Back to Journals » Adolescent Health, Medicine and Therapeutics » Volume 14
Timing and Quality of Antenatal Care Among Adolescent Mothers in a Rural Community, Uganda
Authors Kayemba V , Kabagenyi A , Ndugga P, Wasswa R , Waiswa P
Received 11 May 2022
Accepted for publication 1 February 2023
Published 11 February 2023 Volume 2023:14 Pages 45—61
DOI https://doi.org/10.2147/AHMT.S374296
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Professor Alastair Sutcliffe
Vincent Kayemba,1 Allen Kabagenyi,1 Patricia Ndugga,1 Ronald Wasswa,2 Peter Waiswa3
1Department of Population Studies, Makerere University, Kampala, Uganda; 2Department of Statistical Methods and Actuarial Science, Makerere University, Kampala, Uganda; 3School of Public Health, Makerere University, Kampala, Uganda
Correspondence: Vincent Kayemba, Email [email protected]
Background: Most adolescent mothers attend their first antenatal care (ANC) visit later than the recommended time while others do not receive good quality antenatal care (all the required components of ANC such as iron tablets). This study sought to examine the factors associated with timing of the first ANC visit and quality of ANC among adolescent mothers in Uganda.
Methods: This study was based on quantitative data from 248 adolescent mothers aged 10– 19 years in Luuka district, Eastern Uganda. We selected adolescent mothers who were either pregnant or had infants aged 0– 3 months. We used logistic regression to identify factors associated with timing and receipt of good quality ANC.
Results: The majority of the adolescents (82%) attended ANC for their most recent pregnancy. Of these, 47% made the first visit in the first trimester while 36% received good quality ANC. Having knowledge of danger signs in pregnancy was a determinant of both timing of first ANC visit (aOR = 2.89, 95% CI: 1.04– 8.06) and receipt of good quality ANC (aOR = 6.57, 95% CI: 1.75– 24.65). Other determinants for timing of first ANC visit were mother’s age, partner’s age, having ever given birth, decision maker on health care and daily earnings. Other determinants for quality of ANC included distance to health facility and knowledge of family planning methods.
Conclusion: This study recommends expanding the network of public health facilities further into the rural communities in the district as a means of bringing health services closer to adolescent mothers, deliberate efforts to equip adolescent girls with reproductive health information on pregnancy danger signs, and family planning and empowering adolescent girls to start income-generating activities.
Keywords: antenatal care, ANC timing, ANC quality, Luuka district, adolescent mothers, Uganda
Background
Adolescent pregnancy is a serious public health issue because of its association with adverse negative consequences to both the mother and child. Globally, 42 births occur among every 1000 teenage girls, with this problem mainly witnessed in Sub-Saharan Africa.1 According to the 2016 Uganda Demographic and Health Survey (UDHS), 25% of adolescent girls have either given birth or are pregnant.2 The impact can be associated with higher risk of maternal deaths3 as well as fetal and neonatal mortality of the newborn babies.4 In addition, the incidence of low birth weight and preterm delivery has also shown to be highest among babies born to adolescent mothers.3 However, all these maternal related health problems can easily be detected and minimized through timely access to quality antenatal care (ANC).5,6
Several studies have shown that quality ANC contributes to desired motherhood outcomes such as increased skilled birth attendance; reduction in maternal, neonatal and perinatal morbidity and mortality.7–9 Relatedly, the timing of the first ANC visit is also critical in achievement of the above stated outcomes. The World Health Organization (WHO) recommends a minimum of eight ANC contacts of which the first should be made in the first trimester of pregnancy.9 Timely initiation of ANC contacts offers mothers the opportunity of early detection of Human Immunodeficiency Virus (HIV) and Sexually Transmitted Diseases (STDs), malaria and anaemia prophylaxis, health education and treatment or prevention of complications.5 Despite the benefits of antenatal care, most adolescent mothers are less likely to use ANC services compared with older women.10 Moreover, they are more likely to seek ANC later.3 It has been documented that low utilization of ANC by adolescents is attributed to unplanned pregnancies, and limited financial and social support.10,11 Also, the reproductive health services which are unprepared to handle adolescents, and the long distances to health facilities have been barriers in seeking ANC services.10,11 Quality ANC necessitates that during health facility ANC visits, pregnant mothers should receive a core set of services recommended by the WHO12 – defined here as components of care. These include blood pressure and weight measurement, fetal growth monitoring, urine testing, iron-folic acid supplementation, tetanus vaccination, at least three doses of Intermittent Preventive Treatment with Sulfadoxine-Pyrimethamine (IPTp-SP), deworming after the first trimester, blood group typing if never done, HIV and syphilis testing.9,13
Luuka district contributes a significant proportion to the burden of teenage pregnancy in Uganda, with teenage child-bearing rates high at 11.2% and 18.1% among girls aged 12–17 years and 12–19 years, respectively.14 However, findings from Busoga region where the district is located indicate low ANC utilization rates among adolescent mothers. For instance, up to 57% of adolescent mothers who attended ANC for their most recent live birth made the first ANC visit in the second trimester.2 Additionally, components including urine sample testing, deworming tablets, blood pressure measurement, and Fansidar were the least received (26%, 46%, 52%, and 54% of mothers, respectively).2 This is an indicator of compromised quality of ANC among a significant proportion of mothers.
