Back to Journals » HIV/AIDS - Research and Palliative Care » Volume 15
Time to Viral Re-suppression and Its Predictors among Adults on Second-Line Antiretroviral Therapy in South Wollo Zone Public Hospitals: Stratified Cox Model
Authors Melak D , Wedajo S , Dewau R
Received 26 March 2023
Accepted for publication 9 June 2023
Published 5 July 2023 Volume 2023:15 Pages 411—421
DOI https://doi.org/10.2147/HIV.S406372
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Prof. Dr. Olubunmi Akindele Ogunrin
Dagnachew Melak, Shambel Wedajo, Reta Dewau
Department of Epidemiology and Biostatistics, School of Public Health, College of Medicine and Health Sciences, Wollo University, Dessie, Ethiopia
Correspondence: Dagnachew Melak, Email [email protected]
Background: Even though there are many patients on second-line antiretroviral therapy (ART) in Ethiopia, there is a paucity of evidence on the rate of viral resuppression and its predictors. Therefore, this study aimed to determine a time to viral resuppression and identify predictors among adults on second-line ART in South Wollo public hospitals, northeast Ethiopia.
Methods: A retrospective-cohort study design was employed using patients enrolled in second-line ART from August 28, 2016 to April 10, 2021. Data were collected using a structured data-extraction checklist with a sample size of 364 second-line ART patients from February 16 to March 30, 2021. EpiData 4.6 was used for data entry and Stata 14.2 was used for analysis. The Kaplan–Meier method was used for estimating time to viral resuppression. The Shönfield test was used to check the proportional-hazard assumption, and the “no interaction” stratified Cox assumption was checked using the likelihood-ratio test. A stratified Cox model was applied to identify predictors of viral resuppression.
Results: Median time to viral re-suppression in patients on a second-line regimen was 10 (IQR 7– 12) months. BeingFemale (AHR 1.31, 95% CI 1.01– 1.69), low viral load count at switch (AHR 1.98, 95% CI 1.26– 3.11), normal-range BMI at switch (AHR 1.42, 95% CI 1.03– 1.95), and lopinavir-based second-line regimen (AHR 1.72, 95% CI 1.15– 2.57) were significant predictors of early time to viral resuppression after stratification by WHO stage and adherence level.
Conclusion: Median time to viral re-suppression after switching to second-line ART was 10 months. In the stratified Cox model, female sex, baseline viral copies, second-line regimen type, and BMI at switch were statistically significant predictors of time to viral resuppression. Different stakeholders working on the HIV program should maintain viral resuppression by addressing significant predictors, and ART clinicians should consider ritonavir-boosted lopinavir based second-line ART for newly switched patients.
Keywords: time to viral resuppression, predictors, second-line ART, stratified Cox model
Introduction
The global community has committed to ending the HIV pandemic as a public health threat by 2030 as part of the UN Sustainable Development Goals.1,2 Despite major progress in the response, HIV pandemics continue to pose a serious public health burden globally, especially in sub-Saharan Africa carries the highest burden in which75% of deaths due to HIV/AIDS was accounted in, a Joint United Nations Programme on HIV/AIDS (UNAIDS) 2014 report.1,3
According to a WHO global report, in 2018 6.8% of patients were receiving second-line treatment worldwide.4 In sub-Saharan Africa, nearly 1.63 of every 100 HIV patients switch to second-line antiretroviral therapy (ART) every year.5 In Ethiopia, patients on second-line treatment account for 1.5% of all ART users.6 Although the number of patients switching to second-line ART is increasing in sub-Saharan Africa, the development of treatment failure on second-line ART is a challenge to sustaining viral resuppression.7,8 Second-line ART is recommended for patients resistant to first-line ART that contains a minimum of three active drugs, of which one should be in a new class to increase the likelihood of treatment success and minimize the risk of cross-resistance.9–11
The goal of ART is viral load suppression and increases the CD4 count which eventually improves the general health of the clients and prevents transmission of HIV to others.9,12 For patients on second-line ART, viral re-suppression is considered when the virus is unable to replicate itself in the patient’s blood, viral load maintained <1000 copies/mL, or the virus being undetectable in the blood within a given course of treatment.9 Undetectable viral load makes patients have strong motivation and adhere to their medication and follow-up care, and is a key indicator of treatment success.9,10
Virological suppression varies across different contexts and patient characteristics. Most patients achieve undetectable viral load within 6 months following initiation of second-line ART.13 Achieving and maintaining viral suppression depends on the patient’s personal and clinical factors.11 In previous studies, CD4 count at switch,14,15 viral load count at switch,12,16,17 adherence,12,13,16,18 younger age,17 duration of viremia,17 BMI,15,19 history of TB,19 smoking and alcohol use,20 drug compliance level,18,19 and baseline resistance level to 3TC/TDF18 were some of the predictors of viral re-suppression after switching to second-line ART.
