Back to Journals » Open Access Surgery » Volume 16
Post-Thyroidectomy Complications at St Paul’s Hospital Millennium Medical College, Ethiopia: Associated Factors and Outcomes
Authors Daba SA , Teklewold B, Suga Y, Biratu TD, Hassen IK
Received 28 July 2023
Accepted for publication 12 October 2023
Published 18 October 2023 Volume 2023:16 Pages 77—86
DOI https://doi.org/10.2147/OAS.S428155
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Professor Luigi Bonavina
Shimelis Abegaz Daba,1 Berhanetsehay Teklewold,1 Yisihak Suga,1 Tolesa Diriba Biratu,2 Ibsa Kedir Hassen3
1Department of Surgery, St. Paul’s Hospital Millennium Medical College, Addis Ababa, Ethiopia; 2School of Public Health, St. Paul’s Hospital Millennium Medical College, Addis Ababa, Ethiopia; 3Department of Surgery, Goba General Hospital, Madda Walabu University, Bale, Ethiopia
Correspondence: Shimelis Abegaz Daba, PO.Box 1271, Addis Ababa, Ethiopia, Tel +251 920039871, Email [email protected]
Introduction: Major post-thyroidectomy complications, including recurrent laryngeal nerve injury, hypocalcemia, hypothyroidism, and hematoma, are associated with various risk factors, including the type of thyroid pathology, underlying patient comorbidities, extent of surgical resection, and the level of expertise of the surgeon. This study aimed to assess the magnitude of post-thyroidectomy complications and associated factors.
Methods: A retrospective review of the medical records of 262 patients was conducted, and the data were analyzed using IBM SPSS Statistics version 25. Bivariate and multivariate logistic regression analyses were used to assess the association between the risk factors and post-thyroidectomy complications. Statistical significance was set at P < 0.05.
Results: The majority of the patients (234, 89.4%) were females, and 56.4% were aged between 20 and 40 years. Seventy-seven (29.4%) patients had complication at first follow-up visit, and 54 (20.6%) had permanent complications at the 6-month follow-up. The most frequent complications at the first visit were hypothyroidism (9.9%), symptomatic hypocalcemia (9.5%), and voice hoarseness (5.7%). At the 6-month follow-up, 14.5%, 6.1%, and 2.7% of patients had hypothyroidism, hypocalcemia, and hoarseness of voice, respectively. Subtotal thyroidectomy was significantly associated with post-thyroidectomy complications (P < 0.01).
Conclusion: The prevalence of post-thyroidectomy complications at the SPHMMC was higher than the acceptable rates across guidelines. The complication rate at SPHMMC on first postoperative follow-up and 6-month follow-up visits was higher than that at the other centers. Subtotal thyroidectomy should be avoided or the last option to be considered because it is significantly associated with post-thyroidectomy complications.
Keywords: thyroidectomy, complications, hypothyroidism, hypocalcemia, recurrent laryngeal nerve injury
Introduction
Thyroid pathologies are common disorders of the endocrine system worldwide.1 The total goiter prevalence in the world’s general population is estimated to be 15.8% and in Africa 28.3%.2 The burden of thyroid disease is very high in Ethiopia, and a large number of patients seek surgical care for various pathologies of the thyroid gland each year.1
Thyroid surgery has a significant mortality rate and was not well established until the middle of the nineteenth century. Due to considerable advancements in surgical procedures, anesthetic, infection control, and hemostatic methods,3 it then began to advance more quickly. Even for patients with benign thyroid disease, more aggressive surgical methods for the thyroid gland, such as complete or hemi-thyroidectomy rather than partial thyroidectomy, are being used in modern surgical practice.4
Specific complications after thyroid surgery, such as injury to the recurrent laryngeal nerve (RLN) or external branch of the superior laryngeal nerve (SLN), hypoparathyroidism, hypocalcemia, hypothyroidism, or recurrent hyperthyroidism, are feared because they sometimes result in lifelong morbidity.5 In developing countries, including Ethiopia, thyroid surgery is performed mostly by general surgeons and very rarely by ear, nose and throat surgeons or endocrine surgeons, owing to their rare availability.6 Thyroid surgeries for either benign or malignant pathologies of the thyroid gland are among the most frequently performed surgical procedures at SPHMMC, and different types of thyroidectomies account for about 11% of all major surgeries.1 The most common types of surgeries done were subtotal thyroidectomy (bilateral and unilateral added), lobectomy and isthmusectomy, near total thyroidectomy, lobectomy alone and total thyroidectomy, in decreasing order.1,4
The size of the goiter, sex, age of the patient, underlying pathology (benign, malignant, graves, etc.), experience of the surgeon, extent of thyroidectomy, and whether the surgery is a repeat or primary type are commonly associated risk factors of post-thyroidectomy complications.7–9 Therefore, the main challenge in thyroid surgery is to alleviate the pathology at the lowest possible rate of postoperative complication.4,5 Thus, our study aimed to assess the prevalence and associated risk factors in patients undergoing thyroidectomy at SPHMMC.
