Back to Journals » International Journal of Women's Health » Volume 16
Survival Status and Predictors Among Women with Advanced Stage of Cervical Cancer
Authors Teshome R , Yang I, Woldetsadik E, Girma E, Higgins M, Wells J
Received 16 December 2023
Accepted for publication 20 March 2024
Published 15 April 2024 Volume 2024:16 Pages 605—617
DOI https://doi.org/10.2147/IJWH.S455235
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Professor Elie Al-Chaer
Roza Teshome,1 Irene Yang,2 Edom Woldetsadik,3 Eshetu Girma,4 Melinda Higgins,2 Jessica Wells2
1Department of Midwifery, School of Nursing & Midwifery, College of Health Sciences, Addis Ababa University, Addis Ababa, Ethiopia; 2Nell Hodgson Woodruff School of Nursing, Emory University, Atlanta, GA, USA; 3Department of Oncology, School of Medicine, College of Health Sciences, Addis Ababa University, Addis Ababa, Ethiopia; 4Department of Preventive Medicine, School of Public Health, College of Health Sciences, Addis Ababa University, Addis Ababa, Ethiopia
Correspondence: Roza Teshome, Tel +251-911028610, Email [email protected]
Background: Cervical cancer is one of the leading causes of cancer death in women, even though it is a preventable disease. Most deaths occur in low- and middle-income countries. In addition to early detection and receipt of standard treatments, survivorship is an important component of high quality of care across the cancer continuum.
Objective: To assess the survival status of advanced-stage cervical cancer patients after cancer treatment has started.
Methods and Materials: A one-year prospective cohort study was employed to assess the survival status of women with advanced stages of cervical cancer. A total of 180 cervical cancer patients were recruited, and the study was conducted from January 10, 2022, to September 20, 2023. Data entry and analysis were done in the SPSS 29 version. Descriptive statistics were used to examine participant characteristics. The Kaplan-Meier procedure and log rank test were used to estimate the duration of survival. Bivariate and multivariate Cox regression analyses were computed for predictor variables with survival status.
Results: Patients receiving cancer treatment at FIGO stages IVA and IVB had survived by 56% and 24%, respectively, whereas patients receiving treatment at stages IIB and IIIA had survived by 100%. The estimated mean survival time at one-year follow-up was 5.706 months (95% CI: 3.785– 7.627) for patients with FIGO stage IVB, but 11.537 months (95% CI: 11.199– 11.887) for those with stages II and III (P < 0.001). Women over 60 years old had a 1.5-fold higher risk of death than those under 60 (HR: 1.482, P = 0.040).
Conclusion: The one-year cumulative survival rate among advanced-stage cervical cancer patients was 77%. Major factors associated with survival were age, cancer stage, the presence of anemia, and waiting time for treatment.