Recent evidence shows that more than half of the patients on second-line ART in low- and middle-income countries do not achieve or maintain continuous viral re-suppression.14 In Ethiopia, about one third of adults living with HIV in rural areas do not achieve viral suppression, and viral load suppression in some regions of Ethiopia is still low.21 As a result of this, there is a need for additional work to be done to strengthen the timely and proper use of viral load results to guide clinical decisions for patients on ART.22
Although there are many patients on second-line ART in Ethiopia, there is a paucity of evidence on time to viral resuppression and its predictors after switching to second-line ART. One study focused on the rate of viral resuppression based on a sample from a single health-care setup, and thus the representativeness and generalizability of the findings were limited.23 Unlike that study,23 the current study assessed the median time of viral suppression by including other sites and hospitals not yet assessed. The aforementioned study23 was not analyzed in the current study, since it was published after data collection and analysis had been conducted. Predictors that influence time to viral resuppression vary across different settings and population groups, and thus the use of context-based evidence is crucial for the design and implementation of effective intervention measures.
Studying time to viral resuppression and its predictors among second-line ART patients would be a significant input for different stakeholders regarding the current virological status of second-line ART users and help to plan future third-line ART needs. The study could also be used to track the progress towards the third of the 95–95–95 UNAID target by 2025. Therefore, this study aimed to determine the time to viral resuppression and identify its predictors among patients on second-line ART who had been followed in South Wollo public hospitals in northeast Ethiopia.
Methods
Study Design, Setting, and Period
A multicenter institution-based retrospective-cohort study design was employed. The study was conducted in South Wollo hospitals, which provide second-line ART service. South Wollo carries the highest burden of HIV in the Amhara region. HIV prevalence in South Wollo in 2015–2018 surveillance was 8.7% and 8.5% in Dessie, and the incidence of HIV in Dessie was highest in the Amhara region (5.74 per 1000 population).24 Currently, in South Wollo a total of 1319 patients are on second-line ART.25 South Wollo public hospitals that provide second-line ART include Dessie Comprehensive Specialized Hospital, Boru Meda General Hospital, Akesta General Hospital, Mekaneselam General Hospital, Sayint Primary Hospital, Tenta Primary Hospital, and Wureilu Primary Hospital. The study period was from August 28, 2016 to April 10, 2021, and the data were extracted from February 16 to April 10, 2021.
Participants
The source population was all second-line ART people living with HIV attending South Wollo public hospitals. The study included all HIV-infected patients on second-line therapy who were enrolled during the study period in South Wollo public hospitals providing second-line ART service. Clients who had had follow-up <6 months and who had no second viral load test results were excluded from the study.
Sample-Size Determination and Sampling Technique
The required sample size was determined using Epi Info software by considering the 95% CL, 80% power, and percentage of outcomes in exposed and unexposed groups of variables taken from previous studies on second-line ART. In a previous study, CD4 count, viral load at switch, and adherence level were selected based on their clinical importance and statistically significant association with viral load resuppression after switching to second-line ART. Among all variables, CD4 count at switch to second-line ART15 yielded a sufficient sample size of 364. All hospitals that provide second-line ART services in South Wollo were included in the study. The total sample size was proportionally allocated depending on the number of clients on second-line ART in each hospital during the study period. Participants from each hospital were selected through simple random sampling using a computer-generated lottery method from their ART smart-care registration.
