Back to Journals » Patient Preference and Adherence » Volume 18
Position Adherence in Patients Underwent Pars Plana Vitrectomy with Silicone Oil Tamponade
Authors Gao S , Huang N, Huang W, Lian Y, Xiao H, Yao S
Received 6 December 2023
Accepted for publication 2 April 2024
Published 15 April 2024 Volume 2024:18 Pages 829—838
DOI https://doi.org/10.2147/PPA.S453683
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Jongwha Chang
Saiyu Gao,1– 3 Nanqi Huang,4 Wenmin Huang,5 Yu Lian,5 Huiming Xiao,5 Shuyu Yao5
1Department of Geriatrics, Xiangya Hospital, Central South University, Changsha, Hunan, People’s Republic of China; 2National Clinical Research Center for Geriatric Disorders, Xiangya Hospital, Central South University, Changsha, Hunan, People’s Republic of China; 3Teaching and Research Section of Clinical Nursing, Xiangya Hospital of Central South University, Changsha, Hunan, People’s Republic of China; 4Department of Gastroenterology, The Third Affiliated Hospital of Guangzhou Medical University, Guangzhou, People’s Republic of China; 5Ocular Emergency and Trauma Department, State Key Laboratory of Ophthalmology, Zhongshan Ophthalmic Center, Sun Yat-sen University, Guangdong Provincial Key Laboratory of Ophthalmology and Visual Science, Guangdong Provincial Clinical Research Center for Ocular Diseases, Guangzhou, People’s Republic of China
Correspondence: Shuyu Yao, Email [email protected]
Introduction: Position adherence of patients with Pars Plana Vitrectomy with Silicone Oil Tamponade after discharge is of positive significance. However, patients undergoing a day surgery makes the quality of discharge teaching and readiness for hospital discharge is insufficient, which will influence their position adherence at home.
Aim: This study aimed to find the correlation of discharge teaching, readiness for hospital discharge, and position adherence in patients who underwent PPV with silicone oil tamponade from the day ward.
Methods: This was a cross-sectional survey. One hundred ninety-four patients with day surgery were recruited by convenient sampling from Zhongshan Ophthalmic Center, China. Data were collected using the quality of discharge teaching scale, readiness for hospital discharge scale, and position adherence scale.
Results: Patients’ education level, residence, poor postoperative vision, ophthalmic surgery history, and quality of discharge teaching are the main factors of readiness for discharge. Only 41(21%) patients had good position adherence, and education level and readiness for discharge are the main factors of position adherence.
Discussion: Discharge teaching improves patients’ knowledge and competence of self-care and helps patients prepare for the transition from hospital to home, and readiness for hospital discharge significantly influences position adherence after discharge and indirectly plays a vital role in postoperative vision recovery and surgical effect.
Keywords: discharge teaching, readiness for hospital discharge, position adherence, pars plana vitrectomy with silicone oil tamponade
Introduction
Pars plana vitrectomy with silicone oil tamponade has become an effective surgical method for the treatment of retinal detachment. It aims to allow silicone oil injected into the vitreous body to press the detached retina on the floating roof to reset it and seal the hole.1 Patients were asked to stay in a particular position to ensure surgery effect according to the location of the retinal break, such as face-down position, upright position, and lateral recumbent position, for at least 16 hours per day, lasting at least seven days after the surgery.2
However, the position adherence after surgery puzzles both medical staff and patients. Position adherence represents the compliance of keeping in a particular position for a specified period as they were taught by medical staff. Keeping in a particular position for enough time is inconvenient and complex, and some patients cannot comply strictly.3 If patients take the improper position, Silicone oil covers the lens. It enters the anterior chamber, leading to lens opacity, secondary glaucoma, and other complications, and the time of specific position after surgery significantly affects vision restoration.4 Position adherence directly affects the success rate of retinal reattachment and quality of life.5 Therefore, improving the position adherence of patients with Pars Plana Vitrectomy with Silicone Oil Tamponade is of positive significance.