Studies conducted on timing of ANC utilization show that family size, financial constraints,15 long distance to health facility,15,16 occupation,16 education level,16,17 and religion17 are associated with timing of the first ANC visit. In addition, a study conducted in Tanzania also found out that earlier ANC attendance was associated with gravida of pregnancy and history of pregnancy-related problems.18 Primiparous women and those who had ever experienced a miscarriage or still birth were more likely to initiate the first ANC visit early.18 In relation to receipt of the components of care, earlier studies in Uganda show that age of woman, ANC location, ANC provider cadre, number of ANC visits attended, and maternal education were associated with receipt of the ANC components of care.8,19 Other factors identified included access to media, history of pregnancy-related problems, household economic status, timing of the first ANC visit and family planning.8,19 A study conducted among adolescent women in India20 found that those working were more likely to have their weight monitored, those with power to make decisions regarding major household purchases were more likely to receive tetanus injections and deworming tablets and those of higher education levels were more likely to receive calcium tablets. However, those with family planning knowledge were less likely to have their weight monitored.20
In Uganda, many studies on ANC utilization have been conducted.5,6,8,16,19,21–24 Of these, only studies by Ssetaala et al,8 Bbaale,19 Kisuule et al,5 and Kawungezi et al16 investigated ANC utilization with respect to quality of care received during ANC visits and timing of the first ANC visit . However, these focused on women of the entire reproductive age group (15–49 years). Regarding ANC utilization among adolescent mothers, few studies have been conducted in Uganda.11,25 Rukundo et al assessed stakeholders’ views concerning factors affecting availability, accessibility and utilization of teenager friendly ANC services in Mbarara Municipality, Western Uganda.11 Nansubuga on the other hand investigated factors associated with ANC utilization (frequency of ANC attendance, duration of attendance, ANC provider and services received during ANC visit).25 However, these studies had limitations including, firstly, adolescents’ views concerning utilization of ANC services were not put into consideration.11 Secondly, bivariate analysis technique was applied.25 This approach does not put into consideration other possible confounders. Therefore, there is still scarcity of information on factors associated with ANC utilization among adolescent mothers in Uganda. To address this gap, this study set out to (i) examine the timing to first ANC visit, (ii) examine the quality of care received during ANC visits, and (iii) establish the predictors of timing to first ANC visit and receipt of quality care among adolescent mothers in Luuka district.
Data and Methods
Study Setting
Luuka is located in the Eastern region of Uganda. The district has eight sub-counties and is bordered by Kaliro (North East), Buyende (North), Kamuli (North West), Jinja (South West), Mayuge (South) and Iganga (South East) districts.26 Luuka has a population of 238,020 people of which 28.3% are adolescents.14 The district has 38 health facilities, of which 28 are government and 10 are private facilities, at the level of clinic and health centre two, three and four.26
Study Population
The study population were adolescent mothers aged between 10 and 19 years who were either pregnant or had infants aged 0–3 months.
Study Design and Sampling
The study adopted a cross-sectional quantitative research design. The study employed a two-stage sampling design. In the first stage, we selected three sub-counties with the highest number of teenage mothers attending ANC. These included Bukanga, Ikumbya, and Waibhuga. We intended to have a rural-urban representation since 75% of Uganda’s population live in rural areas while 25% live in urban.27 Therefore, we also purposely selected Luuka town council to represent urban as the rest of the sub-counties represented rural. The second stage of sampling involved selection of three parishes (see Table S1), from each sub-county, with the highest number of teenage mothers who attended ANC. The sampling frame used to select the sub-counties and parishes was based on the most recent data about ANC attendance and was obtained from the only health centre IV in the district – Kiyunga Health Centre IV. Data on ANC attendance, disaggregated by village, were not available. Consequently, we could not select, from each parish, villages with the highest number of teenage mothers who attended ANC. The final respondent was reached with the help of village health team members. If a household had more than one eligible adolescent mother, only one was interviewed.
In this study, the Kish formula was used to estimate the sample size from:
Where: n = Sample size, Z (α/2) = confidence interval (95%), d = margin of error assumed at 5.0%. P = proportion of adolescent girls (12–19 years) in Luuka district who have given birth. This stands at (18.1%).14 In order to cater for the non-response and missing values, the sample size was oversampled by 10% with a design effect of 2.0. The final sample size for the study was 248 adolescent mothers. To determine how many adolescent mothers to collect data from in each parish of a selected sub-county, the Probability Proportional to Size (PPS) approach was used to distribute the minimum sample size across the selected sub-counties and respective selected parishes.
Data Collection
Data collection took place between March and May 2021. A pretested structured questionnaire was used to collect information on socio-demographic characteristics (for both adolescent mother and partner), sexual activity, and reproduction, prenatal and postnatal care. The questionnaire also collected information on knowledge and awareness about pre/postnatal, newborn care practices and danger signs in pregnancy. Additionally, only adolescent mothers who consented (those 18–19 years) or had their parents/ guardians assent to their participation (those 10–17 years) in the study were recruited into the study. The questionnaires were administered to the adolescent mothers through face-to-face interviews by a team of well-trained research assistants. The research assistants comprised those proficient in the use of Lusoga (the major local language spoken in the district). The data were captured electronically on a tablet using Open Data Kit (ODK) software.
Variables
For this study, two outcome variables were considered. We had quality of ANC and timing of the first ANC visit. The first outcome variable points to receipt of the WHO recommended core set of services12 that pregnant women are expected to receive when they visit a health facility for antenatal care. Of all the WHO recommended core set of services, this study focused on only the eight commonly provided core services in Uganda, as per the Ugandan clinical guidelines.13 In this study, adolescent mothers were asked whether, during pregnancy, they received any of the eight components, including blood pressure measurement, urine sample testing, blood sample testing, weight measurement, tetanus toxoid vaccination, iron tablet supplementation, drugs for intestinal worms and SP/Fansidar drugs for malaria prevention. The variable was coded into a binary variable based on the number of ANC components received by an adolescent mother during ANC visits for their most recent birth or pregnancy. Adolescent mothers who received less than eight components comprised the category “Low quality ANC received” and were coded 0 while those who received all the eight components comprised the category “Good quality ANC received” and were coded 1.
