Back to Journals » Clinical Ophthalmology » Volume 15
Visual Outcome and Treatment Frequency of Anti-VEGF Therapy Using the Treat-and-Extend and Treatment Cessation Regimen for Exudative Age-Related Macular Degeneration and Pachychoroid Neovasculopathy
Authors Kinoshita T , Mori J, Hatanaka A, Shimizu M , Imaizumi H
Received 18 August 2021
Accepted for publication 27 September 2021
Published 9 November 2021 Volume 2021:15 Pages 4405—4418
DOI https://doi.org/10.2147/OPTH.S334641
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Scott Fraser
Takamasa Kinoshita, Junya Mori, Akira Hatanaka, Miho Shimizu, Hiroko Imaizumi
Department of Ophthalmology, Sapporo City General Hospital, Sapporo, Japan
Correspondence: Takamasa Kinoshita
Department of Ophthalmology, Sapporo City General Hospital, 1-1, N-11, W-13, Chuoku, Sapporo, 060-8604, Japan
Tel +81 11 726 2211
Fax +81 11 726 9541
Email [email protected]
Purpose: To report the results of anti-vascular endothelial growth factor (VEGF) therapy using treat-and-extend (TAE) and treatment cessation regimens for exudative age-related macular degeneration (AMD) and pachychoroid neovasculopathy (PN).
Methods: We retrospectively studied 101 treatment-naïve eyes of 101 patients with exudative AMD and PN that underwent anti-VEGF therapy using TAE and treatment cessation regimen with a follow-up period of ≥ 12 months. Best-corrected visual acuity (BCVA), treatment frequency, and number of eyes with successful treatment cessation were measured. Successful treatment cessation was defined as dry macula retention without treatment for > 16 weeks after the last injections. Factors related to the successful treatment cessation were evaluated.
Results: BCVA was maintained at the last visit with a mean follow-up period of 49.9 ± 26.9 months. The injection number decreased from 6.8 ± 2.31 at the first year to 3.7 ± 3.64 at the fifth year. At the last visit, 48 (47.5%) eyes were being treated at an interval of ≥ 12 weeks or were under treatment cessation. Successful treatment cessation during the follow-up period and at the last visit were achieved in 56 (55.4%) and 27 (26.7%) eyes, with a median treatment-free period of 66 and 126 weeks, respectively. Good early treatment response and a small recurrence number were associated with successful treatment cessation at the last visit.
Conclusion: Patients with good early response to treatment and fewer recurrences may achieve treatment cessation. This information could help physicians predict the achievement of treatment cessation for a considerable period.
Keywords: age-related macular degeneration, pachychoroid neovasculopathy, anti-vascular endothelial growth factor, treat-and-extend regimen, treatment cessation
Plain Language Summary
Anti-vascular endothelial growth factor therapy for exudative age-related macular degeneration using treat-and-extend (TAE) regimen are popular in common clinical practice. But the results of TAE with treatment cessation regimen have been scarcely reported. We showed that more than a quarter of the eyes were under successful treatment cessation for more than 2 years. Eyes with good early treatment response and a small recurrence number are more likely to achieve successful treatment cessation. This information could help physicians predict the achievement of treatment cessation for a considerable period.
Introduction
Currently, anti-vascular endothelial growth factor (anti-VEGF) therapy is the mainstream management regimen for exudative age-related macular degeneration (AMD), which is among the major causes of severe visual impairment in elderly patients worldwide.1–3 Although there have been encouraging functional and anatomical results regarding the fixed regimen of anti-VEGF injections, patients, clinicians, and health insurance providers have a large treatment burden that is unsustainable in common clinical settings.4–6 Consequently, anti-VEGF therapy, with pro re nata (PRN) or treat-and-extend (TAE) regimens, was introduced.7–9 TAE regimens, with/without modifications, have become increasingly popular in common clinical practice.10
There have been numerous reports regarding anti-VEGF therapy for exudative AMD using TAE regimens.9,11–25 These previous studies reported outcomes as changes in best-corrected visual acuity (BCVA), central retinal thickness (CRT), and injection/visit frequency. Currently, few studies have introduced the TAE protocol with treatment cessation.18,22 Arendt et al reported that patients who achieved treatment cessation using the TAE regimen with a minimum injection number (ie, patients with good early treatment response without subsequent recurrence) did not show post-cessation recurrence.22 However, the detailed relationship of early treatment responses or recurrence frequency with successful treatment cessation remains unclear.
Exudative AMD is usually classified into three subtypes; typical neovascular AMD (tnAMD), polypoidal choroidal vasculopathy (PCV), and retinal angiomatous proliferation (RAP). Previous pivotal studies evaluated the efficacy and safety of anti-VEGF therapy for exudative AMD including all subtypes of exudative AMD.4,6,7,11,13–15,17,19,24–27 Pachychoroid spectrum diseases, which are recently proposed clinical entities, are prevalent in Asian populations.28–30 Previously, pachychoroid neovasculopathy (PN), which involves choroidal neovascularization (CNV), was often diagnosed as AMD, especially in Asian populations.30 Based on the differences in clinical characteristics and genetic background between PN and drusen-driven AMD, they have been recently clearly differentiated.21,30–32
This study aimed to report the visual outcomes and treatment frequency of anti-VEGF therapy for exudative AMD and PN using the TAE and treatment cessation regimen in an Asian clinic. Moreover, we aimed to determine the association of early treatment response and recurrence frequency with treatment cessation under stable conditions.