Keywords: survival status, advanced stage, cervical cancer, tikur anbessa specialized hospital, Ethiopia
Background
Globally, there were over 342,000 deaths and over 604,000 new cases of cervical cancer in 2020.1 The effects of cervical cancer vary depending on the region; evidence indicates that over 85% occurs in low- and middle-income countries.2 Sub-Saharan Africa has the greatest regional incidence and mortality rates, with higher rates in Eastern, Southern, and Middle Africa.1 Ethiopia is likewise confronting a significant cervical cancer burden.3 Ethiopia is expected to have 15,300 new cases of cervical cancer by 2040, up from the anticipated 7,500 occurrences in 2020. Similarly, on an annual basis, the disease’s death toll will rise from 5340 in 2020 to 11,000 in 2040.4
The main factor contributing to cervical precancerous lesions and cancer is persistent human papillomavirus infection.5 Adenocarcinomas, which occur in the glandular columnar layer of the endocervix, account for 10% of cervical cancer cases. Squamous cell tumors, which mostly affect the transformation zone of the ectocervix, account for 90% of cervical cancer cases.6
Worldwide cervical cancer survival rates vary and are often associated with the level of country development.7 Additionally, cervical cancer survival rates vary by race and subregion throughout the African continent. Tumor stage, histology, geographic location, and access to high-quality healthcare all affect survival rates.8 The tumor stage is the main indicator of the prognosis for cervical cancer. The International Federation of Gynecology and Obstetrics (FIGO) staging system for tumors is associated with overall survival and the probability of recurrence.9
The majority of patients in developing countries, such as Ethiopia, present late and have advanced stages of cancer. Their prognosis is significantly worse and may require a combination of treatments, such as radiation, chemotherapy, and surgery. Surgery is the main treatment for cervical cancer at stage IIA or lower, whereas chemo-radiation is used to treat the cancer when it has progressed to stage IIB or above.10
Survival studies measure the overall performance of a group of patients in terms of quality and quantity of life after diagnosis or treatment. Survivorship care is a critical part of providing high-quality care for patients at all stages of the cancer continuum, in addition to early diagnosis and standard treatments.11 In Ethiopia, several studies are related to screening and risk factors for cervical cancer. In Ethiopia, survival studies are beginning to emerge but are limited by retrospective design. Little is known about survival status after cancer treatment starts. This study aimed to assess the survival status of advanced-stage cervical cancer patients after cancer treatment had started.
Methods and Materials
Study Design and Sample
A prospective cohort study was employed to assess the survival status of women with advanced stages of cervical cancer. It was carried out at the Tikur Anbessa Specialized Hospital Oncology Centre, located in Ethiopia’s capital city of Addis Ababa. Approximately 400,000 in-patients and out-patients receive diagnosis and treatment annually from Tikur Anbessa Specialized Hospital (TASH), the largest referral hospital in Ethiopia. TASH’s oncology center offers radiation therapy, chemotherapy, and other supportive and palliative medical services. A total of 180 patients with advanced stages of cancer were recruited.
Recruitment and Baseline Data Collection
At the onset of cancer treatment, 180 patients with histologically confirmed cervical cancer were enrolled in consecutive manner between January 10, 2022, and September 20, 2022. During the recruitment, baseline information on sociodemographic characteristics, reproductive history, pathological and clinical characteristics, treatment start date, diagnosis date, and co-morbidities was collected through interviews and from the patient’s chart. Participants were interviewed after one year from the date of enrollment by telephone. In cases of death, the patient’s husband or relatives were contacted. The last interview was conducted on September 20, 2023.
Data Analysis
Data entry and analysis were done using SPSS version 29.12 Descriptive statistics were used to examine participant characteristics. Kaplan-Meier procedure and Log rank test were used to estimate the duration of survival. Bivariate and multivariate Cox regression analyses were computed for predictor variables with survival status. Predictor variables with a significance level of 0.25 were included in a multivariate Cox proportional hazard model. Both the crude hazard ratio (CHR) and the adjusted hazard ratio (AHR) were used to determine predictor variables, with confidence levels set at 95% and statistical significance at a p-value less than 0.05. The event was defined as the “death of cervical cancer patients”, and the censored group was defined as “patients who survived until the end of the cohort period” and “patients who are lost to follow-up”.
Results
Socio-Demographic Characteristics and Reproductive Health History
A total of 180 advanced-stage cervical cancer patients were enrolled to follow their survival status one year after beginning treatment. Of these, 51.1% were between the ages of 45 and 59, and 28.3% were older than 60. Half of them had no formal schooling. The majority were housewives (Table 1).
 |
Table 1 Socio-Demographic Characteristics of Participants |
For 32.2% of the participants, the age of their first sexual contact was under 15 years, and for 36.1% of the participants, the age of their first marriage was between 9 and 15 years old. For the majority of participants, the age range for their first pregnancy was 15 to 19 years (Table 2).
 |
Table 2 Reproductive History and Clinical Characteristics of Participants |
Clinical Characteristics
Out of all the participants, 49.4% began cancer treatment within 1–6 months of the date of diagnosis, while 19.4% waited longer than 12 months to begin cancer treatment. From the total participants, most of them were treated with radiotherapy (n = 62) and chemotherapy (n = 88) treatments. Eleven, however, died while waiting for treatment, and three did not begin treatment until the end of this study. The 14 patients who did not receive cancer treatment were not included in the survival analysis. Anemia was present in 10.2% of cases, while HIV/AIDS was present in 12% of cases. Treatments with radiation and chemoradiotherapy were 34.4% and 48.9%, respectively. The vast majority of participants were in FIGO stages III and IV (Table 2).
