on physician diagnostic records. Allergen sensitization was defined as having any record of a positive skin prick test result (wheal size ≥ 3 mm) or specific serum immunoglobulin E for aeroallergens greater than the cutoff of 0.35 kUA/L.
Treatment adherence was classified as “good” for never or hardly missed prescribed drug usage or “poor” for frequently or always missed prescribed drug usage. The adjustments of asthma controllers were defined as “step up”, “maintain”, or “step-down” treatment, according to the stepwise management of Global Initiative for Asthma (GINA) 2022.2
Disease control was evaluated via 3-month periodic visits using simple screening tools.2 The patient was considered to have “symptom control” when none of the following four criteria were present within the previous 4 weeks: 1) day-time asthma symptoms more than twice a week, 2) night-time asthma symptoms more than once a week; 3) symptom disturbances of normal activity more than once a week, and 4) use of a rescuer more than twice a week.
Spirometry
Spirometry was performed by a registered nurse using a computer-assisted spirometer (KoKoVR Spirometer; nSpire Health, CO, USA) according to international guidelines applied for quality control.16 The measurements were performed with patients in a standard position, without the use of nose clips. Three values were obtained, and the highest FEV1 and FVC values were used. The FEV1/FVC ratio, FEF25–75%, and peak expiratory flow rate (PEFR) were recorded. Standard BDR tests were performed according to standard protocols, and the best post-bronchodilator FEV1 and PEFR values were recorded.
Abnormal spirometry was defined as either documented expiratory airflow limitation (FEV1< 80% predicted and an FEV1/FVC ratio < 0.9) or documented BDR demonstrated by an increase in FEV1 > 12% or PEFR > 12% of baseline after salbutamol administration.2
Statistical Analysis
Data were analyzed using the R software (version 4.0.4; R Foundation for Statistical Computing, Vienna, Austria). Descriptive data were presented as percentages, means (standard deviation; SD), and medians (interquartile range; IQR). Participant characteristics were compared across spirometry groups (normal and abnormal) using the chi-squared or Fisher’s exact test for a proportion of each categorical variable (sex, obesity, controller used, atopic status, and asthma control status at 3-, 6-, and 12-month follow-up). Continuous data (age at spirometry and age at first wheezing) were compared based on the distribution of data using the mean (Student’s t-test) and median (Mann–Whitney U-test). Children with symptom control and abnormal spirometry were further analyzed to determine the pattern of asthma controller adjustments (stepping down or not stepping down) and treatment outcomes in the two groups. The significance level for all tests was set at p < 0.05.
Results
A total of 402 medical records of eligible patients with asthma were reviewed. Among them, 203 patients with acceptable spirometry and complete BDR results were analyzed (Figure 1). Sixty-five percent of patients were male, with a mean age of 10.9 ± 2.6 years during spirometry testing. Most patients (83.3%) already used asthma controllers, and 47.3% were receiving a treatment level higher than GINA treatment step 2.
 |
Figure 1 Study design and flow diagram. |
According to the predefined criteria in the study, the overall prevalence of abnormal spirometry results was 58.1%. Focusing on the evidence of airflow limitation, 37.4% of treated patients with asthma showed evidence of airflow limitation (Table 1); in contrast, BDR was present in 36.0% of the patients.
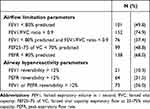 |
Table 1 Spirometry Results of the Study Population (N = 203) |
Table 2 shows the comparison of patient characteristics according to spirometry results. The percentage of current controller use was not significantly different between the two groups (81.4% vs 85.9%, p = 0.51). Although a higher proportion of patients were receiving asthma treatment GINA steps 1–2 in the abnormal spirometry group than those in the normal group, this difference was not statistically significant (57.6% vs 45.8%, p = 0.13). Furthermore, there were no significant differences in the prevalence of obesity, allergic diseases, or allergen sensitization between the two groups.
 |
Table 2 Patient Characteristics According to Spirometry Results (N = 203) |
Of the participants, 90.6% were classified as having symptom control during spirometry testing. There was no significant difference in symptom control and healthcare utilization percentage because of acute asthma (emergency visit, hospitalization, and intensive care unit [ICU] admission) between the abnormal and normal spirometry results in the year before spirometry testing (Table 3). According to the outcomes over 12 months following spirometry, in each 3-month interval post spirometry, there were no significant differences in the rate of symptom control, emergency visits, and systemic steroid use between the two groups. Furthermore, no patients in either group required hospitalization or ICU admission because of acute asthma in the following 12 months post-spirometry.