Readiness for hospital discharge (RHD) is to evaluate the patient’s ability to further rehabilitation after leaving the hospital.6 RHD is both a state and a process characterized by physical stability and competence to manage self-care at home; sufficient support to cope after leaving the hospital; psychological ability to manage the process; and adequate information and knowledge to respond to common problems.7 Higher RHD can reduce medical expenses, related to a higher quality of life and a lower incidence of post-discharge complications and readmission.8–10 Considering the benefits of well-prepared discharge, medical staff provide sufficient discharge teaching to improve patients’ care knowledge, skills, and RHD. Studies show that the quality of discharge teaching (QDT) is vital in the patient’s discharge readiness and self-management at home.11,12 It is also pointed out that the discharge teaching provided by nurses improved the compliance of self-care and clinical outcomes and reduced nursing costs.13
According to Meleis’ transitions theory,14 a transition is the process from one condition or status to another, denoting a change in health status, expectations, abilities, or human systems.15,16 The transition conditions and nursing therapeutics influence the response patterns, conceptualized as outcome indicators. In the transition of patients from hospital to home, patients’ characteristics such as gender, age, and education level were considered transition conditions, which facilitate or hinder the transition progress. The discharge teaching represents the nursing therapeutic,16 and the outcome was the patients’ position adherence. The RHD was considered an internal variable that shapes both the influence of transition conditions and the nursing therapeutic outcome during the transition.
At present, pars plana vitrectomy (PPV) with silicone oil tamponade is increasingly carried out as a day surgery, which refers to patients’ admission, operation, and discharge within 24 hours and has the advantages of short hospital stay, fast recovery, and low economic burden.17 After a short period of discharge teaching in the day ward, patients who underwent day surgery return home to self-care. However, due to workload and time constraints, medical staff must quickly provide many discharge contents for patients. In this case, the discharge teaching received by the patient is more likely to be hasty and insufficient.18 Besides, the patient’s strength, energy, and self-care ability have not been fully restored because of day surgery, which led to the patient’s subjective perception that he is not in good condition and unsuitable for discharge.
This makes the patients’ discharge readiness and position adherence at home doubtful. Accordingly, this study aimed to explore discharge teaching, readiness for hospital discharge, and position adherence in patients who underwent PPV with silicone oil tamponade from day ward and the relationship among them.
Method
Design
This study was a cross-sectional study. One hundred ninety-four patients with ocular fundus disease were recruited through convenient sampling from October 2017 to June 2018 from Zhongshan Ophthalmic Center, China. This study was executed and reported following STROBE Statement (Supplemental Files 1).
Inclusion criteria were as follows: (1) ≥18 years old; (2) diagnosed with retinal detachment and underwent day surgery PPV with silicone oil tamponade; (3) asked to keep in a particular position for at least 16 hours per day, for at least seven days after day surgery; (4) adequate language comprehension ability; (5) voluntary to participate in this study. Moreover, exclusion criteria were as follows: (1) with severe cognitive impairment and hearing impairment; (2) with other serious eye diseases; (3) with other life-threatening severe diseases; (4) participate in another relevant research. Kendall’s sample size calculation principle yields sample sizes 5–10 times the number of variables. In our research, there were 16 variables (8 related to demographic information, 3 to QDTS, 4 to RHDS, and 1 to PAS). Therefore, the sample size in this study was set at 114 to 228 (19× 5×1.2 = 114--19× 10×1.2 =228).
Measurements
Demographic Information Questionnaire
The demographic characteristics of patients were collected by the self-compiled questionnaire with eight items, including age, gender, marital status, educational level, residence, postoperative vision, ophthalmology history, and ophthalmic surgery history. Ophthalmology history represents the history of previous medical conditions involving the eye, including trauma, ocular disease due to systemic conditions, keratitis and cataracts that affect the prognosis of vision. And poor postoperative vision means low vision (best-corrected visual acuity <0.3 but ≥0.05 in both eyes).
