Back to Journals » HIV/AIDS - Research and Palliative Care » Volume 15
Unsafe Infant Feeding Practice and Associated Factors Among HIV Positive Mothers Attending PMTCT in Ethiopia: A Cross-Sectional Study
Authors Zewdu D, Bekele DM , Bantigen KA, Wake AD
Received 12 April 2023
Accepted for publication 9 June 2023
Published 14 June 2023 Volume 2023:15 Pages 325—337
DOI https://doi.org/10.2147/HIV.S414636
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Prof. Dr. Olubunmi Akindele Ogunrin
Demlie Zewdu,1 Daniel Mengistu Bekele,2 Kerebih Abere Bantigen,2 Addisu Dabi Wake3
1Nursing Department, College of Health Sciences, Samara University, Afar, Ethiopia; 2School of Nursing and Midwifery, College of Health Sciences, Addis Ababa University, Addis Ababa, Ethiopia; 3Nursing Department, College of Health Sciences, Arsi University, Asella, Ethiopia
Correspondence: Addisu Dabi Wake, Nursing Department, College of Health Sciences, Arsi University, P.O. Box 193/04, Asella, Ethiopia, Tel +251 910 2867 66, Email [email protected]
Introduction: Infant feeding practices can have an impact on the health of infants born to HIV-positive mothers. Breastfeeding has significant health advantages for newborns even while it increases the risk of HIV transmission from an HIV-positive mother to her child. One-third to half of child HIV infections in African settings may be linked to breastfeeding. This study was intended to investigate the level of unsafe infant feeding practice and associated factors among HIV positive mothers attending PMTCT at selected governmental hospitals in Afar regional state, Ethiopia, 2022.
Methods: A cross-sectional study was done among 423 HIV positive mothers from February 15 to March 15, 2022 in Afar regional state at selected PMTCT providing governmental hospitals. The proportional allocation was done for samples to be taken from Asayta, Dupti and Mohammed Akle hospitals. A systematic sampling technique was performed to select the study participants. Epidata version 3.1 was used for data entry, and SPSS software version 23 was used for statistical analysis.
Results: The majority, 296 (70.0%), of mothers with HIV-positive were aged between 25 and 34 years. The level of unsafe infant feeding practice among HIV-positive mothers was 153 (36.2%). About 270 (63.8%) mothers exclusively breastfed their infants. In multivariable logistic regression analysis, PNC follow-up (AOR=1.814, 95% CI: (1.127, 2.919)), ART follow-up (AOR=1.987, 95% CI: (1.128, 3.501)), and HIV disclosure status (AOR=2.324, 95% CI: (1.470, 3.673)) were significantly associated with unsafe infant feeding practice among HIV-positive mothers.
Conclusion: The level of unsafe infant feeding practice among HIV-positive mothers was high. PNC follow-up, ART follow-up, and HIV disclosure status were significantly associated with unsafe infant feeding practice among HIV-positive mothers. Comprehensive health educations need to be provided for HIV-positive mothers to reduce this problem.