Variable Measurement
The dependent variable was time to viral load resuppression. The time variable in this study was the time from initiation of second-line ART to viral resuppression <1000 copies/mL of blood. The event of interest was success (event = 1) if patients had viral resuppression, with event = 0 if censored. Independent variables were age at initiation of second-line ART, sex, marital status (single/married/divorced/ widowed), place of residence (urban/rural), education (none/primary/secondary/higher education), occupation (government-employed/self-employed/farmer). Behavioral and social factors considered were history of smoking (yes/no), alcohol use (yes/no), chat chewing (yes/no), disclosure (yes/no), and enhanced adherence support given (yes/no).
Clinical and treatment related factors were first-line regimen before switch (efavirenz-based/neverapin-based), second-line regimen (ritonavir-boosted atazanavir [atazanavir/r]- or lopinavir/r-based), history of first-line regimen change (yes/no), viral load count at switch (1000–10,000/10,000–100,000/>100,000 copies/mL), CD4 count at switch (<200/200–400/>400 cells/mm3), adherence (poor/fair/good), functional status (working/ambulatory/bedridden), WHO clinical stage (I/II/III–IV), use of cotrimezazole preventive therapy (yes/no), isoniazid preventive therapy use (yes/no), and BMI at initiation (<18.49/18.5–24.9/>25 kg/m2).
Operational Definitions
Viral resuppression was defined as a viral load count <1000 copies/mL of blood or undetectable viral load after a given duration of treatment.9,26 Right censoring was if the patient died, was lost to follow-up (LTFU), was transferred to another treatment site, developed any other outcome without experiencing viral resuppression, or had not virally resuppressed at the end of the study period. Time defined as the duration taken to re-suppress thier viral load following initiation of second-line ART, and for unsuppressed clients, it was the point at which they had their final measured of viral load or duration since the start of second-line ART (months). Beginning time was defined as the date of second-line ART initiation. Ending time was defined as the date of confirmed viral suppression for suppressed and the last measured time for unsuppressed patients. Adherence was measured by patient self-report of the number of doses they had missed in the month prior, and designated good, fair, or poor.27
Data-Collection Tool and Data Quality Control
A structured data-extraction checklist was prepared in line with the chronic HIV follow-up form and HIV intake forms. Secondary data were collected retrospectively from chronic ART follow-up forms and routinely collected follow-up data available from ART cohort registration, ART intake forms, and viral load registration books. Sociodemographic data were collected from ART follow-up forms and ART intake forms. Two trained nurses working in the ART clinic at each study setting were selected as data extractors.
Data quality was maintained by developing a simple and easily understandable data extraction checklist which was prepared in line with the current chronic HIV care follow-up formats. Two days of training were delivered for all data collectors and supervisors on the purpose of the study, participant selection technique and data extraction methods on patient follow-up forms and registration books, and how to record the data. Supervisors from each site were assigned during data collection to assess incomplete data on a daily based and after the data collection period, the principal investigators also controlled the overall activities during the data collection period.
Data Processing and Analysis
The extracted data were entered and coded in EpiData 4.6 and then it was exported to STATA software (version 14.2) for analysis. Descriptive statistics, including mean, median, and frequency tables were presented to describe the characteristics of the study participants. Rate Viral resuppression after initiation of second-line ART had been described by incidence density and proportion of viral resuppression from the total sample size. Time to viral resuppression was calculated using Kaplan–Meier survival function. Kaplan–Meier curves and tables for log-rank tests were used to estimate overall median survival and compare median survival between categorical variables.
The proportional-hazard assumption using the Shönfield test was checked to determine model fitness. A stratified Cox model without interaction regression was used to identify predictors of viral resuppression after switching to second-line ART. Variables with P<0.25 on bivariate Cox regression were candidates for multivariate analysis of the stratified Cox model. Crude and adjusted HRs with corresponding 95% CIs and P-values were computed and interpreted according to their statistical significance (P<0.05 on multivariate analysis interpreted using AHRs).
