Back to Journals » HIV/AIDS - Research and Palliative Care » Volume 15
Sexual Coercion is Associated with HIV Risk Behavior Among Female Waiters in Jimma Town, Southwest Ethiopia
Authors Imana R, Abdullahi M, Ali R, Eyeberu A , Getachew T , Ahmed J , Mussa I , Amentie E , Wami G, Sime B, Debella A
Received 24 June 2023
Accepted for publication 3 September 2023
Published 15 September 2023 Volume 2023:15 Pages 559—570
DOI https://doi.org/10.2147/HIV.S423867
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 4
Editor who approved publication: Prof. Dr. Olubunmi Akindele Ogunrin
Regasa Imana,1 Misra Abdullahi,1 Rahima Ali,1 Addis Eyeberu,2 Tamirat Getachew,2 Jemal Ahmed,3 Ibsa Mussa,3 Eyobel Amentie,4 Girma Wami,4 Betelhem Sime,5 Adera Debella2
1School of Public Health, College of Health and Medical Sciences, Jimma University, Jimma, Ethiopia; 2School of Nursing and Midwifery, College of Health and Medical Sciences, Haramaya University, Harar, Ethiopia; 3School of Public Health, College of Health and Medical Sciences, Haramaya University, Harar, Ethiopia; 4School of Medicine, College of Health and Medical Sciences, Haramaya University, Harar, Ethiopia; 5Department of Monitoring and Evaluation, public health, Harari Regional Health Bureau, Harar, Ethiopia
Correspondence: Addis Eyeberu, 138, Dire Dawa, Harar, Ethiopia, Tel +251910005436, Email [email protected]
Background: Female waiters are at higher risk of workplace violence including sexual coercion. Even though there are numerous studies on the prevalence of sexual coercion among students, nurses, adolescents, and young pregnant women, studies on the prevalence of sexual coercion among female waiters are limited. Furthermore, there is no evidence existed that show a relationship between sexual coercion and HIV risk behavior in Ethiopia.
Purpose: The purpose of this study was to examine the relationship between sexual coercion and HIV risk behavior among female waiters in Jimma, southwest Ethiopia.
Patients and Methods: We conducted a cross-sectional survey from 1st April to 30, 2018, among 420 female waiters of reproductive age working in the licensed food and drinking establishments in Jimma town. A structured interviewer-administered questionnaire was used to collect data. Statistical analysis was conducted with SPSS version 21 statistical software. A binary logistic regression model was used to determine the association between independent variables and outcome variables.
Results: The lifetime prevalence of sexual coercion among female waiters was 71.4% (95% confidence interval: 67.1– 76.8). More than two-thirds (71.6%) of female waiters engaged in HIV-related risk behaviors. Working in the bar (AOR 4.64, 95% CI: 2.15– 10.0), being a substance user (AOR 3.37, 95% CI: 1.7– 6.7), experiencing sexual coercion (AOR 7.6, 95% CI: 3.8– 15.3) were significantly associated with HIV risk behaviors.
Conclusion: A significant number of female waiters experienced sexual coercion and engaged in HIV-risk behaviors. Workplace, substance use, and sexual coercion were significantly associated with HIV risk behavior. As a result, establishments, town health offices, and other stakeholders should work together to safeguard female waiters from the burdens of sexual coercion, HIV risk behavior, and sexually transmitted infections.