Survival Status
Following their enrollment, 180 patients in FIGO stages IIB to IVB were followed for a year. Of these, 14 did not receive cancer treatment. There were 49 deaths overall. Additionally, seven participants were censored because they were lost to follow-up.
Out of 166 people who received cancer treatment, overall survival was achieved by 77% (Table 3; Figure 1). Patients at FIGO stages IVA and IVB survived by 56% and 24%, respectively, by the end of the one-year follow-up period, whereas patients at stages IIB and IIIA survived by 100% (Table 4).
 |
Table 3 Life Table After Cancer Treatment Started Among Advanced Stage of Cervical Cancer Patients |
 |
Table 4 Survival Time of Cervical Cancer Patients After Treatment by FIGO Stage |
In FIGO stage IVB, the cumulative one-year survival rate was 24%, while in stage IIB, it was 94%. At one-year follow-up, the estimated mean survival time for patients with FIGO stage IVB was 5.706 months (95% CI: 3.785–7.627), but for patients with stage II and III, it was 11.537 months (95% CI: 11.199–11.887) (P < 0.001) (Table 5) and (Figure 2).
 |
Table 5 Estimated Mean Survival Time in Months and Cumulative One-Year Survival by Socio-Demographic and Clinical Characteristics |
 |
Figure 2 Kaplan-Meier survival curve according to FIGO staging. |
Patients with anemia had an estimated mean survival time of 7.235 months (5.248–9.222), which is significantly (P < 0.001) less than those without anemia, who had an estimated mean survival time of 10.926 months (95% CI: 10.411–11.441). (Table 5) (Figure 3).
 |
Figure 3 Kaplan-Meier survival curve according to comorbidity. |
The cumulative one-year survival of patients who did not receive treatment was 21%. The estimated mean survival time among patients who did not receive cancer treatment was 6.786 months (95% CI: 4.844–8.727), which is significantly less than patients who received cancer treatment (P = 0.002) (Table 6, Figure 4).
 |
Table 6 Cox Regression Model for Factors Associated with Survival Status Among Patients with Advanced Stage Cervical Cancer |
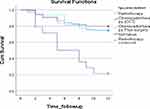 |
Figure 4 Kaplan-Meier survival curve according to type of cancer treatment. |
Among patients over 60 years, the estimated mean survival time was 9.240 months (95% CI: 8.211–10.269), and the cumulative one-year survival rate was 60%, which is significantly lower than that of the other age groups (Table 5, Figure 5).
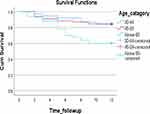 |
Figure 5 Kaplan-Meier survival curve according to age. |
Predictors of Survival Status
Age, cancer stage, comorbidities, treatment waiting time, and receiving cancer treatment were found to be the important factors linked with survival status in both univariate and multivariate Cox regression models.
A statistically significant correlation was found (P = 0.028) between participant age and survival, as determined by the chi-square test (Table 1). There was a 1.5-fold risk of death difference between women over 60 and those under 60 (HR: 1.482, P = 0.040) (Table 6).
A significant association between the presence of comorbidity and survival status was identified among patients with cervical cancer (P < 0.001) (Table 2). Compared to women without anemia, anemic women had over four times the increased risk of dying (HR: 2.389, P = 0.038) (Table 6).
