Back to Journals » International Medical Case Reports Journal » Volume 17
Unusual Case of Right-Side Infective Endocarditis in a 40-Year-Old Woman with Postpartum Endometritis: A Case Report
Authors Markos S , Firdawoke SN, Gagamo ED, Workeneh MZ
Received 14 January 2024
Accepted for publication 28 March 2024
Published 3 April 2024 Volume 2024:17 Pages 275—279
DOI https://doi.org/10.2147/IMCRJ.S457389
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Xudong Zhu
Supplementary video of “Right-Side Infective Endocarditis in Postpartum Endometritis” [457389].
Views: 487
Sura Markos,1 Surafel Nadew Firdawoke,2 Eshetu Dabaro Gagamo,2 Mintesnot Zemedkun Workeneh2
1Department of Internal Medicine, Division of Cardiology, College of Medicine and Health Sciences, Hawassa University, Hawassa, Ethiopia; 2Department of Internal Medicine, College of Medicine and Health Sciences, Hawassa University, Hawassa, Ethiopia
Correspondence: Sura Markos, Tel +251-910878529, Email [email protected]
Abstract: Rarely observed during pregnancy and the postpartum period, right side infective endocarditis (IE) is particularly uncommon among non-drug-addicted individuals. Nonetheless, if it does occur, it poses significant health risks for both the mother and the fetus, even in the absence of pre-existing heart diseases. This case report describes a rare presentation of right-sided IE (IE) in a 40-year-old woman from rural Ethiopia with postpartum endometritis. The patient presented with atypical symptoms, making it challenging to identify the underlying cause. Through careful diagnostic evaluation and a multidisciplinary approach, the team successfully diagnosed and treated the patient, highlighting the importance of swift and accurate diagnosis for managing uncommon right-sided IE cases.
Keywords: postpartum, right-side endocarditis, postpartum endometritis
Introduction
Infective endocarditis (IE) is a serious and potentially life-threatening condition characterized by infection of the endocardium, involving the heart valves, cardiac devices, central catheters, and non-functional embryonic remnants of the right atrium, such as the eustachian valve. It poses a significant public health challenge worldwide and is associated with high mortality and morbidity.1,2 While left-sided IE is more frequently encountered, right-sided IE is relatively uncommon and is often associated with intravenous drug use (IVDU), Intracardiac devices, and central venous catheters.2 This case report aims to shed light on a unique case of right-sided IE occurring in a 40-year-old woman who came from a rural part of Ethiopia with postpartum endometritis after home delivery, with no other known risk factors of IE.
Case Presentation
This is a 40-year-old Para VIII woman from a rural part of Ethiopia, who is on her 10th postpartum day after she delivered a live male neonate vaginally at home. Unfortunately, the neonate died three days after delivery at home. The patient did not undergo regular antenatal follow-up during pregnancy.
The patient presented with a complaint of fever of 1 week duration. The fever was of a high-grade and persistent type associated with lower abdominal pain, foul-smelling vaginal discharge, chills, rigors, global-type headache, tinnitus, vertigo, and easy fatigability. On further inquiry, she had a history of cough associated with whitish sputum for three days. She also reported palpitations, pleuritic chest pain, and shortness of breath on mild exertion.
Otherwise, she denied illicit intravenous (IV) drug use, no history of any intra-cardiac device use, no history of childhood cardiac illness, no history of tooth extraction, no history of renal disease, no history of central venous catheter insertion, no previous history of similar illness, and no known medical illness. She visited a nearby hospital and was referred to our hospital for blood transfusion and further management.
Upon arrival at our hospital, the patient was admitted to the GYN/OBS ward. Physical examination revealed that she was acutely sick, with vital signs of pulse rate (PR) 124 beats per minute, respiratory rate (RR) 36 breaths per minute, temperature (T) 38.4°C, and blood pressure (BP) 127/87 mmHg. There was decreased air entry in the bilateral lower 1/3 of the posterior chest and the bibasilar rales. There was a grade III systolic murmur along the left sternal border, with no radiation. Abdominal examination, there was 19 weeks sized uterus, with mild tenderness upon palpation. Digital pelvic examination revealed dark-red foul-smelling vaginal discharge on the examination glove. Leg swelling or calf tenderness was not observed. There were no skin or mucosal stigmata of endocarditis, lymphadenopathy, signs of meningism, or neurological symptoms or signs. In the laboratory workup, the complete blood count (CBC) profile revealed a white blood cell (WBC) count of 6240/mm3, platelet count of 203,000/mm³, hemoglobin of 6 g/dL, hematocrit of 24 g/dL, mean corpuscular volume (MCV) of 64fl, Erythrocyte sedimentation rate (ESR) of 100 mm/h, and urine analysis showed protein of +4 and blood +2. Blood and urine cultures were unremarkable and other baseline laboratory results were normal. Lumbar Puncture was performed (CSF analysis was non revealing). Rapid diagnostic Test (RDT) and blood film testing for malaria were repeatedly negative.