Materials and Methods
This study adhered to the tenets of the Declaration of Helsinki. This study was approved by the Institutional Review Board of Sapporo City General Hospital before participant recruitment (R02-059-730). The requirement for written informed consent was waived by the ethics committee given the retrospective nature of the study. Instead, the patients were allowed “opt-out” consent.
Inclusion and Exclusion Criteria
This retrospective study consecutively included treatment-naïve eyes of patients aged ≥50 years with exudative AMD and PN involving the fovea. The eyes were diagnosed by a single physician (TK) and treated with ranibizumab (0.5mg, Lucentis; Novartis Pharma AG, Basel, Switzerland) or aflibercept (2mg, Eylea: Bayer AG, Leverkusen, Germany) using TAE regimen between January 2013 and December 2019 with a follow-up period of ≥12 months. During the early and late study periods, ranibizumab and aflibercept were administered, respectively. In the cases with persistent CNV activity, switching of anti-VEGF drugs or concomitant photodynamic therapy (PDT) using verteporfin (6 mg/m2) with anti-VEGF therapy was performed. The final data set was collected before December 25, 2020. For patients with bilateral exudative AMD or PN, we included eyes with the more recently initiated treatments.
The exclusion criteria were as follows: eyes with vitreoretinal diseases other than AMD and PN; glaucoma; high myopia; BCVA worse than 20/1000; significant cataract recommended for surgical interventions at the first anti-VEGF injection; chorioretinal scarring or atrophy involving the fovea; previous treatment using intravitreal injections of anti-VEGF agents or macular laser treatment, including PDT; having undergone intraocular surgeries other than non-complicated cataract surgeries; comorbid systemic diseases, including uncontrolled hypertension and renal failure; and patients who were not diagnosed and treated by a single physician (TK). Moreover, we excluded patients who had not undergone three initial monthly injections or follow-up for ≥12 months after the initial injection.
Ophthalmic Examinations
At baseline, all patients underwent ophthalmic examinations including BCVA and intraocular pressure measurements, slit-lamp biomicroscopy, color fundus photography, fluorescein and indocyanine angiography (F-10; Nidek Co., Ltd, Gamagori, Japan), and spectral-domain optical coherence tomography (SD-OCT, Spectralis OCT instrument, Heidelberg Engineering GmbH, Heidelberg, Germany). Moreover, fundus autofluorescence and optical coherence tomography angiography were performed at the physician’s discretion.
Disease Classification
The diseases were classified as follows: tnAMD, PCV without pachychoroid characteristics, RAP, and PN with/without polypoidal lesions. Before PN introduction, numerous eyes with PN, with and without polypoidal lesions, had been diagnosed with PCV and tnAMD (occult CNV), respectively; however, they were amended before study onset depending on the presence of pachychoroid characteristics. The presence of a pachychoroid was characterized as follows: obscured large choroidal vessels on color fundus photographs, thick choroid and dilated large choroidal vessels (pachyvessels) with an accompanying thin choriocapillaris layer just above the pachyvessels on SD-OCT, and choroidal vascular hyperpermeability on indocyanine angiography.
SD-OCT Examination
To obtain SD-OCT images, we performed horizontal and vertical cross-sectional scans at 30° passing through the fovea, as well as macular volume scans covering an area of 30° × 25° centered on the fovea. Moreover, we obtained cross-sectional enhanced depth imaging OCT images to examine the choroidal structures. The CRT was determined using the Early Treatment of Diabetic Retinopathy Study (ETDRS) center thickness map of 1 mm diameter.
Treatment Design
Prompt TAE
Anti-VEGF therapy involved two TAE regimens; namely, prompt TAE and deferred TAE, which depended on the disease type and lesion size. The prompt TAE regimen was applied for eyes that did not meet the criteria for the deferred TAE. It involved ≥3 monthly injections of anti-VEGF agents until dry macula was achieved with subsequent treatment interval adjustment based on the disease activity. Dry macula is indicative of inactivated CNV lesions without retinal/subretinal hemorrhages and intraretinal/subretinal fluid (SRF), which were confirmed through biomicroscopy and SD-OCT. When confirming the dry macula, retinal pigment epithelial detachment (PED) was not considered.
Deferred TAE
The deferred TAE regimen was applied to patients with tnAMD and PN without polypoidal lesions, which both involved lesions smaller than 1 disc area approximately. Further, this regimen was applied to patients with a history of Antiplatelet Trialists’ Collaboration Events.33 Regarding the deferred TAE regimen, ≥3 anti-VEGF injections were administered until dry macula with subsequent observation without treatment until fluid/hemorrhage recurrence was observed on SD-OCT or biomicroscopically. In case of recurrence, the TAE regimen was restarted with a 4-week injection interval.