Discussion
The main objective of this study was to prospectively assess the precise one-year survival status of advanced stage cervical cancer patients following the initiation of cancer treatment. Overall, 77% of patients survived their first year following cancer treatment, according to this study. Similarly, 74% of 1-year survivors were reported in a multi-national population study involving seven sub-Saharan nations.13 A study conducted in Uganda reported a one-year survival rate of 78.5% among patients who did not get radiotherapy. This may be due to the study design which included patients at all stages.14 An earlier study, conducted in Ethiopia ten years ago, found that the one-year survival rate for patients treated with radiation therapy and/or surgery was 90.4%, a significantly higher rate than the current study. This variation may be due to fact that all cancer stages were included.15 Similar to this, a previous retrospective study carried out in Ethiopia found that one-year survival rate was 92.11%, much higher than our findings. This discrepancy may be explained by the patients’ cancer stages, the study period, or different study designs.16 On the other hand, a substantially lower one-year survival rate 58.6% was reported in a Zimbabwean study involving patients who did not get treatment.17
The survival rate for women over 60 is significantly lower than that of women under 60. This is inconsistent with studies conducted in Brazil18 and Netherlands19 which identified no association between age and survival status. The inconsistency may be explained by the fact that the majority of the patients in these studies received curative therapies. On the other hand, there are plenty of studies that revealed that the significancy association between age and survival.14,16,20–26
The present study showed that survival status is highly affected by stage of cancer. This is supported by many articles.14–16,26,27 Our study adds to the evidence pointing to the need for low- and middle-income countries to develop systems that encourage early cancer diagnosis in order to increase population-level survival.28 A systematic review and meta-analysis showed that prevalence of late-stage presentation among cervical cancer patients in Africa was 62.60% (95% CI 54.83–70.37).29 In Ethiopia, the majority of cervical cancer patients still appear at advanced stages of the disease. One of the most significant prognostic factor is stage at diagnosis, which links early detection with greater odds of survival.15,18,30 One study conducted in Ethiopia found that longer patient intervals (the time interval between the date the patient noticed the first symptom and the date of the biopsy report) are associated with more advanced FIGO-stages at diagnosis. Rural women typically have longer patient intervals. This could be due to a lack of knowledge about cervical cancer and the symptoms that go along with it, or it could be because rural areas of the nation lack access to quality healthcare and medical professionals.30 Furthermore, another study conducted in Ethiopia showed that the primary cause of cervical cancer diagnosis at an advanced stage is non-engagement in care or screening.31
Our study revealed that not receiving cancer treatment and having to wait longer for treatment had a higher risk of death. This finding is comparable to others studies.25,32,33 According to international guidelines, radiation therapy for cervical cancer should begin within 60 days of the diagnosis being confirmed for optimal care and outcomes.34,35 Waiting time for treatment is linked to poor survival and tumor growth. The consequence of disease progression to later stages while awaiting radiation therapy is a higher number of women entering palliative care, which is associated with a high cost of care, poor quality of care, and lower survival rates.36–38
A key finding in our study is the association between survival status and the presence of anemia. Anemia increased the risk of death in both univariate and multivariate regression analyses. This finding is supported by other articles.16,25,27,39 Patients with cervical cancer may have anemia for a variety of reasons, including bleeding from the tumor, tumor invasion of the bone marrow, tumor-induced malnutrition, aberrant iron metabolism, impaired renal function, and compromised bone marrow function.40 The effectiveness of treatment, particularly radiotherapy, appears to be directly impacted by low hemoglobin levels. This is likely because reduced tissue oxygenation results in a reduction in radiosensitivity.41
In our study, HIV, however, was not significantly associated after controlling for age and stage of cancer in multivariate analysis. While some studies have reported an association between HIV/AIDs and survival25,42,43 findings from other studies in Uganda and Ethiopia align with ours.14,39 HIV is thought to increase the incidence of cervical cancer mainly by raising the chance of getting the first precancerous lesion due to a decreased ability to clear high-risk HPV infections and the necessary infection of cervical basal cells.44,45 However, it is unlikely that these mechanisms will have an impact on survival once the cancer develops.46
Limitation, Strengthen and Recommendations
Some limitations were observed in this study. First, the investigation was limited to a one-year follow-up period, preventing comparisons or discussions beyond the one-year survival rate. Additionally, few participants in this cohort study did not receive or complete cancer treatment, necessitating their exclusion from the analysis of the overall survival rate and median survival time. On the other hand, using a prospective cohort and primary data collection is the strength of the study.