Methods and Materials
This study was conducted at SPHMMC, one of the largest tertiary care teaching hospitals in Addis Ababa, Ethiopia, from January 2022 to October 2022. We conducted an institution-based retrospective review to assess the prevalence and risk factors of complications after thyroid surgery. At SPHMMC, thyroidectomies are performed mainly by general surgeons, and endocrine and breast surgeons have come into practice since 2020, when the fellowship began. All adult patients who underwent either primary or both primary and completion thyroidectomy on an elective basis at SPHMMC from January 1, 2019 to December 31, 2021 were included in the study. Patients with incomplete data, patients who underwent neck dissection, patients who already have voice change, difficulty of breathing and difficulty of swallowing prior to surgery, and patients who did not fulfill the inclusion criteria were excluded. A sample size of 262 was calculated using a single-proportion population formula (P = 50%, 95% CI, d = 5%) and the population correction formula, adding 10% for incomplete charts. A simple random sampling technique was used to select the study participants.
Data Collection Procedure and Data Quality Control
A structured questionnaire was developed in English and used for data collection. The medical record number (MRN) of the patient files was collected from the OR logbook, and charts were retrieved. A structured data extraction format was used to collect the required data from the patient charts. The data collection team was comprised of four well-trained general practitioners. All the required data were extracted and recorded using IBM SPSS version 25.
Data Analysis
Three layers of analysis were performed on the gathered and structured data. Using tables, graphs, charts, and cross tabulations, the frequency of incidence of each thyroidectomy complication was evaluated at the first level. Descriptive statistics, such as frequencies and proportions, were computed for categorical variables in order to present the characteristics of the study participants. For continuous variables with a normal distribution, mean and standard deviation were calculated; otherwise, median and interquartile range were computed. Using bivariate and multivariate logistic regression, respectively, the pattern of relationship between the dependent and independent variables was discovered at the second and third levels. The independent variables that were significantly linked to the occurrence of problems following thyroid surgery were then found. At P < 0.05, the relationship between the variables was deemed significant. The strength of the association between dependent and independent variables was expressed using adjusted odds ratio (AOR).
Ethical Approval
Ethical clearance was obtained from the Institutional Review Board (IRB) of St. Paul’s Hospital Millennium Medical College with reference No. PM23/822. The requirement for written informed consent of the patients was waived by IRB because medical data were collected retrospectively and anonymity as well as confidentiality of the patients’ medical data was maintained throughout the study. The Declaration of Helsinki and other applicable rules and regulations were followed during every procedure.