Adjustment of Treatment Intervals and Treatment Cessation
For both regimens, the patients were asked to make visits on the day of injections, and at one week after each injection for assessment of the BCVA, SD-OCT, and adverse events. After the loading phase, in case dry macula was observed on the injection day, the treatment interval was extended by 2 weeks. Moreover, if fluid was observed on the injection day with subsequent disappearance at one post-injection week, the treatment interval was maintained. However, if they persisted at one post-injection week, the treatment interval was shortened by two weeks. In case of intraretinal or subretinal hemorrhages, treatments were administered monthly until dry macula restoration, followed by TAE with treatment interval adjustment by 2 weeks. Treatment interval adjustment was not considered for changes in BCVA and PED.
Until 2017, the maximum treatment interval extension was 12 weeks; subsequently, in 2018, this was amended to 16 weeks. Treatment was discontinued when dry macula was confirmed at the maximum interval. After treatment cessation, the patients were asked to visit the clinic at 12 or 16 weeks after the last injection, which was equivalent to the maximum injection interval for each patient. In case of confirmation of dry macula, the patients were instructed to return after one month, followed by visit interval extension by 1 or 2 months. Successful treatment cessation was defined as dry macula retention without treatment for longer than 16 weeks after the last injections. In case of post-cessation recurrences, TAE was restarted with a 4-week injection interval. The treatment intervals were adjusted for two weeks.
We defined recurrence as recurrent intraretinal and subretinal hemorrhages or fluid accumulations after obtaining the dry macula, regardless of whether the patients were under treatment cessation. For each patient, we recorded the recurrence frequency after the loading phase within the study period.
Outcomes Measures
The main outcome measures were changes in BCVA during the first year and at the last visit. Other outcome measures included changes in BCVA and CRT over time, the proportion of eyes with maintained vision (<0.3 logarithm of minimum angle of resolution (logMAR) BCVA loss) at the last visit, proportion of eyes with good (≥20/40) and poor vision (<20/200) at the last visit, and number of annual injections. To evaluate and compare the long-term treatment burden according to the follow-up periods, we considered the number of annual injections and the observational period without anti-VEGF injections. To this end, we defined the index (estimated annual number of injections [EANI]) as follows: EANI = total injection number during the follow-up period/follow-up period (months) × 12.
Statistical Analyses
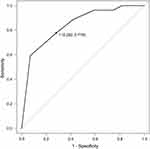
Statistical analyses were performed using the free statistical software R (4.0.2). Data obtained on the injection days were used for analyses of individuals under continuous treatment. Data were presented as mean ± standard deviation unless otherwise specified. We converted the BCVA from decimal visual acuity to the logMAR for statistical analyses and ETDRS letter score for among-study comparisons. The significance of changes in BCVA and CRT was determined using Friedman test. The Bonferroni test was used for post hoc analysis. Between-group comparisons of continuous variables were determined using the Kruskal–Wallis or Mann–Whitney U-tests. Between-group comparisons of categorical variables were determined using Fisher’s exact test. Logistic regression analyses were used to assess the correlation of early treatment response and recurrence frequency with the successful anti-VEGF treatment cessation. Receiver operating characteristic (ROC) curve analysis was performed to determine the cut-off value of the recurrence frequency for successful treatment cessations. Statistical significance was set at a two-sided P value of <0.05.
Results
During the study period, 140 eyes in 123 patients underwent anti-VEGF treatment by a single physician (TK) for exudative AMD and PN without other chorioretinal diseases. Subsequently, 39 eyes in 21 patients were excluded based on the exclusion criteria (Table S1). Finally, we included 101 eyes in 101 patients.
Patient Characteristics
Table 1 summarizes the baseline demographic data. All the included patients had a follow-up period of ≥1 year (mean follow-up period: 49.9 ± 26.9 months). Specifically, 79 (78.2%), 66 (65.3%), 54 (53.4%), and 43 (42.6%) patients were followed up for ≥2, ≥3, ≥4, and ≥5 years, respectively. Additionally, 32 (31.7%) patients discontinued the hospital visits before the final data collection (Table S1; mean follow-up period: 40.7 ± 23.4 months).
 |
Table 1 Baseline Demographic Data of the 101 Studied Patients |
Summary of Treatment
Prompt and deferred TAE were applied to 62 and 39 eyes, respectively. Fifty-six (55.4%), 15 (14.9%), and 30 (29.7%) eyes were treated using aflibercept only, ranibizumab only, and both agents, respectively. The mean ± SD injection number of aflibercept and ranibizumab were 19.1± 14.5 and 8.3 ± 5.9 in the aflibercept only group and ranibizumab only group, respectively. In both agents group, the mean ± SD injection number of aflibercept and ranibizumab were 21.9 ± 17.9 and 9.4± 9.4, respectively. In 24 (61.5%) eyes of 39 eyes initially treated with ranibizumab, switching of anti-VEGF agent to aflibercept was performed because of persistent disease activity. PDT and cataract surgeries were performed in 13 (12.8%) and 27 (26.7%) eyes, respectively.