Results
Sociodemographic Characteristics
Of 364 patient cards, 35 (9.6%) medical folders were taken from primary hospitals, 129 (35.4%) from general hospitals, and 200 (54.9%) from referral-and-above hospitals. Of the 364 second-line ART patients, 205 (55.5%) were male. The mean age of patients was 36.78±12 years, 205 (56.3%) were urban residents, and half 184 (50.5%) were married. Detailed sociodemographic characteristics of the patients are in Table 1.
 |
Table 1 Sociodemographic characteristics of patients on second-line ART in South Wollo Zone public hospitals, Northeast Ethiopia(n=364) |
Behavior-Related Characteristics
In sum, 279 (76.6%) patients had disclosed their HIV status to at least one person and almost half 184 (50.5%) had missed ART doses during the study period. Among these, 39 (21.4%) reported that this was due to forgetting to take the drug. Regarding appointments, 172 (47.3%) had missed at least one clinical visit during the study period. Among these, 40 (23.4%) reported illness as the main reason. Among 224 patients who received enhanced adherence counseling, >90% had - more than two EAC sessions Table 2.
 |
Table 2 Sociobehavioral characteristics of patients on second-line ART in South Wollo Zone public hospitals, Northeast Ethiopia (n=364) |
Clinical and Treatment-Related Characteristics
Median CD4 count at switch was 213 (IQR 124–343) cells/mm3 and median viral load count was14,895 (IQR 4729–41,463) copies/mL. Mean hemoglobin level at switch was 13.309±2.1 g/dL. More than half (56.3%) had been taking efavirenz-based first-line ART, whereas 319 (87.6%) patients were on atazanavir/r-based second-line ART. A total of 194 (53.3%) patients were WHO stage I, 111 (30.5%) stage II, and 59 (16.2%) developed WHO stage III and IV opportunistic infections. Overall, 268 (73.6%) had good adherence, 50 (13.7%) fair adherence, and 46 (12.6%) poor adherence (Table 3).
 |
Table 3 Clinical and treatment-related characteristics of patients on second-line ART IN South Wollo Zone public hospitals, Northeast Ethiopia (n=364) |
Time to Viral Resuppression on Second-Line ART
Median time to viral resuppression after switching to second-line ART was 10 months.7–11,14 After a minimum of 6 months on second-line ART, the incidence of viral resuppression was 84/1000 person-month follow-up, and the proportion of viral resuppression during the study period was 293 (80.5%) (Table 4). The Kaplan–Meier estimation showed that there was a difference in median time to viral resuppression among groups of predictors (WHO clinical stage, viral load at switch, second-line regimen, adherence level, and BMI; (Table 5).
 |
Table 4 Kaplan–Meier estimation of time to viral resuppression |
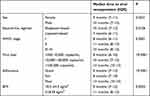 |
Table 5 Median survival time by predictor variable with log-rank test |
Estimated median time to viral resuppression for females was 9 (IQR 7–11) months, which was significantly shorter than for males (10 [IQR 7–12] months, log-rank P=0.0231). For patients on an atazanavir-based second-line regimen, estimated median survival was 10 (IQR 7–12) months, which was longer than patients on a lopinavir-based regimen (7 [IQR 6–11] months; log-rankP=0.0106). By WHO clinical stage, estimated median survival for stage I patients was 8 (IQR 6–11) months,which was relatively shorter than stage II patients (11 [QR 8–13] months; log-rank P=0.0001). There was a significant difference in estimated survival between patients with viral load of 1000–10,000 copies (8 [IQR 6–10] months), 10,000–100,000 copies (10 [IQR 7–12] months), and >100,000 copies (12 [IQR 10–13] months; P<0.0001), but there was no significant difference in median survival between viral load of 10,000–100,000 copies and >100,000 copies. There was a statistically significant difference in median survival of patients with good adherence (9 [IQR 7–12] months) and poor adherence (13 [IQR 10–15] months; log-rank P<0.0001). There was a statistically significant difference in median survival of patients with BMI 18.5–24.9 kg/m2 (9 [IQR 7–12] months) and BMI ≤18.49kg/m2 (11 [IQR 8–12] months; log-rank P=0.0052).
Model Fitness
The overall proportional-hazard assumption was fulfilled in the global test (P=0.1395), but WHO stage and adherence level failed to meet it. To select the best-fitted model for estimating the valid effect of predictors of time to viral resuppression, the standard Cox regression model, stratified Cox regression model without interaction, and stratified Cox model with interaction were compared using the likelihood ratio (LR) test, Akaike’s information criterion (AIC), and Bayesian information criterion.
