Back to Journals » Vascular Health and Risk Management » Volume 20
Retrospective Cohort Angiographic Analysis of Vertebral Artery Dominance, Stenosis Patterns, and Demographic Correlations
Authors Qtaish I, Ayasrah M , Qtaish NR
Received 26 January 2024
Accepted for publication 12 April 2024
Published 22 April 2024 Volume 2024:20 Pages 207—214
DOI https://doi.org/10.2147/VHRM.S453352
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Daniel Duprez
Izzeddin Qtaish,1 Mohammad Ayasrah,2 Noat R Qtaish3
1Radiology and Interventional Radiology, Faculty of Medicine, Jordan University of Science and Technology, Irbid, Jordan; 2Department of Allied Medical Sciences-Radiologic Technology, Faculty of Applied Medical Sciences, Jordan University of Science and Technology, Irbid, Jordan; 3College of Medicine, Al Balqa Applied University, Salt, Jordan
Correspondence: Mohammad Ayasrah, Department of Allied Medical Sciences-Radiologic Technology, Faculty of Applied Medical Sciences, Jordan University of Science and Technology, Irbid, Jordan, Tel +96227201000-26939, Fax +96227201087, Email [email protected]
Background: Differences in dominance and stenosis in the complex vertebral artery (VA) network pose challenges in diagnosing and treating cerebrovascular diseases crucial for brain nutrition. This research examines these intricacies, highlighting the importance of detailed diagnosis and treatment methods.
Objective: To analyze the prevalence of the dominant VA, evaluate the influence of gender and age on steno-occlusion, and explore the correlation between the dominant VA and stenosed VA segments.
Methods: A retrospective study of 249 angiograms from patients with VA stenosed at King Abdullah University Hospital between August 2019 and December 2022. The patients presenting symptoms of vertigo, migraines, headaches, or transient ischemic attacks (TIA) were included, 182 cases were classified based on VA dominance and stenosis severity. The data were analyzed using IBM SPSS 27.
Results: Out of the 182 participants, 64.8% were male, with an average age of 61.3 years and 35.2% were female. The prevalence of stenosis was distributed as follows: 26.4% mild, 44.0% moderate, and 29.7% severe. Statistically significant correlations were observed between hypertension, smoking, hyperlipidemia, and the degree of stenosis (p < 0.05), but not with diabetes. The prevalence of left vertebral artery (VA) dominance was found to be 41.1%. Additionally, there was no gender connection observed in the distribution of steno-occlusion (p = 0.434). There is no notable correlation between the degree of stenosis and the dominant vertebral artery (p > 0.05).
Conclusion: Angiographic findings reveal the complex relationship between the dominance of the VA, patterns of stenosis, and demographic factors. Individuals with a dominant VA had a greater likelihood of developing stenosis on the opposite non-dominant side. The high occurrence of severe stenosis highlights the need for tailored diagnostic and treatment approaches. Understanding vertebral stenosis as a multifaceted interaction of demographic, lifestyle, and anatomical variables is essential for enhancing treatment strategies.