Keywords: AIDS, infant feeding practice, HIV, Afar regional state, Ethiopia, nutrition
Introduction
A serious infection known as acquired immunodeficiency syndrome (AIDS) is brought on by the virus known as human immunodeficiency virus (HIV). During pregnancy, delivery, and breastfeeding are the main times when the virus is passed from an infected mother to her child. If no precautions are taken, between 20% and 45% of infants would be afflicted. HIV infection risk ranges from 5% to 20% while nursing.1
Infant feeding practices, which are modifiable, can have an impact on the health of infants born to HIV-positive mothers. Breastfeeding is the most efficient way to lower the risk of developing common childhood morbidities.2,3 Breastfeeding has significant health advantages for newborns even while it increases the risk of HIV transmission from mother to child. One-third to almost half of child HIV infections in Africa are brought on by breastfeeding.3 The risk of HIV infection in breastfed children can be reduced by cutting down on nursing time, breastfeeding exclusively for the first six months, and preventing, detecting, and treating oral and breast issues.4 HIV-positive women are advised to practice Exclusive replacement feeding (ERF) and Exclusive breast feeding (EBF) for the first six months to increase the likelihood that their children will be HIV-free.4
The World Health Organization’s (WHO) 2010 recommendations represent a turning point in terms of policy advances and clarity, and should lead to far fewer HIV infections and deaths in infants and young children. Infant feeding practices recommended to mothers known to be HIV-positive should support the greatest likelihood of HIV-free survival of their children and not harm the health of mothers. Recommendations on infant feeding and HIV and mortality, and at the same time ensuring that the mothers receive appropriate HIV care and support including ARVs. The revisions capitalize on the maximum benefit of breastfeeding to improve the infant’s chances of survival while reducing the risk of HIV transmission, and are based on the assumption that HIV-positive mothers will either receive lifelong ARV treatment to improve their own health, or if not eligible for treatment, the mother or infant will take ARVs as prophylaxis while breastfeeding.5 According to WHO (2016) recommendations, mothers living with HIV should breastfeed for at least 12 months and may continue breastfeeding for up to 24 months or longer (similar to the general population) while being fully supported for ART adherence if she is receiving ART and there is no evidence of clinical, immune or viral failure.6
The mother’s knowledge of newborn feeding procedures may have an impact on the transmission of HIV from mother to child.1 Studies show that HIV is widespread in various parts of Ethiopia. An Ethiopian demographic health survey done in 2016 revealed that Addis Ababa, South Eastern Tigray, the towns of Oromia, regional state around Addis Ababa, and the majority of towns in Afar and Amhara regional states were epidemic areas.2 But there is little proof that the practice of newborn feeding contributes to this issue.3
About 18.2 million people have access to ART services, according to the 2021 report on worldwide HIV statistics. In 2020, there were about 37.7 HIV-positive individuals. About 1.5 million people contracted the virus for the first time this year. Between 1.2 million and 2.2 million of those with HIV were children (0–14 years age). By 2020, AIDS had caused approximately 680,000 deaths.7 At least two-thirds of all HIV diagnoses and fatalities occur in sub-Saharan Africa, where the pandemic is the most prevalent. Breastfeeding is the main factor in the region for >95% of pediatric HIV infections, which are caused by mother to child transmission (MTCT). The wellbeing of children is often strongly correlated with nursing, according to economic and social circumstances.8
Super Fast-Track Framework, a worldwide action plan that was introduced in 2017, proved successful in preventing new pediatric HIV infections. The needs of children and adolescents influenced HIV prevention and therapy.9 Breastfeeding offers both potential life-saving benefits and an HIV transmission risk in mothers who are HIV positive. The primary issues that need to be addressed are how to enhance healthy dietary requirements and how to improve baby life.10
By 2020, roughly 75,000 youngsters in eastern and southern Africa would have been newly infected with HIV.7 Without ART, there is a 15% to 45% possibility of transfer from mother to child during pregnancy, delivery, and breastfeeding. ART can reduce the chance of transmission to less than 5%.11 By 2020, about 57% of HIV-infected children in eastern and southern Africa have access to antiretroviral therapy (ART).7 It is estimated that 1000 children each day are affected by mother-to-child transmission. According to the United Nations program on HIV/AIDS (UNAIDS), breast milk contributes 15% of HIV transmission, and there are other factors that enhance the risk from 25% to 45%. Age of the infant and mixed feeding before 6 months of age are examples of such influences.12 The majority of African studies found that breast feeding for lengthy periods of time increased the risk of HIV infection by 4–20.13
HIV/AIDS is a major health-care priority in Ethiopia. Despite the fact that the country achieves 97% national PMTCT implementation and gains basic changes at the start of the program, it remains one of the top ten countries in the world with the highest burden of childhood HIV infection due to MTCT, and it remains a major challenge for the country.14 In Ethiopia, 74% of women are aware that HIV can be transferred through breast milk. Approximately, 58% of infants under the age of six months are exclusively breastfed. Around 17% of infants were breastfed with plain water and there were about 5% infants who never fed breast milk.4
Even while PMTCT lessens the risk of transmission, HIV infection can still occur through baby feeding habits, especially mixed breast feeding. All newborn feeding methods were frequently utilized in Ethiopia, including ERF, EBF, and mixed feeding (MF), but there was a gap in safe infant feeding practice. This disparity is primarily attributable to the country’s economic situation. The majority of individuals have a low socioeconomic status, making it difficult to obtain all necessary foods that can be used as a substitute for breast milk. There has been no study done on unsafe infant feeding practice and associated factors among HIV positive mothers attending PMTCT at selected governmental hospitals in the study setting, even worldwide, there is a limitation of the study on this critical problem. This would make information scarcity for the concerned bodies to react up on it and solve it timely as much as possible. Therefore, the findings of this study would fill this gap, providing the insight to all concerned bodies.
