Back to Journals » Patient Preference and Adherence » Volume 18
Subjective Rationalities of Nonadherence to Treatment and Vaccination in Healthcare Decision-Making
Authors Turja T , Rosenlund M , Kuusisto H
Received 13 December 2023
Accepted for publication 26 March 2024
Published 11 April 2024 Volume 2024:18 Pages 821—826
DOI https://doi.org/10.2147/PPA.S454661
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Johnny Chen
Tuuli Turja,1 Milla Rosenlund,2 Hanna Kuusisto2– 4
1Faculty of Social Sciences, Tampere University, Tampere, Finland; 2Faculty of Social Sciences and Business Studies, Department of Health and Social Management, University of Eastern Finland, Kuopio, Finland; 3Department of Neurology, Tampere University Hospital, Tampere, Finland; 4Faculty of Medicine, Tampere University, Tampere, Finland
Correspondence: Tuuli Turja, Email [email protected]
Objective: In this short report contributing to the literature on treatment and vaccination adherence, nonadherence was examined from the perspective of decision-making (DM) practice in healthcare. The objective of this study was to survey the rationalities given for treatment nonadherence and their association with DM practice.
Methods: The Ottawa decision Support Framework was used as a theoretical background for the study. Multiple choice and open-text responses indicating nonadherence were drawn from vignette survey data. The results have been analyzed and reported as descriptive statistics and findings of data-driven content analysis. The number of observatory units was 1032 in the within-subject study design.
Results: DM practice was predominantly associated with nonadherence to vaccination, whereas nonadherence to treatment was consistently associated with attitudinal reasons independent of DM practice. Nonadherence to vaccination was most often rationalized by prior negative experiences in simple DM scenarios. After other DM practices, nonadherence was rationalized by uncertainty and criticism about the benefits of the recommended vaccine. Mistrust toward healthcare providers stood out, first in treatment nonadherence generally and, second, in vaccination nonadherence after simple DM where the final decision was left to the patient.
Conclusion: In medical DM, adherence to treatment and vaccination may be achieved through a recognition of patients’ previous healthcare encounters and potential trust-related concerns, which could pose a risk for nonadherence. To be able to observe these risks, patient engagement and mutual trust should be priorities in decision support in healthcare.
Plain Language Summary: Research on treatment and vaccination adherence aim at increasing knowledge about improving adherence and treatment outcomes. This study examined explanations given for not adhering to treatment and an association between the explanations and medical decision-making practices. Decision-making practices are known to impact patient–physician interaction and the patients’ motivation to have an active role at the appointment. In a shared decision-making (SDM) practice, patients’ participation is encouraged. SDM is built on both medical expertise of the practitioner and individual views, values and preferences of the patient. As opposed to SDM, authoritarian decision-making refers to a practice in which decisions are made solely by the physician. In guided decision-making, the physician shares information with the patient but makes the final decision. In simple decision-making, the final decision is left to the patient after consultation. This empirical study used illustrated vignette survey data from Finland. Out of the 1935 respondents, 64% were female with an average age of 68. In the study design, nonadherence was presumed to depend on a decision-making practice presented. Primary findings showed that nonadherence to treatment is most correlated with attitudinal predetermination of the patient and mistrust toward healthcare providers. Nonadherence to vaccination had a stronger association with decision-making practices. After simple decision-making, declining vaccination was most often explained by prior negative experiences and mistrust toward healthcare providers. After other decision-making practices, explanations for declining included uncertainty and criticism about the benefits of the recommended vaccine. This study underscores the pivotal role of trust in the patient-physician interaction.
Keywords: decision-making, interaction, treatment adherence, trust, vaccination
Introduction
Recent studies highlight the quality of the interaction and trust between the patient and the health care professional (HCP) to support treatment adherence.1,2 This short report introduces a topical study in which treatment adherence is examined from the perspective of decision-making (DM) practice in a physician’s appointment. As the first research question, it is examined which rationalities are given for nonadherence. Subsequently, the second question explores the association between the identified rationalities for nonadherence and the DM practice.