The second outcome variable points to the gestational age (in months) of current pregnancy or pregnancy for the most recent birth at which first ANC visit was made by the adolescent mother. This variable was coded into a binary variable based on adolescent mothers’ responses to the question - how many months pregnant were you when you first received antenatal care for this pregnancy? Adolescent mothers whose first ANC visit was in the first trimester (0–3 months of pregnancy) comprised the category “In the first trimester” and were coded 1. Those whose first ANC visit was after the first trimester (from 4 months of pregnancy) comprised the category “After the first trimester” and were coded 0. The categorization of the outcome variables only included mothers who reported having attended ANC.
The explanatory variables were mother’s age (below 18 or 18–19), partner’s age (same age or older), ever given birth (yes or no), number of children ever born (0–1 or more than 1), mother’s highest education level (primary or secondary), marital status (unmarried or married/cohabiting), partner presence (staying with partner or not staying with partner), distance to nearest health facility (less than 1 km or 1 km or more) and religion (Christian or Moslem; where Christian includes Catholics, Protestants, Pentecostals and Seventh Day Adventists). Other variables analyzed included social support (received no support or received support; where receipt of social support was defined as being accompanied to the health facility for ANC visits by either friends or family members), decisions on health-care seeking (self, husband/partner, relatives/in-laws or jointly with husband/partner), pregnancy wanted (wanted or not wanted), adolescent mother’s working status (working or not working), daily earnings (earn nothing or earn some money), knowledge of obstetric pregnancy danger signs (has knowledge or no knowledge), knowledge of family planning methods (has knowledge or no knowledge), ANC provider cadre (skilled or unskilled) and type of health facility (government, private or own home/TBA’s home).
Data Analysis
Data analyses were done at univariate, bivariate and multivariate levels.
At the univariate level, frequencies and percentage distributions describing the sample of adolescent mothers with respect to the study variables were generated.
At the bivariate level, the association between the explanatory variables and outcome variables was examined. The statistical significance of the association was tested by using the Pearson chi-square (χ2) and Fisher’s exact tests of independence.
At multivariate level, binary logistic regression models were fitted to determine the overall predictors of the study outcomes. Selection of variables for inclusion in the multivariable analysis was based on the results obtained at the bivariate level of analysis. Variables which showed association with the outcome variables at the bivariate level were adopted. However, variables including mother’s age, mother’s education level, distance to nearest health facility, social support, decision maker on seeking health care, pregnancy wanted (intendedness of pregnancy), and type of health facility were also included in the regression analysis model even though they were not significant at bivariate level. This is because of their documented importance, in literature, in influencing ANC utilization. We assessed model adequacy using the link test. An adequately specified model was based on a significant _hat variable and a non-significant _hatsq variable. Multicollinearity between the predictor variables was checked by using the Variance Inflation Factors (VIF). The VIF gives an indication of how much of the inflation of the standard error is caused by Multicollinearity. A very large VIF (10 or greater) for any given variable shows that the variable is closely related to one or more variables.28 Therefore, predictor variables with a VIF of 10 or greater (see Supplementary Material) were excluded from the model. The level of statistical significance was set at p<0.05 and p-values were used to report associations.
Results
Distribution of the Adolescent Mothers
Table 1 shows the distribution of adolescent mothers. More than half of the adolescent mothers were older adolescents aged 18–19 years (56%). Further, almost half (49%) had ever given birth, with 9 in 10 (86%) having at least one child. Those pregnant at the time of the study constituted 51%. Slightly more than half of the mothers (51%) had mistimed pregnancies. That is, they did not want to get pregnant at the time they conceived their current pregnancy or the pregnancy for their most recent birth.
 |
Table 1 Distribution of Adolescent Mothers by Study Variables |
All adolescent mothers in this study had attained a certain level of education. The results show that close to three-quarters of the mothers (72%) had attained primary level while 6 in 10 (60%) were either married or in a union as if married (cohabiting). With regard to religion, nearly three-quarters (72%) of the adolescent mothers were Christians. Most of the adolescent mothers reported having received no social support during their most recent pregnancy or birth (65%). More than two-thirds (68%) of the adolescent mothers were not working and the majority (80%) reported that they earned no daily income.
Notably, most adolescent mothers in this study stayed quite far away from the nearest health facility. Almost 4 out of 5 (72%) adolescent mothers were staying at least 1 km away from the nearest health facility. Results in Table 1 also show that more than two-fifths (46%) of the adolescent mothers made their own decisions on seeking health care. Adolescent mothers who were knowledgeable about pregnancy danger signs and family planning methods constituted the majority (83% and 91%, respectively). Eleven percent of the adolescent mothers were married to adolescent boys and most were currently living with their partners or father of the child (61%).
