Back to Journals » International Medical Case Reports Journal » Volume 17
Tibial Adamantinoma: A Case Report from a Resource-Limited-Setting
Authors Yaynishet YA , Fayisa ST , Dencha BA, Hailu SS
Received 15 September 2023
Accepted for publication 12 March 2024
Published 25 March 2024 Volume 2024:17 Pages 221—225
DOI https://doi.org/10.2147/IMCRJ.S440401
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Xudong Zhu
Yodit Abraham Yaynishet,1 Shimalis Tadasa Fayisa,2 Bereket Amare Dencha,3 Samuel Sisay Hailu1
1Department of Radiology, Addis Ababa University, Addis Ababa, Ethiopia; 2Department of Radiology, Mizan Tepi University, Mizan, Ethiopia; 3Department of Pathology, Bahir Dar University, Bahir Dar, Ethiopia
Correspondence: Yodit Abraham Yaynishet, Department of Radiology, Addis Ababa University, P.O. Box: 9080, Addis Ababa, Ethiopia, Email [email protected]
Introduction: Adamantinoma is an infrequent, low-grade malignant bone tumor, predominantly affecting the tibia and often presents diagnostic challenges due to its nonspecific radiographic characteristics.
Case Presentation: A 55-year-old military personnel, with no history of trauma, who presented with a one-year history of right leg swelling and pain. Radiological examination showed right anterior tibial, mid diaphyseal lytic expansile lesion with internal trabeculations and excisional biopsy led to the diagnosis of adamantinoma. Below knee amputation was done as a definitive management.
Conclusion: Despite diagnostic challenges adamantinoma presents, the patient was referred to oncology and underwent amputation, underscoring the importance of considering adamantinoma in differential diagnosis for persistent bone lesions.
Keywords: adamantinoma, bone tumor, Ethiopia
Introduction
Adamantinoma is a rare primary bone tumor, comprising only 0.1% to 0.5% of all primary bone tumors.1 It predominantly afflicts the long bones, specifically the tibia, and exhibits a wide range of radiologic and histological presentations that often leads to diagnostic challenges.2 Adamantinomas are low-grade malignancies, however, they possess the ability to metastasize, with the lungs being the primary site.3
While the exact etiology of adamantinoma remains elusive, recent genetic and molecular studies have led to better characterizations of this bone tumor, providing some insights into the potential pathogenic mechanisms. Comprehensive molecular characterizations of adamantinoma have revealed genetic alterations that may potentially be targeted for therapeutic interventions.4
The disease is predominantly seen in young adults, with a slight male predominance, and has a tendency for local recurrence, especially in cases of incomplete resection.1,3 Multiple imaging modalities can play a role in its diagnosis. Plain film may demonstrate a soap bubble appearance while CT can be used to look for soft tissue extent as well as cortical involvement. Moreover, MRI is crucial for locoregional staging as well as guiding surgical management.5 Despite the advancements in medical imaging technologies, the diagnosis of adamantinoma can still be challenging due to its often nonspecific radiological findings. The radiographic picture may vary from a purely cystic lesion to an entirely sclerotic lesion, further complicating the diagnostic process. The role of histopathology, therefore, becomes pivotal in the diagnosis, with the typical finding of epithelial nests in a fibrous stroma leading to the diagnosis.6
The rarity of adamantinoma significantly hampers the development of standardized treatment protocols. Surgical resection, at present, remains the mainstay of treatment, with the aim being to achieve a wide resection margin and preserve limb function as much as possible.7 Nonetheless, in certain cases where limb salvage is not achievable, amputation becomes necessary.6
Here, we present a case of adamantinoma arising from the anterior tibia in a 55-year-old male patient in whom amputation was done. We have obtained informed consent from the patient to publish this case.
Case History
The patient is a 55-year-old well-fit male with a distinguished career in military service. He first noted symptoms approximately a year ago, with the onset of swelling and discomfort in his right leg. It was an unexpected development, as he had no prior history of trauma or similar conditions to the affected leg. Initially, the symptoms were subtle and intermittent; however, over the course of the year, they progressed, compelling him to seek medical attention.
The physical examination revealed a swelling in the right proximal leg. Notably, the overlying skin appeared intact, with no observable signs of inflammation or infection such as redness, heat, or pus. The pain, although not severe, was consistent, disrupting his daily activities.
