Back to Journals » HIV/AIDS - Research and Palliative Care » Volume 16
The Association Between Oral Mucosal Lesions and Oral Health-Related Quality of Life Using the Validated Indonesian Version of OHIP-14 Among People Living with HIV/AIDS
Authors Sufiawati I , Amalia T, Dewi TS , Wisaksana R
Received 16 December 2023
Accepted for publication 5 February 2024
Published 8 February 2024 Volume 2024:16 Pages 9—16
DOI https://doi.org/10.2147/HIV.S452154
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Prof. Dr. Olubunmi Akindele Ogunrin
Irna Sufiawati,1 Tuty Amalia,2 Tenny Setiani Dewi,1 Rudi Wisaksana3
1Department of Oral Medicine, Faculty of Dentistry, Universitas Padjadjaran, Bandung, Indonesia; 2Oral Medicine Residency Program, Faculty of Dentistry, Universitas Padjadjaran, Bandung, Indonesia; 3Department of Internal Medicine, Dr. Hasan Sadikin Central General Hospital, Faculty of Medicine, Universitas Padjadjaran, Bandung, Indonesia
Correspondence: Irna Sufiawati, Department of Oral Medicine, Faculty of Dentistry, Universitas Padjadjaran, Jalan Sekeloa Selatan I, Bandung, 40132, Indonesia, Tel +62-22-2504985, Fax +62-22-2532805, Email [email protected]
Background: Oral mucosal lesions in human immunodeficiency virus (HIV) and acquired immunodeficiency syndrome (AIDS) patients, posing a concern for healthcare professionals, impact their oral health-related quality of life (OHRQoL). This study aimed to evaluate the association between oral mucosal lesions and OHRQoL as measured by the validated Indonesian version of the oral health impact profile-14 questionnaire (OHIP-14) among people living with HIV/AIDS (PLWHA).
Methods: A cross-sectional study was conducted at the Central Referral Hospital in West Java, Indonesia. The validity of OHIP-14 was evaluated in 30 PLWHA using inter-item corrected correlation, while reliability was assessed through Cronbach’s alpha and kappa coefficient agreement. Subsequently, a consecutive sample of 110 PLWHA self-completed the validated Indonesian version of OHIP-14 and underwent an oral examination. The association between oral mucosal lesions and OHRQoL was analyzed using the chi-squared test.
Results: The validity test of the OHIP-14 questionnaire produced a rcount > 0.189, meaning that all question items were valid and could be used to describe OHRQoL. The reliability test of the OHIP-14 questionnaire produced a Cronbach’s alpha value of 0.960 (> 0.7), which means that overall, the OHIP-14 questionnaire is reliable and feasible to be used to assess OHRQoL. Among the 110 enrolled participants, 61.8% were female and 38.2% were male, with the mean age 23.5 years old, the majority of them (59.1%) had been taking antiretrovirals (ARV), and (81.5%) had good QoL. There was a statistically significant relationship between oral lesions and quality of life (p< 0.05), particularly acute pseudomembranous candidiasis, angular cheilitis, recurrent intraoral herpes, and Stevens-Johnson syndrome.
Conclusion: This study indicated a significant association between oral mucosal lesions and OHRQoL in PLWHA. The successfully validated Indonesian version of the OHIP-14 questionnaire serves as a reliable and effective tool for assessing OHRQoL among PLWHA.