Keywords: HIV-related risk behaviors, sexual violence, sexual coercion, female waiters, southwest Ethiopia
Introduction
Nowadays, women are increasingly participating in economic activities.1,2 However, they are more vulnerable to workplace violence than men.3 Female waiters are at higher risk of workplace violence including sexual harassment, sexual coercion, and threats of violence.3,4 Sexual coercion is one type of violence that is defined as sexual interaction without mutual agreement with a person who has more authority owing to age, physical status, position, or knowledge.5 Despite the fact that various studies have been conducted on the incidence of sexual coercion among students, nurses, teenagers, and young pregnant females,6–9 There has been little research on the incidence of sexual coercion among female waiters. According to available Ethiopian data, the rate of sexual violence among female waiters is 45.9%.10
Sexual coercion is linked to a number of risky behaviors, many of which have negative health effects.11 Alcohol consumption habits, family living situations, sexual experience, and social and cultural variables all have an impact on the experience of sexual coercion.12 According to a recent study, persons who have been subjected to sexual coercion have significant levels of anxiety, sadness, suicidal thoughts, sleep disruptions, chronic illnesses, and other medical problems.13
Evidence shows that sexual coercion significantly increases HIV risk behaviors.14 Experiencing sexual coercion makes it difficult to negotiate safe sexual activities, increasing their exposure to HIV/AIDS.11 Waitresses are at risk of HIV due to the behaviors of the customers compared to the general population15 Waiters working in cafes/pastry shops/bars/hotels are also at risk of acquiring HIV due to the nature of their profession, which involves frequent interactions with new clients who are frequently searching for sexual relationships and effect of alcohol use.10,15 In 2009, the prevalence of HIV among males and females in Sub-Saharan Africa was 3.4% and 1.4%, respectively.6 The prevalence of HIV in Ethiopia shows decrement from 6.2% in 2011 to 3.3% in 2016.16 However, the trend is varying from region to region. HIV prevalence in Addis Ababa was 1.6%.17 The prevalence of HIV among students in Jimma was 12.2%.18 But HIV prevalence among the adult population was 22.1% in women and 24.3% in men.19
Despite the considerable link between sexual coercion and HIV risk behaviors, it has not been well documented among Ethiopian female waiters. Furthermore, research is focusing on students and commercial sex workers, there is a paucity of research on sexual coercion among female waiters in Ethiopia. This study would be an ideal input for policy maker to design interventions to protect this segment of the population from violence. Thus, the first goal of this study is to determine the burden of sexual coercion and HIV risk among female waiters. The second aim of this research is to determine the relationships between sexual coercion and HIV risk behavior among female waiters working in food and drinking establishments in Jimma town, Ethiopia.
Methods and Materials
Study Design, Setting, and Period
From April 1 to 30, 2018, we conducted a cross-sectional study in Jimma, a town 354 kilometers southwest of Addis Ababa. According to the Jimma Town Health Office report, the town’s total population for 2017/18 was 199,575 people, with 100,347 men and 99,229 women (of whom 43,916 are women of reproductive age). There are 25 medium clinics, 7 primary clinics, 3 NGO clinics, 8 government clinics, 4 diagnostic labs, 21 pharmacies, and 31 pharmacy stores. The town has two government hospitals (one specialized and one general), one major private hospital, and four health facilities. In the town, there are 65 hotels, 44 cafeterias, 119 restaurants, 24 bars/groceries, and 25 pensions.20
Participants
The study population consisted of all chosen female waiters aged 15–49 years who had worked in licensed food and drinking establishments in Jimma town for at least 6 months and were available at the time of data collection. Female waiters who worked at nightclubs and commercial sex workers were not included.
Sample Size and Sampling Procedure
The required sample size was calculated using single population proportion formula with the assumptions of a margin of error(d)=0.05, a confidence level of 95%=1.96, and a proportion of sexual violence (P=45.9%) from a study conducted in Bahir Dar10 and by adding 10% non-response rate, final sample size became 420.
In Jimma town, there are 119 restaurants, 24 bars, 65 hotels, and 44 cafeterias. Since it was difficult to include all of the female waiters in those establishments, we randomly selected 36 restaurants, 7 bars, 20 hotels, and 13 cafeterias. Of those establishments, we census female waiters to know the number of female waiters since their number is unknown. Then 420 female waiters were selected randomly, from 1126 female waiters. Permission was sought from the participants and selected establishment.
Data Collection Tool and Procedure
The data were collected by a face-to-face interviewer using a structured questionnaire which was adopted from the coercion experience survey and the 2017 National Youth Risk Behavior Survey.21 To guarantee consistency, the questionnaire was written in English and then translated into the local language (Afan Oromo) and back to English by a third person who is fluent in both languages. The instrument is divided into four sections: respondents’ socioeconomic factors, their experience with sexual coercion, HIV risk behavior, and their sexual health. Five diploma nurses collected data under the supervision of two BSc nurse supervisors. The data collectors were trained on how to safeguard the participants and respect their privacy. Before the commencement of the interview, consent was obtained from the participants and the establishments. A pre-test on 5% of the total sample size was performed to assure data quality. Each questionnaire was reviewed for completeness and consistency.