The Quality of Discharge Teaching Scale (QDTS)
To measure the quality of discharge teaching, QDTS was used. It is a self-report scale developed by Weiss et al.16 The Chinese version of QDTS was revised by Wang.19 The Chinese version of QDTS consists of 24 items related to three dimensions: teaching contents that patients thought they needed (6 items), teaching contents that patients obtained (6 items), and teaching skills and effectiveness (12 items). QDTS addresses the quality of discharge teaching using a 0 to 10 rating scale. The total scores ranged from 0 to 240, and the total score higher, the better quality of discharge teaching. The reliability coefficient of the Chinese version of QDTS among Chinese patients was 0.924, and the scale’s reliability in this study was 0.865.
Readiness for Hospital Discharge Scale (RHDS)
The readiness for hospital discharge scale was developed by Weiss.15 Moreover, the Chinese version of the RHDS was revised by Zhao et al.20 It has 23 items in total and consists of four dimensions: physical conditions, mastery of disease knowledge, coping ability after discharge, and available social support. Higher scores reflect higher levels of readiness for hospital discharge. The reliability of the scale in this study was 0.916.
Position Adherence Scale (PAS)
This study used a self-designed Position Adherence Scale (PAS). At first, a questionnaire item pool was established based on a literature review. Then the questionnaire was modified by expert consultation. According to the purpose and feasibility of the study, ten medical or nursing experts from Guangzhou tertiary ophthalmic hospital were consulted. All the included experts have been engaged in ophthalmic treatment or nursing for ten years, with a bachelor’s degree or above. After the expert consultation, the ambiguous and difficult-to-answer items are modified to form a formal questionnaire. The validity of the questionnaire is 0.538.
The PAS was used to assess position adherence, and it consists of 4 items with response options “no” and “yes”. Items were assigned a score from 0–1 (1=no, 0=yes) and Item 3 reverse scoring, The total score of PAS is the sum of four items.
Data Collection
From October 2017 to June 2018, patients who met the inclusion criteria were recruited from the Zhongshan Ophthalmic Center, Sun Yat-sen University in Guangdong Province, China, and all patients received the same questionnaires. On their discharge day, patients completed the Demographic Information Questionnaire (DIQ), the Quality of Discharge Teaching Scale (QDTS), and the Readiness for Hospital Discharge Scale (RHDS). One week later, patients completed the Position Adherence Scale (PAS) via a telephone interview.
Data Analysis
Statistical analysis was performed using the chi-square test, Student’s t-test, and Mann Whitney U-test as applicable using SPSS 21.0, released 2012, IBM Corp). Additionally, correlations between the various measures were calculated using Spearman’s rank correlation analyses.
Statistical analyses were conducted with IBM SPSS Statistics version 20.0 (SPSS Inc., Chicago, IL, USA). Descriptive data were presented as means and standard deviations. Pearson’s correlation analyses were used for correlations among discharge teaching, social support, and readiness for hospital discharge. Multiple linear regression analysis was used to analyze the influencing factors of RDHS and PAS.
Ethics
This study complied with the Declaration of Helsinki. And the study was approved by the institutional review board of Zhongshan Ophthalmic Center, Sun Yat-sen University (2020KYPJ037). Participants signed the informed consent before they completed the questionnaire. All eligible participants were informed of their rights and could withdraw anytime.
Results
Demographic Information of Participants
In total, 194 participants participated in the study, and they had an average age of 50.9 years, 88 (45.4%) of the participants were female, 123 (63.4%) lived in cities, 51 (26.3%) had an education level lower than junior high school. Other demographic information of participants was displayed in Table 1.
 |
Table 1 Demographic Information of 194 Patients |
Questionnaire Scores
The QDTS and RHDS questionnaire scores were shown in Table 2, and the questionnaire scores of PAS were presented in Table 3. The total score of the QDTS in the 194 patients was 177.7 ± 25.9, and the dimensions with high to low were teaching skills and effectiveness, teaching contents that patients thought they needed, and teaching contents that patients obtained. The total score of RHDS in the 194 patients ranged from 66 to 209, with an average of 155.2 ± 26.9. Moreover, the scores in dimensions from high to low were physical conditions, mastery of disease knowledge, available social support, and coping ability after discharge. The average scores of the four dimensions were 52.2, 45.7, 34.1, and 23.3, respectively.
 |
Table 2 Status on QDTS and RHDS (n=194) |
 |
Table 3 Status on Patients’ Position Adherence (n=194) |
Table 3 showed that the patient’s position adherence scale scored 0~4 points, averaging 2.46 points. Only 41 patients (21%) scored 4 points and had good position adherence.