Research recommendations that include a prospective cohort and/or clinical trials are encouraged to reduce biases resulting from retrospective studies, particularly in a country like Ethiopia where there is no cancer registry. It is necessary to investigate factors related to survival in the context of Ethiopia further and to prospectively determine the accurate survival rate. In sub-Saharan Africa, there have been notable improvements in the screening, diagnosis, and treatment of cervical cancer patients; nonetheless, more work remains.47 It has been demonstrated that early identification, and screening are beneficial in low-resource environments. And, Immunization against HPV has emerged as a potential primary preventive measure.48 Ethiopia launched the HPV vaccine, a quadrivalent immunization, for the first time in 2018.3 However, because the available approach was not well-utilized, insufficient screening opportunities, patients typically appear with symptoms later-stage.15 A systematic review and meta-analysis showed that in Ethiopia, the pooled estimate of adolescents’ vaccination uptake of at least one dose of HPV vaccine was 55%. This is a low rate and indicates the significant gap comparing to the WHO plan of having 90% of girls should be fully vaccinated by the age of 15 years.
Conclusion
Due to inadequate access to effective management, particularly in low- and middle-income countries, advanced cervical cancer is one of the leading causes of cancer-related mortality among women. This study identified advanced cervical cancer survival rates and associated factors in Ethiopia. The one-year cumulative survival rate among advanced-stage cervical cancer patients was 77%. The mean time of survival after 12 months was 10.392 months. The percentages of patients who survived cancer treatment for stages IIB, IIIA, IIIB, IIIC, IVA, and IVB were 100%, 100%, 92%, 87%, 56%, and 24%, respectively. Patients who received cancer therapy had a survival rate of 70–80%, compared to 21% for those who did not. Major factors associated with survival were age, cancer stage, the presence of anemia, and longer treatment waiting times.
Data Sharing Statement
Data are available upon reasonable request from the corresponding author.
Ethical Statement
Data was collected after ethical clearance was obtained from the Institutional Review Board of Addis Ababa University College of Health Sciences (IRB) (057/21/Nursing). The study was conducted in accordance with the Declaration of Helsinki. A trained data collector verbally informed eligible patients about the objectives and purposes of the study, the benefits of the study, and the requirement of a follow-up interview one-year post-enrollment. Patients were encouraged to ask questions to clarify any issues before deciding whether to participate. Study participants were enrolled when they verbalized their willingness to participate in the study, including participation in the one-year follow-up interview, use of medical records, and possible phone contact for follow-up, and signed the informed consent form.
During the training of data collectors, ethical issues were addressed as an essential component of the research. Privacy and confidentiality were maintained by avoiding the use of identifiers and restricting data access. The principal investigator ensured that the collected raw data was kept safe and confidential, locked in a secure location with password protection implemented for all files. Names of participants were not recorded in study records, and data will be reported in a manner that preserves participant anonymity and prevents the identification or linkage of the participants with the information.
Acknowledgment
We would like to express our gratitude to the Addis Ababa University College of Health Sciences for funding this research. We want to thank all the data collectors who participated in the data collection for this research project.
Author Contributions
All authors contributed to data analysis, drafting, or revising the article, have agreed on the journal to which the article will be submitted, gave final approval of the version to be published, and agree to be accountable for all aspects of the work.
Funding
The study was funded by the Addis Ababa University College of Health Sciences.
Disclosure
The authors declared that there was no conflict of interest.