Results
Sociodemographic Characteristics
A total of 262 participants were included in this study. The majority of the patients were female (89.5%), and more than half of them were between the ages of 20 and 40 years, with the mean and standard deviation of age distribution being 39.7 ± 13 years (Table 1).
 |
Table 1 Sociodemographic and Chief Complaints at Presentation of Post-Thyroidectomy Patients at SPHMMC from January 2019 to December 2021 |
Clinical Characteristics
Nearly 260 (99.2%) patients complained of anterior neck swelling, whereas 52 (19.8%) patients had both anterior neck swelling and compressive symptoms as their chief complaints. Similarly, 99 (37.8%) patients had both toxic symptoms and anterior neck swelling as chief complaints. In contrast, 5 (1.9%) patients had both hoarseness of voice and anterior neck swelling as their main complaints (Table 1).
On physical examination, 209 (79.8%) patients had multinodular goiter, 42 (16%) had solitary nodules, and 10 (3.8%) had diffuse goiters. Retrosternal extension was found in 3 (1.1%) patients, and 4 (1.5%) patients had palpable cervical lymph nodes on physical examination.
Preoperatively, 241 (92%) patients had normal thyroid hormone levels, 6 (2.3%) had high thyroid hormone (free T3 and total T4) levels, and 11 (5.3%) had clinically controlled but biochemically uncontrolled thyroid hormone levels. Most patients 117 (41.7%) were preoperatively diagnosed with CTMNG, followed by NCG 73 (27.9%), malignancy 32 (12.2%), and follicular neoplasm 27 (10.3%) (Figure 1).
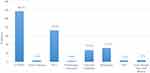 |
Figure 1 Preoperative diagnosis of post-thyroidectomy patients at SPHMMC from January 1, 2019 to December 31, 2021. |
Dunhill’s procedure was the most frequently (101, 38.56%) performed procedure followed by total thyroidectomy (n = 64, 24.4%), lobectomy and isthmusectomy (n = 46, 17.56%), and subtotal thyroidectomy (n = 40, 15.3%). Most thyroidectomies were performed by general surgeons (n = 218, 83.2%). The remaining 44 (16.8%) thyroidectomies were performed by endocrine and breast surgery teams, of which 21 (47.7%) underwent total thyroidectomy, 19 (43.2%) underwent partial thyroidectomies, and the remaining 4 (9.1%) underwent subtotal thyroidectomies. Only 10 (3.8%) patients had a history of thyroid surgery, and completion thyroidectomy was performed during the study period. Intraoperatively, 88 (33.6%) patients had their RLN identified, and there was no documentation of the RLN status in the remaining 174 (66.4%) patients. Parathyroid glands were identified in 44 patients (16.8%), whereas there was no documentation in the remaining 218 (83.2%) patients.
Among the 44 patients who underwent surgery by the endocrine and breast surgery (EBS) team, 19 (43.2%) had total thyroidectomy, 11 (25%) had lobectomy with isthmusectomy, and seven (15.9%) had Dunhill’s procedure. The remaining patients underwent a complete thyroidectomy and lobectomy. Among the patients operated on by the EBS team, 35 (79.5%) had their RLN identified intraoperatively, and parathyroid glands were identified in 20 (45.5%).
Post-Thyroidectomy Complications
During surgery, 14 (5.3%) patients had intraoperative complications, whereas the remaining 248 (94.7%) had a smooth intraoperative course. The most frequent intraoperative complications were stridor upon extubation 8 (3.1%) and significant blood loss 6 (2.3%). Forty-six (17.6%) patients had immediate postoperative complications, while 216 (82.4%) had a smooth immediate postoperative course. The most frequent immediate postoperative complication was symptomatic hypocalcemia (n = 30, 11.5%), followed by hoarseness of voice (n = 14, 5.3%), and hematoma collection (n = 10, 3.8%) (Table 2).
 |
Table 2 Immediate Post-Operative Day Complications in Post-Thyroidectomy Patients |
The rate of post-thyroidectomy complications at the first follow-up visit (within one to two weeks after surgery) was 29.4% (77 of 262 patients had complications). Thirty-two (12.2%) patients had immediate postoperative day complication that persisted until their first follow-up visit. The most frequent complication at the first visit was hypothyroidism (9.9% overall and 8% if we excluded total and completion thyroidectomy cases), followed by symptomatic hypocalcemia (9.5%), and hoarseness of voice (5.7%) (Figure 2). Eleven (4.2%) patients developed seroma collection during their first follow-up visit after thyroidectomy, whereas none of them had seroma collection before discharge from the hospital.