Measurements and Study Variables
In this study, the dependent variables were HIV risk behavior and sexual coercion. The independent variables are type of establishments, age, educational status; residency, substance use, and sexual health.
Sexual coercion was measured using composite variables of six items. The 6 questions were answered yes or no over previous months. If they answered yes to either of these six items, the respondents were deemed sexual violence victims. The items include verbal abuse, suffering annoying kissing by force or unwanted touching of private parts by force or unwanted intercourse by force or unwanted sexual intercourse after taking money/gifts/alcohol, or unwanted sexual intercourse by intimidation/shame.10
HIV risk behavior is defined as an individual’s or a partner’s activity that enhances the possibility of contracting HIV/AIDS. It is measured by composite variables of four items. The 4 questions were answered yes or no over previous months. If they answered yes to one of these four items, the respondents were deemed sexual violence victims such as alcohol consumption/substance use before the last sex, having multiple sexual partners, having intercourse in exchange for money/goods, and inconsistent condom use with a non-regular partner in the previous 12 months.
Sexual health is defined as a sexual practice that is devoid of compulsion, prejudice, and violence.
Early sex: means having sexual intercourse before the age of 18.
Food and beverage establishments: - A place where customers may get food and/or drinks. To fulfill the demands of various clientele, it may range from modest low-cost institutions to enormous high-cost structures. It was measured by asking the waitress the type of establishment.
Intergenerational sex is having heterosexual intercourse with non-marital partner 10 or more years old.
Concurrent sex partners: having sex with two or more persons within one month.
Cross-generational sex: Relationships between older men and younger women are examples of cross-generational sex. Sexual intercourse with a male partner ten or more years older vs young ladies whose partner is less than ten years older.
Data Processing and Analysis
The data were coded, recorded, and entered into EPI data version 3.1 before being exported to SPSS version 21 for data cleaning and analysis. Frequencies and summary statistics (mean, standard deviation, and percentage) were used to describe the research population in terms of relevant factors. The degree of relationship between independent and dependent factors was determined using an odds ratio with a 95% confidence interval. After bivariate logistic regression analysis, variables having a P-value of 0.25 were considered for multivariable analysis. Hosmer-Lemeshow goodness of fit was used to assess model fitness. The association was interpreted in terms of the adjusted odds ratio. The p-value of 0.05 was used to determine statistical significance.
Results
Socio-Demographic and Economic Characteristics
Of the total sample, 392 were interviewed making the response rate of the study 93.3%. Out of those, 203 (51.8%) were urban dwellers. The respondents’ mean age was 23.32 years, with a standard deviation of 2.83 years. The majority of respondents (371 (94.6%) were not married, and the vast majority (85.7%) did not ever attend school. Around 252 (64.3%) of research participants acknowledged using substances at some point in their lives. More than half of the respondents (64.3%) had an average monthly income of less than 1000 Ethiopian birr (ETB), and 147 (37.5%) of the respondents’ households have 3–5 children. (Table 1).
 |
Table 1 Socio-Demographic Characteristics of the Female Waitresses in Jimma Town, Southwest Ethiopia, 2018 |
Sexual Coercion Experience
Of the total participants, an unwanted sexual act was (67.9%), unwelcome touch was (58.9%), forced sex was (33.9%), intercourse in exchange for money or gift was (33.9%), and forced sex by intimidation was (25%) (Figure 1). Around 182 (46.4%) of participants experienced forced sexual intercourse. The most common committer of enforced sex was 92 (50.5%) by stranger, 37 (20.3%) by boyfriend, and 14 (7.7%) by teachers. The prevalence of sexual coercion experienced in the last 12 months was 242 (61.7%) (Table 2). Two hundred eighty (71.4%) female waiters experience lifetime sexual coercion. More than one-third 133 (33.9%) of female waitresses are forced at first sex.
 |
Table 2 Sexual Coercion Experience Among Female Waitresses in Jimma, Ethiopia. 2018 |
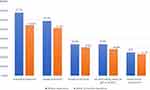 |
Figure 1 Type of sexual coercion experienced by female waiters in Jimma Town, 2018. |
Regarding the outcome of forced sex, 63 (16.1%) of the female waitress had unwanted pregnancies and 56 (14.3%) ended an abortion at least one time (Table 2).