Model 1: standard Cox regression model without stratification by WHO SAGE or adherence (AIC=2932.779).
Model 2: stratified Cox regression model with the assumption of no interactions (AIC=2067.63, best fit).
Model 3: stratified Cox regression model with interaction between predictors (AIC=2070.294).
For LR test statistics, no interaction assumption of the Stratified Cox regression model was fulfilled by comparing the log-likelihood statistics for noninteraction (model 2) or interaction (model 3) under the assumption of model 2 nested in model 3. The LR test result was x2=1.34, and this was insignificant (P=0.5126).
Predictors of Time to Viral Re-suppression
Bivariate Cox regression revealed that sex, education, history of first-line regimen change, WHO stage, CD4 count, viral load, BMI, second-line regimen type, and adherence were independent predictors of time to viral resuppression after switching to second-line ART (P<0.250 and candidates for the final multivariate Cox regression analysis. Multivariate stratified Cox regression without interaction (stratified by WHO stage and adherence) analysis revealed that sex, viral load at switch, BMI, and second-line ART regimen were statistically significant predictors of time to viral resuppression (P≤0.05, Table 6).
 |
Table 6 Bivariate cox regression and stratified cox regression without interaction (stratified by WHO stage and adherence level) analysis of predictors of time to viral resuppression (n=364) |
Adjusting for other predictors and controlling WHO stage and level of adherence by stratification, the rate of viral resuppression in females was 1.31 times higher thanthat of males (AHR 1.31, 95% CI 1.01–1.69). The rate of viral re-suppression for patients with viral load 1000–10,000 copies/mL was 1.98 times higher than that of patients with viral load >100,000 copies/mL after stratification by WHO stage and adherence (AHR 1.98, 95% CI 1.26–3.11).
BMI 18.5–24.9 kg/m2 increased time to viral resuppression by 1.42-fold when compared with BMI ≤18.49 kg/m2 after stratification by WHO stage and adherence (AHR 1.42, 95% CI 1.03–1.95). A lopinavir-based second-line regimen increased the time to viral resuppression by 1.72-fold when compared with an atazanavir-based second-line regimen after stratification by WHO stage and adherence (AHR 1.72, 95% CI 1.15–2.57).
Discussion
Median time to viral suppression was 10 (IQR (7–12) months, in line with a study done in Kenya.28 Patients are expected to achieve viral resuppression within 6 months following the initiation of second-line ART.11 In this study, median time was longer than expected time to viral resuppression, in line with a study done in Mozambique.29 This might be due to a lack of routine viral load testing as per the guidelines in these study settings.27 This suggests that routine viral load testing is important to determine the exact time to viral resuppression10,26 and essential to achieve the third component of the 95–95–95 UNAIDS target.9 It would be better to conduct a prospective cohort study on second-line ART patients to determine the actual time to viral resuppression after switching to second-line ART.
From sociodemographic characteristics, sex was a significant predictor of time to viral resuppression. Being female increased the rate of viral resuppression, consistent with a study done in Ethiopia.30,31 This might be due to better clinical adherence and better response to ART therapy in females than in males,32 and also perhaps due to the lower likelihood of females to be substance abusers. This finding is not supported by a study done in Eastern Europe,12 in which sex had no significant effect on viral suppression. This contradiction might be due to differences in other sociodemographic characteristics of the patients.
Another predictor was viral load at switch: low viral load at switch meant a shorter time to achieve viral resuppression. This finding was consistent with studies done in South Africa,15,17 India,20 and Eastern Europe.12 Patients with low viral load can resuppress early after effective ART initiation, and those with high viral load at switch may have been severely immunocompromised, which can prolong the rate of viral resuppression.33 This finding suggests that timely switching of patients before viral load becomes very high might improve the rate of viral resuppression.14 This finding also suggests that patients with high viral load should receive enhanced adherence counseling services to have a good virological outcome.27
BMI was a significant predictor of time to viral resuppression. The rate of resuppression was higher among patients whose BMI was in the normal range (18.5–24.9 kg/m2). This finding was consistent with studies done in South Africa.15,19 This can be explained by a normal BMI indicating adequate nutritional status, which may affect early immunorecovery and increase T-lymphocyte proliferation, strengthening the body’s defense mechanisms against the replication of HIV.34 This implies that patients with low BMI should receive appropriate nutritional treatment and counseling as per treatment guidelines.