DM practices are known to impact patient–physician interaction and the patient’s motivation at the appointment.3 The patient’s participatory role and engagement in making treatment decisions align effectively with the model where authoritarian DM is viewed against guided, simple, and shared DM.4 The authoritarian DM refers to the traditional, physician-driven practice in which decisions are made by the physician and based solely on medical knowledge. In guided DM, the physician shares information with the patient but makes the final decision. In contrast, simple DM refers to practice in which the final decision is left to the patient after consultation. Typically framed as an ideal among DM practices, shared decision-making (SDM) combines medical knowledge with patient-generated information. In SDM, the patient’s personal situation, views, and values direct the treatment decision beside the clinical expertise of the physician.4
Treatment adherence that is considered an action driven by information and attitudes, rationalities and irrationalities,1 is supported by engaging a patient in the decisions regarding their health and treatment. DM practice can support treatment adherence, but it also entails the possibility of increasing the risk of intentional nonadherence when the patient is left with concerns related to the treatment and insufficient information.1,5,6 SDM practice includes the patient by both providing information and acknowledging their active role in the DM. Consequently, SDM is acknowledged as an important and internalized part of the interaction and trust between a patient and a HCP.7,8
Trust between the patient and the HCP is essential for successful treatment1 and is viewed as constructed of three main factors: ability, benevolence, and integrity.9 In the context of treatment adherence, these factors can be understood as to how the physician is evaluated by their competence, impartiality, and morality. The Ottawa Decision Support Framework (ODSF) has been developed to support DM by guiding HCPs in assessing patients’ decisional needs, providing decision support to address these needs, and evaluating decisional outcomes. ODSF decision support interventions that address trust between HCP and the patient improve the quality of DM, which may favorably affect patients’ actions such as adhering to treatment especially in challenging DM situations.10 In this study, we aimed to evaluate, based on ODSF, the perceived decision support reflected in the rationalities for nonadherence.
Methods
Online survey data were collected in January 2022 from third-sector associations. The primary sample was collected from the Finnish Pensioners’ Federation. The invitation was sent to the members whose e-mail addresses were in the database (N = 30,329), resulting in a sample of 1740 respondents. The sample was complemented by smaller samples from the Finnish Neuro Society, the Finnish Epilepsy Association, and the Organization for Respiratory Health in Finland, resulting in a secondary sample of 195 respondents.
The study complies with the regulations of the Declaration of Helsinki. Informed consent from the participants taken at the beginning of the survey was performed in accordance with relevant guidelines and regulations, approved by The Ethics Committee of the Tampere Region, Finland (id 18/2021). The participants’ informed consent included publication of anonymized responses.
The questionnaire included illustrated vignettes presenting DM scenarios from a clinical appointment. The vignette survey study design was conducted to produce ambiguous stimuli for the respondents instead of collecting conscious evaluations of DM practices. Vignettes are used in survey studies in the medical field11 in cases where, instead of direct questions, a more projective form of study design is justified. The respondents were asked to identify with the role of the patient in repeated scenarios (see Appendix A).
The scenarios presented interactions between a physician and a patient in which the DM practice varied in four conditions: authoritarian, guided, simple, and SDM. The scenarios presenting treatment and vaccination were given in written form and were accompanied by illustrations. Each scenario ended in an apparent consensus between the physician and the patient. The respondent was asked to evaluate their intention to adhere to treatment or vaccination as recommended by the physician in a total of eight scenarios. The DM scenarios have previously been validated in a cross-examination with a standardized SDM-9 scale.
Multiple choice responses indicating nonadherence and open-text responses indicating the rationalities for nonadherence were drawn from vignette survey data. The qualitative analysis of the rationalities for nonadherence was conducted inductively following the content analysis process.12 Descriptive statistics are presented as complementary means for the data-driven content analysis.
Rationalities of Nonadherence Categorized
After the vignettes, participants indicated their intention to adhere to treatment or vaccination. In the within-subjects design, adherence to treatment was measured after each of the four treatment and four vaccination scenarios. The options were 1) unconditional adherence, 2) conditional adherence (needs more information before unconditional adherence), and 3) intentional nonadherence. In the results presented, n indicates the number of observational units, that is, the number of nonadherence responses (N = 1032).