References
1. Sung H, Ferlay J, Siegel RL. et al. Global Cancer Statistics 2020: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin. 2021;71(3):209–249. doi:10.3322/caac.21660
2. Gopu1 U on systemic therapy for cervical cancer P, Febin Antony1, Sunu Cyriac2 KK& AMOD. Updates on systemic therapy for cervical cancer. JIndian J Med Res; 2022:293–302. Available from: http://www.ncbi.nlm.nih.gov/pubmed/23144490.
3. Derbie A, Mekonnen D, Nibret E, Misgan E, Maier M. Cervical cancer in Ethiopia: a review of the literature. Cancer Causes Control. 2023;34(1):1–11. doi:10.1007/s10552-022-01638-y
4. World Health Organization. Global cancer observatory Ethiopia fact Sheet. Int Agency Res Cancer. 2021;133:2020–2021.
5. Dickey BL, Coghill AE, Ellsworth GB, Wilkin TJ, Villa LL, Giuliano AR. An updated systematic review of human papillomavirus genotype distribution by cervical disease grade in women living with human immunodeficiency virus highlights limited findings from latin America. Sex Transm Dis. 2021;48(12):e248–54. doi:10.1097/OLQ.0000000000001412
6. Ferlay J, Colombet M, Soerjomataram I, et al. Estimating the global cancer incidence and mortality in 2018: GLOBOCAN sources and methods. Int, J, Cancer. 2019;144(8):1941–1953. doi:10.1002/ijc.31937
7. Sankaranarayanan R. Cancer survival in Africa, Asia, the Caribbean and Central America. Introduction. IARC Sci Publ. 2011;162:1–5.
8. Drokow EK, Fangninou FF, Effah CY, et al. Cervical cancer survival times in Africa. Front Public Health. 2022;3:10.
9. Bhatla N, Aoki D, Sharma DN, Sankaranarayanan R. Cancer of the cervix uteri: 2021 update. Int J Gynecol Obstet. 2021;155(S1):28–44. doi:10.1002/ijgo.13865
10. Oaknin A, Rubio MJ, Redondo A, et al. SEOM guidelines for cervical cancer. Clin Transl Oncol. 2015;17(12):1036–1042. doi:10.1007/s12094-015-1452-2
11. Clark TG, Bradburn MJ, Love SB, Altman DG. Survival Analysis Part I: basic concepts and first analyses. Br J Cancer. 2003;89(2):232–238. doi:10.1038/sj.bjc.6601118
12. Corporation IBM. IBM SPSS Statistics Version 29; 2023.
13. Griesel M, Parkin D, Thomssen C, Kantelhardt E. Cervical Cancer in Sub-Saharan Africa – a multinational population-based study on treatment guideline adherence. In: Kongressabstracts zur 13 Jahrestagung der Mitteldeutschen Gesellschaft für Frauenheilkunde und Geburtshilfe eV (MGFG). Georg Thieme Verlag KG; 2019.
14. Wabinga H, Ramanakumar AV, Banura C, Luwaga A, Nambooze S, Parkin DM. Survival of cervix cancer patients in Kampala, Uganda: 1995–1997. Br J Cancer. 2003;89(1):65–69. doi:10.1038/sj.bjc.6601034
15. Kantelhardt EJ, Moelle U, Begoihn M, et al. Cervical Cancer in Ethiopia: survival of 1059 Patients Who Received Oncologic Therapy. Oncologist. 2014;19(7):727–734. doi:10.1634/theoncologist.2013-0326
16. Wassie M, Argaw Z, Tsige Y, Abebe M, Kisa S. Survival status and associated factors of death among cervical cancer patients attending at Tikur Anbesa Specialized Hospital, Addis Ababa, Ethiopia: a retrospective cohort study. BMC Cancer. 2019;19(1):1. doi:10.1186/s12885-019-6447-x
17. Chokunonga E, Ramanakumar AV, Nyakabau AM, et al. Survival of cervix cancer patients in Harare, Zimbabwe, 1995–1997. International Journal of Cancer. 2004;109(2):274–277. doi:10.1002/ijc.11670
18. Do Carmo CC, Luiz RR. Survival of a cohort of women with cervical cancer diagnosed in a Brazilian cancer center. Rev Saude Publica. 2011;45(4):661–667. doi:10.1590/S0034-89102011005000029
19. Wenzel HHB, Bekkers RLM, Lemmens VEPP, Van der Aa MA, Nijman HW. No improvement in survival of older women with cervical cancer—A nationwide study. Eur J Cancer. 2021;151:159–167. doi:10.1016/j.ejca.2021.04.014
20. Vishma B, Prakash B, Kulkarni P, Renuka M. Survival and prognostic factors for cervical cancer: a hospital based study in Mysuru, India. Int J Community Med Public Heal. 2016;218:23.