Correlation Between QDTS, RHDS, and PAS
The quality of discharge teaching was highly related to hospital discharge readiness (r = 0.669, p < 0.05). Position adherence had a positive correlation with the quality of discharge teaching (r = 0.240, p < 0. 05) and readiness for hospital discharge (r =0.312, p < 0. 05). The correlations among the measured variables are displayed in Table 4.
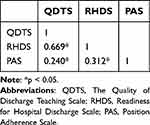 |
Table 4 Correlation Between QDTS, RHDS and PAS (n=194) |
The Multiple Linear Regression Analysis (Stepwise) of Readiness for Hospital Discharge in 194 Patients
The total score of the RHDS was taken as the dependent variable, and eight demographic variables and QDTS were used as the independent variables. The stepwise multiple linear regression analysis was applied. The result was presented in Table 5, and it showed that the QDTS, patients’ education level, residence, poor postoperative vision, and ophthalmic surgery history were the main factors influencing the readiness for hospital discharge of the patients (adjusted R-square = 0.570, F =26.577, p < 0.000).
 |
Table 5 Linear Regression of Patients’ RHDS |
The Multiple Linear Regression Analysis (Stepwise) of Position Adherence in 194 Patients
The total score of the PAS was taken as the dependent variable, and eight demographic variables, QDTS and RDHS, were used as the independent variables. The stepwise multiple linear regression analysis was applied. The result was presented in Table 6, and it showed that the RHDS and the educational level were the main factors influencing the position adherence of the patients (adjusted R-square = 0.091, F = 2.93, p < 0.01).
 |
Table 6 Linear Regression of Patients’ PAS |
Discussion
The QDT and RHD in patients who underwent PPV with silicone oil tamponade were high. The score for teaching content patients thought they needed is more than for teaching content they obtained. This indicates a lack of understanding of patients’ knowledge needs by medical staff, which was consistent with the previous study.
The RHD was lower than that of cataract patients.21,22 This may be due to day surgery for ophthalmic patients and the different setting of the study. Besides, the dimensions of coping ability after discharge and available social support score were low, indicating that the patient’s abilities and potential support are not satisfactory and capable of coping with post-discharge care.
Patients’ education level, residence, poor postoperative vision, and ophthalmic surgery history are the main factors of RHD. Patients with a poor educational background also have lower RHDS. They need more help and guidance from medical staff. While patients with a higher educational level usually could search for and apply adequate information to address problems independently and skillfully.23,24 This can be conducive to the improvement of their care ability.
Generally, tertiary ophthalmic hospitals are located in cities in China. The distance between urban residents and the hospital is relatively close, and it is convenient for them to go for immediate medical treatment and subsequent visits. Objectively, they have more potential support and medical resources after discharge. Therefore, there are fewer concerns and psychological burdens when leaving the hospital. That is why the readiness for hospital discharge of urban residents is relatively higher than those from the countryside. This result is consistent with previous studies.23 Patients with poor postoperative vision will likely have lower RHD, which might cause concern and psychological pressure in postoperative recovery. Moreover, poor postoperative vision also weakens their competence in managing self-care at home.22 Similarly, patients had received ophthalmic surgery for the first time may lack experience in self-care and the ability to cope with healthcare issues and may also be less confident than patients who have undergone ophthalmic surgery.25
Findings suggested that discharge teaching is conducive to improving the score of RHDS.21,25 Discharge teaching improves patients’ ability to respond to new environments and increases their confidence in a successful transition.26 However, patients undergoing daytime surgery are discharged after receiving short discharge teaching, quickly leading to insufficient information, inaccurate understanding, and instruction without individualization.22 Previous studies found that the decreased hospital stay for surgical patients reduced the time available for the knowledge given by the nurses.27,28 It is also shown that discharge teaching helps patients prepare for the transition from hospital to home, and both discharge teaching and readiness for hospital discharge influence patients’ knowledge and competence of self-care and compliance behaviors.29
Only 41 (21%) patients scored 4 points and had good position adherence. 38 (19.6%) patients shortened the duration or stopped keeping in a particular position when their vision improved. This may be because the medical staff did not inform the patient of the importance of long-term posture and the possible consequences. The patient’s position for a long time may cause many physical discomforts, such as eyelid edema, limb numbness, poor breathing, and chest and elbow joint pain, so 80 (41.2%) patients found it challenging to keep in a particular position as they were asked to keep the specific position every day. Besides, nurses provided discharge teaching of the position only once, and after discharge, the patient complied with the specific position either consciously or with family supervision. The lack of continuous postural supervision by the medical staff made the patients’ position adherence much lower. Although this study did not find that discharge teaching significantly affected position adherence, realizing the necessity of PA during discharge teaching is more likely to increase compliance behavior.30 Patients’ education level and RHD are the main factors of PA.