Utilization of ANC
Table 2 presents results on utilization of ANC (that is, ANC attendance, ANC provider, ANC providing facility, number of ANC visits and quality of ANC received) by the adolescent mothers. The results show that more than half (53%) of adolescent mothers who went for ANC made their first visit after the first trimester, with the median gestation time of four months. Overall, the majority (82%) of the adolescent mothers had attended ANC for their most recent pregnancy or birth. However, more than half (53%) did not complete the recommended minimum of four visits, with 13% attending ANC once, 16% attending twice and 24% attending thrice. Only 22% of adolescent mothers who attended ANC completed the recommended minimum number of four visits while slightly more than a quarter (26%) made more than the recommended four ANC visits. The results in Table 2 further indicate that almost all adolescent mothers who attended ANC during their last pregnancy or birth received ANC from a government facility (91%) and from a skilled provider (98%).
 |
Table 2 Distribution of Adolescent Mothers by ANC Attendance, Provider, Providing Facility, Number of ANC Visits and Components of Care Received |
Quality of ANC Received
The majority of the adolescent mothers had their blood sample drawn (96%), weight measured (86%), received a tetanus injection (88%) and received or were able to buy themselves iron tablets/syrup (87%). More than three-quarters (78%) of the adolescent mothers had their blood pressure measured while 7 out of 10 mothers (70%) had their urine samples taken (Table 2). Nearly three-quarters (74%) of the adolescent mothers took antimalarial drugs during their current pregnancy or the pregnancy for their most recent birth and close to two-thirds (65%) took drugs for intestinal worms (Table 2).
Figures 1 and 2 present the percentage distribution of adolescent mothers who attended ANC by the number of ANC components of care received during those visits. The results, which in this study inform the quality of ANC received by the adolescent mothers were based on a nine-item index ranging between zero and eight. The index was adapted from a study by Bbaale.19 Items including whether the mother had her blood pressure and weight measured, urine and blood samples taken, received a tetanus injection, received iron tablets, took drugs for intestinal worms and SP/Fansidar drugs comprise the index. On the index, zero indicates all adolescent mothers who received none of the components during their ANC visit (None) while eight indicates adolescent mothers who received all the components (All). For the recommended components of the package of care considered in this study, the results in Figure 1 show that almost all (97%) adolescent mothers who attended ANC received at least one of the components during ANC visits for their current pregnancy or most recent birth. However, receipt of all the recommended components of care was low with slightly more than one-third (36%) of the adolescent mothers who attended ANC reporting receipt of all. Therefore, only 36% of adolescent mothers in this study received good quality ANC. Even among adolescent mothers who made their first ANC visit in the first trimester (Figure 1), a similar proportion reported receipt of all components. Important to note is that there was a small proportion of adolescent mothers (3%) who attended ANC and yet did not receive any of the recommended components of care. On average, adolescent mothers who attended ANC received five components out of the recommended eight components.
 |
Figure 1 Percentage of all adolescent mothers who attended ANC by number of components of care received during ANC visits. |
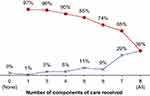 |
Figure 2 Percentage of adolescent mothers who made the first ANC visit in the first trimester by number of components of care received during ANC visits. |
Factors Associated with Quality of ANC and Timing of the First ANC Visit
Table 3 presents results on the association between the independent variables and the outcome variables. The results indicate that having ever given birth (p<0.05) and having knowledge about pregnancy danger signs (p<0.05) were the only factors significantly associated with quality of ANC. A significantly higher proportion (60%) of mothers who received good quality ANC were mothers who had ever given birth. Similarly, the majority (93%) of adolescent mothers who received good quality ANC during their ANC visit were mothers who knew about obstetric pregnancy danger signs.
 |
Table 3 Factors Associated with Quality of ANC and Timing of the First ANC Visit |
However, partner’s age, ever given birth, marital status, partner presence, working status, daily earnings and knowledge about obstetric pregnancy danger signs were the only factors significantly associated with timing of the first ANC visit (Table 3). Almost all mothers (97%) who made the first ANC visit in the first trimester were younger than their partners in terms of age. The majority of the mothers who made the first ANC visit in the first trimester were those who had never given birth while three-fifths (60%) of mothers who made the first ANC visit after the first trimester were those who had ever given birth to a child. More than two-thirds of mothers (67%) who made the first ANC visit in the first trimester were married or cohabiting. Similarly, this group of mothers constituted the majority (53%) among those who made the first visit after the first trimester. Mothers staying with their partners constituted the majority of those who made the first ANC visit in the first trimester as well as after the first trimester. About seven in 10 mothers (71%) who made the first visit in the first trimester and more than half (52%) of those whose first visit was after the first trimester were mothers staying with their partners or father of the child. More than three-quarters (78%) of mothers who made the first ANC visit after the first trimester were not working and were not earning any money (91%). Out of every 10 adolescent mothers who made their first visit in the first trimester, nine were knowledgeable about or aware of the obstetric pregnancy danger signs.
Determinants of Timing of First ANC Visit and Quality of ANC
Multivariate analysis results from binary logistic regression, on factors associated with an adolescent mother’s good quality ANC and timing of the first ANC visit, are presented in Table 4 and Table 5, respectively. From the bivariate analysis, partner’s age, ever given birth, partner presence, daily earnings and knowledge of obstetric pregnancy danger signs were significantly associated with the outcome variables (timing of first ANC visit and quality of ANC). Similarly, marital status and working status were significantly associated with the outcome at bivariate analysis level. However, these were excluded from the regression model due to multicollinearity. Variables including mother’s age, mother’s education level, distance to nearest health facility, social support, decision maker on seeking health care, pregnancy wanted (intendedness of pregnancy), and type of health facility were included in the regression analysis even though they were not significant at bivariate level. This is because of their documented importance, in influencing timing and quality of ANC, in previous literature.
