Back to Journals » Journal of Multidisciplinary Healthcare » Volume 17
Progress in the Application of Lung Ultrasound for the Evaluation of Neonates with Respiratory Distress Syndrome
Received 28 September 2023
Accepted for publication 13 December 2023
Published 3 January 2024 Volume 2024:17 Pages 1—9
DOI https://doi.org/10.2147/JMDH.S442464
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Scott Fraser
Ling-Yun Bao,* Xin-Yue Dao,* Kun Du
Department of Neonate, Kun Ming Children’s Hospital, Yunnan, 650021, People’s Republic of China
*These authors contributed equally to this work
Correspondence: Kun Du, Department of Neonate, Kun Ming Children’s Hospital, No. 28 of Shulin Road, Yunnan, 650021, People’s Republic of China, Tel +86 15388843393, Email [email protected]
Abstract: Neonatal respiratory distress syndrome (NRDS) is a common critical disease in neonates. Early diagnosis and timely treatment are crucial. Historically, X-ray imaging was the primary method for diagnosing NRDS. However, this method carries radiation exposure risks, making it unsuitable for dynamic lung condition monitoring. In addition, neonates who are critically ill require bedside imaging, but diagnostic delays are often unavoidable due to equipment transportation and positioning limitations. These challenges have been resolved with the introduction of lung ultrasound (LUS) in neonatal intensive care. The diagnostic efficacy and specificity of LUS for NRDS is superior to that of X-ray. The non-invasive, dynamic, and real-time benefits of LUS also allow for real-time monitoring of lung changes throughout treatment for NRDS, yielding important insights for guiding therapy. In this paper, we examine the ultrasonographic characteristics of NRDS and the recent progress in the application of ultrasound in the diagnosis and treatment of NRDS while aiming to promote wider adoption of this method.
Keywords: dynamic monitoring, lung ultrasound, neonates, respiratory distress syndrome, NRDS, point of care ultrasound
Introduction
In clinical practice, neonatal respiratory distress syndrome (NRDS) is linked to a spectrum of etiological factors, encompassing prematurity, gestational diabetes, and elective cesarean section. The onset of this syndrome occurs shortly following birth and is attributed to an insufficiency in pulmonary surfactant (PS). Manifesting clinically with symptoms such as tachypnea, grunting or nasal flaring, cyanosis, and the presence of the three concave signs, NRDS exhibits a progressive and pathophysiological trajectory marked by the development of hyaline membranes. This condition constitutes a substantial contributor to neonatal mortality. For a long time, bedside chest X-ray examination has been considered the gold standard for diagnosing NRDS due to the inability of CT to perform bedside examination, but X-ray examination has obvious limitations, manifested as: (1) Children with NRDS usually have severe dyspnea and need mechanical ventilation, and lung ventilation/perfusion abnormalities usually occur in the back due to prolonged supine and gravity effects, while bedside x-rays can only be performed in the supine position, which may mask back lesions due to overlapping images, resulting in missed diagnosis. (2) Bedside radiography requires moving the machine and placing the child in the appropriate position for radiography, which takes time and may delay diagnosis. In addition, moving critically ill children may cause adverse events such as temperature fluctuations and displacement of tracheal tubes/oxygen masks, which may aggravate the condition. (3) Bedside X-ray is difficult to complete the dynamic monitoring of pulmonary disease changes, especially when the disease changes suddenly need to be checked, and its limitations are more obvious. (4) Radiation damage is difficult to avoid completely, which has a potential high risk of DNA damage and cancer. Because radiation damage is more sensitive to cells in the differentiation stage, it may cause greater potential harm to newborns and premature infants in the rapid development stage. In particular, it is difficult to estimate the cumulative dose of primary and passive radiation damage during hospitalization for severely ill newborns and immature premature infants in neonatal intensive care units (NICU) who are frequently exposed to radiation due to lung disease or other medical conditions. Thus, the search for alternative methods has been ongoing. In 1990, Avni et al1 reported for the first time the application of pulmonary ultrasound in the diagnosis of NRDS, and claimed that ultrasound may replace chest radiography. Since then, the neonatal lung ultrasound has been widely used. Ultrasound can accurately and easily identify NRDS,2 transient neonatal respiratory hypertrophy (TTN),3 meconium aspiration syndrome (MAS),4 neonatal pneumonia,5 and pneumothorax.6 Compared with X-ray, ultrasound has higher accuracy and specificity in diagnosing a variety of neonatal lung diseases, including NRDS.7 In 2020, the European Association of Paediatrics and Neonatal Intensive Care published International Evidence-based Guidelines on point-of-care ultrasound for critically ill neonates and children.8 Pulmonary ultrasound is increasingly used in neonatal intensive care unit (NICU) due to its high specificity and sensitivity in the diagnosis of lung lesions, real-time dynamic monitoring, no radiation and convenient operation. It plays an important role in the diagnosis and treatment of NRDS. It can not only be used in the diagnosis and differential diagnosis of NRDS but also can dynamically monitor the therapeutic effect of NRDS and guide treatment. In this paper, the application of pulmonary ultrasound in NRDS in recent years is reviewed, by searching the keywords in EMBASE, PubMed and Cochrane Central from 2015 to 2022. Duplicate literature and literature lacking exact data support for ultrasound diagnosis of NRDS were excluded.