Prompt diagnostic tests were performed, beginning with an AP and lateral X-ray of the affected leg. The radiographic images showed a right anterior tibial, mid diaphyseal lytic expansile lesion with internal trabeculations. The lesion has a narrow zone of transition with associated solid type of periosteal reaction. There are also small adjacent lytic satellite lesions (Figure 1A and B). An abdominal ultrasound was further conducted, which was nonrevealing. Additional tests, such as a chest X-ray, were also carried out to exclude any potential systemic issues which was unremarkable.
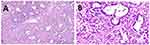
In a context with limited resources, the patient faced constraints in accessing certain diagnostic and treatment options. The challenge of obtaining CT or MRI scans in a timely manner in our setting led the multidisciplinary team to opt for an excisional biopsy of the leg lesion. The histopathology results showed biphasic tumoral tissue composed of mildly atypical round to oval cells arranged in tubular structures and basaloid nests along with variably cellular fibrous stroma which confirmed a diagnosis that was least expected: adamantinoma, a rare and often aggressive type of bone tumor (Figure 2A and B).
Upon diagnosing adamantinoma, the patient was promptly connected with an oncology team experienced in orthopedic cancers. The X-ray findings clearly displayed extensive involvement of the proximal tibia beyond the bone cortex. Taking into account the patient’s overall health, the aggressive nature of adamantinoma, and its specific location, the team concluded that amputation was the most viable treatment option, given the limited availability of alternative treatment methods. Following the amputation, the patient’s wound healed effectively with no evidence of either distant metastasis or local recurrence. Subsequently, the patient was discharged and scheduled for a follow-up appointment.
Discussion
The diagnosis of adamantinoma can be a challenging endeavor due to its low prevalence, its ability to mimic benign bone conditions, and the variation in its radiological presentation.2,8 Misdiagnosis or delayed diagnosis of adamantinoma can increase the risk of local recurrence and distant metastasis.9,10 Therefore, the importance of considering adamantinoma in the differential diagnosis for persistent or unexplained bone lesions cannot be overstated. In this context, the presented case underscores the diagnostic challenges inherent in adamantinoma, with the patient having presented with symptoms of right leg swelling and pain for a year before the diagnosis was confirmed through excisional biopsy.
In the diagnosis of adamantinomas, various imaging techniques are employed. Plain films may display a characteristic “soap bubble” appearance. Computed Tomography (CT) scans, while generally non-specific, are adept at delineating the cortical aspects of the tumor and are essential for detecting pulmonary metastases. However, CT scans are limited in revealing the tumor’s intraosseous expansion. On the other hand, Magnetic Resonance Imaging (MRI) is vital, demonstrating typical findings akin to many bone tumors – low signal intensity on T1-weighted images and high signal intensity on T2-weighted images. MRI’s crucial role extends to locoregional staging, identifying distant cortical abnormalities, and detecting soft tissue or intramedullary extensions. This makes MRI indispensable for determining tumor-free margins, thereby guiding the planning and execution of reconstructive surgery.5,11
A particular diagnostic challenge is posed by osteofibrous dysplasia (OFD), a benign bone condition that can coexist with adamantinoma and share similar histological characteristics. In a study by Schutgens et al, it was demonstrated that the surgical outcome and oncological survival between osteofibrous dysplasia-like adamantinoma and classic adamantinomas were comparable, further complicating the differentiation between the two.7 Nonetheless, histopathology often proves decisive in differentiating between the two conditions, with the presence of an epithelial component in the stroma being a distinguishing feature of adamantinoma.6,7 Furthermore, in the study of adamantinoma through immunohistochemistry, it’s found that the fibrous tissue part of the tumor exhibits a positive reaction to vimentin. Meanwhile, the epithelial cells of the tumor uniquely express a combination of keratin, epithelial membrane antigen (EMA), vimentin, p63, and podoplanin. On the other hand, markers such as estrogen, progesterone, and N-cadherin are identified in typical adamantinoma cases, but they are absent in variants of adamantinoma that resemble osteofibrous dysplasia.5,7
Surgical methods predominantly dictate the treatment of tibial adamantinoma. The most common and effective method is wide excision with clear margins, aiming to remove the tumor and a significant amount of surrounding healthy tissue. This procedure ensures the thorough removal of cancerous cells and reduces the risk of recurrence. Following excision, various reconstruction techniques are employed, such as free vascularized fibular graft, allograft, or endoprosthetic reconstruction, tailored to the extent of the excision and the patient’s specific needs. For adamantinoma in long bones, en-bloc resection is often utilized. This technique entails removing the tumor in one piece with wide surgical margins, serving as a standard approach in certain case12 In more severe instances, where other treatments are not feasible as in the presented case, amputation may be considered as a viable option.13 A study by Kumar et al also reported on a similar case where the patient underwent amputation due to an adamantinoma lesion in the tibia.6
Emerging research has begun to explore the role of adjuvant therapies in the management of adamantinoma. These include radiation therapy and targeted therapies based on molecular analysis of the tumor. For instance, in a study by Ali et al, it was demonstrated that targeted therapies against specific genetic alterations in adamantinomas could be promising avenues for future therapeutic interventions.4
Despite the advances in understanding the disease, the pathogenesis of adamantinoma remains incompletely understood. This knowledge gap, along with the rarity of the disease, poses significant challenges to the development of standardized treatment protocols. Therefore, further research is needed to better understand the pathogenesis of adamantinoma, explore potential therapeutic targets, and ultimately improve patient outcomes.