 |
Figure 2 Overall post-thyroidectomy complications at first (within 1 to 2 weeks postoperative) follow up visit. |
The majority (12, 46%) of patients with hypothyroidism on their first follow-up visit underwent subtotal thyroidectomy and 6 (23.2%) underwent Dunhill’s procedure, whereas only five (19.3%) had total thyroidectomy. Four patients had both hypothyroidism and symptomatic hypocalcemia, and two patients had both hoarseness of voice and hypothyroidism. In contrast, one patient had hoarseness of voice and symptomatic hypocalcemia at the first follow-up.
At the six-month follow-up visit, 54 (20.6%) patients had post-thyroidectomy complications. The most frequent complications were hypothyroidism (n = 38, 14.5%), hypocalcemia (n = 16, 6.1%), and recurrent laryngeal nerve palsy (n = 7, 2.8%). Two (0.8%) patients had dysphonia (Figure 3). Six (2.3%) patients had both hypocalcemia and hypothyroidism, whereas three (1.2%) patients had both hypothyroidism and hoarseness of voice due to RLN palsy (Table 3). None of the patients operated on by the EBS team had persistent hoarseness of voice at the 6-month follow-up, whereas three patients operated on by their team (two of them had total thyroidectomy and one had subtotal thyroidectomy) had persistent hypocalcemia (Table 4).
 |
Table 3 Cross Tabulation of Complications and Type of Thyroidectomy at 6-Month Postoperative Follow-Up Visit |
 |
Table 4 Cross Tabulation of Complications at 6-Month Follow-Up and Level of Expertise of Operating Surgeon |
 |
Figure 3 Post-thyroidectomy complications at 6-month postoperative follow-up visit. |
Factors Associated with Post-Thyroidectomy Complications
We analyzed all variables to identify the association, and findings from the bivariate logistic regression model indicated that the sex of the patient, compressive symptoms, preoperative diagnosis, type of thyroidectomy, and intraoperative RLN identification were associated with complication on first follow-up visit at a P-value of <0.25. We used P-value threshold of <0.25 to include variables that are clinically important and associated with post-thyroidectomy complications across literature. These variables were included in the multivariable logistic regression model to determine the significance of the association between the risk factors and dependent variables (Table 5). Subtotal thyroidectomy was significantly associated with postoperative complications (P < 0.01). Bivariable logistic regression was not performed for complications at the 6-month follow-up because the number of patients with complication at the 6-months follow-up was small; therefore, multivariable logistic regression was not performed.
 |
Table 5 Summary of Bivariable and Multivariable Analysis of Variables Associated with Post-Thyroidectomy Complications on First Follow-Up Visit |
Discussion
The vast majority of patients in the age group of 20–40 years are different from those in previous research at SPHMMC, which was between third and fourth decades.1 This could be due to increased awareness and early health-care seeking behavior of society due to promotion through the media, but further study is needed to determine why the age shift has occurred.