HIV Risk Behaviors
About 161 (41.1%) of the female waitresses reported having regular (cohabiting) boyfriends and 301 (76.8%) have ever had sexual intercourse. Of those, around 161 (41.1%) female waitresses initiate sex early. Peer pressure 98 (32.6%), promised from a partner 56 (18.6%), personal desire 42 (13.9%), force 28 (9.3%), and marriage 35 (11.6%) were the causes of sexual initiation.
More than half of the study participants, 203 (51.8%) had multiple sexual partners. The research participants’ sex concurrency rate was 37.5%. Around 112 (37.2%) of female waiters who initiated intercourse reported having sexual contact with partners older than 10 years. In terms of substance use before the last sexual intercourse, 91 (30.2%) of those who started sexual intercourse reported substance use in the last sex, whereas 210 (69.8%) did not. More than two-thirds (67.4%) of those waitresses used condoms in their most recent sexual encounters. The usage of condoms with all non-regular partners in the previous intercourse was every time for 112 (37.2%) (Table 3).
 |
Table 3 HIV-Related Risk Behaviors Among Female Waitresses of Jimma Town, Southwest Ethiopia, 2018 |
One hundred fifty-four respondents (39.3%) have ever accepted money or gifts in return for sexual intercourse, and 147 respondents (37.5%) have ever gotten money/gifts from their most recent non-regular partners. One hundred thirty-three (90.5%) of those who engaged in transactional intercourse used condoms (Table 3). Of the total study participants, 281 (71.7%) of the participants had at least one of the HIV-related risk behaviors.
Sexual Health
More than half of the respondents 238 (60.7%) ever been tested for HIV. Of the total study participants, 217 (55.4%) female waitresses ever received HIV counseling services.
Sexually transmitted diseases were investigated, and 322 (82.1%) of respondents had heard of STDs and could describe at least one STD symptom. The reported symptoms were vaginal discharge (41.1%), foul-smelling discharge (21.4%), genital ulcer (26.8%), genital itching (17.9%), pain/burning during urination (23.3%), lower abdomen discomfort (10.7%), genital rash (14.3%), and swelling in the groin (1.8%) (Table 4).
 |
Table 4 Sexual Health Among Female Waitresses in Jimma, Ethiopia. 2018 |
Factors Associated with HIV Risk Behavior Among Female Waiters
Workplace, age, substance use, residency, and sexual coercion were all substantially linked with HIV risk behavior after controlling for potential confounding factors in a multivariable logistic model.
Female waiters working in bars were 4.6 times higher odds to engage in HIV risk behaviors compared to their counterparts (AOR 4.64, 95% CI: 2.15–10.0). The odds of engaging in HIV risk behaviors among female waiters who had ever used substances were three times higher than non-substance users (AOR 3.38, 95% CI: 1.7–6.7). Those who encountered sexual coercion in thier life time were 7.6 times higher in having HIV risk behavior compared to thier counterparts (AOR 7.6, 95% CI:3.8–15.3) (Table 5).
 |
Table 5 Factors Associated with HIV Risk Behavior Among Female Waitresses in Jimma Town, 2018 |
Discussion
There has been little research on sexual coercion among Ethiopian female waiters. This finding would be an input for policymakers to design interventions and strategies aimed at lessening the impact of sexual coercion and HIV risk behaviors among female waiters According to this survey, 71.4% of female waiters have experienced sexual coercion at some point in their lives (95% CI: 67.1–76.8). More than two third (71.6%) of female waiters engaged in HIV-related risk behaviors. Furthermore, working in a bar, substance use, and experiencing sexual coercion were all linked to HIV risk behaviors.
The finding of this study showed that more than two third of female waiters faced lifetime experience of sexual coercion This finding was high compared with the study conducted in Ethiopia10 and Uganda.22 This may be due to females being more likely to face sexual violence than others which may increase the prevalence.3 The other justification may be due to the larger sample size of the current study and the nature of the workplace that makes them more vulnerable to sexual violence including sexual coercion. This is supported by a different piece of literature that outlines that the workplace has a direct association with sexual coercion which can increase the prevalence of sexual coercion.23–25 This finding implied that health bureaus should organize and work together with stakeholders working in the area and deliver interventions to decrease the prevalence of sexual coercion. Furthermore, the establishments should have laws and procedures in place to safeguard female waiters from sexual coercion and non-sexual risk behaviors such as Khat chewing and alcohol use at work. This is supported by evidence that showed that lack of adequate awareness regarding the rights and obligations and lack of formal employment procedures in the establishments expose the female waiters and thus awareness creation should be done by different stakeholders.3 Thus, those findings imply policy and practice.
