Back to Journals » Vascular Health and Risk Management » Volume 18
Reasons for the Decline of Cardio-Ankle Vascular Index (CAVI) in Aortic Valve Stenosis (AVS) [Letter]
Authors Takahashi K , Yamamoto T, Shirai K
Received 2 December 2022
Accepted for publication 9 December 2022
Published 23 December 2022 Volume 2022:18 Pages 887—888
DOI https://doi.org/10.2147/VHRM.S399737
Checked for plagiarism Yes
Editor who approved publication: Prof. Dr. Pietro Scicchitano
Koji Takahashi,1 Tomoyuki Yamamoto,1 Kohji Shirai2
1Fukuda Denshi Co., Ltd., Tokyo, Japan; 2Department of Internal Medicine, Mihama Hospital, Chiba, Japan
Correspondence: Tomoyuki Yamamoto, Email [email protected]
View the original paper by Professor Bäck and colleagues
Dear editor
We have read with great interest the article entitled “Arterial Stiffness in Aortic Stenosis and the Impact of Aortic Valve Replacement” by Plunde and Bäck.1 They reported low CAVI values in AVS patients while CAVI increased after surgical aortic valve replacement and indicated that an exceptionally low CAVI could be useful in AVS screening. Their findings shed light on masked arterial stiffness, but some questions still remain to be clarified. For that purpose, we present two findings.
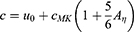
The first is the effect of blood flow velocity (BFV). In AVS, increased ejection time (ET) is commonly observed, which is generally accompanied by decreased BFV downstream. Pulse wave velocity (PWV) is represented by the Moens-Korteweg (MK) formula, which includes the vascular elastic modulus but not BFV, due to the simplified derivation. Lillie et al introduced a more detailed formula, which includes the average BFV and circumferential strain of the vessel as follows.2
[c: PWV, u0: average BFV, cMK: PWV at MK formula, Aη: maximum circumferential strain (affected by peak pressure)].
Therefore, if BFV decreases, the PWV will decrease, as will the CAVI calculated from the PWV. Lillie et al noted that PWV varies by up to 12% with BFV and peak pressure.2
The second is the effect of dynamic elastic modulus (Edyn). ET prolongation is associated with a decrease in pulse wave steepness, or frequency. Bergel reported that canine vessels show an abrupt increase in stiffness between the frequencies of 0 and 2 Hz, and with increasing frequency, there is little further change.3 This increase appeared to be greater for more muscular vessels. In the carotid artery, which contains a lot of smooth muscle, the ratio of Edyn to Static Elastic Modulus (Estatic) is as high as 1.6 times at 2 Hz. He considered that the change in modulus over the critical range is due to the inability of a smooth muscle component to respond to rapid changes in tension.
Since CAVI includes muscular arteries as well as elastic arteries in the measurement section, it is affected by the pulse wave frequency. The degree of change depends on the frequency of the pulse wave and the composition of the artery, thus it cannot be generalized, but CAVI is considered to change distinctively as the frequency decreases.
In AVS with heart murmurs, measurement errors might occur since CAVI uses a phonocardiogram to measure PWV. However, apart from that, the above two causes are physically, and physiologically essential phenomena and careful consideration is necessary. (Supplementary documents)
CAVI measured in dynamic conditions is higher than in static conditions, but the criteria are determined accordingly and there is no problem in general. However, in special conditions with weak and prolonged pulse, which is caused by AVS or the resulting heart failure, CAVI values can be markedly low. Such low values can be useful indicators to detect masked arterial stiffness and elucidate hidden disease, as Plunde and Bäck reported.
Further research and development are expected in the future.
Disclosure
Koji Takahashi and Tomoyuki Yamamoto are employees of Fukuda Denshi Co., Ltd. and involved in the development of CAVI. Kohji Shirai reports no conflicts of interest in this communication.
References
1. Plunde O, Bäck M. Arterial stiffness in aortic stenosis and the impact of aortic valve replacement. Vasc Health Risk Manag. 2022;18:117–122. doi:10.2147/VHRM.S358741
2. Lillie JS, Liberson AS, Mix D, et al. Pulse wave velocity prediction and compliance assessment in elastic arterial segments. Cardiovasc Eng Technol. 2015;6(1):49–58. doi:10.1007/s13239-014-0202-x
3. Bergel DH. The dynamic elastic properties of the arterial wall. J Physiol. 1961;156:458–469. doi:10.1113/jphysiol.1961.sp006687
 © 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.