Back to Journals » Clinical Ophthalmology » Volume 17
Pupil Status with Low-Energy Femtosecond Laser-Assisted Cataract Surgery versus Conventional Phacoemulsification: An Intraindividual Comparative Study
Authors Salgado R , Torres PF, Marinho A
Received 8 December 2022
Accepted for publication 16 January 2023
Published 24 January 2023 Volume 2023:17 Pages 331—339
DOI https://doi.org/10.2147/OPTH.S399788
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Scott Fraser
Ramiro Salgado,1 Paulo F Torres,2 Antonio Marinho3
1Departamento de Oftalmologia do Hospital da Arrábida, Hospital de Santo António, Centro Hospitalar e Universitário do Porto, Vila Nova de Gaia, Porto, Portugal; 2Departamento de Oftalmologia do Hospital da Prelada, Universidade do Porto, Porto, Portugal; 3Departamento de Oftalmologia do Hospital da Luz Arrábida, Universidade do Porto, Porto, Portugal
Correspondence: Ramiro Salgado, Departamento de Oftalmologia do Hospital da Arrábida, Praceta Henrique Moreira 150, Vila Nova de Gaia, 4400-346, Portugal, Tel +351 915677244, Fax +351 224003046, Email [email protected]
Purpose: To compare the pupil changes in low-energy femtosecond laser-assisted cataract surgery (FLACS) with conventional phacoemulsification (CP) intraindividually.
Patients and Methods: A retrospective review of registered surgical data from patients that undergone uncomplicated cataract surgery in a single centre, with randomly assigned femtosecond laser–assisted cataract surgery (FLACS) to one eye and conventional phacoemulsification (CP) to the other, was performed. The recorded pupil images were evaluated at pre and post laser treatment (after suction release) and at several surgical timepoints for both techniques (FLACS and CP). Pupil areas were calculated and compared in the same eye undergone FLACS (pre vs post laser treatment), between eyes (CP vs FLACS) in the same patient and between groups. Subgroups were built regarding age and ocular comorbidity.
Results: This study involved a total of 164 eyes of 82 patients (55 female, 27 male). No statistical differences regarding the total duration of surgery (p=0.805) between FLACS and CP. Pupil measurements between pre and post laser treatment in the FLACS group showed no statistically significant differences (p=0.107). The mean change in pupil area from the beginning until the end of surgery (total variation) was 6.59± 2.08 mm2 in the FLACS group and 6.67± 2.13 mm2 in the CP group, associated to less narrowing of pupil area with FLACS, although not statistically significant (p=0.080). Comorbidity group analysis revealed less, but not significant, pupil narrowing with the FLACS technique (p=0.071). No statistically significant differences between FLACS and CP concerning age subgroups were registered.
Conclusion: This study shows no significant pupil changes, namely myosis, after low-energy FLACS pre-treatment. Comparison between techniques showed less pupil variation in FLACS as compared to CP, more markedly in eyes with comorbidities (particularly with shallow anterior chamber), although non-statistically significant.