Temporal Changes in BCVA
Figure 1 and Table 2 present the temporal changes in BCVA. Compared with the baseline BCVA (0.42 ± 0.41 logMAR), there was a significant improvement in the BCVA at 12 weeks (0.34 ± 0.36 logMAR, p = 0.004), but not at the first year (0.37 ± 0.43 logMAR, p = 0.067) and last visit (0.43 ± 0.45 logMAR, p = 1.000). Eighty-three (82.2%) eyes maintained vision at the last visit. The BCVA was 20/40 or better in 58 (57.4%) and 54 (53.5%) eyes at baseline and last visit, respectively. Moreover, the BCVA was 20/200 or worse in 15 (14.9%) and 14 (13.9%) eyes at baseline and last visit, respectively.
 |
Table 2 Visual Outcome, Central Retinal Thickness, and Treatment Frequency in Different Disease Types |
There were no significant between-disease differences in changes in BCVA at year 1 and last visit (p = 0.349 and p = 0.947, respectively; Table 2). The results were similar when they were analyzed with correction for age. There also were no significant differences in BCVA at year 1 and last visit between eyes treated with prompt and deferred TAE (p = 0.085 and p = 0.936, respectively), eyes treated and not treated with additional PDT (p = 0.444 and p = 0.331, respectively), and eyes of patients who completed and did not complete hospital visits until final data collection (p = 0.929 and p = 0.156, respectively). There were no significant differences in the baseline (p = 0.247) and final BCVA (p = 0.349) between eyes treated and not treated with cataract surgery; however, the BCVA at the first year was significantly worse in eyes treated with cataract surgery (p = 0.018).
Injection Frequency
The injection numbers from the first to fifth year were 6.8 ± 2.31, 4.6 ± 3.24, 4.7 ± 3.51, 4.5 ± 3.53, and 3.7 ± 3.64, respectively. The EANI for included eyes was 5.5 injections/year. There were no significant between-disease differences in EANI (p = 0.324). The injection number in the first year and EANI were significantly smaller in the deferred TAE group (4.8 ± 1.8 and 3.9 ± 2.5, respectively) than in the prompt TAE group (8.0 ± 1.7 and 6.5 ± 2.6, respectively; p < 0.001 for both). Multivariate regression analysis revealed an association of eyes without SRF at baseline (p = 0.045) and eyes treated with deferred TAE (p < 0.001) with smaller EANI (Table 3). At the last visit, 48 (47.5%) and 29 (28.7%) eyes were treated with a treatment interval of ≥12 and <8 weeks, respectively. There were no between-disease differences in the distributions (p = 0.478, p = 0.390, respectively, Table 2).
 |
Table 3 Multivariate Regression Analysis for Determinants That Could Affect the Estimated Annual Number of Injections |
Summary of the Treatment Course
Figure 2 summarizes the treatment course. During the study period, 56 (55.4%) eyes achieved ≥1 successful treatment cessation, with a median treatment-free period of 66 weeks. Additionally, 27 (26.7%) eyes were under successful treatment cessation at the last visit, with a median treatment-free period of 126 weeks. There were no between-disease differences in the distributions (p = 0.453 and p = 0.617, respectively; Table 2). Among the 27 eyes under successful treatment cessation at the last visit, 17 (63.0%), 4 (14.8%), 3 (11.1%), 2 (7.4%), and 1 (3.7%) eyes had 0, 1, 2, 3, and 5 recurrences, respectively, before successful treatment cessation.
Factors Associated with Treatment Cessation
Compared with eyes under continuous treatment, eyes under treatment cessation at the last visit had infrequent SRF at baseline (p = 0.032), frequent subretinal hyperreflective material at baseline (p = 0.036), infrequent disease activity at 12 weeks (p = 0.002), and a smaller recurrence number (p = 0.003, Table 4). Multivariate logistic regression analysis revealed an association of the absence of disease activity at 12 weeks and the recurrence number during the follow-up period with successful treatment cessation at the last visit (Table 5). Moreover, there was a significant association of successful treatment cessation during the follow-up period with a small recurrence number (p = 0.002), use of aflibercept during the loading phase (p = 0.011), and absence of PED at baseline (p = 0.017).
 |
Table 4 Comparison of Variables Between Eyes Under Continuous Treatment and Treatment Cessation |
 |
Table 5 Multivariate Logistic Regression Analysis of Factors Associated with Successful Treatment Cessation at the Last Visits and Successful Treatment Cessation During the Study Period |
ROC analysis with successful treatment cessation at the last visit, and recurrence number set as the objective and explanatory variables, respectively revealed an area under the curve of 0.841 (95% CI: –0.775–0.927, p < 0.001 against diagonal). The curve was closest to the upper-left corner with a sensitivity and specificity of 0.718 and 0.778, respectively, with a cut-off value for the recurrence number of ≤1 (Figure 3).
Central Retinal Thickness
The central retinal thickness was 390 ± 188.1 µm at baseline, which significantly decreased to 269.5 ± 135.2 µm at 12 weeks (p < 0.001). This significant decrease was maintained at year 1 and the last visit (p < 0.01 for both, Table 2).
Serious Adverse Events
Serious ocular adverse events included cataract progression, intraocular pressure elevation >30 mmHg, and retinal pigment epithelial tear in 27 (26.7%), 2 (2.0%), and 1 (1.0%) eye, respectively. Serious systemic adverse events included death, out-of-hospital cardiac arrest, arteriothrombotic events, and progressive dementia in 1 (1.0%), 1 (1.0%), 2 (2.0%), and 4 (4.0%) patients, respectively.