Methods
Study Area and Period
From February 15 to March 15, 2022, a study was undertaken in Afar Regional State at selected PMTCT-providing governmental hospitals. The Afar Region, which covers an area of around 94,760 square kilometers, is located in north-eastern Ethiopia. It borders Eritrea in the north, Tigray in the north-west, Oromia in the south, Somalia in the south-east, Amhara in the west, and the Republic of Djibouti in the east. Five zones and thirty-two districts make up the region, which has seven hospitals and 105 health centers.15 Hotel and home-based female sex workers (FSW) in the Afar Region conduct transactional sex. The majority of adolescent girls engage in sexual encounters with older men, such as migrant laborers and truck drivers. These teenagers have minimum knowledge of HIV/AIDS. Substance usage (khat and shisha) as well as a reduction in the use of preventive measures such as condoms contribute to the spread of HIV/AIDS in the country.16
Study Design
Institution-based cross-sectional study was conducted.
Source Population
All HIV-positive mothers in Afar Regional State, who have a child under the age of one year and are undergoing PMTCT at governmental hospitals.
Study Population
HIV-positive mothers with children under the age of one year who were followed up on at Afar regional states randomly selected PMTCT service providing governmental hospitals.
Inclusion Criteria and Exclusion Criteria
HIV positive mothers having less than one-year-old child who were attending PMTCT in selected governmental hospitals in Afar regional state, from February 15 to March 15, 2022 were included in this study. Whereas, HIV positive mothers having greater than one-year-old children who were attending PMTCT in the selected governmental hospitals were excluded.
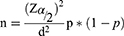
Sample Size Determination
Using a single population proportion formula with a 95% confidence interval, a 5% margin of error, and a 50% proportion of infant feeding practice, the sample size was calculated.
n = 384
Where: n = required sample size
Zα/2 = critical value for normal distribution at 95% confidence interval which equals to 1.96
P = proportion to be estimated (50%)
d = absolute precision (margin of error 5%)
n = 384-by adding 10% non-response rate, the sample size was
n=423
Sampling Technique and Procedure
Three PMTCT-providing hospitals were chosen at random from all governmental hospitals in the Afar Regional state by using simple random sampling (lottery method). The hospitals chosen are Asayta, Dupti and Mohammed Akle. The Sample frame was a card number from an appointment book belonging to HIV positive mothers. The mothers for the interview were chosen through a systematic sampling process. The sample size was computed using PMTCT providing hospitals that was chosen at random. A proportional allocation of the number of cases from each hospital to participate in the study was evaluated. Proportional sample size allocation = was used. The proportional allocated samples for Asayta, Dupti and Mohammed Akle are displayed in figure below (Figure 1).
was used. The proportional allocated samples for Asayta, Dupti and Mohammed Akle are displayed in figure below (Figure 1).
 |
Figure 1 Sampling Procedure of a study on infant feeding practices of HIV positive mothers attending PMTCT services in selected governmental hospitals in Afar regional state, Ethiopia, 2022. |
where N = total number of HIV positive mothers
nf = final sample size of the study, which is 423
nj = number of HIV positive mothers in each hospital
Study Variables
Dependent Variables
- Infant feeding practices
Independent Variables
- Socio demographic variables: Maternal age, marital status, occupation, religion, ethnicity, educational status, monthly income, age of child.