Keywords: low energy femtosecond laser, FLACS, myosis, pupil, phacoemulsification
Introduction
Femtosecond laser-assisted cataract surgery (FLACS) emerged as a novel technique in 2009.1,2 Since then, this technique has evolved considerably, covering several of the conventional surgical steps previously performed in a manual manner (incisions, lens fragmentation, and capsulotomy). The safety and effectiveness of FLACS is consensually established, with considerable evidence.3–5 However, intraoperative miosis has been associated with femtosecond laser-assisted cataract surgery,6–8 which renders inherent difficulties regarding nuclear fragmentation, cortex removal, intraocular implantation of the lens, and increases the risk of posterior capsule rupture.9 This undesired side effect is frequently reported in the vast majority of publications regarding FLACS, which, almost invariably, do not differentiate femtosecond laser based on the pulse pattern, i e, between low and energy pulse femtosecond lasers or do not contemplate low energy pulse at all.10,11
As pointed out by Wu et al12 there are different femtosecond laser devices, generating different pulse patterns, in terms of energy and frequency levels. Most commercially available devices produce high energy (µJ) and low frequency (KHz) pulses; this type of common, femtosecond emission, is driven by chirped pulse amplification (CPA). On the other hand, another type of device produces low energy (nJ) and high frequency (MHz) femtosecond pulses by means of increasing the laser focusing optics’ aperture,13 therefore diminishing the laser spot diameter. The prevalence (in number and magnitude) of miosis with “high-energy” pulse femtosecond lasers has been shown to range between 9.5% and 32%.14,15 There is some evidence that the level of femtosecond laser cutting side effects are associated with prostaglandins release; these higher levels of prostaglandins (measured immediately after the laser pre-treatment), in turn, is accountable for the observed intraoperative myosis.16,17 Oppositely to the aforementioned “mainstream” reports, the few studies regarding pupillary changes with low energy pulse femtosecond lasers, show increasing evidence of minimal to absent narrowing of pupil size.18,19 This difference in behaviour may be related to the laser spots diameter and energy level, with smaller values achieved by “low-energy” devices, thus reducing an associate damage to the neighbour tissues. This fact is prone to reduce prostaglandins levels and, consequently, no significant intraoperative pupil narrowing.
Our present study aims to further investigate on the pupil area changes with low energy pulse FLACS and compare it against the standard phacoemulsification. For this matter, an intraindividual study was performed.
Materials and Methods
This retrospective cohort study was approved by the Ethics Committee at Hospital da Luz Arrabida (HLA), Porto, and adhered to the ethical principles stated in the “Declaration of Helsinki”, with each patient having signed an informed consent. Data were extracted from the charts of all patients who had cataract surgery in both eyes, with randomly assigned conventional phacoemulsification surgery in one eye and femtosecond laser–assisted surgery in the other eye. All patients had surgery between February 2015, and September 2020, at Hospital da Luz Arrabida (HLA). Two cataract and refractive surgeons performed all surgeries at HLA.
Inclusion and Exclusion Criteria
Patients were excluded from the study if they had previous corneal scarring, ocular surgery other than cataract surgery, or relevant axial anisometropia (defined as a ≥ 1 mm-difference in axial length between eyes of the same patient).
Chart Review and Data Collection
Charts were reviewed from surgeries performed between February 2015 and September 2020, and extraction was performed of demographic, clinical, and video recording data such as age, sex, date, type of surgery (conventional phacoemulsification versus femtosecond laser-assisted), procedure’s duration, axial length, anterior chamber depth, cataract degree, ocular comorbidity, surgical videos, and adverse events. Optical interferometer Galilei G6 (Ziemer Ophthalmic systems AG) was used for biometry. Assessment of lens transparency was achieved by examination at the slit lamp followed by a grading procedure according to the Lens Opacities Classification System (LOCS) III. A Placido - dual Scheimpflug device (Galilei G6) was used for corneal tomography and topography assessment. Macular evaluation, by means of spectral-domain optical coherence tomography, was accomplished by a modular ophthalmic imaging platform (Carl Zeiss).
For pupil measuring purposes, recorded images from surgical videos were withdrawn at several time points: (1) at the beginning of both CP and FLACS (immediately before laser docking), (2) immediately after the vacuum suction release (end of femtosecond laser pre-treatment) in the FLACS group, (3) at 5 minutes intraoperatively, (4) at 10 minutes intraoperatively, and (5) at the end of the surgical procedure.
Surgical Technique
Two experienced surgeons (R.S., A.M.). performed all surgeries. The femtosecond laser-assisted lens surgery was performed with a LDV Z8 (Ziemer, Inc., Port, Switzerland) device. Capsulotomy, corneal incisions and lens fragmentation were accomplished by femtosecond laser, with the phacoemulsification device being used for the subsequent steps, such as emulsification, irrigation and aspiration of lens material. FLACS was sequentially performed (femtosecond laser followed by the phacoemulsification) keeping the patient on the same operating bed and in the same operating theatre, as the FS platform employed is a portable one. The phacoemulsification device employed was the Active Fluidics™ torsional phacoemulsification machine (Centurion Vision, Alcon Laboratories, Inc., Fort Worth, USA). All surgeries were unilateral, with one eye at a time. Surgical protocol was the same for both surgeons.