Common LUS Terminologies and Imaging Manifestations in NRDS
Pleural line
This is a strong echogenic reflection caused by the difference in acoustic impedance between the pleura and the lung surface. It appears as a smooth, clear, and regular linear echo on ultrasound. Anomalies include a missing pleural line, rough or blurred appearance, irregularities, or continuous interruptions.9
Lung sliding
During lung respiration, real-time ultrasonography reveals a horizontal relative sliding movement between the visceral and parietal pleura when the ultrasound probe is scanned perpendicular to the ribs. This motion is known as “lung sliding”.9
A-line
When the ultrasound beam is perpendicular to the pleura, a strong echogenic linear reflection is produced. Located below the pleural line and parallel to it, these reflections have equal spacing between them and appear similar to bamboo node patterns. Their echoes gradually diminish from superficial to severe until they disappear.9
B-Line, Confluent B-Line, Alveolar-Interstitial Syndrome (AIS)
B-line is a linear echogenic reflection that originates from the pleural line, is perpendicular to it, radiates outwards into the deep lung field, and extends without attenuation to the edge of the scanning screen. Clinically, its presence indicates an increase in the water content within the lung tissue. When densely packed B-lines are visible within an intercostal space but the echogenicity of the ribs remains clear, such dense B-lines are referred to as confluent B-lines. If two or more intercostal spaces within a scanning area exhibit confluent B-lines, the condition is known as AIS.9
Compact B-Line and “White Lung”
If excessively dense B-lines are present bilaterally in every lung field and the rib shadows have essentially disappeared, this is referred to as a compact B-line. If each scanning area of both lungs reveals dense B-lines, the condition is known as “white lung”.9
Lung Consolidation, Air Bronchogram Sign, and Lung pulse
Lung consolidation refers to lung tissue that appears hepatized (similar to the liver) on an ultrasound image. This may be accompanied by the air bronchogram sign or fluid bronchogram sign. In severe cases, real-time ultrasonography may reveal a dynamic air bronchogram sign. Within the area of consolidation, the air bronchogram sign appears as a series of echogenicities that are either dot-like or linear in shape. On real-time ultrasonography, the consolidated lung tissue can be seen pulsating with the heartbeat when the extent of the lung consolidation is substantial and severe enough to be close to the edge of the heart. This method is known as lung pulse.9
Shred sign
This ultrasonographic manifestation is known as the shred sign and occurs when the boundary between consolidated lung tissue and aerated lung tissue is unclear.9
Lung point
As respiration continues, the lung point is the boundary where lung sliding is alternately seen and not seen on real-time ultrasonography.9
Double Lung point
On the LUS image, a distinct boundary can be formed between the upper and lower lung fields due to variations in the degree or nature of a lesion.9
Sandybeach Sign & Stratosphere sign
In M-mode ultrasonography, a distinctive ultrasound image resembling a sandybeach appears. This consists of a wavy linear high echogenicity above the pleural line, the pleural line itself, and the uniform fine granular echoes produced by lung sliding below the pleural line. This symbol is known as the sandybeach sign or seashore sign. When lung sliding disappears, the granular dot-like echoes beneath the pleural line are replaced by a series of parallel lines known as the bar code sign or barcode sign.9
Ground-Glass Opacity sign
The ground-glass sign is an ultrasound image that appears similar to frosted glass. It indicates mild lung consolidation in which the air bronchogram sign is not yet pronounced.9
Snowflake sign
The snowflake sign is an ultrasound image resembling a snowflake. A distinct air bronchogram sign represents consolidation of the lungs.9
Pleural effusion
Pleural effusion is a collection of fluid that can accumulate within the pleural cavity (the space between the lung and the chest wall). On ultrasound imaging, pleural effusion is a dark area without echo.9
Neonatal NRDS LUS Examination and Diagnosis
LUS Examination Method
