Back to Journals » Clinical Optometry » Volume 15
Parent-Reported Visual Concerns in Children with Cerebral Visual Impairment Presenting to a Pediatric Neurology Clinic
Authors Sumalini R , Errolla P, Lingappa L, Conway M , Subramanian A , Satgunam P
Received 8 March 2023
Accepted for publication 29 June 2023
Published 21 July 2023 Volume 2023:15 Pages 147—158
DOI https://doi.org/10.2147/OPTO.S410903
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Mr Simon Berry
Rebecca Sumalini,1– 3 Premalatha Errolla,4 Lokesh Lingappa,4 Miriam Conway,3 Ahalya Subramanian,3 PremNandhini Satgunam1
1Brien Holden Institute of Optometry and Vision Sciences, L V Prasad Eye Institute, Hyderabad, India; 2Institute for Vision Rehabilitation, L V Prasad Eye Institute, Hyderabad, India; 3Division of Optometry and Vision Sciences, City, University of London, London, United Kingdom; 4Department of Pediatric Neurology, Rainbow Children’s Hospitals, Hyderabad, India
Correspondence: Rebecca Sumalini, Brien Holden Institute of Optometry and Vision Sciences, Institute for Vision Rehabilitation, L V Prasad Eye Institute, Hyderabad, India, Tel +91-40-68102825, Email [email protected]
Purpose: Children with cerebral visual impairment (CVI) present with delayed developmental milestones. Pediatricians and pediatric neurologists are usually the first point of contact, and eye exam largely remains referral based. This study documented the visual concerns reported by parents of children with CVI visiting a pediatric neurology clinic. Additionally, we investigated the association between visual concerns, functional vision measures and visual functions.
Patients and Methods: A cross-sectional study was undertaken in children with CVI (chronological age range: 7 months-7 years). Visual concerns reported by the parents/caregivers were documented as open-ended statements. Additionally, a functional vision assessment was conducted using the CVI Range instrument with phase 1, 2 and 3 indicating low, moderate and high visual functioning, respectively. Grating acuity and contrast sensitivity were measured using Teller acuity cards-II and Ohio contrast cards respectively.
Results: A total of 73 children (mean age of 2.84 ± 1.87 years) were recruited. Sixty-eight parents reported visual concerns that were broadly grouped into 14 unique concerns. Nineteen parents (27.9%) reported more than one visual concern. Difficulty maintaining eye contact and recognizing faces were the top two visual concerns in phases 1 and 2. Missing objects in the lower visual field was the top concern in phase 3. A larger number of visual concerns were reported in phase 1 (43%) than phase 2 (40.6%) and phase 3 (16.2%). Multiple regression analysis revealed that grating acuity, contrast sensitivity and chronological age were able to predict the functional vision, F (3, 55) = 63.0, p < 0.001, r2 = 0.77.
Conclusion: Targeted questions enquiring about eye contact and face recognition can be included in history elicitation in children with CVI in pediatric neurology clinics. In the presence of visual concerns, it will be important to assess grating acuity and contrast sensitivity. A poor functional vision score requires referral for eye examination and vision rehabilitation services.
Keywords: functional vision, neurological visual impairment, CVI range, Teller acuity cards-II, Ohio contrast cards
Introduction
Cerebral visual impairment (CVI) is a neurological visual impairment that arises due to damage to the retro-geniculate visual pathways and can involve both cortical and sub-cortical regions of the brain.1 Children with CVI not only present with typical functional vision limitations as observed in children with ocular visual impairment but additionally have difficulty with visual processing skills.2 These children can also have developmental delays in one or multiple areas such as motor, speech, cognition, hearing and vision depending on the location and severity of the brain damage.3 Therefore, in line with other healthcare sectors such as general health4 or specific health issues,5,6 parent/caregiver concerns form an integral basis for history taking and are helpful in deciding appropriate interventions and referral.