- Maternal related factors: Disclosure status of HIV, antenatal care (ANC) follow up, postnatal care (PNC) follow up, ART follow up, place of birth, type of delivery.
- Maternal and infant health condition: Infant mouth ulcer, mother’s breast problem.
- Health workers related factors: Counseling by health worker.
Operational Definition
Infant feeding practices: a collection of guidelines for the proper feeding of newborns and infants in order to avoid HIV transmission from mother to child. It could be safe or unsafe.
Safe infant feeding practice: Up to six months, the percentage of mothers who exclusively breastfed their infants.
Unsafe infant feeding practice: Proportion of mothers who practiced mixed feeding up to six months. Unsafe infant feeding practice can be associated with infant health issues like diarrhea and malnutrition.17
Exclusive breast feeding: Giving the infant no other food or drink, including water, other than breast milk (including expressed breast milk), with the exception of drops or syrups containing vitamins, mineral supplements or prescribed medicines.
Exclusive replacement feeding: feeding a kid who is not receiving breast milk with infant commercial or home produced milk for the first six months, or until the child is fully nourished on family foods, whichever comes first, or the infant if younger than six months. This should be done with an acceptable breast-milk substitute, such as a commercial formula or a home-made formula supplemented with micronutrients.
Mixed breast feeding: Breastfeeding with non-human milk, fluids, water, solid feeds for the first 6 months of life or until the day of the interview if the infant is less than six months. They began supplementing the infant’s diet when he or she was less than six months old.
Tools for Data Collection
Data were collected using a pretested structured questionnaire adapted from a review of relevant literatures.17 The questions and statements were sorted and ordered based on the goals that could be addressed. The questionnaire was content validated by experts after being modified to the local context and the research objective by the investigator and translated into Amharic language and Amharic version was back translated into English. The investigator verified for consistency between the original and back translated versions to ensure dependability and validity.
Data Quality Control and Collection Process
Before the real survey, a pretest was performed on 5% of the samples at Logya hospital and Samara health center, and significant changes were made based on the results. Many redundant and undesirable variables were eliminated. Cronbach’s alpha was used to verify the tool’s reliability after it had been validated and pretested (0.76).
Three BSc Nurses conducted face-to-face interviews and observations at PMTCT providing units to collect data. The principal investigator gave data collectors a one-day training and orientation on the study’s purpose and relevance, how to gather and record the relevant information, data collection methodologies, the entire content of the questionnaire, and maintaining confidentiality. One supervisor (MSc Nurse) and the primary investigator were in charge of the data collectors at all times. The collected data was reviewed for completeness at the end of each day, and a corrective discussion was held with all data collectors for the next day’s data collection.
Statistical Analysis
Epidata version 3.1 was used for coding and data entry. SPSS software version 23 was used to clean and analyze the data. Descriptive statistics was performed. Bivariable and multivariable logistic analyses were utilized to evaluate the relationship between independent variable and infant feeding practice. To control for potential confounders, the variables that indicated a connection with the outcome variable in the Bivariable logistic analysis with a p value <0.25 were moved into the final multivariable logistic regression model. The Hosmer and Lemeshow test was used to determine model fitness, not significant (p value = 0.17). To examine the strength of the link, an adjusted odds ratio (AOR) was calculated with a 95% CI, and a p value <0.05 was considered significant. Tables and figures were used to display the result.