Second-line regimen type was a significant predictor of time to viral suppression. Patients on LPV/r-based second-line ART were more likely to experience viral resuppression than those on ATV/r-based second-line ART. This finding was consistent with a study done in Johannesburg, South Africa15 and one in Cambodia.35 This could be due to the fact that lopinavir is highly potent and less prone to inherent virus resistance.15,35,36 This study finding was also supported by a systematic review and meta-analysis study that concluded that a lopinavir/r-based second-line regimen had good efficacy in viral resuppression and immunological recovery and little drug resistance.37
Strengths and Limitations
We studied patients followed up in all hospitals in South Wollo with an adequate sample size from each hospital, and thus the generalizability of the findings is better. This study uses the stratified Cox model, which is an important extension of the ordinary Cox regression model, to allow for covariates with disproportionate hazards. Secondary data (data registered for another purpose) were used, which made it difficult to measure some predictor variables in appropriate ways and to find other important predictor variables. In the stratified Cox model, there was no way to assess the effect of stratification variables.
Conclusion
This study revealed that the median time to viral resuppression after switching to second-line ART was 10 months. Female sex, low viral load at switch, normal BMI, and lopinavir-based second-line regimen type were significant predictors of time to viral resuppression after stratification by WHO clinical stage and adherence. Those patients who failed to achieve viral resuppression may need additional adherence support to improve treatment outcomes.
Patients on lopinavir/r-based second-line ART have better virological outcomes. For hospitals, it is better to have adequate stock and increase utilization of lopinavir/r-based second-line regimens. ART clinicians and case managers should provide enhanced adherence counseling for all patients with high viral load. Health-care providers in hospitals should provide nutritional counseling and appropriate treatment for those patients with low BMI. This study has some limitations; therefore, it requires additional prospective studies by including such variables as substance use–related factors, organ-function tests, and other predictors by measuring variables directly from the patients. Some predictor variables in this study indicate time variation; therefore, it would be better to conduct time-dependent Cox regression to determine the valid effect of predictor variables on time to viral resuppression.
Abbreviations
ART, antiretroviral therapy; UNAIDS, Joint United Nations Programme on HIV/AIDS; WHO, World Health Organization.
Data Sharing
The datasets generated and analyzed during the current study are not publicly available due to confidentiality issues, but are available from the corresponding author upon reasonable request.
Ethics
Ethics clearance was obtained from the Institutional Review Board of Wollo University College of Medicine and Health Science (reference CMHS/803/13/22). Patient information was secured and locked. Patients found to be virally unsuppressed during data collection were identified, ART clinicians and case managers in the hospital informed, and prepared for adherence counseling support and assessed their clinical conditions and managed accordingly. Informed consent was waived by the Institutional Review Board of Wollo University College of Medicine and Health Science, since secondary data by document review were used; however, written consent was obtained from each study setting and a legal agreement signed with authorized personnel in hospitals. This study complied with the Declaration of Helsinki.
Acknowledgments
First and foremost, we would like to acknowledge Wollo University School of Public Health for allowing us to study this issue. We would also like to acknowledge the North and South Wollo zonal health departments and Dessie health department for their willingness to cooperate and provide information regarding second-line ART patients in South Wollo hospitals. Lastly, our gratitude goes to our friends and associates for their intellectual, technical, and nontechnical support.
Author Contributions
All authors made a significant contribution to manuscript development, whether in the conception, study design, execution, acquisition of data, analysis, and interpretation, took part in drafting, revising, or critically reviewing the article, gave final approval of the version to be published, have agreed on the journal to which the article has been submitted, and agree to be accountable for all aspects of the work.
Funding
The sources of funding for this research were Dessie Health Science College and Wollo University. The role of the funding body was the design of the study, collection, analysis, and interpretation of data, and writing the manuscript and financial support.