Keywords: OHIP-14, oral mucosal lesions, oral health-related quality of life
Introduction
Since the HIV-AIDS infection became a global pandemic, various abnormalities in the oral cavity among individuals living with HIV-AIDS have been identified, and they persist as a challenge even in the highly active antiretroviral era.1 The research findings from various countries indicate that 60–90% of individuals living with HIV-AIDS experience at least one abnormality in the oral cavity, commonly referred to as oral lesions, during the course of the disease. These oral lesions frequently manifest as the initial clinical symptoms of HIV infection, potentially serving a crucial role in the early detection of the disease. Moreover, these oral lesions can significantly impact the overall quality of life for people living with HIV/AIDS.2–4
According to World Health Organization (WHO), quality of life is the perception of an individual as a man or woman in life, in terms of the cultural context and value systems of where they live, and in relation to their standard of living, expectations, goals, and concerns. It encompasses a comprehensive range of physical health, psychological condition, independence level, social relationship, and their relationship to the serene facets of their environment.5 Patients’ assessment of their quality of life in relation to health often differs markedly from that of health care professionals. Therefore, patient-based assessment of health status is very important for health measurement. The questionnaire that is often used to assess oral health-related quality of life (OHRQoL) is the oral health impact profile-14 (OHIP-14). OHIP-14 is a questionnaire that contains seven different dimensions (functional limitations, physical discomfort, psychological discomfort, physical disability, psychological disability, social disability, and handicaps). All of these dimensions contain two questions each that define OHRQoL.6
Oral lesions can affect the OHRQoL of HIV/AIDS patients, which remains a problem that attracts the attention of health professionals.5,7 Oral lesion infections seen in HIV infection include bacterial infections, fungal infections other than candida, and reactions to drugs.1,8–10 Bajomo (2014) reported that pseudomembranous candidiasis, erythematous candidiasis, and linear gingival erythematosus (LGE) are significantly correlated with poorer quality of life. Those who have necrotizing ulcerative gingivitis (NUG) tend to have a worse OHRQoL, compared to those who do not have these oral lesions.11
The aim of this study was to assess the association between oral mucosal lesions and oral health-related quality of life (OHRQoL) as measured by the validated Indonesian version of the oral health impact profile-14 questionnaire (OHIP-14) among people living with HIV/AIDS (PLWHA).
Materials and Methods
A cross-sectional method was conducted on 110 people living with HIV/AIDS, selected using consecutive sampling. The inclusion criteria encompassed HIV/AIDS patients aged 18 years and above, who possessed an understanding of Indonesian. The exclusion criteria included HIV/AIDS patients with severe immune system conditions, other serious disorders, or mental health issues, who were unable to cooperate in completing the questionnaire and undergoing oral examinations. Additionally, patients unwilling to participate in the study and those with incomplete medical records data were also excluded. Before undergoing examination and interviews, the research participants formally consented to their involvement by signing a consent form. Subsequently, an oral cavity examination was conducted for each respondent to identify the presence of oral lesions, utilizing a diagnostic tool. Additionally, thorough documentation of observed oral lesions was performed.
To measure the oral health-related quality of life (OHRQoL), the oral health impact profile (OHIP-14) index, which includes seven dimensions consisting of 14 questions, was used. Each dimension consists of two questions using a Likert scale. The categories for each question are as follows: 0 = never, 1 = very rarely (once a month), 2 = sometimes (twice a week), 3 = often (every day), 4 = very often (several times a day). The total score is 56. A higher score indicates a lower quality of life in relation to oral health. The OHRQoL category division is based on the calculation of the score interval between the highest and lowest scores, namely: Good = 0–18, Moderate = 19–37, and Poor = 38–56.
The data collection process comprised two stages. Initially, the questionnaire was adapted, and its validity and reliability were tested in the first stage. Subsequently, the second stage involved collecting data from the research subjects using the previously validated OHIP-14 questionnaire. During the adaptation stage, two certified sworn translators with diverse backgrounds conducted the initial translation from English to Indonesian. Then, the results were consolidated into a comprehensive translation referred to as the initial questionnaire. Subsequently, the initial questionnaire underwent retranslation into English by two translators. The outcomes were further discussed with the oral medicine team, leading to the development of the final Indonesian version of OHIP-14 before undergoing validation.