 |
Table 4 Logistic Regression Analysis Results of Determinants of Receipt of Good Quality ANC |
 |
Table 5 Logistic Regression Analysis Results of Determinants of Timing of the First ANC Visit |
Determinants of Receipt of Good Quality ANC
As shown in Table 4, distance to nearest health facility, knowledge of obstetric pregnancy danger signs and knowledge of family planning methods were the only statistically significant factors associated with receipt of good quality ANC. The odds of receiving good quality ANC were lower for mothers staying at least 1 km away from the nearest health facility (aOR = 0.424, 95% CI: 0.189, 0.952) compared with those staying less than 1 km away. Similarly, mothers who had knowledge of family planning methods had lower odds of receiving good quality ANC (aOR = 0.262, 95% CI: 0.070, 0.982) compared with those who had no such knowledge. Mothers who were knowledgeable about obstetric pregnancy danger signs were found to be 6.6 times more likely to receive good quality ANC (aOR = 6.567, 95% CI: 1.750, 24.648) compared with those who were not knowledgeable about these signs.
Determinants of Timing of the First ANC Visit
Results presented in Table 5 show that adolescent mother’s age, partner’s age, ever given birth, decision maker on seeking health care, daily earnings and knowledge of obstetric pregnancy danger signs were the only factors statistically significantly associated with timing of the first ANC visit. The odds of making the first ANC visit in the first trimester were highest for older adolescent mothers (aOR = 2.125, 95% CI: 1.01, 4.46), adolescent mothers younger than their partners (aOR = 4.337, 95% CI: 1.06, 17.71), those who earn a daily income (aOR = 3.930, 95% CI: 1.53, 10.09), and those with knowledge of obstetric pregnancy danger signs (aOR = 2.888, 95% CI: 1.04, 8.06). Older adolescent mothers (18–19 years) were twice as likely to make the first ANC visit in the first trimester compared with the younger ones (14–17 years). Adolescent mothers younger than their partners and those who reported earning a daily income were four times more likely to make the first ANC visit in the first trimester compared with those whose age was the same as their partner’s and earned no daily income. Unlike adolescent mothers without knowledge of obstetric pregnancy danger signs, those with such knowledge were three times more likely to make the first ANC visit in the first trimester. The odds of making the first ANC visit in the first trimester were lowest for adolescent mothers who had ever given birth (aOR = 0.273, 95% CI: 0.12, 0.6) compared with those who had never given birth. Similarly, adolescent mothers whose decisions on seeking health care were made by relatives or in-laws were less likely to make their first ANC visit in the first trimester (aOR = 0.290, 95% CI: 0.09, 0.96) compared with those whose decisions on seeking health care were made by themselves.
Discussion
This study sought to examine timing of the first ANC visit, quality of ANC and associated predictors among adolescent mothers in Luuka district. Understanding these aspects of ANC utilization particularly among this special group of mothers is pertinent to the efforts of the district health office and other stakeholders involved in designing interventions to improve utilization of maternal health services.
Our findings revealed that most adolescent mothers delayed initiating the first ANC visit. That is, most adolescent mothers made their first ANC visit after the first trimester. This finding is similar to what was observed in Nigeria, where most adolescent mothers started ANC in the fourth month or later.17 Understanding why adolescent mothers delay their first ANC visit was beyond the scope of this study. However, previous studies have attributed the delay to fear of pregnancy disclosure, long distance to health facility, lack of knowledge of pregnancy and ANC, travel costs to health facility and preference for traditional care to ANC.29,30 Furthermore, we found that among adolescent mothers whose first ANC visit was in the first trimester, only a small proportion received all the recommended components of care. This contrasts with the Ugandan clinical guidelines which indicate that mothers should receive all eight components of care in the first trimester.13 Additionally, it casts doubt on the quality of ANC received. These findings point to the need for interventions to improve initiation of the first visit as well as uptake of the components of care among adolescent mothers.
This study also revealed that knowledge about obstetric pregnancy danger signs is a determinant of both receipt of good quality ANC and timing of the first ANC visit among adolescent mothers. These findings show that knowledge of health information is an important factor in utilization of health-care services as posited by Ali et al in their literature review on factors affecting utilization of antenatal care among pregnant women.31 Considering that more than three-quarters (78%) of the adolescent mothers in this study who made their own decisions on health-care seeking were those knowledgeable about pregnancy danger signs, it is plausible to assert that knowledge of pregnancy danger signs empowers adolescent mothers to confidently make their own decisions on health-care seeking. For that reason, they are able to make timely ANC visits. It is also likely that they are able to consistently attend ANC throughout pregnancy, resulting in receipt of all the recommended components of care, which in our study is considered good quality care. This underscores the importance of equipping adolescent girls in the district with reproductive health information.
This study found that other determinants of receipt of good quality care among adolescent mothers in the district were distance to nearest health facility and knowledge about family planning methods. According to the 2014 Uganda National Housing and Population census, 22.1% of households in Luuka district are located 5 km or more away from the nearest public health facility.14 Furthermore, 13.2% of households in the same district are 5 km or more away from the nearest health facility, irrespective of whether it is public or private.14 Such long distances away from the nearest health facility have been shown to hinder utilization of maternal health-care services.8,32 It is therefore not surprising that in this study, adolescent mothers staying at least 1 km away from the nearest health facility were less likely to receive good quality ANC. Putting into consideration that the majority of the adolescent mothers receive ANC from a public health facility (Table 2), there is an urgent need to expand the network of public health facilities further into the rural communities as a means of bringing health services including ANC closer to adolescent mothers.