A linear array probe with a frequency of 9–14 MHz is used for LUS examinations of neonates. Examinations can be performed in the supine, prone, and lateral positions, or the position can be selected based on the location of the lesion. To prevent missing any sections of the lung during the examination, the lung is divided into anterior, lateral, and posterior zones based on the anterior axillary line and posterior axillary line. This divides each lung into three regions, resulting in a total of six regions using the 6-zone method. This results in a 12-zone method if further divisions are made at the level of the nipples on either side. Some clinicians further divide it into 14 zones by adding the parasternal line and the midline at the back.7 Due to the small body surface area and lung volume of neonates, the 6-zone method is frequently used. The longitudinal scanning method (with the probe perpendicular to the ribs) is the most common method, while transverse scanning (with the probe parallel to the intercostal spaces) can be used to investigate focal lesions as a supplementary method.10
Normal and NRDS LUS Findings
In normal neonates, B-mode ultrasonography reveals that the pleural line and A-line of the lung are both smooth, clear, and regular. Spaced equally and arranged in parallel, they form a “bamboo sign”. In M-mode ultrasonography, it presents as a “sandybeach sign”, whereas in real-time ultrasonography, it manifests as the “lung sliding” sign. There is no evidence of alveolar-interstitial syndrome, pleural effusion, or lung consolidation observed. A few B-lines may be seen after birth, but they disappear completely within 3–7 days. In neonates delivered prematurely, the presence of B-lines may exhibit prolonged persistence. The absence of pulmonary surfactant among newborns afflicted with NRDS leads to an elevation in alveolar surface tension, culminating in alveolar collapse and the onset of pulmonary edema. On ultrasound, this appears as lung consolidation with an air bronchogram sign, abnormal pleural lines, the absence of A-lines, double lung points, and alveolar-interstitial syndrome changes in non-consolidated areas, along with pleural effusion.10,11
NRDS LUS Diagnosis and Grading
Qualitative Diagnosis of NRDS Using LUS
In 1990, researchers first reported that the ultrasound image of neonates with NRDS revealed an echogenicity posterior to the liver. This echogenicity was proposed as a diagnostic indicator for NRDS. With the continuous development of ultrasound technology, its diagnostic advantages over X-ray for NRDS have become more evident. Researchers have recently found that ultrasound has a high sensitivity and specificity for diagnosing NRDS.12,13 When multiple ultrasound signs are present concurrently, the sensitivity and specificity can reach 100%. For instance, when lung consolidation, abnormalities in the pleural line, and diffuse pulmonary edema coexist, or when lung consolidation, abnormalities in the pleural line, and absence of the A-line coexist, the sensitivity and specificity for diagnosing NRDS are both 100%.14,15 Lung consolidation is an essential sign for diagnosing NRDS, especially when distinguishing it from transient tachypnea of the newborn (TTN). In severe cases, lung pulse may also be detected.16,17 An ultrasound may reveal that the degree and nature of lesions in both lungs of a neonate with NRDS can be inconsistent. For example, one lung may exhibit consolidation while the other does not. Similarly, different regions of the same lung can also display varying degrees and types of lesions, such as one region exhibiting consolidation and another exhibiting edema or pleural effusion. This contradicts the traditional concept derived from chest X-rays, which suggest that both lungs have a uniform ground-glass appearance.
Quantitative Diagnosis of NRDS Using LUS
Compared with other imaging tests, ultrasound relies more on the operator’s skill, understanding of the image, and familiarity with the patient’s condition. The ultrasonic image features of NRDS are common, but also vary with the course of the disease. When different doctors use ultrasound to judge the degree of disease, there is inevitably subjectivity, which is not conducive to the formation of a unified diagnostic standard and curative effect evaluation system. Therefore, some scholars put forward quantitative evaluation, namely ultrasonic scoring system. LUS scoring system can help to determine the severity of the condition.15 This scoring system was used for the first time in neonates in a 2015 prospective study conducted by the French researcher Brat.17 In their study, the lung was divided into six zones using the 6-zone method. Based on the presence of A-line, B-line, and lung consolidation on the ultrasound, a score ranging from 0 to 3 was assigned to each lung region (Table 1). The total score ranged between 0 and 18 points. This scoring method was used to quantitatively assess the efficacy of exogenous PS on continuous positive airway pressure (CPAP) in NRDS. When the LUS score was greater than 2 or 4, the probability of requiring PS increased from 21% to 39% in neonates ≥34 weeks of gestation and from 25% to 72% in those <34 weeks. In addition, for neonates with a gestational age <34 weeks, a score >4 predicted a 100% sensitivity for the need for PS.