Afterward, a test of the validity and reliability of the final questionnaire was carried out on 30 respondents. The external testing of the validity of the OHIP-14 questionnaire in Indonesian was carried out by calculating the correlation coefficient using the point biserial correlation (rcount ≥ rtable), while the internal reliability testing was carried out by calculating the Kuder-Richardson Formula 20 (KR-20), reliable if KR-20 ≥ 0.6, and the external reliability analysis was done using kappa agreement to assess the extent to which the questionnaire can provide consistent and reliable results, and to measure the level of agreement between raters in interpreting questions or statements in the questionnaire.12 The validity test was carried out by correlating each item in a variable with its total score. The resulting correlation value would be tested with the rtable value to see whether each instrument is valid or not. The value of rtable was determined by α = 0.05 and n-2 degree of freedom. With a sample size of n = 30, the value of rtable = 0.189 was obtained. Furthermore, the reliability test was carried out to ascertain whether the instrument used was reliable or not, with the meaning of reliable being that if the instrument is tested repeatedly, the results will be the same.13 For reliability testing, Cronbach’s alpha technique was used. The value of Cronbach’s alpha is to see whether the instrument is reliable or not. If it is found that Cronbach’s alpha value is greater than 0.7, then the entire instrument is said to be reliable.
The second stage was the data collection, which was carried out at the Teratai Clinic, Dr. Hasan Sadikin Central General Hospital, with the following stages: the subjects were given an explanation of the method, aims, and objectives of the research, then the patients who were willing to be the research sample signed informed consent. Anamnesis and intra-oral examination were carried out to see the condition of the found oral lesions; interviews were conducted by filling out a questionnaire regarding 14 questions of the OHIP-14 questionnaire whose validity and reliability had been tested.
Testing the validity of the OHIP-14 in Indonesian was carried out by calculating the value of the inter-item correlation coefficient (rcount ≥ rtable) and reliability testing was carried out by calculating Cronbach’s alpha (α≥0.7) and kappa coefficient agreement analysis. The association between oral mucosal lesions and OHRQoL was analyzed using the chi-squared test.
Results
The study was started by testing the validity of the questionnaire on 30 respondents to measure the high level of accuracy and consistency of the research instruments used in data collection. From the results of the validity analysis, it was found that all 14 items of the OHIP-14 questionnaire produced a value of rcount >0.189, meaning that all question items are valid and can be used to describe the oral health-related quality of life (OHRQoL) (Table 1). The results of the OHIP-14 questionnaire reliability test showed a Cronbach’s alpha value of 0.960 (> 0.7), which means that overall, the OHIP-14 questionnaire is reliable and feasible to be used to assess the OHRQoL.
 |
Table 1 Validity Test Results |
The study subjects consisted of 68 men and 42 women. The age group with the highest number was18 to 29 years comprising 41 people, while the lowest was the age group of ≥ 50 years with five people, and the majority of them (59.1%) had been taking antiretrovirals (ARV) (Table 2).
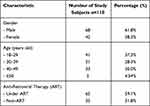 |
Table 2 Characteristic of the Study Subjects |
Oral manifestations of HIV/AIDS found include acute pseudomembranous candidiasis, erythematous candidiasis, hyperpigmentation, median rhomboid glossitis, angular cheilitis, linear gingival erythema, oral hairy leukoplakia, recurrent intraoral herpes, recurrent aphthous stomatitis, cytomegalovirus (CMV) ulcers, and Stevens-Johnson syndrome (SJS). The statistical analysis results showed that there was a relationship between the present of oral lesions and OHRQoL (p<0.05). As many as 81.5% of people with oral lesions had a good OHRQoL, 13% had a moderate OHRQoL and 5.6% had a poor OHRQoL, while 100% of those without oral lesions had a good OHRQoL (Table 3). Furthermore, the results of the chi-squared test analysis revealed that acute pseudomembranous candidiasis, angular cheilitis, recurrent intraoral herpes, and Stevens-Johnson syndrome were significantly related to OHRQoL, while no statistically significant association was observed for other types of oral lesions (Table 4).