Adolescent mothers with knowledge about family planning methods were less likely to receive good quality ANC than those who had no knowledge about these methods. These findings are similar to those from a study in India.20 They however contrast with Habibov and Zainiddinov33 whose findings implied that women who appreciated knowledge of family planning as a health-care service were also more likely to appreciate ANC services. There is need to integrate family planning service provision with ANC. This creates a perfect opportunity to advise women on the importance of ANC and could, in the long term, contribute to increased receipt of good quality ANC among adolescent mothers by them receiving all the recommended components of care.
With regard to timing of first ANC visit, adolescent mother’s age, partner’s age, having ever given birth, adolescent mother’s decision maker on health-care seeking, and daily income earnings were found to determine the likelihood of an adolescent mother in Luuka district to make the first ANC in the first trimester. Results from this study show that older adolescent mothers (18–19 years) were more likely to make their first ANC visit in the first trimester. As may be expected, the majority (94%) of the adolescent mothers, in this study, who had ever given birth to more than one child were older adolescent mothers (see supplementary material). Therefore, early initiation of ANC among older adolescent mothers compared with their younger counterparts could be attributed to better knowledge, garnered from previous ANC sessions attended, about the benefits and necessity of initiating ANC in the first trimester.
In this study, adolescent mothers who were younger than their partner were more likely to make the first ANC visit in the first trimester. Partners who are of the same age as adolescent mothers are assumed to be school going. As such, they might not have the capacity to care for girls they have impregnated. Therefore, we attribute the finding indicating early enrollment for ANC by adolescent mothers younger than their partners to willingness and ability of older husbands/partners to support their female partners by, for instance, accompanying them to the health facility and providing money for costs associated with ANC such as transport. There is evidence that such support from husbands/partners contributes to early enrollment for ANC.18
The likelihood of having the first ANC visit in the first trimester was lowest among adolescent mothers whose decisions on health-care seeking were made by relatives or in-laws rather than themselves. This finding is consistent with findings from a study in Kenya34 which revealed that adolescent mothers in Kenya whose decision to attend an ANC clinic was made by others were less likely to book their first ANC visit in the first trimester compared with those whose decision was made by themselves. The reason for this finding could be an adolescent’s high dependence which makes them compliant to the relatives’ or in-laws’ recommendations on health-care matters, including when to start attending the ANC clinic.
Compared with adolescent mothers who had no daily income earnings, the likelihood of making the first ANC visit in the first trimester was highest for adolescent mothers who earned some income on a daily basis. A possible explanation for this finding is that, without income, early initiation of ANC is inhibited as it renders the adolescent mother unable to meet costs associated with seeking ANC35–37 such as transport fees and buying some essential medicines, in the event that they are unavailable at the public health facility where majority of the adolescent mothers in this study sought ANC.
This study also found that adolescent mothers who had ever given birth were less likely to attend their first ANC visit in the first trimester compared with those who were yet to give birth. These findings agree with Gross et al whose study on timing of antenatal care for adolescent and adult pregnant women in south-eastern Tanzania revealed that being in the first pregnancy was strongly associated with three weeks earlier attendance of ANC.18 Having known the importance of ANC attendance to a pregnant woman, following ANC attendance during previous pregnancy, it would be expected of adolescent mothers who have ever given birth to initiate ANC attendance in the first trimester. However, findings from this study are contrary to this expectation. Notwithstanding other factors that could have prevented adolescent mothers who had ever given birth from attending ANC in the first trimester, this study presumes that delayed initiation of ANC among these mothers could be attributed to the fact that the pregnancies were unintended. The other reason could be self-confidence because there is evidence from Rwanda that a greater confidence and gained experience from earlier pregnancies could contribute to poor ANC utilization outcomes.38 This highlights the need to sensitize adolescent mothers about the necessity of initiating the first ANC visit early, irrespective of the circumstances surrounding pregnancy conception or birth history.
Limitations of the Study
First, information on ANC in this study was collected retrospectively, implying that mothers were required to recall events on ANC utilization for the most recent pregnancy carried. This study minimized the recall bias and therefore increased the accuracy of findings since information on ANC was collected from adolescent mothers who were currently pregnant or had just given birth three months ago.
Second, the study considered a small sample size and the fact that findings were only from one district. For this reason, the results may not be generalizable to similar population groups within the Eastern region. Additionally, being a cross-sectional study, causality cannot be determined. However, appropriate methodological approaches were used and thus the study findings are reliable and can inform ANC service improvement among adolescent mothers in the district.
Conclusion
This study has established that non/low-adherence to the recommended timing of first ANC contact and quality of care persists among adolescent mothers in Luuka. The implication of this is that those who fall victim are at a heightened risk of associated pregnancy complications. This calls for urgent interventions to counteract the inhibiting factors, most of which are socio-economic in nature, as highlighted in the study findings. Therefore, there is need to expand the network of public health facilities further into the rural communities in the district as a means of bringing health services closer to adolescent mothers. To achieve this, more facilities need to be constructed. We envisage that this will significantly improve the quality of ANC through increased uptake of all recommended ANC components of care. It could also improve timing and number of ANC contacts made by adolescent mothers.
Additionally, there should be deliberate efforts to equip adolescent girls with reproductive health information. A case in point, as established by this study, is information on pregnancy danger signs and family planning. This can be achieved with the integration of health-care services. For example, integrating family planning and ANC service provision avails an opportunity for passing on information on ANC as mothers are being counseled on family planning matters. This study reiterates the importance of income to health service uptake. As a way of supporting adolescent girls to earn an income, we recommend strengthening the operationalization of programs like youth livelihood program and other similar ones aimed at financially supporting youth to establish income generating activities.