Keywords: Vertebral artery dominance, stenosis, cerebrovascular diseases, risk factors, retrospective angiographic study
Introduction
The complex network of blood vessels that nourish the brain serves a crucial role in preserving its well-being and functionality. Specifically, the posterior cerebral circulation depends on the vertebral arteries (VAs) as its main channels.1 These arteries are the first branches of the subclavian arteries, situated at the cervical region. The right subclavian artery originates from the truncus brachiocephalic artery, whereas the left subclavian artery emerges from the aorta. It is not unusual to find variations in the origin and entrance locations of the vertebral arteries (VAs) into the transverse foramen of the cervical vertebrae. These variations are thought to be caused by changes in the stages of embryonic development.2 The convergence of the right and left vertebral arteries takes place in the pontomedullary area, resulting in the creation of the basilar artery, which is an essential part of the vertebrobasilar artery system (VBS). The VBS provides essential nourishment to vital components like the spinal cord, internal ears, brainstem, cerebellum, midbrain, thalamus, and some parts of the temporal and occipital cortex.3 Moreover, when there is a blockage in the carotid artery, the VBS intervenes by providing alternative arteries to provide blood flow to the front part of the brain.4
Traditionally, the vertebral arteries are categorized into four segments: the proximal segment (V1), the transverse process segment (V2), the suboccipital segment (V3), and the intracranial segment (V4).5 Although Doppler Ultrasonography (DUSG) can provide a rapid evaluation of vertebral arteries in clinical settings,6 it cannot provide an accurate assessment of their origin and distal parts.7 While cervical CT or MR angiography can offer more precise evaluations,5 traditional angiography investigations continue to be the most reliable method.8 Recent study, using DUSG and angiographic testing, has shown the distinct measurements, rates of flow, and capacities of VAs, highlighting the specific characteristics of these arteries.9
It is important to note that changes in the VAs might cause damage to the vertebrobasilar network.10 It is hypothesized that the endothelium of the VA is prone to structural damage as a result of elevated blood volume and flow.6 The presence of hypoplastic vertebral arteries (VAH) has been recognized as a possible risk factor for posterior circulation ischemia, specifically in relation to the V1 segment. Studies have indicated that most cases of ischemic diseases in this area are related to the main vertebro-basilar artery, and it is common for the vertebral artery (VA) to have a bigger diameter or be closer to the basilar artery (BA).11 The prevalence of vertebrobasilar artery (VA) dominance can lead to abnormalities in the structure and function of the vertebrobasilar artery system, which may possibly elevate the likelihood of cerebrovascular accidents in the posterior circulation.9 Although recent research have explored the influence of dominant vertebral artery (VA) on vertebro-basilar system (VBS), there is still limited evidence connecting dominant VA with VA steno-occlusion.12 The primary objective of this study is to enhance the existing research by investigating the frequency of dominant vertebral artery (VA), the impact of gender and age on steno-occlusion, and the relationship between dominant VA and steno-occluded VA segments. The study specifically focuses on patients who received treatment at King Abdullah University Hospital. Furthermore, it examined the association between chronic conditions such as hyperlipidemia, hypertension (HTN), and diabetes mellitus (DM) with vertebral stenosis.
Materials and Methods
In the current investigation, 249 individual applications for angiogram between August 2019 and December 2022 were retrospectively examined. The guidelines outlined in the Declaration of Helsinki were followed and the study was approved by the Institutional Review Board of Jordan University of Science and Technology No.15/148/2022 dated 18/4/2022. The informed consent was obtained from the study participants.
These 249 individuals came to KAUH with general problems like vertigo, migraines, headaches, and imbalanced movement patterns, or with more specific concerns like TIA or small strokes. Inclusion criteria involved all adult patients with VA stenosis proved by one or more modalities of radiology imaging including cervical CTA, neck DUSG, and MRA scans and confirmed by Digital subtraction angiography (DSA). The study’s exclusion criteria involved excluding persons who met the following conditions: those with inadequate data, situations where the angiography examination was incomplete, patient with cardiac causes of thrombo-embolization, or with history of drug abuse as they have a higher risk of VA stenosis which obscure the role of the VA dominance on the VA stenosis.
As a consequence of applying these criteria, 67 instances were excluded from the initial data set, leaving 182 viable cases for detailed review and assessment.
The patients were categorized into three unique groups according to their vertebral artery (VA) dominance: codominant, left-dominant (Lt. dominant), and right-dominant (Rt. dominant). The categorization of VA dominance was established based on the diameter of the vertebral artery. The extracranial vertebral artery typically has a luminal diameter ranging from around 3 to 5 millimeters. Vertebral arteries (VAs) having a diameter less than 2 millimeters were classified as hypoplastic VAs.12 When the diameter disparity between the vertebral arteries is below 0. Millimeters 0.3,6 they are categorized as codominant. The most common form is left vertebral artery dominance.1
The patients were classified into three separate categories based on the degree of stenosis: mild (stenosis up to 50%), moderate (stenosis ranging from 50% to 90%), and severe stenosis (surpassing 90%) to total occlusion. Demographic data, encompassing age and gender, were rigorously gathered, alongside risk factors such as hyperlipidemia, (HTN), and (DM). Furthermore, the precise site of the stenosis, specifically whether it impacted the Left Vertebral Artery or Right Vertebral Artery, was recorded for further examination.