Preparation protocol of was the same for both groups of patients, ie, tropicamide 0.28 mg in association with phenylephrine hydrochloride 5.4 mg contained in the form of an ophthalmic insert, with placement in the lower conjunctival sac and oxybuprocaine hydrochloride 4 mg/l eyedrops 20 minutes before procedure. No specific medication for myosis prevention was administered in the femtosecond group, nor additional steroid or non-steroid anti-inflammatory drugs (NSAID) were administered in the preoperative period to any of the patients. This specific protocol, without preoperative use of NSAID drugs (as this use is currently regarded as a standard practice) was explained to all patients, with given consent by each one of them. Although available as a backup measure, no intraoperative agents, like intracameral mydriatic mixtures, needed to be administered. Intracameral cefuroxime was injected in every patient at the end of each surgery.
In the FLACS group, vacuum suction was set at approximately 420 mbar and the following laser procedures were performed: lens fragmentation (in six pieces with a 6-mm diameter) at 105% laser energy, corneal incisions (main of 2.8 mm and secondary paracentesis of 1.2 mm) and capsulotomy (5.2-mm diameter) at 90% laser energy. Further surgical steps followed immediately after suction release (phacoemulsification device employed for emulsification, irrigation, and aspiration of lens material) and were performed in the same way for both groups (FLACS and CP).
All patients were prescribed with prednisolone, ibuprofen and ofloxacin eyedrops postoperatively for 3 weeks.
Pupil Area Measurement
Pupil area was measured at the established time points, after analysing images from the recorded surgical videos. For that purpose, we have adopted the Fiji image processing program from ImageJ (software version 2.0.0-rc-49/1.51a) as suggested by Mirshahi et al,18 which enables direct area measurements by tracing pupil margin. Calibration was accomplished by using the constant limbus horizontal size as a reference, allowing pixel measurements conversion into millimetres for each eye.
Statistical Analysis
The analysis involved the examination of possible differences in pupil area from the baseline preoperative measurement and along the different timepoints, comparing both techniques intraindividually (within subjects) and interindividually (between subjects). Subgroup analysis was also performed to evaluate pupil area changes with respect to age and comorbidity.
Regarding pupil change pre-laser versus post-laser treatment in the FLACS group of eyes, a paired t-test was applied. Comparison of pupil size between the FLACS and CP in the same patient (within-subject) at each time point was accomplished by a paired t-test.
Differences in pupil size between groups at different times were compared using analysis of variance (ANOVA). A mixed-design ANOVA was applied, considering pathology (yes or no) and type of pathology (when associated) as a between-subjects factor. Regarding the within-subjects’ factors, type of surgery (FLACS or CP) and time were used. Before the analysis, the sphericity assumption was tested using the Mauchly’s Test, and when the assumption was not accomplished, the Greenhouse-Geisser correction results were reported.
A statistical significance level of α=0.05 and a power of 95% were chosen, with P-values < 0.05 being considered statistically significant. All statistical analyses were performed using SPSS (Statistical Package for the Social Sciences, version 28, Chicago, Illinois).
Results
Preoperative Patient Data
The study population consisted of 164 eyes of 82 patients, with 55 female (67%) and 27 male (33%), and a mean age of 73.4 ± 8.5 years (median: 74, range: 55–95). For each patient, one of the eyes underwent FLACS and the other was operated with CP; therefore, in the total population, 82 eyes (50%) had femtosecond laser-assisted surgery and 82 eyes (50%) underwent conventional phacoemulsification.
Table 1 shows the patients’ preoperative characteristics by technique group. There was no statistically significant difference between the 2 groups preoperatively.