Children with CVI are more likely to first present to a pediatric or pediatric neurology clinic rather than an ophthalmology clinic as many of these children suffer from seizures and developmental delays which are more obvious than vision problems. A typical pediatric neurology history also covers vision concerns, but usually this is under the sub-section of headache.7 In a small minority of cases where there are obvious vision problems such as poor eye contact, parents may directly visit an ophthalmology clinic first, but for a vast majority of children visits to the eye clinics are referral based. The referral for vision testing is largely left at the discretion of the pediatrician/pediatric neurologist based on their observations (such as fixing and following light) and concerns reported by the parents/caregivers. The inability to capture visual concerns appropriately is likely to lead to a missed referral diminishing the opportunity for early intervention in the domain of visual rehabilitation. As the overall development of the child and the learning process is dependent on vision (close to 80%),8–11 it is be important to characterize these concerns.
The primary aim of this study is to determine the commonly reported parental concerns of children’s functional vision limitations when presenting to a pediatric neurology clinic following a diagnosis of CVI. The secondary aims are to understand the association between parent reported vision concerns and functional vision assessment using the CVI Range, which is a well-established tool to quantify the functional vision assessment of children with CVI.12 Additionally, we determine the association of functional vision assessment with commonly measured clinical visual functions (visual acuity and contrast sensitivity). Both parameters have been noted to play a vital role in day-to-day functional vision activities.13
Materials and Methods
A prospective, cross-sectional study was carried out in the pediatric neurology clinic of Rainbow children’s hospitals, a tertiary multi-disciplinary pediatric hospital located in Hyderabad, Telangana, India. This work is a part of a larger study being carried out by the research group consisting of collaborators from L V Prasad Eye Institute, Hyderabad, India, Rainbow Children’s Hospitals, Hyderabad, India, and City, University of London, London, UK, on children with CVI. Ethics approval was obtained from all three participating organizations, and the study followed the tenets of the Declaration of Helsinki. For the purpose of this study, parental concerns are reported.
Participants
Study participants were children (in the age range of 7 months to 7 years) diagnosed with CVI by the pediatric neurologist (author LL) based on magnetic resonance imaging scans of the brain, medical history and general observation of visual behaviour such as fixing and following light as is commonly practiced in these clinics. While the diagnostic criteria for CVI varies and remains broad,14 studies have shown that a contributory medical history (pre- or peri-natal history) and an abnormal MRI are strong risk factors for diagnosing CVI.15,16 Ideally, a complete ophthalmological examination will be needed to rule out anterior visual pathway defects. However, currently in pediatric neurology clinics, the diagnosis is made using MRI scans, medical history and general observation of visual behaviour and therefore the same diagnostic criteria were used in the current study. Informed written consent was obtained from the parents of the participating child. Verbal assent was obtained from children who were able to comprehend.
Instruments
Parental concerns about the functional vision limitations of the child were asked as an open-ended question, “What are the vision-related problems that you have noticed in your child?” without any specific leads or prompts. All visual concerns were recorded. No structured questionnaire was used for collecting this information.
Assessment of Functional Vision
Functional vision scoring was carried out using the CVI Range instrument, a commonly used functional vision scale designed for children with CVI.12 The ten characteristics that are included in the CVI Range are listed in Table 1. All characteristics were assessed as recommended12 through examiner observation, parent interview and direct assessment.17 Each characteristic is graded separately, and the total score is the summation of the score obtained on all characteristics and can lie between 0.0 and 10.0 with a higher value indicating better functional vision. Based on the total score, the child is categorized into one of the three phases, phase 1 = building visual behavior (score range: 0 to 3.0), phase 2 = integrating vision with function (3.25 to 7.0) and phase 3 = resolution of CVI characteristics (7.25 to 10.0). The CVI Range is usually administered through two ratings (i) across-the-characteristics scale (an overall understanding of the child’s visual abilities) and (ii) within-the-characteristics scale (rating of each characteristic to understand the extent of the individual contribution to the overall visual functioning of the child).12 Due to time constraints in assessing both ratings, we restricted our assessment to “within-the-characteristics” scale.