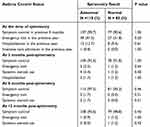 |
Table 3 Asthma Control Status and Spirometry Results (N = 203) |
There were 107 patients with asthma that had abnormal spirometry despite clinically defined “symptom control” with spirometry testing. Two different asthma controller adjustment patterns were detected simultaneously. Twenty-three (21.5%) out of 107 patients received stepping-down treatment, defined as “symptom-based adjustment”; in contrast, 84 (78.5%) out of 107 patients received non-stepping-down treatment, defined as “spirometry-based adjustment”. The asthma outcomes over 12 months for both treatment algorithms are shown in Figure 2. There was no statistically significant difference in the loss of disease control between the spirometry-based and symptom-based adjustment groups at 12 months after spirometry (4/84 [4.8%] vs 1/23 [4.4%]; p = 1.00).
 |
Figure 2 Physician decision on treatment according to spirometry results and outcomes. |
Discussion
This study explored lung function abnormalities in the selected population: school-aged patients with asthma receiving treatment. Abnormal spirometry was found in 58.1% of treated school-aged patients with asthma. Our study used a broader definition of abnormal spirometry, including airflow limitation and albuterol bronchial responsiveness. Both features are characteristic of asthma and represent airway dysfunction.5
The strength of this study lies in the informative use of the dataset. Data in this study were obtained from structured medical records to ensure the accuracy and completeness of various asthma outcomes, such as symptom control, healthcare utilization for acute asthma, controller use, and medication compliance. All asthma outcomes were assessed by nurses or physicians during each visit through direct interviews. The protocolized schedule of our visiting institutes facilitated repeated analyses at 3, 6, and 12 months post-spirometry to assess long-term asthma outcomes. However, this study had some limitations that must be addressed. The single spirometry results for each individual may not demonstrate the association with symptom control for a year.
Previous studies have reported differences in the prevalence of abnormal lung function because of variances in definitions and different populations studied. The reported prevalence, based on airflow obstruction, ranges from 23.5% to 60% in pediatric asthma.6,10,11,15 Lo et al10 studied 575 children with asthma treated in the United Kingdom and found that 23.5% had airflow obstruction. Another recent prospective study15 reported that 27.5% of Thai children with well-controlled asthma still had airflow obstruction. In this study, the prevalence of abnormal spirometry regarding airflow obstruction (37.4%) was higher than that in other studies. The persistence of airflow obstruction after asthma treatment in patients with asthma might be affected by various patient and environmental factors beyond appropriate asthma treatment. Kwong et al17 reported unchanged lung function in inner-city children with asthma despite appropriate asthma treatment over 3–5 years, which showed that treatment or level of asthma control did not change lung function.
Atopy and being overweight are significant factors affecting lung function in children with asthma.4,18 Ciprandi et al19 showed a relationship between BMI and low FEV1; patients who were overweight had double the risk, and patients with obesity had triple the risk of having pathological FEV1. Contrarily, we found no significant differences in the percentage of obesity and atopic risk between the abnormal and normal spirometry groups. We did not explore several other clinical factors that might affect persistently impaired lung function from early childhood, such as pre-natal/perinatal lung insults,18 severe early-life respiratory tract infections,20 maternal smoking, and environmental tobacco smoke.18,21
More than 90% of the patients in this study maintained symptom control throughout the follow-up period, and abnormal spirometry was not associated with poor asthma outcomes during periodic evaluation over the 12-month post-spirometry period. A weak correlation between symptom control and lung function has been reported in many studies.9,10 However, many controversial issues remain regarding the use of lung function to classify asthma severity or predict future asthma outcomes in pediatric asthma studies. Data from 416 children in a controlled clinical trial6 showed a significant association between pre-bronchodilator FEV1 and asthma outcomes. The lower the FEV1 percentage, the higher the risk of asthma exacerbation in the following 4 months. Additionally, FEV1 reversibility has been identified as the strongest factor for predicting the need for a higher dose of asthma medications in the year following spirometry assessment.13 However, some pediatric asthma studies have failed to demonstrate a good correlation between spirometry and asthma severity classified by symptom frequency or medication use.8,11 Although airway obstruction in patients with asthma is an important feature of severe diseases or airway remodeling despite receiving treatment, some patients can improve over time by adherence to medication. It has been accepted that airway structure changes can occur even in asymptomatic asthma.2,5 Hence, spirometry, which detects airway dysfunction, might not simultaneously change with the patient’s symptoms.