 |
Table 1 Brat lung ultrasound scoring |
Using the Brat scoring system to direct NRDS treatment, researchers in China refined the lung zoning and modified the scoring for pulmonary edema ventilation conditions. Some researchers adopted a 12-zone division for the lungs, assigning a value between 0 and 3 to each lung zone (Table 2). The total score ranged between 0 and 36 points. The results suggested that a score of ≤10 could be used as a predictive value for successful extubation, with a sensitivity and specificity of 95% and 82%, respectively.
 |
Table 2 12-zone lung ultrasound scoring |
Some scholars have adopted the 14-zone 70-point scoring system for the lung. Compared to the Brat scoring system, this method emphasizes the extent of coalescent B-lines and includes an assessment of the pleural line. Each lung zone is scored from 0 to 5 (Table 3). Observations at 12, 24, 48, and 72 hours after PS replacement therapy revealed that the lung scores decreased gradually. Using a threshold of 40.5 to predict the risk of extubation failure, the sensitivity and specificity were determined to be 92.31% and 93.88%, respectively. If the score exceeds 40.5, the risk of extubation failure increases, suggesting immediate extubation is not advisable. In contrast, if the score is less than 40.5, it is advised to extubate as soon as possible in order to reduce the duration of mechanical ventilation. The consistent view among different ultrasound scoring systems is that the higher the score, the more severe the NRDS disease. The difference is that each system has different number of lung partitions, including different sonovisual features, clinical features and observation outcome indicators. However, the more partitions and the more indicators are included, the longer the inspection time and the larger the scope, which has been questioned by some scholars.18–20 They noted that the scoring systems require a thorough lung scan, which may not be suitable for critically ill patients. In addition, they noted that the systems do not clearly specify how to score when coalescent B-lines occupy intercostal spaces that are not within the scoring range, and that they tend to overlook the impact of the device, probe, and imaging method on A-line and B-lines. As a result, Liu et al21 believes that the clinical utility of such scoring systems is limited and does not warrant wider application. In conclusion, in the diagnosis and monitoring of NRDS, it is still controversial whether the sound and image characteristics are reliable or the scoring system is reliable. Both have advantages and disadvantages, but they are susceptible to operator subjectivity, and more objective evaluation methods need to be explored.
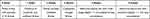 |
Table 3 14-zone lung ultrasound scoring |
Grading of NRDS Using LUS
Liu et al conducted a multicenter prospective study with 275 qualified cases.21 Based on clinical practice, they proposed a practical and operable NRDS LUS grading system and developed a consensus among experts.10 This system assigns a grade to RDS based on ultrasound manifestations and the incidence of severe complications. The grading is as follows: Mild refers to lung consolidation that appears as a ground-glass sign on ultrasound imaging and can affect all lung fields or only some intercostal spaces; moderate refers to lung consolidation on ultrasound imaging that appears as a snowflake sign but has not yet affected all lung zones; severe refers to any one or more of the following criteria: 1) On ultrasound, lung consolidation appears as a snowflake sign and has affected all lung zones; 2) The extent and range of lung consolidation, regardless of severity, has resulted in serious complications like pulmonary hemorrhage, pneumothorax, extensive atelectasis (affecting at least one lung zone), or persistent pulmonary hypertension. In comparison to chest X-ray grading, LUS grading specifically includes complications. This is more advantageous for treatment selection and is conducive to the proper management and enhanced prognosis of NRDS in its early stages. The method is simple and easy to learn and can be used to make diagnosis and appropriate clinical decision quickly.
Ultrasound Monitoring in NRDS Treatment
Ultrasound plays a significant role in monitoring the treatment of NRDS as indicated by research. LUS has demonstrated a high degree of dependability in monitoring the treatment with PSs and has advantages over chest X-rays. On ultrasound, NRDS primarily manifesting as pulmonary edema may not necessarily be treated with PS, while NRDS manifesting primarily as lung consolidation can be treated with PS.4 De Martino et al studied 133 neonates with RDS on continuous positive airway pressure (CPAP) therapy with a gestational age of ≤ 30 weeks.22 PS therapy was administered to these neonates based on the European guidelines.23 They recorded LUS scores using the Brat ultrasound scoring system before the administration of PS and then analyzed the diagnostic accuracy of the ultrasound score in predicting the need for PS therapy and the requirement for a second dose. In the study, 68 newborns received a single dose of PS, and 19 newborns received two doses. When the LUS score was >6 or >8, the likelihood of requiring PS therapy increased from 51% to 82% or 92%, respectively. The probability of needing a second dose of PS increased from 14% to 31% when the ultrasound score was >10. Overall, the predictive accuracy for the requirement of PS therapy and a second dose were 89% and 72%, respectively. Raschetti et al24 divided neonates with a gestational age of ≤32 weeks into two groups. In the control group, neonates with a gestational age of ≤28+6 weeks with a fraction of inspired oxygen (FiO2) of >0.3 or those with a gestational age of ≥29 weeks with FiO2 of >0.4, were administered PS within 72 hours of birth. PS therapy was administered to patients diagnosed with RDS in the experimental group either when FiO2 exceeded the mentioned values or when the LUS score was above 8 (whichever occurred first). Comparing the timeliness of PS administration between the two groups, a greater proportion of neonates in the experimental group received PS therapy within 3 hours of birth, increasing from 71.4% to 90%. In addition, the maximum FiO2 level was reached in the experimental group before administering PS, which was reduced from 0.4 to 0.33. Combining ultrasound with oxygenation status enhances both the accuracy and timeliness of predicting the need for PS, thereby reducing delays in optimal treatment times. In most infants who were administered PS, ultrasound findings revealed a reduction or even disappearance of lung consolidation, a decrease in B-lines, the return of lung sliding and A-lines, and a more regular pleural line.