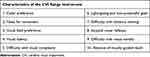 |
Table 1 The Ten Common Characteristics Observed in Children with CVI: The CVI Range Instrument12 |
Assessment of Grating Acuity
Teller acuity cards-II (TAC-II)18 were used to assess binocular presenting grating acuity. This test follows a preferential looking paradigm and is a 2-alternate forced choice (2-AFC) test. The gratings are vertically oriented. As the chronological age range of the children was 7 months and above, the first card was presented at 55 cms and then the decision to continue at the same testing distance or moving closer/farther was taken depending on the response of the child. As this cohort consists of children with visual impairment, the closest working distance used was 19 cms.18 The length of the card (55 cms) was used as a reference to ensure that the testing distance was maintained while presenting the cards. The descending method of limits (from the lowest to the highest spatial frequency) paradigm was used to threshold the grating acuity with the examiner being masked to the grating location (as the cards were arranged upside down) until obtaining the child’s response. The spatial frequency that can be measured using TAC-II from the closest testing distance of 19 cms is 0.23 cycles per centimeter (CPCM) (0.07 CPD) to farthest testing distance of 84 cms is 38.0 CPCM (57.0 CPD) (~2.63 to −0.27 logMAR). If the response to one card was incorrect (i.e. the child was looking or pointing to the blank side of the cards), then the same card was presented one more time and the response that was obtained two out of three times was considered to be the final response for that particular card. In case the child was not/incorrectly responding to a particular card two out of three times, then the card that was presented earlier was considered to be the end point of the test.
Assessment of Contrast Sensitivity
Ohio contrast cards19 were used to assess binocular presenting contrast sensitivity. Similar to TAC-II, these cards also follow the preferential looking paradigm with a 2-AFC test but use horizontally oriented gratings. All children were tested at 57 cm,19 which was used as an easy reference as it was the length of the card. Twelve contrast sensitivity levels can be measured using the Ohio contrast cards, i.e. from 100% to 2.2%. Thresholding paradigm of descending method of limits (i.e. from the easily identifiable contrast level to the difficult to identify contrast level) was used, and the examiner was masked to the location of the grating until obtaining the child’s response. Additionally, the estimation technique was used to arrive at the threshold contrast level similar to that described above for TAC-II.
Eliciting the visual concerns of the children from the parents/caregivers, and the tests of visual functions were carried out by a single examiner (author RS). The assessment of functional vision was carried out by the author RS with the assistance of a trained vision rehabilitation professional (author PE).
Statistical Analysis
Data was analyzed using IBM SPSS software (ver. 20, Chicago, USA). Pearson chi-square was used to determine the significance in frequency distributions of visual concerns in the different phases of CVI. Spearman-rho was used to test the correlation between functional vision and visual functions. Kruskal-Wallis test was used to determine the statistical significance of visual functions across the 3 phases of CVI and across the chronological age categories. Multiple regression analysis was carried out to determine the parameters that best predict the functional vision score.
Results
A total of 73 children (mean age: 2.84 ± 1.87 years, range: 7 months–7 years, 74% males (n = 54)) with CVI were recruited. Only a small minority of children previously underwent an eye examination (n = 11, 15%) and in addition comprehensive eye evaluation findings carried out as part of a larger study were available in 10 children (13.6%). In the total 21 children (28.7%) in whom these findings were available, optic atrophy was noted to be the most common ocular abnormality (n = 14, 66.6%), followed by normal fundus findings in 6 children (28.5%) and 1 child who had retinopathy of prematurity (4.7%). All the children had abnormal MRI findings, including 2 children who had genetic aetiology of CVI.
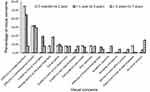
Five parents (6.8%) did not report any specific visual concerns, while the remaining (n = 68) did. Nineteen parents (27.9%) reported two visual concerns, giving rise to a total of 87 visual concerns documented from all participants. The reported visual concerns could be grouped into 14 unique visual concerns (Figure 1).
Functional Vision Assessment and Visual Concerns
One child (crying constantly) could not be assessed using the CVI range instrument. The remaining children (n = 72) were categorized into 3 phases based on their CVI range score (a higher score indicates better functional vision) (phase 1, n = 30 (41.6%); phase 2, n = 27 (37.5%), phase 3, n = 15 (20.8%)). The frequency distribution of all the visual concerns (including no visual concerns, n = 5) was found to be significantly different across all 3 phases of CVI (p = 0.012, Pearson chi-square). The distribution of the concerns across the phases is shown in Figure 1. The frequency distribution of visual concerns in individual phases: phases 1 and 2 (p = 0.46, Pearson chi-square), phases 2 and 3 (p = 0.06, Pearson chi-square) was found to be comparable, however, phases 1 and 3 were found to be significantly different (p = 0.012, Pearson chi-square). Among the 19 children whose parents reported more than one visual concern, the distribution of them in the phases was as follows: phase 1, n = 7 (36.8%); phase 2, n = 9 (47.3%); phase 3, n = 3 (15.7%).