 |
Table 3 Analysis of the Association Between the Presence/Absence of Oral Lesions and Oral Health-Related Quality of Life |
 |
Table 4 Association Between Oral Lesions and Quality of Life |
Discussion
The current study initiated by conducting validity and reliability tests on the OHIP-14 questionnaire, comprising 14 questions administered to 30 respondents. The validity was established through point biserial correlation analysis, demonstrating good internal reliability. The external reliability test also confirmed the questionnaire’s suitability for assessing responses in PLWHA. Previous studies in various countries, conducted by Mohamed et al, Rovaris et al, and Liberali et al, utilized the OHIP-14 questionnaire, also demonstrating valid results in assessing the quality of life among HIV patients.7,14,15
During clinical examinations, HIV patients on antiretroviral therapy (ART) exhibited various oral mucosal lesions, including oral hyperpigmentation, recurrent aphthous stomatitis, and recurrent intraoral herpes. This finding aligns with a previous study that also identified oral lesions, including oral hyperpigmentation and aphthous stomatitis in HIV patients on ART.16 Meanwhile, among HIV patients who were not on ART, observed oral lesions included oral candidiasis, linear gingival erythematous, and oral hairy leukoplakia (OHL). In line with prior research by Batavia et al, the most prevalent oral lesions in people living with HIV and not on ART were acute pseudomembranous candidiasis, oral hairy leukoplakia, and recurrent intraoral herpes.17
The research findings revealed that among HIV patients with oral mucosal lesions, most of them had a good OHRQoL, however we found 13% patients had a moderate OHRQoL and 5.6% patients had a poor OHRQoL. Conversely, all HIV patients without oral lesions showed a good OHRQoL. Acute pseudomembranous candidiasis, angular cheilitis, recurrent intraoral herpes, and Stevens-Johnson syndrome were identified as statistically significant types of oral lesions. The presence of oral lesions correlated with symptoms such as pain, discomfort, functional limitations, and dissatisfaction with appearance, collectively impacting the overall quality of life for affected patients.14,18,19
Acute pseudomembranous candidiasis, commonly known as oral thrush, can lead to discomfort, burning sensations, and a disturbed sense of taste, altering the perception of food and reducing appetite. Additionally, it may impact the swallowing process, causing difficulties in chewing and speaking, ultimately affecting the patient’s quality of life. This aligns with other findings which also identified pseudomembranous candidiasis as an oral lesion with significant implications for the patient’s quality of life.11,20
Recurrent intraoral herpes, while not directly linked to HIV infection, exhibits recurrent characteristics and can cause pain, impacting patients physically, psychologically, and socially, thereby reducing their overall quality of life. This observation aligns with a study by Rovaris et al, which also identified herpes simplex infections as commonly found lesions with similar implications.4,14
Stevens-Johnson syndrome is recognized as a delayed-type hypersensitivity reaction to drugs, manifesting as severe and life-threatening mucocutaneous diseases characterized by erythematous macules, hemorrhagic erosions, painful ulcers, blisters, and detachment of both the epidermis and mucous membrane.21,22 Previous studies have highlighted a higher incidence of SJS among HIV-infected individuals, contributing to increased rates of mortality and morbidity.23,24 Moreover, others studies indicated that SJS may lead to high rates of long-term sequelae, impacting both the physical and mental health and affecting the quality of life for survivors. The findings underscore the importance of raising awareness regarding these effects among SJS survivors.12,13
This study has some limitations. Firstly, the use of a cross-sectional design inherently comes with methodological limitations. Further research should explore the QoL of PLWHA exhibiting significant signs of disease, whether current or past. Additionally, it is essential to assess the correlation between the OHRQoL and various risk factors of oral manifestations of HIV/AIDS, such as the degree of immunosuppression, smoking, alcohol consumption, oral hygiene, poor dietary intake, psychological factor, mode of HIV transmission, and comorbidities.
Conclusion
The findings of this study demonstrated a statistically significant association between oral mucosal lesions and the oral health-related quality of life in HIV/AIDS patients, emphasizing the importance of considering oral health within the broader context of overall well-being. Additionally, the use of the OHIP-14 questionnaire in this study affirmed the validity and reliability of the Indonesian version, establishing it as an effective tool for assessing the OHRQoL among people living with HIV/AIDS. Future research should aim to explore the specific impact of various oral mucosal lesions and their associated risk factors on the quality of life of people living with HIV/AIDS.