Discussion
We retrospectively examined the visual outcome in patients with exudative AMD and PN who were treated with anti-VEGF agents using the TAE regimen with a mean follow-up period of 4 years. There have been numerous reports regarding the outcomes of anti-VEGF therapy using the TAE regimen; however, the long-term outcomes remain unclear.19,23 The mean BCVA at year 1 was 0.37 logMAR (66.5 letters) with a mean gain of 2.7 letters. Although the visual gain was smaller than previously reported values, the absolute BCVA was comparable.11,14–16,19,20,23 Change in the BCVA at the last visit was −0.7 letters, which was worse than that reported by Traine et al and Berg et al (+3.6 letters and +7.4 letters, respectively).19,23 However, the absolute BCVA in our study was 0.43 logMAR (62.3 letters), which was comparable to those at year 4 in the previous reports (63.4 letters and 63.5 letters, respectively). Contrastingly, in our study, 53.5% of the eyes had good (≥20/40) final BCVA at the last visit, which was slightly better than that in the previous study (45.2%).23
Given that this was a retrospective study conducted at a common clinical practice, there were some minor protocol deviations, including one-week injection delays from the planned days. This could cause multiple recurrences, which leads to a less favorable visual outcome. Another reason for the lower improvement in our study may be our inclusion of eyes with better baseline BCVA than those in previous studies. In our study, 58 (57.4%) and 29 (28.7%) eyes had good (≥20/40) and excellent (≥20/25) baseline BCVA, respectively, with a mean BCVA of 63 letters. This could impede visual improvement due to the ceiling effect; moreover, as previously reported, these eyes could be vulnerable to vision loss.13,34 Furthermore, previous studies excluded eyes requiring additional treatment other than anti-VEGF treatment; however, we included these cases to represent real-world treatment outcomes of exudative AMD in common clinical practice.19,23 These may have contributed to the inconsistencies in the visual outcome.
There were no between-disease differences in visual outcomes. Matsumoto et al evaluated the efficacy of intravitreal aflibercept using the TAE regimen in Japanese patients with type 1 neovascular AMD and PN and reported similar treatment effectiveness in both diseases, which is consistent with our results.21 A randomized study on monthly or PRN regimens reported that patients with RAP lesions showed favorable visual outcome in the first year.26 Conversely, another study using the TAE regimen reported that RAP lesion was a predictive factor of poor visual outcome at year 2.17 The present study could not clarify this issue since we only included 9 eyes with RAP lesions. There is a need for future studies with larger sample sizes in each disease group and longer follow-up periods.
The number of treatments over time in our study was similar to that in a previous report.23 Compared with the monthly injection regimen, the TAE regimen reduces the injection number with comparable visual improvement.15,20 However, the TAE regimen may involve overtreatment for a certain proportion of eyes. Previous studies have shown that 20–34% of patients needed no additional injections after the loading phase during the first year.35–37 Similarly, in our study, 10 (25.6%) eyes treated with deferred TAE did not require additional injections after the three loading injections until the last visit, with a median follow-up period of 165 weeks. Recent studies have introduced more individually customized regimens with favorable visual outcomes and reduced injection numbers.37,38 These regimens involved initial monthly treatment until CNV stabilization with subsequent observation without treatment. Treatment was initiated after recurrence with the treatment interval being determined based on the disease recurrence interval. These regimens may allow overtreatment prevention, as well as reduction of the treatment burden, and possible adverse events.
Another effective measure for reducing the patients’ burden may be treatment cessation after stabilization following continuous treatment. Recent studies have reported successful treatment cessation in 14.8–26.0% of patients after continuous treatment.23,27,39 Similarly, in our study, approximately a quarter of all eyes were treatment-free at the last visit, with a median treatment-free period of 126 weeks.
Factors associated with frequent injections include PED and vitreomacular adhesion at baseline,40–43 as well as the use of ranibizumab rather than aflibercept.24 The correlation between SRF at baseline and treatment frequency remains unclear.20,40,41,43,44 In our study, the presence of SRF at baseline was associated with frequent injections. Moreover, the absence of PED at baseline and treatment initiation with aflibercept rather than ranibizumab were associated with successful treatment cessation for >16 weeks. This is consistent with previous findings. However, successful treatment cessation at the last visit was not associated with the aforementioned characteristics; rather, it was associated with the absence of disease activity at 12 weeks and fewer recurrences. Muether et al reported that intraocular VEGF levels did not correlate with CNV type or size.45 Therefore, based on only baseline phenotypical characteristics, it may be difficult to predict successful treatment cessation with VEGF suppression. Instead, clinicians may predict the long-term treatment cessation based on the early treatment response and the recurrence number.
In our study, ROC analysis revealed that the optimal cut-off value of the recurrence number for predicting successful treatment cessation at the last visits was 1. This suggests that eyes with ≥2 recurrences are unlikely to show long-term successful treatment cessation. This information may help physicians answer common questions from patients regarding whether they could achieve successful treatment cessation.