Difficulty in recognizing faces (phase 1, n = 12 (40%); phase 2, n = 10 (37%)) and maintaining eye contact (phase 1, n = 9 (30%); phase 2, n = 12 (44.4%)) were noted to be the most common visual concerns in phases 1 and 2. The third highest visual concern of unable to look or track lights primarily was found in phase 1 (n = 7, 23.3%). Children in phase 3 (i.e. those who had better function) primarily had concerns with missing objects in the lower/side field (n = 4, 26.7%) (Figure 1 and Table 2).
 |
Table 2 Distribution of Children Across the 3-Phases of CVI Along with Chronological Age Categories, Visual Functions and Visual Concerns |
As face recognition and eye contact were reported as the top two visual concerns overall, further analysis was carried out based on the functional vision. Functional vision of children whose parents reported difficulty with face recognition and eye contact (considered as group 1) was compared against those whose parents reported other visual concerns (considered as group 2). Children in group 1 were noted to be significantly younger (mean: 2.25 ± 1.55 years, n = 36) when compared to those in group 2 (mean: 3.41 ± 1.98 years, n = 37) (p = 0.01, Mann–Whitney). Functional vision (p = 0.02, Mann–Whitney) was noted to be significantly poorer in children in group 1 when compared to group 2 (Figure 2 and Table 3).
 |
Table 3 Comparison of Vision-Related Parameters in Children Reported to Have Difficulty in Face Recognition and Eye Contact (Group 1) and Those Reported to Have Other Visual Concerns (Group 2) |
Functional Vision Assessment and Visual Functions
The association between the functional vision score using the CVI Range and visual functions was studied. We were unable to quantify grating acuity and contrast sensitivity in a small proportion of children as they were unable to appreciate the demonstration plate (acuity, n = 5 (6.8%), contrast, n = 4 (5.4%)) despite cooperating for testing. A small percentage of children did not cooperate to complete the test, acuity, n = 2 (2.7%), contrast, n = 8 (10.9%) and functional vision assessment, n = 1 (1.3%) (Table 2).
Chronological ages were significantly different across the 3 phases of CVI (p = 0.001, Kruskal-Wallis), with more younger children (<3 years old) found in phase 1. Grating acuity and contrast sensitivity were also found to be significantly different across the 3 phases of CVI (p < 0.001, n = 59) with age as a covariate using linear-mixed model analysis. Grating acuity, contrast sensitivity and chronological age were used in a multiple regression analysis to predict the functional vision score. The prediction model was statistically significant (F (3, 55) = 63.6, p < 0.001) and accounted for approximately 77% (r2=0.77) of the variance of functional vision score. The interaction of the three parameters together was found to be the best predictor when compared to an individual or combination of just two parameters. The regression analysis for each predictor variable when other 2 predictors are controlled for is as follows: For every 1.0 logMAR increase (i.e. worsening) in grating acuity, there would be a significant decrease in the functional vision score by 2.8 points (β = −2.8, p < 0.001). However, for every 1.0 logCS increase (ie, better) in contrast sensitivity value, there would be a significant increase in the functional vision score by 1.3 points (β = 1.3, p = 0.04). However, for every one-month increase in the age, only a small but not significant increase in the functional vision score by 0.02 points was noted (β = 0.02, p = 0.1).
Visual functions of children whose parents reported difficulty with face recognition and eye contact (considered as group 1) were compared against those whose parents reported other visual concerns (considered as group 2). In case of parents reporting difficulty in face recognition/eye contact along with any other concern, the child was categorized in group 1. Grating acuity was poorer in group 1 when compared to group 2 and was noted to be tending towards significance between both groups (p = 0.06, Mann–Whitney) (Figure 3 and Table 3). Contrast sensitivity was noted to be significantly poorer in children in group 1 when compared to group 2 (p = 0.009, Mann–Whitney) (Figure 4 and Table 3).