Abbreviations
AIDS, acquired immunodeficiency syndrome; ART, antiretroviral therapy; CMV, cytomegalovirus; HIV, human immunodeficiency virus; KR-20, Kuder-Richardson formula 20; LGE, linear gingival erythematosus; NUG, necrotizing ulcerative gingivitis; OHIP-14, oral health impact profile-14; OHR-QoL, oral health-related quality of life; OHL, oral hairy leukoplakia; PLWHA, people living with HIV/AIDS; QoL, quality of life; SJS, Stevens-Johnson syndrome; WHO, world health organization.
Data Sharing Statement
The data used in the current study are available from the corresponding author upon reasonable request.
Ethical Clearance and Consent to Participant
This study was conducted in accordance with the Declaration of Helsinki. Ethical approval was obtained from the Research Ethics Commission of Universitas Padjadjaran No. 1361/UN6.KEP/EC/2019. In addition, written informed consent was obtained from all study participants. Confidentiality of the acquired information was ensured through the use of code numbers instead of the participants’ name or identification number.
Acknowledgment
The authors would like to thank the staffs at Teratai Clinic, Dr. Hasan Sadikin Central General Hospital, Bandung, Indonesia, for their kind assistance.
Disclosure
The authors report no conflicts of interest in this work.
References
1. Tappuni AR. The global changing pattern of the oral manifestations of HIV. Oral Dis. 2020;26(S1):22–27. doi:10.1111/odi.13469
2. Sharma G, Oberoi SS, Vohra P, Nagpal A. Oral manifestations of HIV/AIDS in Asia: systematic review and future research guidelines. J Clin Exp Dent. 2015;7(3):e419–e427. doi:10.4317/jced.52127
3. Umeizudike KA, Osagbemiro BB, Daramola OO, Adeyemo TA. Oral health related quality of life among HIV positive patients attending two HIV outpatient clinics in Nigeria - a cross sectional study. Afr Health Sci. 2021;21(2):566–575. doi:10.4314/ahs.v21i2.11
4. Lomelí-Martínez SM, González-Hernández LA, de Ruiz-Anaya AJ, et al. Oral Manifestations Associated with HIV/AIDS Patients. Medicina. 2022;58(9):1214. doi:10.3390/medicina58091214
5. Bennadi D, Reddy CVK. Oral health related quality of life. J Int Soc Prev Community Dent. 2013;3(1):1–6. doi:10.4103/2231-0762.115700
6. Campos LA, Peltomäki T, Marôco J, Campos JADB. Use of oral health impact profile-14 (OHIP-14) in different contexts. What is being measured? Int J Environ Res Public Health. 2021;18(24):13412. doi:10.3390/ijerph182413412
7. Mohamed N, Saddki N, Yusoff A, Mat Jelani A. Association among oral symptoms, oral health-related quality of life, and health-related quality of life in a sample of adults living with HIV/AIDS in Malaysia. BMC Oral Health. 2017;17(1):1–11. doi:10.1186/s12903-017-0409-y
8. Denny CE, Ramapuram J, Bastian TS, Ongole R, Binnal A, Natarajan S. Oral lesions in HIV/AIDS patients on highly active antiretroviral therapy. World J Dent. 2016;7(2):95–99. doi:10.5005/jp-journals-10015-1373
9. Rosa DE, Sufiawati I. Case Series of HIV-associated oral lesions among antiretroviral-naive patients during the COVID-19 pandemic. Int Med Case Rep J. 2023;16:73–82. doi:10.2147/IMCRJ.S398736
10. Novianti Y, Sufiawati I. Clinical assessment and management in improving the quality of life of HIV/AIDS patients with oral candidiasis: a case series. HIV AIDS. 2023;15:683–696. doi:10.2147/HIV.S434175