21. Maranga IO, Hampson L, Oliver AW, et al. Analysis of factors contributing to the low survival of cervical cancer patients undergoing radiotherapy in Kenya. PLoS One. 2013;8(10):10. doi:10.1371/journal.pone.0078411
22. Chokunonga E, Ramanakumar AV, Nyakabau AM, et al. Survival of cervix cancer patients in Harare, Zimbabwe, 1995–1997. Int J Cancer. 2004;109(2):274–277. doi:10.1002/ijc.11670
23. Thulaseedharan JV, Malila N, Swaminathan R, et al. Survival of Patients With Cervical Cancer in Rural India. J Clin Gynecol Obstet. 2015;4(4):290–296. doi:10.14740/jcgo367w
24. Carneiro SR, De Araújo Fagundes M, Neves LMT, Da Silva Souza G, Da Conceição Nascimento Pinheiro M. Five-year survival and associated factors in women treated for cervical cancer at a reference hospital in the Brazilian Amazon. PLoS One. 2017;12(11):1–11. doi:10.1371/journal.pone.0187579
25. Seifu B, Fikru C, Yilma D, Tessema F, Brody JP. Predictors of time to death among cervical cancer patients at Tikur Anbesa specialized hospital from 2014 to 2019: a survival analysis. PLoS One. 2022;17(2 February):1–15. doi:10.1371/journal.pone.0264369
26. Jayant K, Sankaranarayanan R, Thorat RV, et al. Improved survival of cervical cancer patients in a screened population in rural India. Asian Pacific J Cancer Prev. 2016;17(11):4837–4844.
27. Khamis SI, Mrema AS, Katanga J, Lugina EL. Survival in Cervical Cancer and Its Predictors at Ocean Road Cancer Institute From January to December 2012. JCO Glob Oncol. 2021;7(7):734–739. doi:10.1200/GO.20.00616
28. Cancer Council Australia. Understanding Cervical Cancer; 2019:4–68. Available from: https://www.cancer.org.au/assets/pdf/understanding-cervical-cancer-booklet.
29. Tekalign T, Teshome M, Ekwunife OI. Prevalence and determinants of late-stage presentation among cervical cancer patients, a systematic review and meta-analysis. PLoS One. 2022;17(4):1–13. doi:10.1371/journal.pone.0267571
30. Begoihn M, Mathewos A, Aynalem A, et al. Cervical cancer in Ethiopia-predictors of advanced stage and prolonged time to diagnosis. Infect Agent Cancer. 2019;14(1):1–7. doi:10.1186/s13027-019-0255-4
31. Mattern J, Letendre I, Sibiude J, et al. Diagnosis of advanced cervical cancer, missed opportunities? BMC Womens Health. 2022;22(1):1–6. doi:10.1186/s12905-022-01668-3
32. Musa J, Nankat J, Achenbach CJ, et al. Cervical cancer survival in a resource-limited setting-North Central Nigeria. Infect Agent Cancer. 2016;11(1):0–7. doi:10.1186/s13027-016-0062-0
33. Dereje N, Addissie A, Worku A, et al. Association between waiting time for radiotherapy initiation and disease progression among women with cervical cancer in Addis Ababa, Ethiopia. Int J Cancer. 2021;149(6):1284–1289. doi:10.1002/ijc.33689
34. Koh WJ, Abu-Rustum NR, Bean S, et al. Cervical cancer, version 3.2019. JNCCN J Natl Compr Cancer Netw. 2019;17(1):64–84. doi:10.6004/jnccn.2019.0001
35. Marth C, Landoni F, Mahner S, McCormack M, Gonzalez-Martin A, Colombo N. Cervical cancer: ESMO Clinical Practice Guidelines for diagnosis, treatment and follow-up. Ann Oncol. 2017;28(Supplement 4):iv72–83. doi:10.1093/annonc/mdx220
36. Ababa A, Kantelhardt EJ, Assefa M Association between waiting time for radiotherapy initiation and disease progression among women with cervical cancer in; 2021:1284–1289.