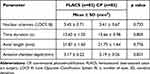 |
Table 1 Patient Demographic and Clinical Characteristics |
Preoperatively, the pupil area after dilation presented no statistically significant difference between the techniques, with 45.01±7.60 mm2 in the FLACS group and 45.00±7.60 mm² in the CP group (p=0.748). Comorbidity, as shown in Table 2, was present in 47 eyes (28.7%) of 23 patients and distributed as follows: glaucoma and pseudo exfoliation in 22 eyes (13.4%); shallow (<2.5 mm depth) anterior chamber in 10 eyes (6%), mild non-proliferative diabetic retinopathy in 8 eyes (4.8%), Fuchs dystrophy in 4 eyes (2.4%), high myopia in 2 eyes (1.2%), and post-retinal central venous thrombosis in one eye (0.6%). No adverse events were registered.
 |
Table 2 Comorbidity |
Postoperative Data
In the FLACS group, pupil area comparison between pre and post laser treatment showed no statistically significant differences (p=0.107, 95% CI (Confidence Interval): −0.01 to 0.05), with a mean value of 45.01±7.60 mm2 and 44.98±7.61 mm2, respectively (Figure 1). The mean change in pupil area between preoperative and post-laser treatment was 0.02 ± 0.12 mm2 (median: 0.01, minimum: −0.02, maximum: 1).
 |
Figure 1 Means ± standard deviations of preoperative and post-laser pupil areas in 82 eyes undergoing low-energy femtosecond laser assisted cataract surgery (FLACS). |
Regarding the comparison between FLACS and CP, pupil area measurements were performed along surgical timepoints for both techniques (Figure 2). The intraindividual analysis (within-subjects) revealed a marked difference, close to the limit of significance, between FLACS and CP techniques at the end of surgery, with a mean pupilar area of 38.41±7.01 mm2 and 38.33±7.04 mm2, respectively (p=0.051). More distinctly, a statistically significant difference between the techniques was shown at 10 minutes intraoperatively, with a slightly larger pupil in the FLACS group (mean difference of 0.09±0.38 mm²) as opposed to CP (p=0.032, CI: 0.01 to 0.17).
The mean change in pupil area from the beginning until the end of surgery (total variation) was 6.59±2.08 mm2 in the FLACS group and 6.67±2.13 mm2 in the CP group; the mean difference between the two techniques was 0.07 ± 0.38 mm², associated to less narrowing of pupil area with FLACS, although not statistically significant (p=0.080) (Table 3).
 |
Table 3 Comparison of Mean Pupilar Area Along Surgical Timepoints Between FLACS and CP |
Pupil narrowing was correlated positively with the duration of surgery, being similar in both techniques (R=−0.401 and R=−0.426; p<0.001).
Concerning the comparison of total pupil variation between techniques in eyes with ocular comorbidities versus eyes without ocular morbidities (as a between-subject factor), a non-statistically significant difference of 0.07±0.04 mm2, although close to the limit of significance, was shown (p=0.071; 95% CI: −0.01 to 0.16]). When comorbidity was present, the mean difference between techniques in total pupil variation was 0.19±0.59 mm2, with less narrowing in the FLACS group, but not statistically significant (p=0.131, 95% CI: −0.06 to 0.44), whereas in eyes without comorbidity, the mean difference between techniques was 0.03±0.22 mm2 (p=0.391, 95% to CI: −0.03 to 0.08) (Figure 3).
Regarding the comorbidity subgroups analysis, the pseudo exfoliation syndrome subgroup showed the higher degree of myosis during surgery amongst all subgroups, which was similar for both techniques (p=0.614) (Table 4). However, comparison between the two techniques revealed a mean difference of 0.78±0.95 mm² (p=0.176), close to the limit of significance, in eyes with shallow anterior chamber, associated with a lesser pupil narrowing in the FLACS group.
 |
Table 4 Comparison of Total Pupil Variation Between FLACS and CP According to Comorbidity |
Two subgroups were created, considering the median age (74 years old). In eyes of patients aged ≤74 years, the mean difference in pupil variation between techniques was 0.06±0.44 mm² (p=0.379), whereas the mean difference in pupil variation was 0.09±0.28 mm² in eyes of patients above 74 years old, close to the limit of significance (p=0.058). An independent t-test (between-subjects) comparing the two age subgroups (above and below 74 years of age), showed no statistically difference significance between FLACS and CP (p=0.716).