Perri et al conducted a study on 56 neonates who were treated with CPAP.25 The Brat ultrasound scoring system was used to determine the early need for PS therapy, and the results were compared to chest X-rays. The results indicated that LUS offers higher sensitivity and specificity than chest X-rays. Furthermore, LUS demonstrated a superior positive predictive value (PPV) and negative predictive value (NPV). Zong et al noted in their research that there was a positive correlation between LUS scores obtain prior to and after PS administration and chest X-ray grading.15 De Martino et al used LUS scores to assess the efficacy of PS therapy and compared the results to those obtained from chest X-rays.23 Their findings pointed to a high level of consistency between the two methods.
In addition, the high sensitivity and specificity of LUS monitoring has proven useful for assessing extubation during mechanical ventilation. Various studies have found that neonates who failed extubation demonstrated signs of pulmonary edema and lung consolidation on LUS, even when pre-extubation chest X-rays revealed no obvious abnormalities. These neonates could be successfully extubated after appropriate interventions such as positioning and patting, restricting fluid intake, managing infections, and performing alveolar lavage.26 This highlights the importance of LUS in promptly identifying the causes of extubation failure in neonates with NRDS.
LUS in Diagnosing Complications of NRDS
NRDS can have various complications like pneumothorax, pulmonary hemorrhage, pneumonia, and bronchopulmonary dysplasia (BPD). Multiple studies have found that ultrasound has a significantly higher detection rate for the complications of NRDS than X-rays. This is consistent with the findings of Sawires et al, who determined that LUS is superior to chest X-rays for detecting NRDS-related complications.27
Pneumothorax
Pneumothorax ultrasound manifestations include the absence of lung sliding, the presence of the pleural line and A-line, the absence of the B-line, the presence of a lung point, and the bar code sign. In cases of extensive pneumothorax, however, the lung point may not be visible.6 In approximately 30% of pneumothorax cases, supine chest X-ray examinations miss the diagnosis. Although this rate can be reduced with upright chest X-rays, supine imaging is the norm for neonates. LUS can be performed in any position, and its diagnostic accuracy is significantly higher than that of chest X-rays, with high levels of specificity and sensitivity. Abdalla et al conducted a prospective study on neonates suspected of having pneumothorax and found that when three ultrasound signs were present simultaneously—the absence of lung sliding, the bar code sign, and the absence of B-line—the sensitivity, specificity, PPV, and NPV for diagnosing pneumothorax were all 100%, consistent with the findings of Abdalla W et al.28 Moreover, a study revealed that individual ultrasound signs are also useful in diagnosing neonatal pneumothorax.5 Both, the absence of lung sliding and the bar code sign had a sensitivity, specificity, and accuracy of 100%. The absence of B-line demonstrated 100% NPV, while the lung point revealed a sensitivity of 90.3% and specificity of 100%.29 Deng et al also reported that the absence of B-line, lack of lung sliding, and the presence of a lung point have sensitivities of 100%, 100%, and 94%, respectively, with specificities all being 100%.6 However, it is essential to note that relying on a single symptom may not yield accurate diagnoses. Conditions such as pleural adhesions, subcutaneous emphysema, and lung bullae for instance, can also show the absence of lung sliding and the bar code sign. In cases of extensive pneumothorax, a lung point may not be visible. Therefore, a comprehensive clinical analysis should be combined with these symptoms. When pneumothorax is clinically suspected, a pneumothorax diagnostic flowchart can help in making an accurate diagnosis.10
Pulmonary Hemorrhage
The sensitivity of LUS in diagnosing neonatal pulmonary hemorrhage has been demonstrated to be quite high. The shred sign, lung consolidation accompanied by the air bronchogram sign, and pleural effusion are the primary ultrasound characteristics upon which a diagnosis of pulmonary hemorrhage is based. Ultrasonographic manifestations of the primary lung disease may also include abnormalities in the pleural line, absence of the A-line, and AIS.11,30 The shred sign is the most prevalent ultrasonographic sign of pulmonary hemorrhage, among these, with a sensitivity of 91.2% and a specificity of 100% for diagnosing neonatal pulmonary hemorrhage.30 Ultrasonographic manifestations are proportional to the severity of pulmonary hemorrhage. In cases of mild hemorrhage, the shred sign may be predominant, while in cases of severe hemorrhage, the shred sign may be observed at the periphery of the consolidation zone.30 The range of lung consolidation accompanied with the air bronchogram sign correlates with the severity of the hemorrhage. Mild hemorrhages may only exhibit a localized consolidation just beneath the pleura, whereas more severe hemorrhages typically present with a larger consolidation area. The extent and range of consolidation may not be a direct manifestation of pulmonary hemorrhage as they are primarily associated with the underlying disease.31 However, it is important to note that while LUS has a high sensitivity for pulmonary hemorrhage, it lacks specificity. Similar ultrasonographic patterns can also be observed in other lung diseases.32 In cases where pulmonary hemorrhage is suspected, it is crucial to combine ultrasound findings with clinical manifestations for an accurate diagnosis.