This study has several limitations. First, this was a retrospective study with a relatively small sample size, especially in disease subgroup analyses. Other limitations include the use of two different anti-VEGF agents, maximum treatment intervals, treatment regimens, and different follow-up period. Considerable patients underwent additional PDT and cataract surgery. These could limit the robustness of our findings. However, such heterogeneity is common in clinical practice for updating and providing better medical care, especially for relatively long-term follow-up periods. Lastly, since this study was performed to describe the results of AMD treatment in a common clinical practice, genetic background were not examined.
Conclusions
In conclusion, we reported the outcomes of anti-VEGF treatment for exudative AMD and PN using the TAE regimen. Visual acuity was maintained during the mean follow-up period of 4 years. Patients with good early response to treatment and fewer recurrences may achieve treatment cessation. This information may help clinicians provide more individualized anti-VEGF treatment and reduce the patients’ burden.
Abbreviations
VEGF, vascular endothelial growth factor; TAE, treat-and-extend; AMD, age-related macular degeneration; PN, pachychoroid neovasculopathy; BCVA, best-corrected visual acuity; PRN, pro re nata; CRT, central retinal thickness; CNV, choroidal neovascularization; PDT, photodynamic therapy; SD-OCT, spectral-domain optical coherence tomography; tnAMD, typical neovascular age-related macular degeneration; PCV, polypoidal choroidal vasculopathy; RAP, retinal angiomatous proliferation; ETDRS, Early Treatment of Diabetic Retinopathy Study; SRF, subretinal fluid, PED, pigment epithelial detachment; logMAR, logarithm of minimum angle of resolution; EANI, estimated annual number of injections; ROC, receiver operating characteristic, SD, standard deviation.
Data Sharing Statement
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
Ethics Approval and Informed Consent
This study was approved by the Institutional Review Board of Sapporo City General Hospital before participant recruitment (R02-059-730). The requirement for written informed consent was waived by the ethics committee because the analysis used anonymous clinical data that were obtained after each patient agreed to treatment by written consent. Instead, the patients were allowed “opt-out” consent.
Consent for Publication
We have not included any information or images requiring consent.
Acknowledgments
We would like to thank Editage for English language editing.
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Funding
No funding was received for this research.
Disclosure
The authors declare that they have no competing interest.
References
1. Bourne RRA, Jonas JB, Bron AM, et al. Prevalence and causes of vision loss in high-income countries and in eastern and central Europe in 2015: magnitude, temporal trends and projections. Br J Ophthalmol. 2018;102(5):575–585. doi:10.1136/bjophthalmol-2017-311258
2. Wong WL, Su X, Li X, et al. Global prevalence of age-related macular degeneration and disease burden projection for 2020 and 2040: a systematic review and meta-analysis. Lancet Glob Health. 2014;2(2):e106–e116. doi:10.1016/S2214-109X(13)70145-1
3. Kawasaki R, Yasuda M, Song SJ, et al. The prevalence of age-related macular degeneration in Asians: a systematic review and meta-analysis. Ophthalmology. 2010;117(5):921–927. doi:10.1016/j.ophtha.2009.10.007
4. Rosenfeld PJ, Brown DM, Heier JS, et al. Ranibizumab for neovascular age-related macular degeneration. N Engl J Med. 2006;355(14):1419–1431. doi:10.1056/NEJMoa054481
5. Brown DM, Kaiser PK, Michels M, et al. Ranibizumab versus verteporfin for neovascular age-related macular degeneration. N Engl J Med. 2006;355(14):1432–1444. doi:10.1056/NEJMoa062655
6. Heier JS, Brown DM, Chong V, et al. Intravitreal aflibercept (VEGF Trap-Eye) in wet age-related macular degeneration. Ophthalmology. 2012;119(12):2357–2548. doi:10.1016/j.ophtha.2012.09.006
7. Fung AE, Lalwani GA, Rosenfeld PJ, et al. An optical coherence tomography-guided, variable dosing regimen with intravitreal ranibizumab (Lucentis) for neovascular age-related macular degeneration. Am J Ophthalmol. 2007;143(4):566–583. doi:10.1016/j.ajo.2007.01.028
8. Spaide R. Ranibizumab according to need: a treatment for age-related macular degeneration. Am J Ophthalmol. 2007;143(4):679–680. doi:10.1016/j.ajo.2007.02.024
9. Engelbert M, Zweifel SA, Freund KB. ‘Treat and extend’ dosing of intravitreal anti-vascular endothelial growth factor therapy for type 3 neovascularization/retinal angiomatous proliferation. Retina. 2009;29(10):1424–1431. doi:10.1097/IAE.0b013e3181bfbd46
10. Singh RP, Stone TW, Hahn P, eds. 2019 Global Trends in retina Survey. Chicago, IL: American Society of retina specialists; 2019. Available from: https://www.asrs.org/international/global-trends-in-retina.