Result
Sociodemographic Characteristics
The study included a total of 423 mothers who were HIV positive and had children under the age of one year. There was a 100% response rate. Three hundred twenty-four mothers (76.6%) who reported their marital status were married. About 35.5% of mothers were grade 1–8 educated in terms of maternal education (Table 1).
 |
Table 1 Sociodemographic Characteristics of HIV Positive Mothers Attending PMTCT at Selected Governmental Hospitals in Afar Regional State, Ethiopia, 2022 [N = 423] |
Maternal Related Factors
More than half (60%) of the 423 respondents, or 254, attended ANC follow-up during their recent pregnancy. Of the mothers, 272 (64.3%) made their HIV status known. Only 7.5% of mothers went for a fourth ANC visit (Table 2).
 |
Table 2 Maternal-Related Factors of HIV Positive Mothers Attending PMTCT at Selected Governmental Hospitals in Afar Regional State, Ethiopia, 2022 [N = 423] |
Mother and Infant Health Conditions
Less than half (173, 40.9%) of the mothers had encountered breast problems. Majority 352 (83.2%) of the infants had not encountered an oral ulcer (Table 3).
 |
Table 3 Health Condition of Mother and Infant Among HIV Positive Mothers Attending PMTCT at Selected Governmental Hospitals in Afar Regional State, Ethiopia, 2022 [N = 423] |
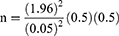
Counseling Practice of Health Workers
Most (318, 75.2%) of the mothers answered that the health worker explained to them about different feeding options (Figure 2).
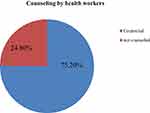 |
Figure 2 Counseling practice of health workers on infant feeding options among HIV positive mothers attending PMTCT at selected governmental hospitals in Afar regional state, Ethiopia, 2022 [n= 423]. |
Level of Infant Feeding Practice
The majority of respondents, 270 (63.8%), exclusively breastfed their infants for the first six months, which is a safe feeding technique, whereas just 153 (36.2%) mothers mix breast milk with other foods (Figure 3). A total of 423 women (100%) had ever breastfed their child. None of the mothers who responded used replacement feeding exclusively.
 |
Figure 3 Level of infant feeding practices among HIV positive mothers attending PMTCT at selected governmental hospitals in Afar regional state, Ethiopia, 2022 [n= 423]. |
Factors Affecting Infant Feeding Practice
Bivariable logistic analysis revealed significant relationship between infant feeding practice and maternal education, ANC follow-up, ART follow-up, revelation of HIV status and health-care provider advice on various feeding alternatives. However, PNC follow-up, ART follow-up and disclosure status of HIV were found to be substantially linked with unsafe infant feeding practice in the multivariable logistic regression.
When compared to their counterparts, HIV-positive women who did not receive PNC follow-up were two times more likely to practice unsafe feeding practices (AOR = 1.814, 95% CI: 1.127–2.919). When compared to other HIV-positive women, those who did not receive ART follow-up were two times more likely to practice unsafe feeding practice (AOR = 1.987, 95% CI: 1.128–3.501). HIV positive mothers who did not disclose their HIV status to others were 3 times more likely to practice unsafe infant feeding (AOR = 2.324, 95% CI: 1.470–3.673) as compared to mothers who did disclose their HIV status (Table 4).
Discussion
In 2021, the estimated figure of children aged 0–19 who were living with HIV were 2.73 million worldwide. Daily, around 850 children became infected with HIV and about 301 children died from AIDS-related causes, such as insufficient access to HIV prevention, care and treatment services.18 The objective of this study was to investigate unsafe infant feeding practices and associated factors among HIV positive mothers undergoing PMTCT in selected governmental hospitals in Afar Regional state, Ethiopia.