Bronchopulmonary Dysplasia (BPD)
The ultrasonographic characteristics of BPD consist of pleural thickness, a coarse pleural line, diffuse AIS, post-diaphragmatic hyperechoic appearance, sub-diaphragmatic small cysts, and a rough diaphragmatic muscle. Among these, a coarse pleural sign is sensitive, while the presence of small cysts and a rough diaphragmatic muscle are highly specific indicators. Moreover, AIS is more prevalent in infants diagnosed with moderate and severe bronchopulmonary dysplasia.33 Liu et al reported that infants having “alveolar interstitial syndrome” within three days of birth and “shred sign” at 28 days post-birth are ultrasound characteristics that have predictive value for BPD.33 The sensitivity and specificity for these signs are 81.25% and 51.02% for AIS, and 31.25% and 97.96% for the “shred sign”, respectively. In their prospective study, Hansmann and Alonso-Ojembarrena, suggested that a LUS score of ≥5 within two weeks post-birth in extremely low birth weight infants can predict the onset of BPD.32,34 A score of ≥4 at four weeks post-birth can predict moderate to severe BPD, with a sensitivity and specificity of 74% and 100% for the former, and 100% and 80% for the latter. Furthermore, Liu et al conducted LUS examinations on patients clinically diagnosed with BPD and oxygen dependence for more than two months.3 They discovered that some of the patients had other conditions like atelectasis and pneumonia, indicating that LUS can be beneficial in clarifying the cause and management of the disease, particularly in patients diagnosed with BPD based solely on the duration of their oxygen dependence.
Although the advantages of ultrasound in the diagnosis, treatment effect and complication monitoring of NRDS have been confirmed by a large number of literatures, it still has limitations. For example: (1) Operators in different regions have not undergone unified training, and the performance of ultrasonic equipment used is different, which leads to the bias of inspection results, which is not conducive to the development of multi-center research; (2) Both ultrasound scoring and characterization of characteristic ultrasound images are subjective and may require more objective methods to evaluate them.
In conclusion, a large number of clinical practices have proved that X-ray radiography, which used to be the gold standard for the diagnosis of NRDS, has many shortcomings, including missed diagnosis and misdiagnosis due to the limitation of the position of radiography; the inability to dynamically monitor lung lesions due to radiation damage; the risk of aggravating the disease due to moving children during the imaging. The application of pulmonary ultrasound in the diagnosis and treatment of NRDS has better solved the above problems and provided us with a new understanding of the disease, which has greatly reduced the rate of missed diagnosis and misdiagnosis of NRDS and its complications, promoted the improvement of treatment strategies, such as the rational use of pulmonary surfactant and the reasonable application of invasive/non-invasive ventilation, etc., and improved the prognosis of children. Such as reducing the incidence of ventilator-associated pneumonia, bronchopulmonary dysplasia and so on. However, the difference of ultrasonic equipment performance, the difference of operator technology, and the difference of interpretation standards for ultrasonic results can affect the accuracy and comparability of inspection results. Therefore, the standardized training of ultrasound operators and the establishment of more objective results evaluation criteria will be more conducive to the promotion of the technology, so as to benefit more newborns.
Funding
Kunming Health Commission Health Research Project (NO.2022-06-03-007).
Disclosure
The authors report no conflicts of interest in this work.