11. Gupta O, Shienbaum G, Patel AH, Fecarotta C, Kaiser RS, Regillo CD. A treat and extend regimen using ranibizumab for neovascular age-related macular degeneration clinical and economic impact. Ophthalmology. 2010;117(11):2134–2140. doi:10.1016/j.ophtha.2010.02.032
12. Engelbert M, Zweifel SA, Freund KB. Long-term follow-up for type 1 (subretinal pigment epithelium) neovascularization using a modified “treat and extend” dosing regimen of intravitreal antivascular endothelial growth factor therapy. Retina. 2010;30(9):1368–1375. doi:10.1097/IAE.0b013e3181d50cbf
13. Abedi F, Wickremasinghe S, Islam AF, Inglis KM, Guymer RH. Anti-VEGF treatment in neovascular age-related macular degeneration: a treat-and-extend protocol over 2 years. Retina. 2014;34(8):1531–1538. doi:10.1097/IAE.0000000000000134
14. Berg K, Pedersen TR, Sandvik L, Bragadóttir R. Comparison of ranibizumab and bevacizumab for neovascular age-related macular degeneration according to LUCAS treat-and-extend protocol. Ophthalmology. 2015;122(1):146–152. doi:10.1016/j.ophtha.2014.07.041
15. Wykoff CC, Croft DE, Brown DM, et al. Prospective trial of treat-and-extend versus monthly dosing for neovascular age-related macular degeneration: TREX-AMD 1-year results. Ophthalmology. 2015;122(12):2514–2522. doi:10.1016/j.ophtha.2015.08.009
16. Arnold JJ, Campain A, Barthelmes D, et al. Two-year outcomes of “treat and extend” intravitreal therapy for neovascular age-related macular degeneration. Ophthalmology. 2015;122(6):1212–1219. doi:10.1016/j.ophtha.2015.02.009
17. Matsumoto H, Morimoto M, Mimura K, Ito A, Akiyama H. Treat-and-extend regimen with aflibercept for neovascular age-related macular degeneration: efficacy and macular atrophy development. Ophthalmol Retina. 2018;2(5):462–468. PMID: 31047326. doi:10.1016/j.oret.2017.09.002
18. Adrean SD, Chaili S, Grant S, Pirouz A. Recurrence rate of choroidal neovascularization in neovascular age-related macular degeneration managed with a treat-extend-stop protocol. Ophthalmol Retina. 2018;2(3):225–230. PMID: 31047590. doi:10.1016/j.oret.2017.07.009
19. Berg K, Roald AB, Navaratnam J, Bragadóttir R. An 8-year follow-up of anti-vascular endothelial growth factor treatment with a treat-and-extend modality for neovascular age-related macular degeneration. Acta Ophthalmol. 2017;95(8):796–802. doi:10.1111/aos.13522
20. Silva R, Berta A, Larsen M, Macfadden W, Feller C, Monés J. Treat-and-extend versus monthly regimen in neovascular age-related macular degeneration: results with ranibizumab from the TREND Study. Ophthalmology. 2018;125(1):57–65. doi:10.1016/j.ophtha.2017.07.014
21. Matsumoto H, Hiroe T, Morimoto M, Mimura K, Ito A, Akiyama H. Efficacy of treat-and-extend regimen with aflibercept for pachychoroid neovasculopathy and type 1 neovascular age-related macular degeneration. Jpn J Ophthalmol. 2018;62(2):144–150. doi:10.1007/s10384-018-0562-0
22. Arendt P, Yu S, Munk MR, Ebneter A, Wolf S, Zinkernagel MS. Exit strategy in a treat-and-extend regimen for exudative age-related macular degeneration. Retina. 2018;39(1):27–33. doi:10.1097/IAE.0000000000001923
23. Traine PG, Pfister IB, Zandi S, Spindler J, Garweg JG. Long-term outcome of intravitreal aflibercept treatment for neovascular age-related macular degeneration using a “treat-and-extend” regimen. Ophthalmol Retina. 2019;3(5):393–399. doi:10.1016/j.oret.2019.01.018
24. Ohji M, Lanzetta P, Korobelnik JF, et al. Efficacy and treatment burden of intravitreal aflibercept versus intravitreal ranibizumab treat-and-extend regimens at 2 years: network meta-analysis incorporating individual patient data meta-regression and matching-adjusted indirect comparison. Adv Ther. 2020;37(5):2184–2198. PMID: 32222903; PMCID: PMC7467478. doi:10.1007/s12325-020-01298-x
25. Ohji M, Takahashi K, Okada AA, Kobayashi M, Matsuda Y; Terano Y for the ALTAIR investigators. Efficacy and safety of intravitreal aflibercept treat- and-extend regimens in exudative age-related macular degeneration: 52- and 96-week findings from ALTAIR. a randomized controlled trial. Adv Ther. 2020;37(3):1173–1187. doi:10.1007/s12325-020-01236-x
26. Ying G, Maguire MG, Daniel E, Huang J, Martin D. Association of baseline characteristics and early vision response with 2-year vision outcomes in the comparison of AMD treatments trials (CATT). Ophthalmology. 2015;122(12):2523–31.e1. doi:10.1016/j.ophtha.2015.08.015
27. Maguire MG, Martin DF, Ying G-S; Comparison of Age-related Macular Degeneration Treatments Trials (CATT) Research Group. Five-year outcomes with anti–vascular endothelial growth factor treatment of neovascular age-related macular degeneration: the comparison of age-related macular degeneration treatments trials. Ophthalmology. 2016;123(8):1751–1761. doi:10.1016/j.ophtha.2016.03.045