Disclosure
The authors declare that they have no conflicts of interest.
References
1. World Health Organization. Global Health Sector Strategy on HIV 2016–2021. World Health Organization; 2016.
2. UNAIDS. An Ambitious Treatment Target to Help End the AIDS Epidemic. UNAIDS; 2014.
3. UNAIDS. United Nations programme on HIV/AIDS. In: The Gap Report. Geneva: UNAIDS; 2014:1–334.
4. World Health Organization. Technical Report Aids Medicines and Diagnostics Service. World Health Organization; 2020.
5. Jensen DM. Monitoring and switching of first-line antiretroviral therapy in sub-Saharan Africa: collaborative analysis of adult treatment cohorts. Physiol Behav. 2018;176(1):1570–1573.
6. Assefa Y, Gilks CF, Lynen L, et al. International journal of infectious diseases performance of the antiretroviral treatment program in Ethiopia, 2005–2015: strengths and weaknesses toward ending AIDS. Int J Infect Dis. 2017;60:70–76. doi:10.1016/j.ijid.2017.05.012
7. Avert. “Alarming” rates of second-line HIV treatment failure in sub-Saharan Africa; 2019.
8. Phillips A, Shroufi A, Vojnov L, et al. Sustainable HIV treatment in Africa through viral-load-informed differentiated care. Nature. 2015;528(7580):S68–76. doi:10.1038/nature16046
9. Suppression VL. Reaching the third 95: viral load suppression among key population individuals living with HIV. 2013.
10. UNAIDS. The need for routine viral load testing. Available from: http://www.unaids.org/sites/default/files/media_asset/JC2845_en.pdf.
11. Centers for Disease Control and Prevention. Evidence of HIV treatment and viral suppression in preventing the sexual transmission of HIV. Dep Heal Hum Serv. 2018;4:15.
12. Chkhartishvili N, Sharvadze L, Dvali N, et al. Virologic outcomes of second-line antiretroviral therapy in Eastern European country of Georgia. AIDS Res Ther. 2014;11(1):1–6. doi:10.1186/1742-6405-11-18
13. Murphy RA, Sunpath H, Castilla C, et al. Second-line antiretroviral therapy: long-term outcomes in South Africa. J Acquir Immune Defic Syndr. 2012;61(2):158–163. doi:10.1097/QAI.0b013e3182615ad1
14. Huang X, Xu L, Sun L, et al. Six-year immunologic recovery and virological suppression of HIV patients on LPV/R-based second-line antiretroviral treatment: a multi-center real-world cohort study in China. Front Pharmacol. 2019;10:1–8. doi:10.3389/fphar.2019.01455
15. Shearer K, Evans D, Moyo F, et al. Treatment outcomes of over 1000 patients on second-line, protease inhibitor-based antiretroviral therapy from four public-sector HIV treatment facilities across Johannesburg, South Africa. Trop Med Int Heal. 2017;22(2):221–231. doi:10.1111/tmi.12804
16. Chakravarty J, Sundar S, Chourasia A, et al. Outcome of patients on second line antiretroviral therapy under programmatic condition in India. BMC Infect Dis. 2015;15(1). doi:10.1186/s12879-015-1270-8
17. Johnston V, Fielding K, Charalambous S, et al. Second-line antiretroviral therapy in a workplace and community-based treatment programme in South Africa: determinants of virological outcome. PLoS One. 2012;7(5):e36997. doi:10.1371/journal.pone.0036997
18. Chen J, Zhang M, Shang M, Yang W, Wang Z, Shang H. Research on the treatment effects and drug resistances of long-term second-line antiretroviral therapy among HIV-infected patients from Henan Province in China. BMC Infect Dis. 2018;18:1–12.