The prevalence of post-thyroidectomy complications at the first follow-up visit was 29.4%. The rates of complications are high when compared to those reported in guidelines and various studies (hypothyroidism (9.9% overall and 8% for partial thyroidectomies), symptomatic hypocalcemia (9.5% vs 6.2%), and hoarseness of voice (5.7% vs 4.1%)).4,10–12 The high rate in this study could be because the majority of patients were operated on by general surgeons, and most of these surgeons do not practice sub-capsular dissection. Since a fellowship program was previously established a few years ago and currently, thyroid procedures are primarily carried out by a group of endocrine surgeons or fellows, this may be improved soon. The presence of 11 patients with seroma collection on their first follow-up visit, while none of them had seroma collection in the immediate postoperative period, could be explained by the universal practice of putting a glove drain for the first 24 hours after thyroidectomy by almost all surgeons at our institution. However, the practice of removing the glove drain on the first day postoperatively could be a point of debate, although some literature opposes universal glove drain placement at all.13,14
The majority of patients (21 out of 26) who presented with clinical hypothyroidism (high TSH and low T3 and T4 levels) on their first follow-up visit underwent partial thyroidectomy. This shows that even though the majority of SPHMMC surgeons prefer to leave part of thyroid in situ out of concern that their patients will not be able to afford levothyroxine, a significant number of partial thyroidectomy patients may still experience hypothyroidism after surgery, which is higher than the 4% to 5% clinical hypothyroidism rate after partial thyroidectomy.15,16
Overall, 54 (20.6%) patients had persistent complication at 6−month follow-up visit, which was significantly higher than that reported in other studies.10 The majority (38, 14.5%) had hypothyroidism, followed by hypocalcemia 16 (6.1%) and hoarseness of voice 7 (2.7%), which showed a higher rate of persistent RLN palsy and hypocalcemia due to inadvertent parathyroid gland injury or resection compared to other studies.3,11,17–19 At sixth month follow-up visit, 33 (12.5%) patients had complications that had persisted since their first follow-up visit, and another 33 (12.5%) patients had complications at the first visit that had improved, indicating that they had transient complications. There were 21 (8.01%) patients who had complications at the 6-month follow-up but did not have complications during their first follow-up visit, which could be due to different surgeons or residents evaluating them at the follow-up clinic and the lack of using a uniform template to assess the presence of these patients during their postoperative follow-up.
At 6-month follow-up, compared to the patients operated on by the general surgeon’s team, those operated on by the endocrine and breast surgery team had a lower rate of hypocalcemia (3 vs 13), and none of the patients operated on by the EBS team had hoarseness of voice. This could be because endocrine and breast surgery teams almost always perform sub-capsular dissection and routinely identify RLN and parathyroid glands17,20 or because the EBS team operated on fewer patients than the general surgery team. Generally, among the study subjects, the RLN was identified intraoperatively in only one-third (33.6%) of the patients, whereas no documentation or RLN was identified in the remaining patients. This could be due to the lack of a specific standard template for operation notes, incomplete documentation by residents, or lack of electronic medical records (EMR). Generally, this result shows that practice at SPHMMC is not in line with the current standard that recommends routine RLN identification during thyroid dissection.3,21–23
Using a multivariable logistic regression model, the type of thyroidectomy performed had statistically significant associations with complication on first follow-up visit. The results showed that patients who underwent subtotal thyroidectomy were 2.89 times more likely to present with complication at first follow-up visit (AOR = 2.89) (95% CI: 1.29–6.50) (P < 0.01), which is in line with studies conducted in Greece and the United States, suggesting that total and subtotal thyroidectomies are at high risk.9,12 This is mainly because, in these procedures, both sides of the thyroid lobes are mobilized, and hence, the risk of injury to the RLN and parathyroid glands increases.
Variables that showed a significant association with complication on first follow-up visit (P < 0.25) on bivariable logistic regression included sex of the patient, compressive symptoms, preoperative diagnosis, type of thyroidectomy, and intraoperative RLN identification; however, they did not show a significant association on multivariate logistic regression.
Physical characteristics of patients, such as the presence of MNG, large goiter size, diffuse or solitary nodules, the presence of palpable cervical lymph nodes, and retrosternal extension, did not demonstrate a statistically significant association with post-thyroidectomy complications in this study, although they did in other studies.7,18,24–26 The preoperative thyroid function status, use of anticoagulant medications, prior thyroid surgery, failure to identify parathyroid glands intraoperatively, and level of expertise of the operating surgeon did not show a statistically significant association with post-thyroidectomy complications in this study, which is inconsistent with the findings of several other studies.2,9,18,27,28
The team of the general surgeons performed surgery on more than 83.2% of the patients. Only 16.8% of the patients had surgery performed by breast and endocrine surgeon teams. Due to the dearth of these subspecialists, there were fewer patients operated on by the endocrine surgery team; over the course of the three years examined in this research, only two endocrine surgery fellows and one head and neck surgeon performed thyroid surgeries, primarily on patients with thyroid cancer and neck dissection.