The analysis of the data was performed with the IBM SPSS 27 statistical program. The chi-square (χ2) test was utilized to compare categorical factors linked to the general features across patients with different degrees of VA stenosis, whilst a t-test was implemented to evaluate disparities in age and gender.
Results
Among the 182 patients who participated in this study, 118 (64.8%) were male, while 64 (35.2%) were female. The mean age of all patients was 61.3 years, with a standard deviation of 12.6 years. Male patients had a mean age of 60.7 years and a standard deviation of 13.2 years, whereas female patients had a mean age of 62.15 years and a standard deviation of 11.5 years as shown in Table 1. It is important to mention that the average age of female patients was substantially greater than that of male patients (p = 0.001).
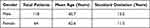 |
Table 1 Demographic Characteristics of Patients by Gender |
An in-depth analysis of the medical records of the participants in our study revealed a notable variation in the extent of vertebral stenosis Table 2. More precisely, 26.4% of the subjects had mild stenosis, indicating a relatively insignificant narrowing in their vertebral arteries. In addition, 44.0% of the participants had moderate stenosis, indicating a significant level of vascular constriction. Nevertheless, we were more alarmed when we observed that 29.7% of the participants encountered severe stenosis.
 |
Table 2 Distribution of Vertebral Artery Stenosis Severity in Study Participants |
The distribution of the major risk factors for DM, HTN, smoking, and hyperlipidemia is shown in Figure 1. Remarkably, 27.5% of patients indicated that they had never been diagnosed with diabetes, and a substantial fraction (19.8%) had no previous diagnosis of hypertension (HTN). Simultaneously, 25.8% of the group engaged in smoking, while 11.5% showed signs of hyperlipidemia.
 |
Figure 1 The distribution of the major risk factors of VA stenosis. |
In the examined cohort, 33 patients (18.1%) had a right-dominant (VA), 73 patients (40.1%) displayed left-dominant VA, and 76 patients (41.7%) had a codominant VA pattern. Out of the 106 patients with a dominant VA (58.2%), 41 were female (38.7%) and 65 were male (61.3%). While there was a higher prevalence of dominant VA among male patients, statistical analysis indicated no significant association between gender and dominant side in this population. The obtained p-value (0.434) exceeds the conventional significance threshold of 0.05, suggesting that gender is not a significant factor influencing dominant VA laterality in this study cohort.
Steno-occlusion was seen in 11 patients with right-dominant vertebral artery (VA) (6%), 22 patients with right non-dominant VA (12.1%), and none of the patients with right codominant VA. Furthermore, steno-occlusion was seen in 31 patients with left-dominant vertebral artery (VA) (17%), 41 patients with left non-dominant VA (22.5%), and one patient with left co-dominant VA (0.5%) as illustrated in Table 3.
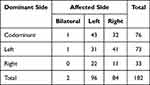 |
Table 3 Distribution of Vertebral Artery Dominance and Affected Side in Study Participants |
Importantly, when mainly left and right vertebral arteries were compared, there were statistically significant differences between the occurrence of vertebral stenosis on the left and right sides (p-value = 0.030 for Pearson Chi-Square; p-value = 0.020 for Likelihood Ratio) as shown in Table 4, suggesting a discrepancy in the distribution of stenosis between the two sides of the vertebral arteries.
 |
Table 4 Chi-Square Test Results for Comparison of Vertebral Stenosis Distribution Between Left and Right Sides |
Similarly, there was no notable association observed between the severity of stenosis in the vertebral artery (VA) (mild, moderate, and severe) and the dominance of the VA (p > 0.05). Notably, the most common and severe narrowing of the blood vessels (14.8% or 27 out of 182 cases) was found in situations where the left side was dominant as shown in Table 5. On the other hand, the highest incidence of moderately narrowed blood vessels (24.8% or 44 out of 182 cases) was identified in cases where both sides were equally prominent.