As a follow-up question after a selection of nonadherence, the respondents were asked to give explanation to the intended nonadherence. The responses were given in free form. In a data-driven content analysis, the responses were first coded in distinct categories (Figure 1) which were later combined into fewer themes: unable to say (eg, makes the final decision later), attitude (eg, prejudice against any treatment), uncertainty (eg, unsure benefits of the treatment or the vaccination), and prior negative experiences (either personal or indirect experiences from friends and family).
 |
Figure 1 Rationalities of nonadherence: From coding categories to themes. |
Results
Among the 1935 respondents, the majority were female (64%) over 68 years old (M = 68.35; SD = 10.01). The distribution of adherence showed that adherence to treatment and vaccination were the most common responses to the scenarios. The mode of intended adherence was found in all eight scenarios, with a total percentage of 68. Conditional adherence was selected in every fourth of the scenarios. Nonadherence was selected in 7% of the cases. Tables 1 and 2 show the proportions among the coded rationalities for the treatment (n = 312) and vaccination (n = 720) scenarios separately (N = 1032).
 |
Table 1 Nonadherence to Treatment |
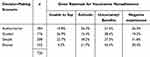 |
Table 2 Nonadherence to Vaccination |
Nonadherence to Treatment
Nonadherence to treatment was most rationalized in a manner that was coded as an attitudinal reason. The two most consistently expressed attitudes were toward the treatment and toward the healthcare provider.
Among the attitudes toward treatment, the most prevalent were mentions regarding lack of motivation when it comes to receiving treatment and especially medication: “Why are there only options for medication?” or “I don’t use medication at all”.
Among the attitudes toward a healthcare provider, a lack of trust in received information, public sector, or expertise appeared to be in question: “I would go to a private sector provider” or “I would need a specialist”.
Nonadherence to Vaccination
Vaccination scenarios were found to have more variation in subjective rationalities than treatment adherence. In the simple DM scenario, nonadherence to vaccination was mostly rationalized by prior negative experiences. Out of the negative, personal experiences, mistrust toward HCPs was emphasized. One repeated theme in the responses was the presumption that HCPs are biased because they are influenced by the pharmaceutical industry. In the following response, mistrust was associated with general recommendations that do not acknowledge individual conditions and situations:
It’s not about some stupid vaccination resistance but about my personal situation, which is not understood. I have a unique situation, but vaccinations are usually recommended for everyone. I trust my own view the most. This is built on reading information about my condition and on my bodily sensations.
Among the negative, indirect experiences that were given, the risk of vaccination was often weighed against how “a healthy individual can suffer the illnesses or diseases”, thus not needing vaccinations against them.
There are too many risks in agreeing to take vaccinations. My sister got one and now has epilepsy. I am healthy enough to endure, for example, the corona virus.
After authoritarian, guided, and SDM scenarios, nonadherence to vaccination was most often rationalized by uncertainty and criticism about the benefits of the recommended vaccine. These two dimensions came through, for example, in the open response, “I believe vaccines are ineffective”.
Discussion
Nonadherence to treatment and vaccination were studied by examining the descriptive statistics and open-text responses drawn from vignette survey data. Among the subjective rationalities of nonadherence, attitudinal rationalities were emphasized in treatment nonadherence, whereas vaccination nonadherence appeared to depend on DM practice more heavily.
Uncertainty and criticism about the benefits of the recommended vaccine was the mode in authoritarian, guided, and shared decision-making scenarios. Antecedent negative experiences emerged in simple DM leading to nonadherence to vaccination. Mistrust toward healthcare providers was used to rationalize vaccination nonadherence, particularly in cases where the final decision was left to the patient. In this simple DM practice, patients may perceive their emphasized DM role as deriving from the physician’s inability or carelessness in deciding, which leads to a lack of trust toward the physician.9 The findings are in line with prior studies in which SDM is associated with relatively high trust between HCP and the patient.7,8,13
Overall, this study supports prior findings about the importance of trust in treatment and medication adherence and contributes to the evidence of intentional nonadherence associating with patients’ reduced trust in healthcare providers.1,7–9 The findings show that nonadherence to treatment can underlie mistrust toward either received information or a healthcare provider. Furthermore, the findings are in line with the model introduced by Reach, in which trust is generated by a physician’s positive attitude.1 Patient’s trust building on the physician’s attitude emphasizes the decision-making practice as something the HCP chooses to be implemented as a part of patient-centered care.2
Scenario studies are employed when in need of a more projective study design for a questionnaire. Addressing the research question with this methodology, we sought to test if the association between DM practices and nonadherence holds in an indirect form of self-report. In addition to this study supporting the previous findings of the association between medical DM and nonadherence to vaccination, it contributes to the theory-building by emphasizing the role of trust in decision support.