The finding of this study showed that 63.8% of HIV-positive mothers exclusively breastfed their infants for the first six months. This study finding is greater than the study report of SNNPR regional state, Ethiopia 56.3%.1 This might be because the majority of the respondents received advice regarding the benefits and drawbacks of EBF as a safe feeding technique from health-care professionals. But practicing EBF is not that much excellent. This might be related to that all mothers who were counseled about different feeding options did not feed their child as they had counseled.
This study finding is consistent with the study conducted in southern Ghana (62%).19 However, the finding of this study is lower than the that study conducted in Nigeria (91.4%), Mekele (90%), Jigjiga (93.6%), and Shashemene (96.6%).8,20–22 These major differences might be the result of cultural differences in feeding practice and economic potential; most of mothers have poor economic status and for life they had gone out of home immediately after giving birth to work any job and separated from their infant for several hours. By this reason, an infant is obligated to feed any food/cereals which are found in the house. For the first six months, none of HIV-positive mothers had engaged in exclusive replacement feeding. This might be due to current cost inflation and almost all mothers cannot afford to buy the formula food.
About 36.2% of respondents in the study had experienced mixed feeding. The result was consistent with research done in SNNPR (35.6%),1 and southern Ghana (40%).19 However, it was greater than studies conducted in Kenya, Addis Ababa, Bahir Dar, and Debre Markos, 18.2%, 23%, 10.9%, and 14.2%, respectively.4,10,11,17 The majority of mothers’ expectations that breast milk alone is not sufficient for the infant might be the main causes of this disparity. In this study, 72.6% of mothers had PNC follow-up, which is less than the studies done in Shashemene (100%), Bahir Dar (94.3%) and Mekele (96.1%).17,21,22 This might be due to health extension workers and other health professionals might not have enough house-to-house visits after the mother returned to her home as a result of the challenging weather condition.
In this study, 56.7% mothers of them had ART follow-up, which is less than the studies conducted in Debre Markos (70.8%), Shashemene (97.9%) and Mekele (76.3%).10,21,22 Besides, it was lower than the study done in SNNPR, which reported ART follow-up (60.7%).1 This might be because mothers are more aware of the value of ART in preventing HIV transmission from mother to child. This might also be connected to various pharmacological adverse effects and insufficient rehabilitative health worker education. In this study, 64.3% of mothers had disclosed they were HIV positive. This finding was lower than the studies done in Bahir Dar (79.6%), Debre Markos (88.8%), Mekelle (90.3%) and SNNPR (95.6%).1,10,17,21 This might relate to fear of stigma and discrimination.
When compared to their counterparts, HIV-positive women who did not receive PNC follow-up were two times more likely to practice unsafe feeding practices (AOR = 1.814, 95% CI: 1.127–2.919). This might be due to that HIV-positive woman who did not receive ART follow-up missed the information about infant feeding, which would be provided at the PNC follow-up.
When compared to other HIV-positive women, those who did not receive ART follow-up were two times more likely to practice unsafe feeding practice (AOR = 1.987, 95% CI: 1.128–3.501). According to the WHO suggestion, all HIV-positive mothers should receive life-long ART to encourage health and infants.23 The possible justification could be that HIV-positive women who did not receive ART follow-up have no insight about the disease since they did not attend the ART follow-up. In fact, this would lead to unsafe infant feeding practice.
HIV positive mothers who did not disclose their HIV status to others were 3 times more likely to practice unsafe infant feeding (AOR = 2.324, 95% CI: 1.470–3.673) as compared to mothers who did disclose their HIV status. This might be due to that HIV-positive woman who did not disclose their HIV status did not get essential support from the health-care professional. Thus, this would lead to unsafe infant feeding practice.
Limitations of the Study
Cause and effect relation was not assured, because the study design is cross-sectional. The other limitation was that there is a scarcity of the study that has addressed this critical topic. This made the comparison of associated factors very challenging. Therefore, hopefully, this study will be the baseline for the future researchers who need to conduct their study on this serious topic.