19. Fox MP, Ive P, Long L, Maskew M, Sanne I. High rates of survival, immune reconstitution, and virologic suppression on second-line antiretroviral therapy in South Africa. J Acquir Immune Defic Syndr. 2010;53(4):500–506. doi:10.1097/QAI.0b013e3181bcdac1
20. Desai M, Dikshit R, Patel D, Shah A. Early outcome of second line antiretroviral therapy in treatment-experienced human immunodeficiency virus positive patients. Perspect Clin Res. 2013;4(4):215. doi:10.4103/2229-3485.120170
21. Report F. Ethiopia population-based HIV impact assessment; 2020.
22. Pepfar. Ethiopia country operational plan COP2020/FY2021 strategic direction summary; 2020.
23. Wedajo S, Degu G, Deribew A, Ambaw F. Rate of viral re-suppression and retention to care among plhiv on second-line antiretroviral therapy at Dessie comprehensive specialized hospital, northeast Ethiopia: a retrospective cohort study. HIV/AIDS - Res Palliat Care. 2021;13:877–887. doi:10.2147/HIV.S323445
24. Care P. Epidemiology of HIV infection in the Amhara Region of Ethiopia, 2015 to 2018 surveillance data analysis; 2020.
25. Departement South Wollo Zonal Health. south wollo zone health facility five month ART utilization report; 2013.
26. Médecins Sans Frontières. Making viral load routine: successes and challenges in the implementation of routine HIV viral load monitoring. UNITAID Rep. 2016;2016:1–35.
27. Federal Ministry of Health of Ethiopia. National comprehensive HIV prevention, care, and treatment training for pharmacy professionals participant manual; 2018.
28. Maina EK, Mureithi H, Adan AA, Muriuki J, Lwembe RM, Bukusi EA. Incidences and factors associated with viral suppression or rebound among HIV patients on combination antiretroviral therapy from three counties in Kenya. Int J Infect Dis. 2020;97:151–158. doi:10.1016/j.ijid.2020.05.097
29. Finci I, Flores A, Gutierrez Zamudio AG, et al. Outcomes of patients on second- and third-line ART enrolled in ART adherence clubs in Maputo, Mozambique. Trop Med Int Heal. 2020;25(12):1496–1502. doi:10.1111/tmi.13490
30. Diress G, Dagne S, Alemnew B, Adane S, Addisu A. Viral load suppression after enhanced adherence counseling and its predictors among high viral load HIV seropositive people in North Wollo Zone public hospitals, Northeast Ethiopia, 2019: retrospective cohort study. AIDS Res Treat. 2020;2020:154.
31. Desta AA, Woldearegay TW, Futwi N, et al. HIV virological non-suppression and factors associated with non-suppression among adolescents and adults on antiretroviral therapy in northern Ethiopia: a retrospective study. BMC Infect Dis. 2020;20(1):1–10. doi:10.1186/s12879-019-4732-6
32. Bezabhe WM, Chalmers L, Bereznicki LR, Peterson GM, Bimirew MA, Kassie DM. Barriers and facilitators of adherence to antiretroviral drug therapy and retention in care among adult HIV-positive patients: a qualitative study from Ethiopia Article ID e97353. PLoS One. 2014;9(5).
33. Patel D, Cortina-Borja M, Thorne C, et al. Time to undetectable viral load after highly active antiretroviral therapy initiation among HIV-infected pregnant women. Clin Infect Dis. 2007;44(12):1647–1656.
34. Li X, Ding H, Geng W, et al. Predictive effects of body mass index on immune reconstitution among HIV-infected HAART users in China. BMC Infect Dis. 2019;19(1):1–9. doi:10.1186/s12879-018-3567-x
35. Ferradini L, Ouk V, Segeral O, et al. High efficacy of lopinavir/r-based second-line antiretroviral treatment after 24 months of follow up at ESTHER/Calmette Hospital in Phnom Penh, Cambodia. J Int AIDS Soc. 2011;14(1):14. doi:10.1186/1758-2652-14-14
36. Ndashimye E, Arts EJ. The urgent need for more potent antiretroviral therapy in low-income countries to achieve UNAIDS 90-90-90 and complete eradication of AIDS by 2030. Infect Dis Poverty. 2020;1(2019):1–8.
37. Huang Y, Huang X, Luo Y, et al. Assessing the efficacy of lopinavir/ritonavir-based preferred and alternative second-line regimens in HIV-infected patients: a meta-analysis of key evidence to support WHO recommendations. Front Pharmacol. 2018;9:1–12. doi:10.3389/fphar.2018.00890
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