References
1. Avni E, Braude P, Pardou A, Matos C. Hyaline membrane disease in the newborn: diagnosis by ultrasound. Pediatr Radiol. 1990;20:143–146. doi:10.1007/BF02012957
2. Brogi E, Bignami E, Sidoti A, et al. Could the use of bedside lung ultrasound reduce the number of chest x-rays in the intensive care unit? Cardiovasc Ultrasound. 2017;15(1):23. doi:10.1186/s12947-017-0113-8
3. Chen SW, Fu W, Liu J, et al. Routine application of lung ultrasonography in the neonatal intensive care unit. Medicine. 2017;96(2):e5826. doi:10.1097/MD.0000000000005826
4. Liu J, Fu W, Qin SJ. Lung ultrasound to guide the administration of exogenous pulmonary surfactant in respiratory distress syndrome of newborn infants: a retrospective investigation study. Front Pediatr. 2022;10:952315. PMID: 36340730; PMCID: PMC9635001. doi:10.3389/fped.2022.952315
5. Raimondi F, Rodriguez Fanjul J, Aversa S, et al. Lung ultrasound for diagnosing pneumothorax in the critically ill neonate. J Pediatr. 2016;175:74–78.e1. doi:10.1016/j.jpeds.2016.04.018
6. Deng BY, Li N, Wu WS, et al. Use of neonatal lung ultrasound for the early detection of pneumothorax. Am J Perinatol. 2020;37(9):907–913. PMID: 31146293. doi:10.1055/s-0039-1688999
7. Liu J, Xia RM, Ren XL, Li JJ. The new application of point-of-care lung ultrasound in guiding or assisting neonatal severe lung disease treatment based on a case series. J Matern Fetal Neonatal Med. 2020;33(23):3907–3915. PMID: 30835592. doi:10.1080/14767058.2019.1590332
8. Singh Y, Tissot C, Fraga MV, et al. International evidence-based guidelines on Point of Care Ultrasound (POCUS) for critically ill neonates and children issued by the POCUS Working Group of the European Society of Paediatric and Neonatal Intensive Care (ESPNIC). Crit Care. 2020;24(1):65. PMID: 32093763; PMCID: PMC7041196. doi:10.1186/s13054-020-2787-9
9. Liu J, Sorantin E, Cao HY.Neonatal Lung Ultrasonography. People’s Medical Publishing House. 2018.
10. The Society of Pediatrics, Asia-Pacific Health Association; The Division of Critical Ultrasound, Society ofPediatrics, Asia - Pacific Health Association; The World Interactive Network Focused On Critical Ulrasound China Branch. Expert consensus on ultrasound diagnosis and gradation of neonatal respiratory distress syndrome. Chin Pediatr Emerg Med. 2021;28(07):545–551.
11. Shao RJ, Du MJ, Xie JT. Use of lung ultrasound for the diagnosis and treatment of pleural effusion. Eur Rev Med Pharmacol Sci. 2022;26(23):8771–8776. PMID: 36524495. doi:10.26355/eurrev_202212_30548
12. Oktem A, Yigit S, Oğuz B, Celik T, Haliloğlu M, Yurdakok M. Accuracy of lung ultrasonography in the diagnosis of respiratory distress syndrome in newborns. J Matern Fetal Neonatal Med. 2021;34(2):281–286. PMID: 30957609. doi:10.1080/14767058.2019.1605350
13. Sharma D, Farahbakhsh N. Role of chest ultrasound in neonatal lung disease: a review of current evidences. J Matern Fetal Neonatal Med. 2019;32(2):310–316. doi:10.1080/14767058.2017.1376317
14. Jiang QX, Shi LJ, Shen LY, et al. Application value of a new lung ultrasound scoring method in neonatal respiratory distress syndrome treatment. Ultrasound Med Biol. 2022;48(2):275–282. PMID: 34782166. doi:10.1016/j.ultrasmedbio.2021.10.009
15. Ma H, Yan W, Liu J. Diagnostic value of lung ultrasound for neonatal respiratory distress syndrome: a meta-analysis and systematic review. Med Ultrason. 2020;22(3):325–333. doi:10.11152/mu-2485
16. Zong H, Huang Z, Zhao J, et al. The value of lung ultrasound score in neonatology. Front Pediatr. 2022;10:791664. PMID: 35633958; PMCID: PMC9130655. doi:10.3389/fped.2022.791664
17. Brat R, Yousef N, Klifa R, et al. Lung ultrasonography score to evaluate oxygenation and surfactant need in neonates treated with continuous positive airway pressure. JAMA Pediatr. 2015;169(8):e151797. doi:10.1001/jamapediatrics.2015.1797
18. Fernández LR, Hernández RG, Guerediaga IS, et al.; Pulmonary Ultrasound Section of the Neonatal Ultrasound Working Group of the Spanish Society of Neonatology. Usefulness of lung ultrasound in the diagnosis and follow-up of respiratory diseases in neonates. An Pediatr. 2022;96(3):252.e1–252.e13. PMID: 35315321. doi:10.1016/j.anpede.2022.01.002
19. Raimondi F, Migliaro F, Corsini I, et al. Lung ultrasound score progress in neonatal respiratory distress syndrome. Pediatrics. 2021;147(4):e2020030528. PMID: 33688032. doi:10.1542/peds.2020-030528
20. Mongodi S, De Luca D, Colombo A, et al. Quantitative lung ultrasound: technical aspects and clinical applications. Anesthesiology. 2021;134(6):949–965. PMID: 33819339. doi:10.1097/ALN.0000000000003757
21. Liu J. The lung ultrasound score cannot accurately evaluate the severity of neonatal lung disease. J Ultrasound Med. 2020;39(5):1015–1020. PMID: 31737918. doi:10.1002/jum.15176
22. Liu J, Li J, Shan RY, et al. Ultrasound diagnosis and grading of neonatal respiratory distress syndrome: a multicenter prospective study. Chin Pediatr Emerg Med. 2020;27(11):801–807.