37. Tsai CH, Kung PT, Kuo WY, Tsai WC. Effect of time interval from diagnosis to treatment for non-small cell lung cancer on survival: a national cohort study in Taiwan. BMJ Open. 2020;10(4):1–15. doi:10.1136/bmjopen-2019-034351
38. Ramey SJ, Asher D, Kwon D, et al. Delays in definitive cervical cancer treatment: an analysis of disparities and overall survival impact. Gynecol Oncol. 2018;149(1):53–62. doi:10.1016/j.ygyno.2017.12.010
39. Gizaw M, Addissie A, Getachew S, et al. Cervical cancer patients presentation and survival in the only oncology referral hospital, Ethiopia: a retrospective cohort study. Infect Agent Cancer. 2017;12(1):1–7. doi:10.1186/s13027-017-0171-4
40. Fyles AW, Milosevic M, Pintilie M, Syed A, Hill RP. Anemia, hypoxia and transfusion in patients with cervix cancer: a review. Radiother Oncol. 2000;57(1):13–19. doi:10.1016/S0167-8140(00)00245-0
41. Wassie M, Aemro A, Fentie B, Khatami F. Prevalence and associated factors of baseline anemia among cervical cancer patients in Tikur Anbesa Specialized Hospital, Ethiopia. BMC Womens Health. 2021;21(1):1–8. doi:10.1186/s12905-020-01152-w
42. Kigula-Mugambe JB, Kavuma A. Effect of HIV serological status on outcome in patients with cancer of cervix treated with radiotherapy. East Afr Med J. 2006;83(8):416–423. doi:10.4314/eamj.v83i8.9455
43. Wu ES, Urban RR, Krantz EM, et al. The association between HIV infection and cervical cancer presentation and survival in Uganda. Gynecol Oncol Reports. 2020;31:100516. doi:10.1016/j.gore.2019.100516
44. Leitao MM, White P, Cracchiolo B. Cervical cancer in patients infected with the human immunodeficiency virus. Cancer. 2008;112(12):2683–2689. doi:10.1002/cncr.23504
45. Palefsky JM, Minkoff H, Kalish LA, et al. Cervicovaginal Human Papillomavirus Infection in. J Natl Cancer Inst. 1999;91(3):226–236. doi:10.1093/jnci/91.3.226
46. Dryden-Peterson S, Bvochora-Nsingo M, Suneja G, et al. HIV infection and survival among women with cervical cancer. J Clin Oncol. 2016;34(31):3749–3757. doi:10.1200/JCO.2016.67.9613
47. Burt LM, McCormak M, Lecuru F, et al. Cervix Cancer in Sub-Saharan Africa: An Assessment of Cervical Cancer Management. JCO Global Oncology. 2021;7:173–182. doi: 10.1200/go.20.00079
48. Sankaranarayanan R, Budukh AM, Rajkumar R. Effective screening programmes for cervical cancer in low- and middle-income developing countries. Bulletin of the World Health Organization. 2001;79(10):954–962. doi: 10.1590/S0042
 © 2024 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2024 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.