The observational data in this study explored one of the problematic situations in asthma medication adjustment, wherein abnormal spirometry was present in definite symptom control accompanied by good medication adherence. This study found that both symptom- and spirometry-based approaches for treatment adjustment resulted in a comparable rate of uncontrolled disease. However, these findings should be interpreted with caution because of the study’s retrospective nature, which might have led to several biases. This study excluded patients with incomplete follow-up data; therefore, regularly visiting patients tended to demonstrate good adherence. This was supported by a high disease control rate (up to 95% in both groups). In addition, this study’s overall rate of good adherence to medication was quite high (81.8%). However, this finding highlights physicians’ difficulty in utilizing spirometry or other objective tests in asthma management.
However, our study has some limitations. Spirometry assessments in this study were performed at different time points during the disease course, depending on clinical decisions with no standard protocols. Some were used as objective markers of disease control before discontinuing asthma control; in contrast, others were evaluated for baseline lung function after the initiation of asthma treatment. Further longitudinal or prospective studies using interval spirometry assessments should be conducted to address the clinical question of optimizing the use of spirometry tests in real-world pediatric practice.
Conclusion
Abnormal spirometry results were observed in more than half of the treated school-aged patients with asthma. Abnormal spirometry results were not associated with poor asthma outcomes during the 12-month follow-up period in this selected population. Both symptom-based and spirometry-based adjustments of asthma controllers resulted in comparable symptom control over a 12-month follow-up period.
Abbreviations
BDR, bronchodilator responsiveness; FEV1, forced expiratory volume in 1 second; FEV1/FVC, ratio of FEV1 to forced vital capacity; FEF25–75%, forced expiratory flow between 25% and 75% of vital capacity; FeNO, fractional exhaled nitric oxide; GINA, Global Initiative for Asthma; ICS, inhaled corticosteroids; IQR, interquartile range; SD, standard deviation; PEFR, peak expiratory flow rate.
Data Sharing Statement
The data that support the findings of this study are available from the corresponding author upon reasonable request.
Ethics Approval and Informed Consent
Ethics committee approval from the Faculty of Medicine, Prince of Songkla University (REC-65-261-1-1, approved on August 15, 2022) was obtained prior to study initiation. The study was performed in accordance with the Declaration of Helsinki and informed consent was obtained from the parents or legal guardians of all study participants prior to study commencement.
Acknowledgments
We would like to thank all the respiratory nurses of the Pediatric Pulmonology and Allergy Clinic at Songklanagarind Hospital, who performed standard spirometry for all patients with asthma throughout the study period, as well as detailed interviews for asthma symptom control assessment of all patient visits.
Author Contributions
All authors made a significant contribution to the work reported, whether that was in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Funding
This work was supported by the Faculty of Medicine, Prince of Songkla University (grant number REC 65-261-1-1). The sponsor had no involvement in the study design, analysis and interpretation of data, or in the decision to submit the article for publication.
Disclosure
The authors report no conflicts of interest related to this work.
References
1. Asher MI, García-Marcos L, Pearce NE, Strachan DP. Trends in worldwide asthma prevalence. Eur Respir J. 2020;56(6):2002094. doi:10.1183/13993003.02094-2020
2. Global initiative for asthma. Pocket guide for asthma management and prevention. Available from: https://ginasthma.org/pocket-guide-for-asthma-management-and-prevention/.