Conclusion
The level of unsafe infant feeding practice among HIV-positive mothers was high. Prevalence of mixed feeding is also high in the area. This showed that there is a greater chance of HIV infection, particularly in all exposed infants. Multivariable logistic regression showed that PNC follow-up, ART follow-up, and HIV disclosure statuses were significantly associated with unsafe infant feeding practice among HIV-positive mothers.
We suggest that all the concerned bodies should develop effective programs and plans to enhance safe feeding practice among mothers who were HIV positive. Comprehensive health educations need occur among HIV-positive mothers to reduce this problem. To enhance and sustain the recommended infant feeding practice among HIV-positive women, health professionals working at PMTCT are advised to provide health education and counseling in a more thorough manner. Health extension workers should persuade HIV-positive women to give birth in medical facilities so that their child can receive crucial new-born care. It is advised that all HIV-positive mothers carefully attend their ANC, ART follow-up appointments and implement any potentially safe feeding recommendations made at these appointments. Finally, we recommend the researchers to conduct the study on this topic including different predictors of unsafe infant feeding.
Data Sharing Statement
The data used to support the findings of this study are included within the article.
Ethics Approval and Consent to Participate
Ethical clearance was gained from institutional review board (IRB) of Addis Ababa University, College of Health Sciences, and School of Nursing and Midwifery. Then, the official letter of permission was sent to selected governmental hospitals that provide PMTCT in Afar Regional State. Permission was obtained from those concerned bodies. Participated mothers were informed about the objectives and significance of the study and about the confidentiality issues prior to data collection. To secure the privacy and confidentiality of the participants, personal identifiers were not used. The mothers were also informed that they have full right to withdraw from this study at any phase. There were no any samples taken from the participants which could harm them. Thus, since there were no potential risks that may cause any harm to the study participants, a verbal informed consent was obtained from all mothers prior to the commencement of this study and their parents were contacted for the participants under the age of 18 years. This was approved by IRB of Addis Ababa University, College of Health Sciences, and School of Nursing and Midwifery. During this study, all human procedures were performed as per the Declaration of Helsinki. However, no animals were considered for this study.
Acknowledgments
The authors would like to acknowledge Addis Ababa University, selected governmental hospitals, data collectors, and the study participants.
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Funding
Addis Ababa University, Ethiopia.
Disclosure
The authors declare that they have no conflicts of interest in this work.
References
1. Mengstie A, Tadese T. Assessment of factors associated with infant and young child feeding practices of human immunodeficiency virus (HIV) positive mothers in selected hospitals of Southern Nations, Nationalities, and Peoples’ Region (SNNPR) Ethiopia. J AIDS Clin Res. 2016;8(6):80–92. doi:10.5897/JAHR2015.0355
2. Kibret GD, Ferede A, Leshargie CT, Wagnew F, Ketema DB. Trends and spatial distributions of HIV prevalence in Ethiopia. Infect Dis Poverty. 2019;9:1–9.
3. Hladik W, Shabbir I, Jelaludin A, et al. HIV/AIDS in Ethiopia: where is the epidemic heading? Sex Transm Infect. 2006;82(1):1989–1992. doi:10.1136/sti.2005.016592
4. Negash S, Mesfin F, Egata G, Watanabe M, Noutoshi Y. Infants and young children feeding practice and associated factors among HIV positive mothers of children 0 – 23 months in health centers of Gulele sub ‑ city, Addis Ababa, Ethiopia. BMC Res Notes. 2019;12:1–6. doi:10.1186/s13104-018-4038-6
5. World Health Organization. Guidelines on HIV and Infant Feeding: An Updated Framework for Priority Action. World Health Organization; 2010.
6. World Health Organization. United Nations Children’s Fund. Guideline: Updates on HIV and Infant Feeding: The Duration of Breastfeeding, and Support from Health Services to Improve Feeding Practices Among Mothers Living with HIV. Geneva: World Health Organization; 2016.