 |
Table 5 Cross Tabulation of Vertebral Artery Dominance and Degree of Stenosis in Study Participants |
Discussion
The vertebral arteries are, integral parts of the posterior circulation, supply blood to many crucial areas of the brain and a portion of the upper spinal cord.13 Comprehending the distinct structural variations and connections with stenosis is crucial for the detection and management of cerebrovascular diseases.14 Cerebrovascular illnesses, which include a wide range of problems affecting blood arteries and the flow of blood in the brain, present a substantial worldwide health problem.15 Vertebral artery (VA) stenosis, whether occurring in the extracranial or intracranial segments, is a significant cause of strokes in the posterior circulation.16 To prevent these situations, it is necessary to tackle specific issues and inequalities. Comprehension of the pathogenesis of cerebrovascular illnesses requires a comprehension of the complex circulatory network that nourishes the brain. The posterior circulation, which is primarily controlled by the vertebral arteries, is essential for guaranteeing enough blood flow to crucial brain areas.17
Variations in vertebral artery dominance and stenosis patterns provide difficulties in detecting and treating cerebrovascular disorders.18 Recent advances in imaging technology, along with an increasing understanding of the importance of the posterior circulation, encouraged an investigation into the complex elements of vertebral artery dominance and stenosis.19 Researchers attempted to better understand the delicate interaction of these variables, digging into anatomical differences, demographic factors, and lifestyle impacts related to vertebral stenosis. These discoveries have the potential to transform clinical practices by allowing healthcare practitioners to give more exact diagnoses, personalized treatments, and preventative methods. In order to achieve these objectives, we undertook a thorough retrospective angiographic study to fill information gaps and provide nuanced insights into vertebral artery dominance, stenosis patterns, risk factors, and their relationships with demographic characteristics.
This study aimed to examine the complex relationship between vertebral artery dominance, stenosis, and demographic variables by a retrospective angiographic analysis. This study clarifies key facets of posterior circulation ischemia.20 Although not statistically significant, our data indicated a greater occurrence of VA stenosis in patients with dominant side of the VA (58.2%) compared to the co-dominant side (41.8%) as depicted in Table 5.
Multiple criteria are present in the literature to ascertain the dominant vertebral artery (VA). Several research suggest that there is an observed asymmetry in vertebral arteries, with a minimum diameter difference of 0.3 mm.6 However, other studies argue that a minimum difference of 30% is necessary.21 The absence of a specific definition for VA stenosis is a result of studies frequently include individuals who are not healthy, having small sample sizes, or utilizing various imaging techniques such as ultrasonography, angiography (DSA), or MRI.22 Angiography is often regarded as the most reliable and accurate tool for assessing the entire VA area.14,23,24
The study found that a significant number of subjects (44.0%, N=182) had mild stenosis of the vertebral artery (VA), whereas 29.7% had severe stenosis. The results closely correspond to previous study, which reported that 37.5% of the participants had mild stenosis, while 16.1% had severe stenosis.25 The uniformity of these percentages across research underscores the importance of comprehending the prevalence and distribution of VA stenosis severity in various groups, hence enhancing our understanding of wider trends in vascular health.
For our study, we used a dominance criterion based on a difference in diameter of 0.3 mm. In 41.1% of instances, the left vertebral artery (VA) showed dominance, whereas the right vertebral artery diameter was prominent in 18.1% of cases. The results are consistent with a prior investigation that found a prevalence of 58% for the left VA and 19% for the right VA.23
No dominance was observed in 41.8% of instances, while left-side dominance was observed in 40.1% of cases and right-side dominance was shown in 18.1% of cases. Figure 2. The co-dominance percentages discovered in this study differ from those described in the literature, with one study documenting 26.5% and another reporting 23%. Notably, our analysis found that left VA dominance was the prevailing pattern, accounting for 42% of cases. This closely aligns with the 58% described in a previous study.26 These discrepancies highlight the heterogeneity in results among various study inquiries.
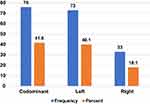 |
Figure 2 Frequency and percentage of VA dominancy. |
We performed an evaluation of atherosclerotic risk factors, including hypertension, hyperlipidemia, smoking, and diabetes. The study showed significant correlations between hypertension, cigarette smoking, and hyperlipidemia with the severity of VA stenosis (P-values of 0.002, 0.043, and 0.034, respectively, as shown in Table 6). Nevertheless, there was no substantial correlation found between DM and VA stenosis, as shown by a p-value of 0.401, which is above the standard significance threshold of 0.05.
 |
Table 6 Association Between Atherosclerotic Risk Factors and Vertebral Artery Stenosis |
Unlike our study, a prior study showed a strong association between all risk variables for atherosclerosis and Vertebral Artery Occlusive Disease.27 The disparity in findings highlights the significance of taking into account differences in research methodology, demographics, and other factors that may impact the observed correlations.