3. Bui DS, Walters HE, Burgess JA, et al. Childhood respiratory risk factor profiles and middle-age lung function: a prospective cohort study from the first to sixth decade. Ann Am Thorac Soc. 2018;15(9):1057–1066. doi:10.1513/AnnalsATS.201806-374OC
4. Dharmage SC, Bui DS, Walters EH, et al. Lifetime spirometry patterns of obstruction and restriction, and their risk factors and outcomes: a prospective cohort study. Lancet Respir Med. 2023;11(3):273–282. doi:10.1016/S2213-2600(22)00364-2
5. Moeller A, Carlsen KH, Sly PD, et al. Monitoring asthma in childhood: lung function, bronchial responsiveness and inflammation. Eur Respir Rev. 2015;24(136):204–215. doi:10.1183/16000617.00003914
6. Salviano LDDS, Taglia-Ferre KD, Lisboa S, Costa ACCD, Campos HDS, March MFP. Association between fraction of exhaled nitric oxide and spirometry data and clinical control of asthma in children and adolescents. Rev Paul Pediatr. 2018;36(1):8. doi:10.1590/1984-0462/;2018;36;1;00015
7. Simon MR, Chinchilli VM, Phillips BR, et al.; Childhood Asthma Research and Education Network of the National Heart, Lung, and Blood Institute. Forced expiratory flow between 25% and 75% of vital capacity and FEV1/forced vital capacity ratio in relation to clinical and physiological parameters in asthmatic children with normal FEV1 values. J Allergy Clin Immunol. 2010;126(3):527–34.e348. doi:10.1016/j.jaci.2010.05.016
8. Schifano ED, Hollenbach JP, Cloutier MM. Mismatch between asthma symptoms and spirometry: implications for managing asthma in children. J Pediatr. 2014;165(5):997–1002. doi:10.1016/j.jpeds.2014.07.026
9. Lee MS, Kao JK, Lee CH, et al. Correlations between pulmonary function and childhood asthma control test results in 5–11-year-old children with asthma. Pediatr Neonatol. 2014;55(3):218–224. doi:10.1016/j.pedneo.2013.10.003
10. Lo DK, Beardsmore CS, Roland D, et al. Lung function and asthma control in school-age children managed in UK primary care: a cohort study. Thorax. 2020;75(2):101–107. doi:10.1136/thoraxjnl-2019-213068
11. Lazova S, Priftis S, Petrova G, Naseva E, Velikova T. MMEF25–75 may predict significant BDR and future risk of exacerbations in asthmatic children with normal baseline FEV1. Int J Physiol Pathophysiol Pharmacol. 2022;14(1):33–47.
12. Heffler E, Crimi C, Campisi R, et al. Bronchodilator response as a marker of poor asthma control. Respir Med. 2016;112:45–50. doi:10.1016/j.rmed.2016.01.012
13. Pongracic JA, Krouse RZ, Babineau DC, et al. Distinguishing characteristics of difficult-to-control asthma in inner-city children and adolescents. J Allergy Clin Immunol. 2016;138(4):1030–1041. doi:10.1016/j.jaci.2016.06.059
14. Huang J, Zhang M, Zhang X, Wang L. Airway hyper-responsiveness and small airway function in children with well-controlled asthma. Pediatr Res. 2015;77(6):819–822. doi:10.1038/pr.2015.42
15. Uppala R, Kaenpugdee P, Srisutthikamol S, Teeratakulpisarn J. Assessment of small airway function and reversibility in symptom-controlled asthma in pediatric patients. Asian Pac J Allergy Immunol. 2019;37(1):25–29. doi:10.12932/AP-170817-0138
16. Graham BL, Steenbruggen I, Miller MR, et al. Standardization of spirometry 2019 update. An official American Thoracic Society and European Respiratory Society technical statement. Am J Respir Crit Care Med. 2019;200(8):e70–e88. doi:10.1164/rccm.201908-1590ST
17. Kwong KY, Lu YZ, Jauregui E, Scott L. Persistent airflow obstruction in inner-city children with asthma. Allergy Asthma Proc. 2021;42(4):310–316. doi:10.2500/aap.2021.42.210043
18. Bui DS, Lodge CJ, Burgess JA, et al. Childhood predictors of lung function trajectories and future COPD risk: a prospective cohort study from the first to the sixth decade of life. Lancet Respir Med. 2018;6(7):535–544. doi:10.1016/S2213-2600(18)30100-0
19. Ciprandi G, Schiavetti I, Bellezza fontana R, Sorbello V, Ricciardolo FL. Overweight and obesity as risk factors for impaired lung function in patients with asthma: a real-life experience. Allergy Asthma Proc. 2014;35(4):e62–e71. doi:10.2500/aap.2014.35.3773
20. van Meel ER, Mensink-Bout SM, den Dekker HT, et al. Early-life respiratory tract infections and the risk of school-age lower lung function and asthma: a meta-analysis of 150 000 European children. Eur Respir J. 2022;60(4):2102395. doi:10.1183/13993003.02395-2021
21. Savran O, Ulrik CS. Early life insults as determinants of chronic obstructive pulmonary disease in adult life. Int J Chron Obstruct Pulmon Dis. 2018;13:683–693. doi:10.2147/COPD.S153555
 © 2024 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2024 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