To some extent, educational level determines cognitive ability and psychological endurance. Highly educated patients are more likely to recognize the importance of specific positions and may be able to overcome practical difficulties in several ways.23 Previous study also showed that education background had a positive effect on adherence of patients.31 RHD significantly influences position adherence after discharge and indirectly plays a vital role in postoperative vision recovery and surgical effect. When the patients are well prepared for discharge, they have enough physical and psychological resources to deal with many problems after discharge, which makes them better able to manage themselves and comply with a specific posture. This result was similar to previous studies, which stated that sufficient RHD could enhance satisfactory outcomes, such as higher quality of life, unscheduled clinic visits, and post-discharge coping difficulty.8–10
Discharge may occur when the patient has adequate post-discharge support and is willing to leave the hospital. It is necessary to take a routine evaluation of patients’ RHD into consideration. To improve patients’ RHD, the hospital should provide online medical services for patients in remote areas. These online supports may relieve their psychological stress and difficulty accessing medical care after discharge. More psychological counseling should be provided for patients with poor postoperative vision or first-time ophthalmic surgery to enhance their confidence in recovery. Most important, more attention on improving the quality of discharge teaching is needed. Medical staff should constantly enrich the content of discharge teaching by better understanding patients’ expectations and individual needs. They can effectively use guidance skills, pay attention to the patient’s understanding and feedback, and ask questions to confirm that the patient masters the content. More straightaway language and vivid metaphors should be used, especially for patients with a low educational background or first-time ophthalmic surgery. To improve patient position adherence and enhance RHD, the nurses should explain the relationship between the unique position and the filler so that patients understand the importance of maintaining the position for a successful operation. Moreover, more continuous position monitoring can be done online after discharge, such as sending regular reminders to patients.
Limitation
This study had some limitations. First, participants of this study were recruited only from one ophthalmic hospital in Guangdong Province, and the results may not be generalized to the whole country. Second, the sample size of 194 is relatively small, which may affect the reliability of the results. Besides that, this study was a cross-sectional survey, and patients were influenced by objective and subjective factors when filling out those questionnaires, which caused some bias in the results. Finally, different positions had a greatly effect on patient position adherence. For example, head down/prone may be more difficult to adhere for most patients to supine position. However, location of retinal break and specific position of the patients were not collected in this study.
Conclusion
Patients who underwent PPV with silicone oil tamponade were asked to keep in a particular position to ensure the surgery effect. Whether patients going through the day surgery stay in a particular position for enough time depends on their regulation of themselves after discharge. RHD indicates whether the patients complete a safe discharge process, continue further rehabilitation and return to society, and it significantly impacts position adherence.
Although discharge teaching is not an essential factor in position adherence, it promotes patients’ awareness of the importance of position adherence. We also found that patients’ educational background, residence, poor postoperative vision, ophthalmic surgery history, and discharge teaching are the main factors of RHD. Therefore, more online medical services and psychological counseling should be provided for those patients, and more attention on improving the quality of discharge teaching is needed. Future research should focus on the factors influencing position adherence, and interventions to improve discharge readiness and position adherence in ophthalmic surgery patients could be conducted in clinical settings.