While our study gives important insights into the demographic and medical picture of VA stenosis, it has numerous limitations. The study’s retrospective methodology brings inherent biases, and the sample size may not adequately represent the larger population. Furthermore, the lack of particular lifestyle data, such as physical activity and eating habits, prevents a thorough examination of potential risk variables. To address these limitations, future research should aim for prospective studies with bigger, diverse cohorts and extensive lifestyle assessments.
Conclusion
This retrospective angiographic analysis provides a thorough summary of vertebral artery dominance, stenosis patterns, and their relationship to demographic parameters. The variety in dominance patterns and the prevalence of severe stenosis highlight the complexity of VA stenosis, needing individualized methods to diagnosis and care. Individuals with a dominant Vertebral Artery (either on the right or left side) had a greater likelihood of developing stenosis on the opposite non-dominant side.
Considering vertebral stenosis as a multidimensional illness impacted by demographic, lifestyle, and anatomical factors is critical for designing effective prevention and management measures. This study provides a platform for future research into the complicated interplay of these factors and their consequences for clinical practice. By gaining a better understanding of VA stenosis, healthcare providers can improve their diagnostic and treatment techniques, thereby improving the quality of care for patients. Collaborative efforts among academics, clinicians, and policy makers are required to untangle the complexity of VA stenosis and pave the road for improved cerebrovascular disease healthcare services and outcomes.
Acknowledgments
We would like to thank our respectful research assistants for their distinguished role of data collection.
Funding
The authors did not receive support from any organization for the submitted work, to assist with the preparation of this manuscript, or for conducting this study. No funds, grants, or other support was received.
Disclosure
The authors report no conflicts of interest in this work.
References
1. Akar ZC, Dujovny M, Slavin KV, Gomez-Tortosa E, Ausman JI. Microsurgical anatomy of the intracranial part of the vertebral artery. Neurol Res. 1994;16(3):171–180. doi:10.1080/01616412.1994.11740221
2. Bordes SJ, Iwanaga J, Zarrintan S, Watanabe K, Tubbs RS. Accessory vertebral artery: an embryological review with translation from adachi. Cureus. 2021;13(2):e13448. doi:10.7759/cureus.13448
3. Stojanovic B, Vasovic L, Trandafilovic M, Vlajkovic S, Drevensek M. Arterial abnormalities and associated variations of the vertebrobasilar system on the brain base: apropos of a rare case. Int J Morphol. 2022;40(3):750–754. doi:10.4067/S0717-95022022000300750
4. Maitas O, Bob-Manuel T, Price J, et al. Vertebral artery interventions: a comprehensive updated review. Curr Cardiol Rev. 2023;19(1):127–138. doi:10.2174/1573403X18666220317093131
5. Celikyay ZRY, Koner AE, Celikyay F, Denız C, Acu B, Firat MM. Frequency and imaging findings of variations in human aortic arch anatomy based on multidetector computed tomography data. Clin Imaging. 2013;37(6):1011–1019. doi:10.1016/j.clinimag.2013.07.008
6. Jeng JS, Yip PK. Evaluation of vertebral artery hypoplasia and asymmetry by color-coded duplex ultrasonography. Ultrasound Med Biol. 2004;30(5):605–609. doi:10.1016/j.ultrasmedbio.2004.03.004
7. Grasso G, Alafaci C, Passalacqua M, Tschabitscher M, Salpietro FM, Tomasello F. Landmarks for vertebral artery repositioning in bulbar compression syndrome: anatomic and microsurgical nuances. Neurosurgery. 2005;56(1 Suppl):
8. Little SB, Sarma A, Bajaj M, et al. Imaging of vertebral artery dissection in children: an underrecognized condition with high risk of recurrent stroke. RadioGraphics. 2023;43(12):e230107. doi:10.1148/rg.230107
9. Cagnie B, Petrovic M, Voet D, Barbaix E, Cambier D. Vertebral artery dominance and hand preference: is there a correlation? Man Ther. 2006;11(2):153–156. doi:10.1016/j.math.2005.07.005
10. Hong JM, Chung CS, Bang OY, Yong SW, Joo IS, Huh K. Vertebral artery dominance contributes to basilar artery curvature and peri-vertebrobasilar junctional infarcts. J Neurol Neurosurg Psychiatry. 2009;80(10):1087–1092. doi:10.1136/jnnp.2008.169805
11. Ergun O, Gunes Tatar I, Birgi E, Hekimoglu B. Evaluation of vertebral artery dominance, hypoplasia and variations in the origin: angiographic study in 254 patients. Folia Morphol. 2016;75(1):33–37. doi:10.5603/FM.a2015.0061
12. Chen X, Xu J, Zhang Y, Lin M, Wang H, Song Y. Evaluation of hemodynamic characteristics in posterior circulation infarction patients with vertebral artery dominance by color Doppler flow imaging and transcranial Doppler sonography. Int J Neurosci. 2021;131(11):1078–1086. doi:10.1080/00207454.2020.1773820
13. Ko HY, Huh S. Clinical and functional anatomy of the spinal cord. In: Handbook of Spinal Cord Injuries and Related Disorders. Springer; 2021.