23. De Martino L, Yousef N, Ben-Ammar R, et al. Lung Ultrasound Score Predicts Surfactant Need in Extremely Preterm Neonates. Pediatrics. 2018;142(3). doi:10.1542/peds.2018-0463
24. Sweet DG, Carnielli VP, Greisen G, et al. European consensus guidelines on the management of respiratory distress syndrome: 2022 update. Neonatology. 2023;120(1):3–23. PMID: 36863329; PMCID: PMC10064400. doi:10.1159/000528914
25. Raschetti R, Yousef N, Vigo G, et al. Echography-Guided Surfactant Therapy to Improve Timeliness of Surfactant Replacement: a Quality Improvement Project. J Pediatr. 2019;212:137–143.e1. doi:10.1016/j.jpeds.2019.04.020
26. Perri A, Riccardi R, Iannotta R, et al. Lung ultrasonography score versus chest X-ray score to predict surfactant administration in newborns with respiratory distress syndrome. Pediatr Pulmonol. 2018;53(9):1231–1236. doi:10.1002/ppul.24076
27. Sawires HK, Abdel Ghany EA, Hussein NF, et al. Use of lung ultrasound in detection of complications of respiratory distress syndrome. Ultrasound Med Biol. 2015;41(9):2319–2325. doi:10.1016/j.ultrasmedbio.2015.04.024
28. Abdalla W, Elgendy M, Abdelaziz AA, et al. Lung ultrasound versus chest radiography for the diagnosis of pneumothorax in critically ill patients: a prospective, single-blind study. Saudi J Anaesth. 2016;10(3):265–269. doi:10.4103/1658-354X.174906
29. Fei Q, Lin Y, Yuan TM. Lung ultrasound, a better choice for neonatal pneumothorax: a systematic review and meta-analysis. Ultrasound Med Biol. 2021;47(3):359–369. PMID: 33341304. doi:10.1016/j.ultrasmedbio.2020.11.011
30. Liu J, Qiu R, Gao Y. Lung ultrasound for diagnosis of neonatal pulmonary hemorrhage. Chin J Perinat Med. 2019;22(10):740–743.
31. Ren XL, Fu W, Liu J, et al. Lung ultrasonography to diagnose pulmonary hemorrhage of the newborn. J Matern Fetal Neonatal Med. 2017;30(21):2601–2606. doi:10.1080/14767058.2016.1256997
32. Alonso-Ojembarrena A, Lubián-López SP. Lung ultrasound score as early predictor of bronchopulmonary dysplasia in very low birth weight infants. Pediatr Pulmonol. 2019;54(9):1404–1409. doi:10.1002/ppul.24410
33. Liu J, Qiu RX, Gao YQ. Application of lung ultrasound in diagnosis of bronchopulmonary dysplasia in premature infants. Chin J Pract Pediatr. 2020;35(2):97–100.
34. Hansmann G, Sallmon H, Roehr CC, Kourembanas S, Austin ED, Koestenberger M. European Pediatric Pulmonary Vascular Disease Network (EPPVDN). Pulmonary hypertension in bronchopulmonary dysplasia. Pediatr Res. 2021;89(3):446–455. PMID: 32521539; PMCID: PMC7979539. doi:10.1038/s41390-020-0993-4
 © 2024 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2024 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