11. Bajomo AS, Ayo-Yusuf OA, Rudolph MJ, Tsotsi NM. Impact of oral lesions among South African adults with HIV/AIDS on oral health-related quality of life. J Dent Sci. 2013;8(4):412–417. doi:10.1016/j.jds.2013.04.011
12. Hoffman M, Chansky PB, Bashyam AR, et al. Long-term physical and psychological outcomes of Stevens-Johnson syndrome/toxic epidermal necrolysis. JAMA dermatol. 2021;157(6):712–715. doi:10.1001/jamadermatol.2021.1136
13. Cekic S, Canitez Y, Yuksel H, et al. A comprehensive assessment of long-term complications in patients with Stevens-Johnson syndrome and toxic epidermal necrolysis. Int Arch Allergy Immunol. 2023;184(10):994–1002. doi:10.1159/000531366
14. Rovaris NS, Galato D, Schuelter-Trevisol F, et al. Oral health status and its impact on the quality of life of children and adolescents living with HIV-1. BMC Res Notes. 2014;7(1):1–7. doi:10.1186/1756-0500-7-478
15. Liberali SA, Coates EA, Freeman AD, Logan RM, Jamieson L, Mejia G. Oral conditions and their social impact among HIV dental patients, 18 years on. Aust Dent J. 2013;58. doi:10.1111/adj.12031
16. Mary EO, Abiola OA, Titilola G, Mojirayo OO, Sulaimon AA. Prevalence of HIV related oral lesions in people living with HIV and on combined antiretroviral therapy: a Nigerian experience. Pan Afr Med J. 2018;31:1–10. doi:10.11604/pamj.2018.31.180.13574
17. Batavia AS, Secours R, Espinosa P, Jean Juste MA, Severe P, Pape JW. Diagnosis of HIV-associated oral lesions in relation to early versus delayed antiretroviral therapy: results from the CIPRA HT001 trial. PLoS One. 2016;11. doi:10.1371/journal.pone.0150656
18. Villanueva-Vilchis M-C, López-Ríos P, García I-M, Gaitán-Cepeda L-A. Impact of oral mucosa lesions on the quality of life related to oral health. An etiopathogenic study. Med Oral Patol Oral Cir Bucal. 2016;21(2):e178–e184. doi:10.4317/medoral.20866
19. Zucoloto ML, Maroco J, Campos JADB. Impact of oral health on health-related quality of life: a cross-sectional study. BMC Oral Health. 2016;16(1):2–7. doi:10.1186/s12903-016-0211-2
20. Hosain Pour A, Salari S, Ghasemi Nejad Almani P. Oropharyngeal candidiasis in HIV/AIDS patients and non-HIV subjects in the Southeast of Iran. Curr Med Mycol. 2018;4(4):1–6. doi:10.18502/cmm.4.4.379
21. Hasegawa A, Abe R. Recent advances in managing and understanding Stevens-Johnson syndrome and toxic epidermal necrolysis [version 1; peer review: 2 approved]. F1000Research. 2020;9(612). doi:10.12688/f1000research.24748.1
22. Lerch M, Mainetti C, Terziroli Beretta-Piccoli B, Harr T. Current perspectives on Stevens-Johnson syndrome and toxic epidermal necrolysis. Clin Rev Allergy Immunol. 2018;54(1):147–176. doi:10.1007/s12016-017-8654-z
23. Knight L, Muloiwa R, Dlamini S, Lehloenya RJ. Factors associated with increased mortality in a predominantly HIV-infected population with Stevens Johnson syndrome and toxic epidermal necrolysis. PLoS One. 2014;9(4):e93543. doi:10.1371/journal.pone.0093543
24. Chateau AV, Dlova NC, Dawood H, Aldous C. Outcomes of Stevens–Johnson syndrome and toxic epidermal necrolysis in HIV-infected patients when using systemic steroids and/or intravenous immunoglobulins in Pietermaritzburg, South Africa. South Afr J HIV Med. 2019;20(1):1–8. doi:10.4102/sajhivmed.v20i1.944
 © 2024 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2024 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