We found that the prevalence of HIV risk behavior among female waiters was 71.6%. This finding is higher than a study done in Uganda (59%).26 This might be because of the research population. In Uganda, the research population consists of female waiters and other participants. However, the subjects in this study are all female waiters. Another possible explanation is that sexual coercion is common in this research, which may increase the possibility of HIV-related risk behavior. There is evidence that waitresses participate in behaviors that enhance their chances of contracting HIV.27
This study identified that female waiters who were working in bars were 4.6 times more likely to engage in HIV-risk behavior than female waiters working in cafeterias. This may be due to the customer flow being high in the bar compared to the cafeteria then increases the possibility of getting exposed to behaviors that increase HIV risk behaviors. Furthermore, alcohol use is more common in bars than in cafeterias which can increase HIV risk behaviors. The finding of this study implied that HIV prevention efforts must target female waiters to prevent the further spread of HIV to the general population.
In this study, female waiters who had ever used substances were three times more likely to engage in HIV risk behavior than non-substance users. This finding was harmonized with the study conducted in the Jimma zone, Ethiopia (23) and Uganda (17). Substance use may create psychological discomfort, rendering female waiters unable to control themselves, exposing them to unsafe sexual activity and subsequently HIV risk behaviors. Evidence suggests that alcohol use is a mediator for HIV risk behaviors, causing physiological discomfort and subsequently increasing HIV risk behavior.28,29 Evidence shows that substance use is associated with HIV risk behaviors among female waiters.30
Sexual coercion was shown to be substantially linked with HIV risk behavior. One possible reason is that sexual coercion makes it difficult for women to negotiate safe sex and have sex without using a condom, which increases HIV risk behaviors. Furthermore, suitability customers’ behaviors in the food and beverage may be changed after alcohol intake, which may expose the waiters to violence and then to HIV risk behaviors. This is backed by other studies that show a link between sexual coercion and HIV risk behavior.31–33
Strengths and Limitations of the Study
The research’s strength includes it addresses a not well-studied population as well as the greater sample size. Owing to the sensitive nature of the research issue, participants may have underreported risk behaviors as a consequence of a social desirability bias in face-to-face interviews. There was a chance of recollection biases when determining certain sexual behaviors. Another weakness of the study is its cross-sectional design.
Conclusion
Nearly two-thirds of female waitresses had a lifetime experience of sexual coercion. This study also revealed a significant number of female waitresses engaged in HIV-risk behavior. Working in a bar, substance use, and experiencing sexual coercion were all linked to HIV risk behaviors Policymakers should put in place current legal penalties that protect women from gender-based violence by raising policy understanding about the burden and consequences of sexual coercion.
Data Sharing Statement
The data sets used in this work are accessible upon reasonable request from the corresponding author. After the defense, the thesis was uploaded to websites. Thus, the unpublished thesis paper is available on the Jimma University repository website34 (https://repository.ju.edu.et/handle/123456789/4152).
Ethical Approval
The Jimma University Institute of Health’s Institutional Review Board authorized the study procedure. A permission letter was acquired from the Population and family health department, and the Jimma town health office wrote an official letter of cooperation to the individual FDEs. The study was conducted in line with the Declaration of Helsinki. Before the interviews, all research participants were told about the purpose of the study, and agreement was acquired. Confidentiality was guaranteed. For participants under 18 years, informed voluntary consent was obtained from their parents/guardians.
Acknowledgment
The authors would like to thank Jimma University, the Jimma town health office, the Jimma town culture, and tourist office, all research participants, and data collectors for their cooperation and contributions to this work.
Author Contributions
All authors contributed significantly to the study, whether in the conception, study design, execution, data acquisition, analysis, and interpretation, or drafting, revising, or critically reviewing the article; gave final approval of the version to be published; agreed on the journal the article be submitted; and agree to be accountable for all aspects of the study.