As a critical note, the survey was conducted at the beginning of 2022, when the societal discussion on COVID vaccinations was vivid and opinions on the benefits and risks aroused strong feelings. This may have caused some respondents to assume that the vaccine specifically referred to the corona vaccine. However, the corona vaccination was not mentioned in the questionnaire.
Conclusion
In medical DM, adherence to treatment and vaccination can be improved by a practice in which HCPs acknowledge patients’ prior experiences and possible trust issues, which could pose a risk for nonadherence. Trust plays a pivotal role in treatment adherence and should be given greater emphasis also in the decision support provided to patients.
Acknowledgments
We would like to thank Virpi Jylhä, a participating investigator who had a major role collecting the data for this study.
Funding
This work was supported by the Strategic Research Council (SRC) established within the Academy of Finland (project numbers 31213358418 and 31213358415).
Disclosure
The authors report no conflicts of interest in this work.
References
1. Reach G. How is patient adherence possible? A novel mechanistic model of adherence based on humanities. Patient Prefer Adherence. 2023;17:1705–1720. doi:10.2147/PPA.S419277
2. Ruksakulpiwat S, Benjasirisan C, Ding K, et al. Utilizing social determinants of health model to understand barriers to medication adherence in patients with ischemic stroke: a systematic review. Patient Prefer Adherence. 2023;17:2161–2174. doi:10.2147/PPA.S420059
3. Liu Y-Q, Guo Y-L, Xu J, et al. Shared decision-making in hemophilic arthropathy rehabilitation: a qualitative study. Patient Prefer Adherence. 2023;17:249–257. doi:10.2147/PPA.S394095
4. Birkeland S, Bismark M, Barry MJ, Möller S. Is greater patient involvement associated with higher satisfaction? Experimental evidence from a vignette survey. BMJ Qual Saf. 2022;31:86–93. doi:10.1136/bmjqs-2020-012786
5. Brett J, Fenlon D, Boulton M, et al. Factors associated with intentional and unintentional non‐adherence to adjuvant endocrine therapy following breast cancer. Eur J Cancer Care. 2018;27:e12601. doi:10.1111/ecc.12601
6. Mukhtar O, Weinman J, Jackson SH. Intentional non-adherence to medications by older adults. Drugs Aging. 2014;31:149–157. doi:10.1007/s40266-014-0153-9
7. Belcher VN, Fried TR, Agostini JV, Tinetti ME. Views of older adults on patient participation in medication-related decision making. J Gen Intern Med. 2006;21:298–303. doi:10.1111/j.1525-1497.2006.00329.x
8. Matthias MS, Salyers MP, Frankel RM. Re-thinking shared decision-making: context matters. Patient Educ Couns. 2013;91:176–179. doi:10.1016/j.pec.2013.01.006
9. Mayer RC, Davis JH, Schoorman FD. An integrative model of organization trust. Acad Manage Rev. 1995;20:709–733. doi:10.2307/258792
10. Hoefel L, O’Connor AM, Lewis KB, et al. Anniversary update of the Ottawa decision support framework part 1: a systematic review of the decisional needs of people making health or social Decisions. Med Decis Making. 2020;40(5):555–581. PMID: 32659154. doi:10.1177/0272989X20936209
11. Nafees B, de Freitas HM, Beaudet A, Todd E, Gin-Sing W. A health state utility study to elicit societal values associated with pulmonary hypertension. Patient Prefer Adherence. 2023;17:2119–2130. doi:10.2147/PPA.S400061
12. Elo S, Kyngäs H. The qualitative content analysis process. J. Adv Nurs. 2008;62(1):107–115. doi:10.1111/j.1365-2648.2007.04569.x
13. Rieckmann P, Boyko A, Centonze D, et al. Achieving patient engagement in multiple sclerosis: a perspective from the multiple sclerosis in the 21st Century steering group. Mult Scler Relat Disord. 2015;4:202–218. doi:10.1016/j.msard.2015.02.005
 © 2024 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2024 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