Discussion
To this point, no other intraindividual study comparing low-energy femtosecond laser with conventional phacoemulsification was performed regarding pupil area variation.
The vast majority of publications approach mainly high-energy femtosecond laser devices, with strong evidence of laser-induced myosis by this type of laser.20,21 On the other hand, some recent evidence is being apparent that low-energy femtosecond laser does not induce such narrowing of the pupil.22
Our study’s results agree with the published literature regarding the same type of femtosecond pulse.18,19,22 No significant pupil changes were observed in the present study with low-energy FLACS, in contrast with the reported common association of laser-induced myosis with high-energy and low-frequency femtosecond pulse machines available in the market.23,24 Again, the rationale for this difference may be that smaller laser spots, as produced by a high numerical aperture in the laser optics of “low-energy” devices, would reduce associate damage to the neighbouring tissues. Consequently, this weaker impact would translate into a lower prostaglandins level, and thus producing lesser intraoperative myosis.
Aside from tissue interaction, another aspect may contribute to the loss of preoperative mydriasis, such as the patient transfer time. This transfer process is mandatory for most platforms using high-energy pulse,25,26 since the related FS machines are not portable; in contrast, portability is a feature of the low-energy pulse platform available in the market. Similarly, in our study, no complications regarding capsule-related events were observed; namely, no incomplete capsulotomies, anterior capsular tags, and anterior or posterior capsular tears were registered. This evidence is opposed to most reviews’ conclusions about FLACS, but it should stressed that these reports neither contemplate “low-energy” devices or, if included, differentiate between the two types of femtosecond pulse.10,11,27
This study found some differences in pupil area variation between FLACS and CP along surgical time (timepoints), although not statistically significant. Reports of a significant higher pupil area with FLACS immediately after suction,19 were not apparent in our study. In those studies, anti-inflammatory eye drops were placed preoperatively on the eye population. It should be stressed that opposed to such reports, no anti-inflammatory drug was administered in any of our study eyes. Therefore, no potential bias in laser interaction on ocular tissues due to the myosis inhibition’s role of such drugs was registered in the present study.
The findings regarding a greater amount of pupil narrowing in eyes with comorbidities during conventional cataract surgery are consistent with the published literature. Nevertheless, the present study further reveals that there is a strong but non-statistically significant difference in eyes with a shallow anterior chamber (<2.5 mm), between FLACS and CP. A possible explanation for this difference may rely on the fact that the time of anterior chamber exposure with CP is longer than with FLACS (as several surgical steps are performed with a “closed” eye globe, through laser). This, in turn, would facilitate reflective myosis upon “open-eye” manipulation with CP.
In this study, surgical procedure time (from beginning to the end), was similar in both techniques, with no statistically significant difference between FLACS and CP (p>0.05); the portability of the employed femtosecond machine may contribute to this aspect, as the patient remains in the same surgical environment (same bed and a single operating room) during the whole femtosecond-phacoemulsification sequence. Our study results are in agreement with few other published reports,28 regarding the negligible impact on surgical time associated to portable femtosecond devices.
Conclusion
In conclusion, this intraindividual study provides extended evidence of lack of laser-induced myosis with low-energy FLACS. Furthermore, regarding pupil status, low-energy femtosecond laser-assisted energy seems to compare favorably with conventional phacoemulsification in the presence of certain ocular comorbidities. Although not statistically significant, this difference arises an interesting discussion and, also in line with contemporary literature, it recommends revision of some established, global opinions on FLACS. Further studies on low-energy femtosecond laser-assisted cataract surgery, involving higher samples and rigorous variable control, are in demand for this matter.