Funding
This research was funded in part by Jimma University. However, the funder had no involvement in the data collection, analysis, and interpretation, as well as the paper authoring.
Disclosure
The authors report no conflicts of interest in this work.
References
1. Puhazhendhi V, Jayaraman B. Increasing women’s participation and employment generation among rural poor: an approach through informal groups. Indian J Agric Econ. 1999;54(3):287–295.
2. Harper S, Zeller D, Hauzer M, Pauly D, Sumaila UR. Women and fisheries: contribution to food security and local economies. Mar Policy. 2013;39:56–63. doi:10.1016/j.marpol.2012.10.018
3. Zewude B, Habtegiorgis T, Winter SC. Victimizations and surviving of workplace violence against waitresses in southern Ethiopia. PLoS One. 2021;16(12):e0261883. doi:10.1371/journal.pone.0261883
4. Hoel H, Einarsen S. Violence at Work in Hotels, Catering, and Tourism. Geneva: International Labor Office; 2003.
5. Koss MP, Gidycz CA, Wisniewski N. The scope of rape: incidence and prevalence of sexual aggression and victimization in a national sample of higher education students. J Consult Clin Psychol. 1987;55(2):162. doi:10.1037/0022-006X.55.2.162
6. Tusiime S, Musinguzi G, Tinkitina B, et al. Prevalence of sexual coercion and its association with unwanted pregnancies among young pregnant females in Kampala, Uganda: a facility based cross-sectional study. BMC Women’s Health. 2015;15(1):79. doi:10.1186/s12905-015-0235-9
7. Worke MD, Koricha ZB, Debelew GT. Prevalence of sexual violence in Ethiopian workplaces: systematic review and meta-analysis. Reprod Health. 2020;17(1):195. doi:10.1186/s12978-020-01050-2
8. Takele A, Setegn T. Sexual coercion and associated factors among female students of Madawalabu University, Southeast Ethiopia. Adv. Public Health. 2014;2014:417517. doi:10.1155/2014/417517
9. Van Decraen E, Michielsen K, Van Rossem R, Temmerman M, Herbots S. Sexual coercion among in-school adolescents in Rwanda: prevalence and correlates of victimization and normative acceptance. Afr J Reprod Health. 2012;16(3):139–153.
10. Worke MD, Demelash H, Meseret L, Bezie M, Abebe F. Factors associated with sexual violence among waitresses working in Bahir Dar City, Ethiopia: a mixed-method study. BMC Women’s Health. 2022;22(1):209. doi:10.1186/s12905-022-01806-x
11. Stockman JK, Campbell JC, Celentano DD. Sexual violence and HIV risk behaviors among a nationally representative sample of heterosexual American women: the importance of sexual coercion. J Acquir Immune Defic Syndr. 2010;53(1):136. doi:10.1097/QAI.0b013e3181b3a8cc
12. Yemsrach K, Aliye K, Bisrat Z, Robera O. Sexual coercion and associated factors among female private university students in Bishoftu Town, East Shewa Ethiopia. J Womens Health Issues Care. 2017;6(4):2.
13. O’Sullivan LF, Byers ES, Brotto LA, Majerovich JA. Access to and use of sexual health care services among young Canadians with and without a history of sexual coercion. Can Fam Physician. 2015;61(10):e467–e473.
14. Hoffman S, O’Sullivan L, Harrison A, Dolezal C, Monroe-Wise A. HIV risk behaviors and the context of sexual coercion in young adults’ sexual interactions: results from a diary study in rural South Africa. Sex Transm Dis. 2006;33(1):52–58. doi:10.1097/01.olq.0000187198.77612.d8
15. Hooper AG. Perceptions of Risky Sexual Behaviours Among University of Cape Coast Female Students. University of Cape Coast; 2018.
16. Kibret GD, Ferede A, Leshargie CT, Wagnew F, Ketema DB, Alebel A. Trends and spatial distributions of HIV prevalence in Ethiopia. Infect Dis Poverty. 2019;8(1):90. doi:10.1186/s40249-019-0594-9
17. Adal M. Systematic review on HIV situation in Addis Ababa, Ethiopia. BMC Public Health. 2019;19(1):1–11. doi:10.1186/s12889-019-7885-8
18. Belachew T, Jira C, Mamo Y. HIV seroprevalence among students of Jimma University, Southwest Ethiopia. Ethiop J Health Sci. 2004;14(1):65–74.