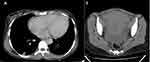
Abdominopelvic ultrasound revealed that sub involuted uterus, minimal free peritoneal collection, minimal hypo-echoic pelvic collection suggestive of Peripartal pelvic infection and later on Abdominopelvic CT scan including lower chest was done and showed bilateral peripheral lower lung patchy nodular opacities and enlarged uterus with subinvolution suggestive of Endometritis and septic pulmonary embolism (Figure 1) and chest x-ray as shown below (Figure 2).
Echocardiography revealed a large tricuspid valve vegetation with tricuspid regurgitation and dilated right chambers (Figure 3 and Supplementary Video).
Treatment and Outcome
Initially, she was admitted to the Gynecology and Obstetrics Department with a diagnosis of puerperal sepsis secondary to endometritis along with severe anemia due to acute blood loss. The treatment plan consisted of metronidazole 500 mg intravenously (IV) three times daily (TID) and ceftriaxone 1 g IV twice daily (BID) administered for 5 days. In addition, the patient received four units of cross-matched blood transfusions. However, despite antibiotic administration, her symptoms worsened.
Consequently, the antibiotic regimen was revised to include broad-spectrum antibiotics, and artesunate (antimalarial therapy) was added owing to the endemicity of malaria in the region, despite repeated negative blood films for malaria. Four days after the revised antibiotic approach, the patient’s fever did not subside, and decided to pursue total abdominal hysterectomy as a last resort to treat sepsis. This decision was based on the refractory nature of sepsis caused by endometritis. Concurrently, a medical consultation was sought and echocardiography was performed, revealing the presence of a large tricuspid valve vegetation.
Subsequently, the patient was transferred to an Internal Medicine ward with a diagnosis of right-sided IE associated with postpartum endometritis. Vancomycin (1 g IV twice daily) was initiated and continued for 4 weeks. Over time, the patient’s fever subsided and her hemodynamic condition stabilized. Consequently, the patient was discharged in an improved state. During discharge, the patient was advised to attend regular follow-up appointments at our cardiac clinic. Additionally, she was provided with information on various contraceptive methods including bilateral tubal ligation.
Discussion
Right-sided IE accounts for 5–10% of all IE cases and is often associated with IVDU, intracardiac devices, and central venous catheters.3
Pregnancy and postpartum IE carry a high risk of maternal and fetal mortality, with rates ranging from 10% to 15%. This condition commonly leads to left-sided IE, frequently affecting the mitral valve. While it is uncommon in non-intravenous drug abusers during pregnancy and the postpartum period, it is associated with IVDU and the presence of cardiac devices, similar to the general population.2–4
To the best of our knowledge, there have been few reports in the scientific literature that directly link right side IE to postpartum endometritis-associated sepsis (also known as puerperal sepsis). However, there have been reports of native tricuspid valve IE following septic abortion.5–7
In cases of right-sided IE, the tricuspid valve is predominantly affected (>90%), either alone or along with the pulmonary valve, right ventricular outflow tract, right ventricular free wall, embryonic remnants of the right atrium (eustachian valve), and very rarely, the pulmonary valve affects alone.3,6
The diagnosis of right-sided IE is usually delayed, especially in non-IV drug addicts, owing to its atypical presentation. The signs and symptoms are relatively different from left-sided IE, and some patients lack traditional risk factors for IE, as was the case with our patient, who presented with puerperal sepsis. This unique clinical presentation often leads to a misdiagnosis or mistreatment, making the diagnosis of right-sided IE an exception. Therefore, a strong clinical suspicion is necessary to establish a diagnosis, as the Dukes diagnostic criteria for IE are rarely support right-sided cases. Any echocardiographic features indicating vegetation involvement in the right heart structures, along with positive blood cultures showing a typical organism, should be considered diagnostic for right-sided endocarditis.2,3,8,9
The mainstay treatment for right-sided IE is intravenous antibiotics that are directed towards the most common pathogenic organisms based on empirical antibiotic coverage or blood culture sensitivity tests. In certain cases, such as ours, where the majority of blood cultures are negative because of prior antibiotic exposure prior to blood collection or poor sampling techniques, empirical antibiotics targeting staphylococcus spp are recommended. Compared to left side IE, Right side IE has a good prognosis and responds well to medical therapy alone; surgery is reserved for those who fail medical therapy.9–11
Therefore, this is a rare case of right-sided IE occurring during the postpartum period as part of puerperal sepsis in the absence of any other risk factors such as IVDU. The patient responded well to the medical treatment and was successfully discharged.