Ethics Approval and Consent to Participate
The study was approved by the institutional review board of Zhongshan Ophthalmic Center, Sun Yat-sen University (2020KYPJ037). Participants signed the informed consent before they completed the questionnaire. All eligible participants were informed of their rights and they can withdraw at any time. The whole study was performed following relevant guidelines and regulations.
Acknowledgments
We appreciated all participants in the study.
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Funding
This work was supported by the Medical Scientific Research Foundation of Guangdong (A2022301).
Disclosure
The authors report no conflicts of interest in this work.
References
1. Kokavec J, Wu Z, Sherwin JC, Ang AJS, Ang GS. Nd:YAG laser vitreolysis versus pars plana vitrectomy for vitreous floaters. Cochrane Database Syst Rev. 2017;2017(6). doi:10.1002/14651858.CD011676.pub2
2. Morimoto E, Shimada Y, Sugimoto M, Mizuguchi T, Tanikawa A, Horiguchi M. Adherence to face-down and non-supine positioning after macular hole surgery. BMC Ophthalmol. 2018;18(1):18. doi:10.1186/s12886-018-0683-8
3. Seno Y, Shimada Y, Mizuguchi T, Tanikawa A, Horiguchi M. Compliance with the face-down positioning after vitrectomy and gas tamponade for rhegmatogenous retinal detachments. Retina. 2015;35(7):1436–1440.
4. Shimada Y, Seno Y, Mizuguchi T, Tanikawa A, Horiguchi M. Patient adherence to the face-down positioning after macular hole surgery. Clin Ophthalmol. 2017;11:1099–1104. doi:10.2147/OPTH.S135144
5. Suzuki K, Shimada Y, Seno Y, Mizuguchi T, Tanikawa A, Horiguchi M. Adherence to the face-down positioning after vitrectomy and gas tamponade: a time series analysis. BMC Res Notes. 2018;11(1):142. doi:10.1186/s13104-018-3257-1
6. Steele NF, Sterling YM. Application of the case study design: nursing interventions for discharge readiness. Clin Nurse Specialist. 1992;6(2):79–84. doi:10.1097/00002800-199200620-00008
7. Galvin EC, Wills T, Coffey A. Readiness for hospital discharge: a concept analysis. J Adv Nurs. 2017;73(11):2547–2557. doi:10.1111/jan.13324
8. Meng N, Liu RA, Wong MM, Liao JP, Feng C, Li XL. The association between patient-reported readiness for hospital discharge and outcomes in patients diagnosed with anxiety disorders: a prospective and observational study. J Psychiatr Ment Health Nurs. 2020;27(4):380–392. doi:10.1111/jpm.12592
9. Piccenna L, Lannin NA, Gruen R, Pattuwage L, Bragge P. The experience of discharge for patients with an acquired brain injury from the inpatient to the community setting: a qualitative review. Brain Injury. 2016;30(3):241–251. doi:10.3109/02699052.2015.1113569
10. Siow E, Lo SM, Yeung KL, Yeung RSD, Choi KC, Chair SY. Factors and post-discharge outcomes associated with patients’ readiness for discharge from the emergency medicine ward: a prospective study. Int Emerg Nurs. 2019;46:100773. doi:10.1016/j.ienj.2019.04.002
11. Yam CHK, Wong ELY, Cheung AWL, Chan FWK, Wong FYY, E-k Y. Framework and components for effective discharge planning system: a delphi methodology. BMC Health Serv Res. 2012;12:12. doi:10.1186/1472-6963-12-12
12. Yang J, He Y, Jiang L, Li K. Colorectal patients’ readiness for hospital discharge following management of enhanced recovery after surgery pathway a cross-sectional study from China. Medicine. 2020;99(8):e19219.