Conclusion and Recommendation
The overall complication rates after thyroid surgery at first follow-up visit and 6-month follow-up visits were 29.4% and 20.6%, respectively. The prevalence of post-thyroidectomy complications at SPHMMC is high compared to the complication rates across various studies and guidelines. Patients undergoing partial thyroidectomy could still have hypothyroidism, requiring levothyroxine supplementation for the rest of their lives. Subtotal thyroidectomy has significant association with post-thyroidectomy complications.
This study should also be conducted at a national level, across various institutions using a larger sample size, to determine the magnitude of post-thyroidectomy complications and associated factors in Ethiopia.
Limitations of the Study
This study was conducted at a single institution, and it is difficult to generalize the results of this study. The data collected were secondary data, which could have led to missing information from the patient charts. The sample size of this study was relatively small.
Acknowledgment
We acknowledge the data collectors, OR staff, medical record room, and support staff for their assistance during data collection.
Disclosure
The authors report no conflicts of interest in this work.
References
1. Suga Y, Abebe E. Patterns of Surgically Treated Thyroid Disease… Patterns of Surgically Treated Thyroid Disease: A Two Years Review at St. Paul Hospital Millennium medical College, Addis Ababa, Ethiopia Addis Ababa, Ethiopia. Ethiopian J Health Sci. 2020;30(1):31. doi10.4314/ejhs.v30i1.5
2. Veetil P, Panchangam R. Does goitre size and delayed surgical intervention adversely affect surgical outcome? A multi-centric experience on thyroidectomy. Formos J Surg. 2021;54(6):219. doi:10.4103/fjs.fjs_223_20
3. Lukinović J, Bilić M. OveRview of thyroid surgery complications. Acta Clin Croat. 2020;59:2020.
4. Bergenfelz A, Jansson S, Kristoffersson A, et al. Complications to thyroid surgery: results as reported in a database from a multicenter audit comprising 3660 patients. Langenbeck’s Arch Surg. 2008;393(5):667–673. doi:10.1007/s00423-008-0366-7
5. Farrar WB. Complications of thyroidectomy. Surg Clin North Am. 1983;63(6):1353–1361. doi:10.1016/S0039-6109(16)43193-2
6. Watters DAK, Wall J. Thyroid surgery in the tropics. ANZ J Surg. 2007;77(11):933–940. doi:10.1111/j.1445-2197.2007.04286.x
7. Abboud B, Sargi Z, Akkam M, Sleilaty F. Risk factors for postthyroidectomy hypocalcemia. J Am Coll Surg. 2002;195(4):456–461. doi:10.1016/S1072-7515(02)01310-8
8. Caulley L, Johnson-Obaseki S, Luo L, Javidnia H. Risk factors for postoperative complications in total thyroidectomy: A retrospective, risk-adjusted analysis from the National Surgical Quality Improvement Program. Medicine. 2017; 96(5):e5752
9. Karamanakos SN, Markou KB, Panagopoulos K, et al. Complications and risk factors related to the extent of surgery in thyroidectomy Results from 2043 procedures. Hormones. 2010;9(4):318–325. doi:10.14310/horm.2002.1283
10. Spear SA, Theler J, Sorensen DM. Complications after the surgical treatment of malignant thyroid disease. Mil Med. 2008;173(4):399–402. doi:10.7205/MILMED.173.4.399
11. Rosato L, Avenia N, Bernante P, et al. Complications of thyroid surgery: analysis of a multicentric study on 14,934 patients operated on in Italy over 5 years. World J Surg. 2004;28(3):271–276. doi:10.1007/s00268-003-6903-1
12. Article O. Assessment of the morbidity and complications of total thyroidectomy. Arch Otolaryngol Head Neck Surg. 2002;128(4):389–392. doi:10.1001/archotol.128.4.389
13. Article O, Fassas S, Mamidi I, et al. To drain or not to drain after thyroid surgery: a randomized controlled trial at a tertiary Hospital in East Africa. Afr Health Sci. 2013;13(3):748–755. doi:10.4314/ahs.v13i3.33
14. Ramouz A, Rasihashemi SZ, Daghigh F, Faraji E, Rouhani S. Predisposing factors for seroma formation in patients undergoing thyroidectomy: cross-sectional study. Ann Med Surg. 2017;23:8–12. doi:10.1016/j.amsu.2017.09.001
15. Abraham CR, Ata A, Stain SC, Khalaf ZM, Hazimeh Y. Time to hypothyroidism following hemithyroidectomy. Cureus. 2022;14:2014.