7. Iftikhar S, Ghias M, Shahid S, Ali MR, Hassan MU, Numan A. Clinical and biochemical indicators of disease severity and neurological findings in COVID-19: a study of King Edward Medical University (KEMU), Pakistan. Pak J Pharm Sci. 2021;34:275–281.
8. Town J. Infant feeding practice and associated factors among HIV positive mothers in Debre Markos Referral Hospital East Gojam zone, North West Ethiopia. Pan Afr Med J. 2019;2019:1–7.
9. Points KEY. Prevention of mother-to-child transmission (PMTCT) of HIV; 2018.
10. Wakwoya EB, Zewudie TA, Gebresilasie KZ. Infant feeding practice and associated factors among HIV positive mothers in Debre Markos Referral Hospital East Gojam zone, North West Ethiopia. Pan Afr Med J. 2016;8688:1–13.
11. Andare N, Ochola S, Chege P. Determinants of infant feeding practices among mothers living with HIV attending prevention of mother to child transmission Clinic at Kiambu Level 4 Hospital, Kenya: a cross-sectional study. Nutr J. 2019;18:1–8. doi:10.1186/s12937-018-0428-9
12. Omwenga JM, Murithinjiru J. Determinants of infant feeding practices among HIV-positive mothers attending comprehensive care clinic at Ahero sub-county hospital, Kenya. Inter J Nov Res Healthcare Nurs. 2016;3:127–135.
13. United J, Programme N. HIV and Infant Feeding Guidelines for Decision-Makers. World Health Organization; 1998.
14. Yitayew YA, Bekele DM, Demissie BW, Menji ZA. Mother to child transmission of HIV and associated factors among HIV exposed infants at public health. HIV/AIDS Res Palliat Care. 2019;Volume 11:343–350. doi:10.2147/HIV.S221409
15. Afar national regional state rural land use and administration policy; 2008. 1–16. Available from: https://faolex.fao.org/docs/pdf/eth165071.pdf.
16. Towns FA, Kilologia AS. Afar region first baseline assessment for mobile HIV counseling and testing program first assessment towns: Awash Sebat Kilo; 2008.
17. Town BD, State AR. Infant feeding practice and associated factors among HIV positive mothers attending ART clinic in governmental health institutions of Bahir Dar Town, Amhara Regional State, Ethiopia, 2017. J AIDS Clin Res. 2017. doi:10.4172/2155-6113.1000755
18. UNICEF DATA. HIV Statistics - Global and Regional Trends; 2021. Available from: https://data.unicef.org/topic/hivaids/global-regional-trends/.
19. Laar SA, Govender V. Factors influencing the choices of infant feeding of HIV- positive mothers in Southern Ghana: the role of counsellors, mothers, families and socio-economic status. J AIDS HIV Res. 2011;3:129–137.
20. Paul NI, Alex-hart BA. Breastfeeding Practice among HIV positive mothers receiving care for PMTCT at the University of Port Harcourt Teaching Hospital (UPTH), Port Harcourt, Nigeria. Arch Curr Res Int. 2019;19:1–8.
21. Health G, Town M, Region T, Girma Y, Aregay A, Biruh G. Infant feeding practice and associated factors among HIV positive mothers infant feeding practice and associated factors among HIV positive mothers enrolled in Governmental health facilities in Mekelle town, Tigray Region, North Ethiopia. Pan Afr Med J. 2016. doi:10.17303/jaid.2014.401
22. Demissie DB. Infant feeding practice and associated factors of HIV positive mothers attending prevention of mother to child transmission and antiretroviral therapy clinics in shashemene referral hospital.2016.
23. World Health Organization. HIV/AIDS: infant feeding and nutrition; 2021. Available from: https://www.who.int/news-room/questions-and-answers/item/hiv-aids-infant-feeding-and-nutrition.
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.