Abbreviations
AMNEP, Adolescent Motherhood, Vulnerability Assessment, Maternal and Newborn Care Practices in Eastern Uganda; ANC, Antenatal Care; HIV, Human Immunodeficiency Virus; ICT, Information, Communication and Technology; STDs, Sexually Transmitted Diseases; TBA, Traditional Birth Attendant; UDHS, Uganda Demographic and Health Survey; UNCST, Uganda National Council of Science and Technology; WHO, World Health Organization.
Data Sharing Statement
The dataset used and analyzed during the current study is available from AK on reasonable request.
Ethics Approval and Consent to Participate
This study is part of a larger research project titled Adolescent Motherhood, Vulnerability Assessment, Maternal and Newborn Care Practices in Eastern Uganda (AMNEP). AMNEP study and its method of obtaining participants’ consent was approved by the Uganda National Council of Science and Technology (UNCST) under registration number HS1248ES and Mildmay Uganda Research Ethics Committee (MU-REC) under registration number 0811-2020. AMNEP study also received district clearance from the district health officer (DHO) and the chief administrative officer (CAO) of Luuka district. Prior to enrollment into the study, written informed consent was obtained from all adolescent mothers aged 18 and 19 years. Adolescent mothers aged between 10 and 17 years were enrolled into the study after providing a written informed emancipated minor consent if they were emancipated minors. Otherwise, a written informed assent together with a written informed consent from their respective parents or guardians were obtained prior to participation in the study.
Acknowledgments
The authors of this study are grateful to Makerere University and Carnegie Corporation of New York which provided financial support to this study, through the Makerere Carnegie – Supporting Early Career Academics (SECA) program. The authors are grateful to the Principal Investigator of the AMNEP project - Dr. Allen Kabagenyi for availing data for the analyses. We also express gratitude to the adolescent mothers who took part in the study, the Luuka district leadership, and the village health teams who acted as guides during data collection.
Author Contributions
All authors made a significant contribution to the work reported, they took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Funding
The study was funded by Makerere University and Carnegie Corporation of New York, USA through the Supporting Early Career Academics (SECA) program.
Disclosure
The authors declare that they have no competing interests.
References
1. UNICEF. Adolescent health regional profiles; 2021. Available from: https://data.unicef.org/resources/adolescent-health-dashboard-regional-profiles/.
2. Uganda Bureau of Statistics and ICF. Uganda Demographic and Health Survey, 2016. Kampala, Uganda and Rockville, Maryland, USA: Uganda Bureau of Statistics and ICF; 2018.
3. World Health Organization. Pregnant Adolescents. Geneva, Switzerland: World Health Organization; 2006.
4. Kumar A, Singh T, Basu S, Pandey S, Bhargava V. Outcome of teenage pregnancy. Indian J Pediatr. 2007;74(10):927–931. doi:10.1007/s12098-007-0171-2
5. Kisuule I, Kaye DK, Najjuka F, et al. Timing and reasons for coming late for the first antenatal care visit by pregnant women at Mulago hospital, Kampala Uganda. BMC Pregnancy Childbirth. 2013;13:1–7. doi:10.1186/1471-2393-13-121
6. Tetui M, Ekirapa EK, Bua J, Mutebi A, Tweheyo R, Waiswa P. Quality of antenatal care services in eastern Uganda: implications for interventions. Pan Afr Med J. 2012;13:1–15. doi:10.11604/pamj.2012.13.27.1427
7. Oliobi WC, Nwafor JI, Ikeotuonye AC, et al. Pattern of antenatal care among antenatal clinic attendees at Alex Ekwueme Federal University Teaching Hospital Abakaliki, Nigeria. Int J Res Med Sci. 2019;7(11):4096. doi:10.18203/2320-6012.ijrms20194973
8. Ssetaala A, Nabawanuka J, Matovu G, et al. Components of antenatal care received by women in fishing communities on Lake Victoria, Uganda; A cross sectional survey. BMC Health Serv Res. 2020;20(1):1–9. doi:10.1186/s12913-020-05739-9
9. World Health Organization. WHO recommendations on antenatal care for a positive pregnancy experience. Geneva, Switzerland: World Health Organization; 2016. Available from: http://www.who.int.
10. Worku EB, Woldesenbet SA. Factors that influence teenage antenatal care utilization in John Taolo Gaetsewe (JTG) District of Northern Cape Province, South Africa: underscoring the Need for Tackling Social Determinants of Health. Int J Matern Child Heal AIDS. 2016;5(2):134–145. doi:10.21106/ijma.157
11. Rukundo GZ, Abaasa C, Natukunda PB, Ashabahebwa BH, Allain D. Antenatal services for pregnant teenagers in Mbarara Municipality, Southwestern Uganda: health workers and community leaders’ views. BMC Pregnancy Childbirth. 2015;15(1):1–5. doi:10.1186/s12884-015-0772-0
12. Islam MM, Masud MS. Determinants of frequency and contents of antenatal care visits in Bangladesh: assessing the extent of compliance with the WHO recommendations. PLoS One. 2018;13(9):1–22. doi:10.1371/journal.pone.0204752
13. Ministry of Health Uganda. Uganda clinical guidelines 2016: national guidelines for management of common conditions. Minist Heal Uganda. 2016;2016:1–1142.
14. Uganda Bureau of Statistics. The National Population and Housing Census 2014 - Area Specific Profile Series. Kampala, Uganda: Uganda Bureau of Statistics; 2017.