Acknowledgments
João Duarte Reis, MSc, Biostatistics, Coimbra, Portugal, provided statistical support.
Disclosure
The authors have no financial conflicts of interest to disclose.
References
1. Nagy Z, Takacs A, Filkorn T, Sarayba M. Initial clinical evaluation of an intraocular femtosecond laser in cataract surgery. J Refract Surg. 2009;25:1053–1060. doi:10.3928/1081597X-20091117-04
2. Mastropasqua L, Toto L, Mastropasqua A, et al. Femtosecond laser versus manual clear corneal incision in cataract surgery. J Refract Surg. 2014;30:27–33. doi:10.3928/1081597X-20131217-03
3. Grewal DS, Schultz T, Basti S, Dick HB. Femtosecond laser-assisted cataract surgery–current status and future directions. Surv Ophthalmol. 2016;61:103–131. doi:10.1016/j.survophthal.2015.09.002
4. Dick HB, Schultz T. A review of laser-assisted versus traditional phacoemulsification cataract surgery. Ophthalmol Ther. 2017;6:7–18. doi:10.1007/s40123-017-0080-z
5. Mastropasqua L, Toto L, Mattei PA, et al. Optical coherence tomography and 3-dimensional confocal structured imaging system-guided femtosecond laser capsulotomy versus manual continuous curvilinear capsulorhexis. J Cataract Refract Surg. 2014;40:2035–2043. doi:10.1016/j.jcrs.2014.05.032
6. Nagy ZZ, Takacs AI, Filkorn T, et al. Complications of femtosecond laser-assisted cataract surgery. J Cataract Refract Surg. 2014;40:20–28. doi:10.1016/j.jcrs.2013.08.046
7. Roberts TV, Lawless M, Bali SJ, Hodge C, Sutton G. Surgical outcomes and safety of femtosecond laser cataract surgery: a prospective study of 1500 consecutive cases. Ophthalmology. 2013;120:227–233. doi:10.1016/j.ophtha.2012.10.026
8. Diakonis VF, Yesilirmak N, Sayed-Ahmed IO, et al. Effects of femtosecond laser-assisted cataract pretreatment on pupil diameter: a comparison between three laser platforms. J Refract Surg. 2016;32:84–88. doi:10.3928/1081597X-20151229-03
9. Hashemi H, Seyedian MA, Mohammadpour M. Small pupil and cataract surgery. Curr Opin Ophthalmol. 2015;26:3–9. doi:10.1097/ICU.0000000000000116
10. Ewe SY, Abell RG, Vote BJ. Femtosecond laser-assisted versus phacoemulsification for cataract extraction and intraocular lens implantation: clinical outcomes review. Curr Opin Ophthalmol. 2018;29:54–60. doi:10.1097/ICU.0000000000000433
11. Lundstrom M, Dickman M, Henry Y, et al. Femtosecond laser-assisted cataract surgeries reported to the European registry of quality outcomes for cataract and refractive surgery: baseline characteristics, surgical procedure, and outcomes. J Cataract Refract Surg. 2017;43:1549–1556. doi:10.1016/j.jcrs.2017.09.029
12. Wu BM, Williams GP, Mehta JS, Mehta JS. A comparison of different operating systems for femtosecond lasers in cataract surgery. J Ophthalmol. 2015;2015:616478. doi:10.1155/2015/616478
13. Chang JS, Chen IN, Chan WM, Ng JC, Chan VK, Law AK. Initial evaluation of a femtosecond laser system in cataract surgery. J Cataract Refract Surg. 2014;40:29–36. doi:10.1016/j.jcrs.2013.08.045
14. Diakonis VF, Kontadakis GA, Anagnostopoulos AG, et al. Effects of short-term preoperative topical ketorolac on pupil diameter in eyes undergoing femtosecond laser-assisted capsulotomy. J Refract Surg. 2017;33:230–234. doi:10.3928/1081597X-20170111-02
15. Jun JH, Hwang KY, Chang SD, Joo CK. Pupil-size alterations induced by photodisruption during femtosecond laser-assisted cataract surgery. J Cataract Refract Surg. 2015;41:278–285. doi:10.1016/j.jcrs.2014.10.027