Conclusion
We have found a biopsy proven case of adamantinoma arising from the tibia in a patient with a year long history of leg pain who eventually underwent amputation. This case highlights the diagnostic complexities of adamantinoma and underscores the importance of maintaining a high index of suspicion for this rare tumor in cases of persistent or unexplained bone lesions.
Data Sharing Statement
The datasets used during the current study are available from the corresponding author on reasonable request.
Ethical Consideration
To publish this case report and related images, we received written informed consent from the patient. Institutional approval was not required to publish the case details.
Acknowledgment
We thank the patient for allowing the publication of this case report.
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis, and interpretation, or in all these areas; they took part in drafting, revising, or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted, and agree to be accountable for all aspects of the work.
Funding
There was no specific grant provided for this work by public, private, or nonprofit funding organizations.
Disclosure
The authors report no conflicts of interest in this work.
References
1. Aytekin MN, Öztürk R, Amer K. Epidemiological study of adamantinoma from US surveillance, epidemiology, and end results program: III retrospective analysis. J Oncol. 2020;2020.
2. Chen J, Zhang J. Adamantinoma filling the medullary space of the tibia: a case report. Radiol case rep. 2019;14(11):1330–1333. doi:10.1016/j.radcr.2019.08.013
3. Schwarzkopf E, Tavarez Y, Healey JH, et al. Adamantinomatous tumors: long‐term follow‐up study of 20 patients treated at a single institution. J Surgical Oncol. 2020;122(2):273–282. doi:10.1002/jso.25950
4. Ali NM, Niada S, Morris MR, et al. Comprehensive molecular characterization of adamantinoma and OFD-like adamantinoma bone tumors. Am J Surg Pathol. 2019;43(7):965–974. doi:10.1097/PAS.0000000000001251
5. Limaiem F, Tafti D, Malik A. Adamantinoma, in StatPearls. StatPearls Publishing; 2023.
6. Kumar A, Sharma R, Verma AK, et al. An unusual case of adamantinoma of long bone. Autopsy Case Reports. 2021;11:e2021276.
7. Varvarousis DN, Skandalakis GP, Barbouti A, et al. Adamantinoma: an updated review. in vivo. 2021;35(6):3045–3052. doi:10.21873/invivo.12600
8. Dashti NK, Howe BM, Inwards CY, et al. High-grade squamous cell carcinoma arising in a tibial adamantinoma. Human Pathol. 2019;91:123–128. doi:10.1016/j.humpath.2018.11.018
9. Deng Z, Gong L, Zhang Q, et al. Outcome of osteofibrous dysplasia-like versus classic adamantinoma of long bones: a single-institution experience. J Orthopaedic Surg Res. 2020;15(1):1–9. doi:10.1186/s13018-020-01769-5
10. Horvai A, Dashti NK, Rubin BP, et al. Genetic and molecular reappraisal of spindle cell adamantinoma of bone reveals a small subset of misclassified intraosseous synovial sarcoma. Mod Pathol. 2019;32(2):231–241. doi:10.1038/s41379-018-0115-6
11. Van Rijn R, Bras J, Schaap G, et al. Adamantinoma in childhood: report of six cases and review of the literature. Pediatric Radiol. 2006;36(10):1068–1074. doi:10.1007/s00247-006-0272-5
12. Smyth SL, Siddiqi A, Athanasou N, et al. Adamantinoma: a Review of The Current Literature. J Bone Oncol. 2023;41:100489. doi:10.1016/j.jbo.2023.100489
13. Zumárraga JP, Cartolano R, Kohara MT, et al. Tibial adamantinoma: analysis of seven consecutive cases in a single institution. Acta ortopedica brasileira. 2018;26(4):252–254. doi:10.1590/1413-785220182604192680
 © 2024 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2024 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.