28. Warrow DJ, Hoang QV, Freund KB. Pachychoroid pigment epitheliopathy. Retina. 2013;33(8):1659–1672. doi:10.1097/IAE.0b013e3182953df4
29. Pang CE, Freund KB. Pachychoroid neovasculopathy. Retina. 2015;35(1):1–9. doi:10.1097/IAE.0000000000000331
30. Miyake M, Ooto S, Yamashiro K, et al. Pachychoroid neovasculopathy and age-related macular degeneration. Sci Rep. 2015;5(1):16204. doi:10.1038/srep16204
31. Hosoda Y, Yoshikawa M, Miyake M, et al. CFH and VIPR2 as susceptibility loci in choroidal thickness and pachychoroid disease central serous chorioretinopathy. Proc Natl Acad Sci U S A. 2018;115(24):6261–6266. doi:10.1073/pnas.1802212115
32. Yamashiro K, Hosoda Y, Miyake M, Ooto S, Tsujikawa A. Characteristics of pachychoroid diseases and age-related macular degeneration: multimodal imaging and genetic backgrounds. J Clin Med. 2020;9(7):2034. doi:10.3390/jcm9072034
33. Antiplatelet trialist collaboration. Collaborative overview of randomised trials of antiplatelet therapy prevention of death, myocardial infarction, and stroke by prolonged antiplatelet therapy in various categories of patients. BMJ. 1994;308(6921):81–106. doi:10.1136/bmj.308.6921.81
34. Ciulla TA, Hussain RM, Pollack JS, Williams DF. Visual acuity outcomes and anti–vascular endothelial growth factor therapy intensity in neovascular age-related macular degeneration patients: a real-world analysis of 49 485 eyes. Ophthalmol Retina. 2020;4(1):19–30. doi:10.1016/j.oret.2019.05.017
35. Holz FG, Amoaku W, Donate J, et al. Safety and efficacy of a flexible dosing regimen of ranibizumab in neovascular age-related macular degeneration: the SUSTAIN study. Ophthalmology. 2011;118(4):663–671. PMID: 21459217. doi:10.1016/j.ophtha.2010.12.019
36. Kuroda Y, Yamashiro K, Miyake M, et al. Factors associated with recurrence of age-related macular degeneration after anti-vascular endothelial growth factor treatment: a retrospective cohort study. Ophthalmology. 2015;122(11):2303–2310. PMID: 26271842. doi:10.1016/j.ophtha.2015.06.053
37. Ohnaka M, Nagai Y, Sho K, et al. A modified treat-and-extend regimen of aflibercept for treatment-naïve patients with neovascular age-related macular degeneration. Graefes Arch Clin Exp Ophthalmol. 2017;255(4):657–664. doi:10.1007/s00417-016-3507-7
38. Mantel I, Niderprim SA, Gianniou C, Deli A, Ambresin A. Reducing the clinical burden of ranibizumab treatment for neovascular age-related macular degeneration using an individually planned regimen. Br J Ophthalmol. 2014;98(9):1192–1196. doi:10.1136/bjophthalmol-2013-304556
39. Nishikawa K, Oishi A, Hata M, et al. Four-year outcome of aflibercept for neovascular age-related macular degeneration and polypoidal choroidal vasculopathy. Sci Rep. 2019;9(1):3620. doi:10.1038/s41598-019-39995-5.0
40. Ritter M, Simader C, Bolz M, et al. Intraretinal cysts are the most relevant prognostic biomarker in neovascular age-related macular degeneration independent of the therapeutic strategy. Br J Ophthalmol. 2014;98(12):1629–1635. doi:10.1136/bjophthalmol-2014-305186
41. Waldstein SM, Wright J, Warburton J, Margaron P, Simader C, Schmidt-Erfurth U. Predictive value of retinal morphology for visual acuity outcomes of different ranibizumab treatment regimens for neovascular AMD. Ophthalmology. 2016;123(1):60–69. doi:10.1016/j.ophtha.2015.09.013
42. Waldstein SM, Simader C, Staurenghi G, et al. Morphology and visual acuity in aflibercept and ranibizumab therapy for neovascular age-related macular degeneration in the VIEW trials. Ophthalmology. 2016;123(7):1521–1529. doi:10.1016/j.ophtha.2016.03.037
43. Ashraf M, Souka A, Adelman RA. Age-related macular degeneration: using morphological predictors to modify current treatment protocols. Acta Ophthalmol. 2018;96(2):120–133. doi:10.1111/aos.13565
44. Busbee BG, Ho AC, Brown DM, et al. Twelve-month efficacy and safety of 0.5 mg or 2.0 mg ranibizumab in patients with subfoveal neovascular age-related macular degeneration. Ophthalmology. 2013;120(5):1046–1056. PMID: 23352196. doi:10.1016/j.ophtha.2012.10.014
45. Muether PS, Hermann MM, Dröge K, Kirchhof B, Fauser S. Long-term stability of vascular endothelial growth factor suppression time under ranibizumab treatment in age-related macular degeneration. Am J Ophthalmol. 2013;156(5):989–993. doi:10.1016/j.ajo.2013.06
 © 2021 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2021 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.