15. Tolefac PN, Halle-Ekane GE, Agbor VN, Sama CB, Ngwasiri C, Tebeu PM. Why do pregnant women present late for their first antenatal care consultation in Cameroon? Matern Heal Neonatol Perinatol. 2017;3(1):1–6. doi:10.1186/s40748-017-0067-8
16. Kawungezi PC, Akiibua D, Aleni C, et al. Attendance and utilization of antenatal care (ANC) services: multi-center study in upcountry areas of Uganda. Open J Prev Med. 2015;5(3):132–142. doi:10.4236/ojpm.2015.53016.Attendance
17. Alex-Ojei CA, Odimegwu CO. Correlates of antenatal care usage among adolescent mothers in Nigeria: a pooled data analysis. Women Heal. 2021;61(1):38–49. doi:10.1080/03630242.2020.1844359
18. Gross K, Alba S, Glass TR, Schellenberg JA, Obrist B. Timing of antenatal care for adolescent and adult pregnant women in south-eastern Tanzania. BMC Pregnancy Childbirth. 2012;12. doi:10.1186/1471-2393-12-16
19. Bbaale E. Factors influencing the utilisation of antenatal care content in Uganda. Australas Med J. 2011;4(9):516–526. doi:10.4066/AMJ.2011.849
20. Fulpagare PH, Saraswat A, Dinachandra K, et al. Antenatal care service utilization among adolescent pregnant women–evidence from Swabhimaan programme in India. Front Public Heal. 2019;7(December). doi:10.3389/fpubh.2019.00369
21. Uldbjerg CS, Schramm S, Kaducu FO, Ovuga E, Sodemann M. Perceived barriers to utilization of antenatal care services in northern Uganda: a qualitative study. Sex Reprod Health Care. 2020;23. doi:10.1016/j.srhc.2019.100464
22. Chi PC, Bulage P, Urdal H, Sundby J. A qualitative study exploring the determinants of maternal health service uptake in post-conflict Burundi and Northern Uganda. BMC Pregnancy Childbirth. 2015;15(1):1–14. doi:10.1186/s12884-015-0449-8
23. Conrad P, De Allegri M, Moses A, et al. Antenatal care services in rural Uganda: missed opportunities for good-quality care. Qual Health Res. 2012;22(5):619–629. doi:10.1177/1049732311431897
24. Benova L, Dennis ML, Lange IL, et al. Two decades of antenatal and delivery care in Uganda: a cross-sectional study using Demographic and Health Surveys. BMC Health Serv Res. 2018;18(1):1–15. doi:10.1186/s12913-018-3546-3
25. Nansubuga R. Factors affecting the utilization of antenatal care services among adolescent pregnant mothers. Case study of Naguru Teenage Health Center, Kampala. Int Stat Inst. 2011;2011:6012–6017.
26. Ministryof Health Uganda. National Health Facility Master List 2018; 2018. Available from: http://library.health.go.ug/sites/default/files/resources/National.Health.Facility.Master.List.2018_0.pdf.
27. Uganda Bureau of Statistics. The national population and housing census 2014 - main report. Kampala; 2016.
28. Vörösmarty G, Dobos I. Green purchasing frameworks considering firm size: a multicollinearity analysis using variance inflation factor. Supply Chain Forum. 2020;21(4):290–301. doi:10.1080/16258312.2020.1776090
29. Jinga N, Mongwenyana C, Moolla A, Malete G, Onoya D. Reasons for late presentation for antenatal care, healthcare providers’ perspective. BMC Health Serv Res. 2019;19. doi:10.1186/s12913-019-4855-x
30. Mgata S, Maluka SO. Factors for late initiation of antenatal care in Dar es Salaam, Tanzania: a qualitative study. BMC Pregnancy Childbirth. 2019;19. doi:10.1186/s12884-019-2576-0
31. Ali SA, Dero AA, Ali SA, Ali GB. Factors affecting the utilization of antenatal care among pregnant women: a literature review. Int J Tradit Complement Med. 2016;2(2):41–45. doi:10.28933/sina-ijtcm-2016
32. Ndugga P, Naminyonga N, Sebwufu D. Determinants of early post natal care in Uganda: further analysis of the 2016 demographic and health survey. Dhs. 2019;2019:1.
33. Habibov N, Zainiddinov H. Do family planning messages improve antenatal care utilization? Evidence from Tajikistan. Sex Reprod Healthc. 2017;13:29–34. doi:10.1016/j.srhc.2017.05.005
34. Ndambuki SM, Oyindamola BY, Aimakhu CO. Factors influencing utilization of antenatal care services among teenage mothers in malindi sub-county Kenya-A cross sectional study. Sci J Public Heal. 2017;5(2):61. doi:10.11648/j.sjph.20170502.12
35. Chaibva CN, Roos JH, Ehlers VJ. Adolescent mothers’ non-utilisation of antenatal care services in Bulawayo, Zimbabwe. Curationis. 2009;32(3):14–21. doi:10.4102/curationis.v32i3.1219
36. Paudel YR, Jha T, Mehata S. Timing of first antenatal care (ANC) and inequalities in early initiation of ANC in Nepal. Front Public Heal. 2017;5:1–6. doi:10.3389/fpubh.2017.00242
37. Simkhada B, Teijlingen VER, Porter M, Simkhada P. Factors affecting the utilization of antenatal care in developing countries: systematic review of the literature. J Adv Nurs. 2008;61(3):244–260. doi:10.1111/j.1365-2648.2007.04532.x
38. Rurangirwa AA, Mogren I, Nyirazinyoye L, Ntaganira J, Krantz G. Determinants of poor utilization of antenatal care services among recently delivered women in Rwanda; a population based study. BMC Pregnancy Childbirth. 2017;2017:1–10. doi:10.1186/s12884-017-1328-2
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.