16. Jun JH, Yoo YS, Lim SA, Joo CK. Effects of topical ketorolac tromethamine 0.45% on intraoperative miosis and prostaglandin E2 release during femtosecond laser-assisted cataract surgery. J Cataract Refract Surg. 2017;43:492–497. doi:10.1016/j.jcrs.2017.01.011
17. Schultz T, Joachim SC, Stellbogen M, Dick HB. Prostaglandin release during femtosecond laser-assisted cataract surgery: main inducer. J Refract Surg. 2015;31:78–81. doi:10.3928/1081597X-20150122-01
18. Mirshahi A, Ponto K. Changes in pupil area during low-energy femtosecond laser-assisted cataract surgery. J Ophthalmic Vis Res. 2019;14(3):251–256. doi:10.18502/jovr.v14i3.4780
19. Germano C, Germano R, Cid F, Germano FA, Carricondo P, Germano J. Comparison of pupillary diameter variation between conventional phacoemulsification versus femtosecond laser-assisted cataract surgery. Arq Bras Oftalmol. 2022;85(1). doi:10.5935/0004-2749.20210091
20. Wang J, Su F, Wang Y, Chen Y, Chen Q, Li F. Intra and post-operative complications observed with femtosecond laser-assisted cataract surgery versus conventional phacoemulsification surgery: a systematic review and meta-analysis. BMC Ophthalmol. 2019;19(1):177. doi:10.1186/s12886-019-1190-2
21. Popovic M, Campos-Möller X, Schlenker MB, Ahmed II. Efficacy and safety of femtosecond laser-assisted cataract surgery compared with manual cataract surgery: a meta-analysis of 14 567 eyes. Ophthalmology. 2016;123(10):2113–2126. doi:10.1016/j.ophtha.2016.07.005
22. Mirshahi A, Schneider A, Latz C, Ponto KA. Perioperative pupil size in low-energy femtosecond laser-assisted cataract surgery. PLoS One. 2021;16(5):e0251549. PMID: 33999970; PMCID: PMC8128224. doi:10.1371/journal.pone.0251549
23. Walter K, Delwadia N, Coben J. Continuous intracameral phenylephrine-ketorolac irrigation for miosis prevention in femtosecond laser-assisted cataract surgery: reduction in surgical time and iris manipulation. J Cataract Refract Surg. 2019;45:465–469. doi:10.1016/j.jcrs.2018.11.004
24. Schultz T, Joachim SC, Szuler M, Stellbogen M, Dick HB. NSAID pretreatment inhibits prostaglandin release in femtosecond laser-assisted cataract surgery. J Refract Surg. 2015;31:791–794. doi:10.3928/1081597X-20151111-01
25. Roberts H, Wagh VK, Mullens IJM, Borsci S, Ni MZ, O’Brart DPS. Evaluation of a hub-and-spoke model for the delivery of femtosecond laser assisted cataract surgery within the context of a large randomised controlled trial. Br J Ophthalmol. 2018;102(11):1556–1563. doi:10.1136/bjophthalmol-2017-311319
26. Lubahn JG, Donaldson KE, Culbertson WW, Yoo SH. Operating times of experienced cataract surgeons beginning femtosecond laser-assisted cataract surgery. J Cataract Refract Surg. 2014;40:1773–1776. doi:10.1016/j.jcrs.2014.03.024
27. Roberts HW, Wagh VK, Sullivan DL, et al. A randomized controlled trial comparing femtosecond laser-assisted cataract surgery versus conventional phacoemulsification surgery. J Cataract Refract Surg. 2019;45(1):11–20. doi:10.1016/j.jcrs.2018.08.033
28. Yu AY, Ni LY, Wang QM, et al. Preliminary clinical investigation of cataract surgery with a noncontact femtosecond laser system. Lasers Surg Med. 2015;47:698–703. doi:10.1002/lsm.22405
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.