Conclusion
This case report underscores the need for vigilant evaluation and consideration of Right side IE, particularly atypical cases. Successful management of right-sided IE in this patient with a history of postpartum endometritis highlights the importance of prompt diagnosis and interdisciplinary collaboration. By sharing such cases, we contribute to the knowledge base and enhance the awareness of unusual manifestations of right-sided IE in the absence of other traditional risk factors.
Ethical Issue
The patient provided written informed consent for publication of this case, and case-specific information and images were included in the consent form. This institution does not require ethical approval for publication of a single case report.
Acknowledgment
We’d like to thank our patient for permitting us to write this case.
Funding
No specific grant from funding organizations in the public, private, or nonprofit sectors has been provided for this manuscript.
Disclosure
The authors report no conflicts of interest in this work.
References
1. Momtazmanesh S, Saeedi Moghaddam S, Malakan Rad E, et al. Global, regional, and national burden and quality of care index of endocarditis: the global burden of disease study 1990–2019. Eur J Prev Cardiol. 2022;29:1287–1297. doi:10.1093/eurjpc/zwab211
2. Baddour LM, Wilson WR, Bayer AS, et al. Infective endocarditis in adults: diagnosis, antimicrobial therapy, and management of complications: a scientific statement for healthcare professionals from the American Heart Association. Circulation. 2015;132(15):1435–1486. doi:10.1161/CIR.0000000000000296
3. Shmueli H, Thomas F, Flint N, Setia G, Janjic A, Siegel RJ. Right‐sided infective endocarditis 2020: challenges and updates in diagnosis and treatment. J Am Heart Assoc. 2020;9(15):e017293. doi:10.1161/JAHA.120.017293
4. Kebed KY, Bishu K, Al Adham RI, et al. Pregnancy and postpartum infective endocarditis: a systematic review. In
5. Baniya A, Duwadee P, Sujata KC, et al. Infective endocarditis of tricuspid valve following septic abortion: a case report. Ann Med Surg. 2023;85(12):6262–6265. doi:10.1097/MS9.0000000000001437
6. Grover A, Anand IS, Varma J, et al. Profile of right-sided endocarditis: an Indian experience. Int J Cardiol. 1991;33(1):83–88. doi:10.1016/0167-5273(91)90155-I
7. Aslam AF, Aslam AK, Thakur AC, Vasavada BC, Khan IA. Staphylococcus aureus infective endocarditis and septic pulmonary embolism after septic abortion. Int J Cardiol. 2005;105(2):233–235. doi:10.1016/j.ijcard.2004.11.020
8. Varona JF, Guerra JM. Tricuspid valve endocarditis in a nonaddicted patient without predisposing myocardiopathy. Revista Española De Cardiología. 2004;57(10):993–996. doi:10.1016/S0300-8932(04)77229-2
9. Muñoz AF, Vargas DA. Right-sided infective endocarditis. Infect Endocarditis. 2019;2019:1.
10. ESC Scientific Document Group. 2023 ESC guidelines for the management of endocarditis: developed by the task force on the management of endocarditis of the European Society of Cardiology (ESC) Endorsed by the European Association for Cardio-Thoracic Surgery (EACTS) and the European Association of Nuclear Medicine (EANM). Eur Heart J. 2023;2023:1.
11. Hussain ST, Witten J, Shrestha NK, Blackstone EH, Pettersson GB. Tricuspid valve endocarditis. Ann Cardiothorac Surg. 2017;6(3):255–261. doi:10.21037/acs.2017.03.09
 © 2024 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2024 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.