14. Magklara EP, Pantelia ET, Solia E, et al. Vertebral artery variations revised: origin, course, branches and embryonic development. Folia Morphol. 2021;80(1):1–12. doi:10.5603/FM.a2020.0022
15. Liu C, Du L, Wang S, et al. Differences in the prevention and control of cardiovascular and cerebrovascular diseases. Pharmacol Res. 2021;170:105737. doi:10.1016/j.phrs.2021.105737
16. Cloud GC, Markus HS. Vertebral Artery Stenosis. Curr Treat Options Cardiovasc Med. 2004;6(2):121–127. doi:10.1007/s11936-004-0040-5
17. Feng Y, Liu J, Fan T, et al. Vertebral artery stenoses contribute to the development of diffuse plaques in the basilar artery. Front Bioeng Biotechnol. 2020;2:8.
18. Burle VS, Panjwani A, Mandalaneni K, Kollu S, Gorantla VR. Vertebral artery stenosis: a narrative review. Cureus. 2022;14(8):e28068. doi:10.7759/cureus.28068
19. Khan S, Cloud GC, Kerry S, Markus HS. Imaging of vertebral artery stenosis: a systematic review. J Neurol Neurosurg Psychiatry. 2007;78(11):1218–1225. doi:10.1136/jnnp.2006.111716
20. Madonis SM, Jenkins JS. Vertebral artery stenosis. Prog Cardiovasc Dis. 2021;65:55–59. doi:10.1016/j.pcad.2021.02.006
21. Smith AS, Bellon JR. Parallel and spiral flow patterns of vertebral artery contributions to the basilar artery. Am J Neuroradiol. 1995;16(8):1587–1591.
22. Park J, Kim J, Roh J. Hypoplastic vertebral artery: frequency and associations with ischaemic stroke territory. J Neurol Neurosurg Psychiatry. 2007;78(9):954–958. doi:10.1136/jnnp.2006.105767
23. Şahin H, Gökçe M. An association between vertebral artery dominance and steno-occlusion of the vertebral artery segments: a retrospective angiographic study. J Clin Neurosci. 2021;92:203–206. doi:10.1016/j.jocn.2021.08.008
24. Yazıcı A, Inanç Y. Evaluation of BPPV with vertebral artery values. Neuropsychiatr Dis Treat. 2018;14:1975–1979. doi:10.2147/NDT.S169991
25. Qureshi AI, Babar S, Saeed O, Saleem MA, Wallery SS. Vertebral artery occlusive disease: data from the angiographically confirmed vertebral artery disease registry. J Stroke Cerebrovasc Dis off J Natl Stroke Assoc. 2018;27(11):3294–3300. doi:10.1016/j.jstrokecerebrovasdis.2018.07.026
26. Vural A, Çiçek ED. Is the asymmetry between the vertebral arteries related to cerebral dominance? Turk J Med Sci. 2019;49(6):1721–1726. doi:10.3906/sag-1904-161
27. van der Toorn JE, Engelkes SR, Ikram MK, et al. Vertebrobasilar artery calcification: prevalence and risk factors in the general population. Atherosclerosis. 2019;286:46–52. doi:10.1016/j.atherosclerosis.2019.05.001
 © 2024 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2024 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