13. Koelling TM, Johnson ML, Cody RJ, Aaronson KD. Discharge education improves clinical outcomes in patients with chronic heart failure. Circulation. 2005;111(2):179–185. doi:10.1161/01.CIR.0000151811.53450.B8
14. Meleis AI, Sawyer LM, Im E-O, Messias DKH, Schumacher K. Experiencing transitions: an emerging middle-range theory. Adv Nurs Sci. 2000;23(1):12–28. doi:10.1097/00012272-200009000-00006
15. Weiss ME, Piacentine LB. Psychometric properties of the Readiness for Hospital Discharge Scale. J Nurs Measure. 2006;14(3):163–180. doi:10.1891/jnm-v14i3a002
16. Weiss ME, Piacentine LB, Lokken L, et al. Perceived readiness for hospital discharge in adult medical-surgical patients. Clin Nurse Spec. 2007;21(1):31–42. doi:10.1097/00002800-200701000-00008
17. Cadariu F, Enache A, Avram M, Muresan C, Olariu S. Day surgery in Romania. Annali Italiani Di Chirurgia. 2017;88(6):567–571.
18. Zhang J, Yao S, Huang F, et al. Exploring the role of social support between discharge teaching and readiness for discharge in ocular fundus disease patients: a cross-sectional study. J Ophthalmol. 2021;2021:1–9. doi:10.1155/2021/5547351
19. Wang BH, Wang H, Yang CZ. Reliability and validity of the Chinese version of the Quality of Discharge Teaching Scale. Chin J Nurs. 2016;51(6):752–755.
20. Zhao H, Feng X, Yu R, Gu D, Ji X. Validation of the Chinese Version of the readiness for Hospital Discharge Scale on patients who have undergone laryngectomy. J Nurs Res. 2016;24(4):321–327. doi:10.1097/JNR.0000000000000126
21. Zhang A, Feng X, Qiu C. Discharge teaching, readiness for hospital discharge and post-discharge outcomes in cataract patients: a structural equation model analysis. J Nurs Manage. 2021;29(3):543–552. doi:10.1111/jonm.13169
22. Qiu C, Feng X, Zeng J, Luo H, Lai Z. Discharge teaching, readiness for discharge, and post-discharge outcomes in cataract patients treated with day surgery: a cross-sectional study. Indian J Ophthalmol. 2019;67(5):612–617. doi:10.4103/ijo.IJO_1116_18
23. Qian J, Qian M, Ren Y, et al. Readiness for hospital discharge and influencing factors: a cross-sectional study on patients discharged with tubes from the department of hepatobiliary surgery. BMC Surg. 2021;21(1). doi:10.1186/s12893-021-01119-0
24. Cai W, Zheng X, Wang R, et al. Factors of parents-reported readiness for hospital discharge in children with acute leukemia: a cross-sectional study. J Healthc Eng. 2022;2022:4082196. doi:10.1155/2022/4082196
25. Nurhayati N, Songwathana P, Vachprasit R. Surgical patients’ experiences of readiness for hospital discharge and perceived quality of discharge teaching in acute care hospitals. J Clin Nurs. 2019;28(9–10):1728–1736. doi:10.1111/jocn.14764
26. Knier S, Stichler JF, Ferber L, Catterall K. Patients’ perceptions of the quality of discharge teaching and readiness for discharge. Rehabil Nurs. 2015;40(1):30–39. doi:10.1002/rnj.164
27. Foust JB. Discharge planning as part of daily nursing practice. Appl Nurs Res. 2007;20(2):72–77. doi:10.1016/j.apnr.2006.01.005
28. Foust JB, Vuckovic N, Henriquez E. Hospital to home health care transition: patient, caregiver, and clinician perspectives. Western J Nurs Res. 2012;34(2):194–212. doi:10.1177/0193945911400448
29. Geng G, He W, Ding L, Klug D, Xiao Y. Impact of transitional care for discharged elderly stroke patients in China: an application of the Integrated Behavioral Model. Topic Stroke Rehabilitat. 2019;26(8):621–629. doi:10.1080/10749357.2019.1647650
30. Unni E, Shiyanbola OO, Farris KB. Change in medication adherence and beliefs in medicines over time in older adults. Global J Health Sci. 2015;8(5):39–47. doi:10.5539/gjhs.v8n5p39
31. Ingersgaard MV, Andersen TH, Norgaard O, Grabowski D, Olesen K. Reasons for nonadherence to statins - a systematic review of reviews. Patient Preference Adherence. 2020;14:675–691. doi:10.2147/PPA.S245365
 © 2024 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2024 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