16. Verloop H, Louwerens M, Schoones JW, Kievit J, Smit JWA, Dekkers OM. Risk of hypothyroidism following hemithyroidectomy: systematic review and meta-analysis of prognostic studies. J Clin Endocrinol Metab. 2012;97(7):2243–2255. doi:10.1210/jc.2012-1063
17. Ríos-Zambudio A, Rodríguez J, Riquelme J, Soria T, Canteras M, Parrilla P. Prospective study of postoperative complications after total thyroidectomy for multinodular goiters by surgeons with experience in endocrine surgery. Ann Surg. 2004;240(1):18–25. doi:10.1097/01.sla.0000129357.58265.3c
18. Thomusch O, Machens A, Sekulla C, et al. Multivariate analysis of risk factors for postoperative complications in benign goiter surgery: prospective multicenter study in Germany. World J Surg. 2000;24(11):1335–1341. doi:10.1007/s002680010221
19. Kalyoncu D, Gönüllü D, Gedik ML, et al. Analysis of the factors that have an effect on hypocalcemia following thyroidectomy. Turkish J Surg. 2013;29(4):171–176. doi:10.5152/UCD.2013.2438
20. Steurer M, Passler C, Denk DM, Schneider B, Niederle B, Bigenzahn W. Advantages of recurrent laryngeal nerve identification in thyroidectomy and parathyroidectomy and the importance of preoperative and postoperative laryngoscopic examination in more than 1000 nerves at risk. Laryngoscope. 2002;112(1):124–133. doi:10.1097/00005537-200201000-00022
21. Dl T, Thantry G, Shastri R. Capsular dissection: a preferred technique in total. World J Surg Surgical Res. 2022;5:1–3.
22. Chisthi MM, Kuttanchettiyar KG. Capsular dissection technique for reducing recurrent laryngeal neuropraxia and temporary hypoparathyroidism after thyroidectomy: a single center experience. Int J Otorhinolaryngol Head Neck Surg. 2015;1(1):17–22.
23. Chow TL, Chu W, Lim BH, Kwok SPY. Outcomes and complications of thyroid surgery: retrospective study. Hong Kong Med J. 2001;7(3):261–265.
24. Dener C. Complication rates after operations for benign thyroid disease. Acta Otolaryngol. 2002;122(6):679–683. doi:10.1080/000164802320396394
25. Berri T, Houari R. Complications of thyroidectomy for large goiter. Pan African Med J. 2013;16(138):1937–8688.
26. Bawa D, Alghamdi A, Albishi H, et al. Post-thyroidectomy complications in southwestern Saudi Arabia: a retrospective study of a 6-year period. Ann Saudi Med. 2021;41(6):369–375. doi:10.5144/0256-4947.2021.369
27. Sosa JA, Bowman HM, Tielsch JM, Powe NR, Gordon TA, Udelsman R. The importance of surgeon experience for clinical and economic outcomes from thyroidectomy. Ann Surg. 1998;228(3):320–330. doi:10.1097/00000658-199809000-00005
28. Patel KN, Yip L, Lubitz CC, et al. The American association of endocrine surgeons guidelines for the definitive surgical management of thyroid disease in adults. Ann Surg. 2020;271:21–93.
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