19. Bedaso NG, Debusho LK. Clinics register based HIV prevalence in Jimma zone, Ethiopia: applications of likelihood and Bayesian approaches. BMC Infect Dis. 2022;22(1):1–14. doi:10.1186/s12879-021-06965-0
20. Abajebel S, Jira C, Beyene W. Utilization of a health information system at the district level in Jimma zone Oromia regional state, South west Ethiopia. Ethiop J Health Sci. 2011;21(Suppl 1):65–76.
21. Lutz TM, Ferreira KE, Noel JK, Bruder MB. Secondary analysis of one state’s Youth Risk Behavior Surveillance System (YRBSS) data by individualized education program (IEP) status. Disabil Health J. 2023;16(1):101393. doi:10.1016/j.dhjo.2022.101393
22. Noubiap JJN, Nansseu JRN, Ndoula ST, et al. Prevalence and correlates of HIV-risky sexual behaviors among students attending the Medical and Social Welfare Center of the University of Maroua, Cameroon. BMC Res Notes. 2015;8(1):1–11. doi:10.1186/s13104-015-1638-2
23. Fitzgerald L. Unseen: the sexual harassment of low-income women in America. Equal Divers Incl. 2020;39(1):5–16. doi:10.1108/EDI-08-2019-0232
24. Gutek BA, Morasch B. Sex‐ratios, sex‐role spillover, and sexual harassment of women at work. J Soc Issues. 1982;38(4):55–74. doi:10.1111/j.1540-4560.1982.tb01910.x
25. Klein O, Arnal C, Eagan S, Bernard P, Gervais SJ. Does tipping facilitate sexual objectification? The effect of tips on sexual harassment of bar and restaurant servers. Equal Divers Incl. 2021;40(4):448–460. doi:10.1108/EDI-04-2019-0127
26. Tumwesigye NM, Atuyambe L, Wanyenze RK, et al. Alcohol consumption and risky sexual behavior in the fishing communities: evidence from two fish landing sites on Lake Victoria in Uganda. BMC Public Health. 2012;12(1):1–11. doi:10.1186/1471-2458-12-1069
27. Agardh A, Odberg-Pettersson K, Östergren P-O. Experience of sexual coercion and risky sexual behavior among Ugandan university students. BMC Public Health. 2011;11(1):1–12. doi:10.1186/1471-2458-11-527
28. Elkington KS, Bauermeister JA, Zimmerman MA. Psychological distress, substance use, and HIV/STI risk behaviors among youth. J Youth Adolesc. 2010;39(5):514–527. doi:10.1007/s10964-010-9524-7
29. Browne FA, Wechsberg WM. The intersecting risks of substance use and HIV risk among substance-using South African men and women. Curr Opin Psychiatry. 2010;23(3):205–209. doi:10.1097/YCO.0b013e32833864eb
30. Finch K, Novotny TE, Ma S, Qin D, Xia W, Xin G. Smoking knowledge, attitudes, and behaviors among rural-to-urban migrant women in Beijing, China. Asia Pac J Public Health. 2010;22(3):342–353. doi:10.1177/1010539509335034
31. Puffer ES, Kochman A, Hansen NB, Sikkema KJ. An evidence-based group coping intervention for women living with HIV and a history of childhood sexual abuse. Int J Group Psychother. 2011;61(1):98–126. doi:10.1521/ijgp.2011.61.1.98
32. Purdie MP, Abbey A, Jacques-Tiura AJ. Perpetrators of intimate partner sexual violence: are there unique characteristics associated with making partners have sex without a condom? Violence Against Women. 2010;16(10):1086–1097. doi:10.1177/1077801210382859
33. Allsworth JE, Anand M, Redding CA, Peipert JF. Physical and sexual violence and incidents of sexually transmitted infections. J Womens Health. 2009;18(4):529–534. doi:10.1089/jwh.2007.0757
34. Imana R, Abdullahi M, Ali R. Sexual coercion, HIV risk behavior and sexual health among female waitresses in Jimma town, south west Ethiopia; 2018.
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