Functional Vision Assessment and Chronological Age
Children were divided into 3 categories based on their chronological age (Figure 5). The frequency distribution of all visual concerns (including no visual concerns, n = 5) was found to be comparable across all 3 age categories (p = 0.35, Pearson chi-square). Difficulty in recognizing faces (7 months to 1 year, n = 7, 53.8%; >1 to 3 years, n = 14, 43.8%) and maintaining eye contact (7 months to 1 year, n = 4, 30.8%; >1 to 3 years, n = 10, 31.3%) were noted to be the top two concerns in these age categories. In children above 3 years of age, difficulty in maintaining eye contact remained as a major visual concern (n = 8, 28.6%) followed by missing objects on the lower/side field (n = 5, 17.9%) (Figure 5 and Table 2).
Discussion
This study aimed to document the visual concerns of children with CVI presenting to a pediatric neurology clinic as reported by their parents/caregivers. Fourteen unique visual concerns have been identified in these children with the most common ones being difficulty in maintaining eye contact and recognizing faces. This finding is in agreement with the earlier literature that has reported face identification as one of the symptoms.20,21
The significantly different frequency distribution of visual concerns across the 3 phases of CVI based on the functional vision score is an important finding. Functional vision assessment is often carried out in vision rehabilitation centres and is specifically important in children with developmental delays. The functional vision performance in these children could be very different due to interaction of delays in multiple areas (such as vision, fine motor, gross motor, cognition and speech) and may not be fully explained by the ocular diagnosis alone.22 However, we report that grating acuity, contrast sensitivity and chronological age taken together are able to best predict the functional vision score of the child. These findings indicate the importance of functional vision assessment to understand the child’s visual potential that forms the basis to devise suitable vision rehabilitation strategies.23
Contrast sensitivity is not as commonly assessed as visual acuity in general clinical examination.13 In this study, we found that a change in contrast sensitivity measure affects the functional vision score of the child as well. It is therefore important for clinicians to integrate contrast sensitivity testing into their regular clinical practice, interpret the findings and explain contrast enhancing measures to parents as well.24 An easy-to-remember 3-word strategy for clinicians related to enhancing contrast for children with CVI includes: Big Bold Bright.24
Children of parents who did not report any vision concern (phase 3 = 4, phase 2 = 1) had a range of acuity between 0.19 (close to normal) and 1.28 logMAR (moderate visual impairment) and contrast sensitivity ranging from 0.6 (reduced) to 1.66 (normal/near normal) logCS. This indicates that parents may not always be able to identify visual concerns in children with CVI even if their acuity and contrast are significantly reduced. Developmental delays could make it harder for parents to notice visual problems. Our study findings highlight that parents of all children with CVI should be questioned about the child’s functional vision problems as in some children these problems can be missed or not looked for. Upon questioning, parents will also be aware to look for those domains of functional vision. Children with poor eye contact, inability to recognize faces or look at or track lights were easily identified by the parents as having difficulties with visual problems and this was co-related with clinical measures of visual function.
As mentioned previously, pediatric ophthalmology/optometry services largely remain referral-based services for children with neurological visual impairment, eg, CVI. This is most likely due to the child having multiple developmental delays and motor and speech being the more obvious areas compared to vision. This is also reflected in the very low percentage of children (15%) in our study who previously had an ophthalmology/optometry assessment. Educating parents/caregivers about ocular conditions in children that need evaluation is useful and is the key to plan better rehabilitation strategies and provide guidance to therapists. A recent study highlighted the lack of awareness of early detection of CVI amidst clinicians and emphasized the need for more research from different geographic areas, ethnicities, etc.21 The results of our study contribute towards this effort to expand this literature base.
As the assessment and management of children with CVI is multi-disciplinary,25 it requires close collaborative work between professionals and need-based cross referrals. In one of our ongoing studies, we have found a moderate correlation between the developmental quotient and the functional vision score (r = 0.5).26 This highlights the importance of referral by the developmental psychologist/pediatrician in referring children with lower developmental quotients for comprehensive eye care services and for eye care professionals to refer for an assessment of the child’s overall development if the child is noted to have poor functional vision. Early intervention therapists primarily physiotherapists, occupational therapists, speech therapists and special educators regularly interact with children having developmental delays with underlying causes of neurological conditions such as cerebral palsy as part of their therapy sessions. Approximately 60–70% of children with cerebral palsy also have CVI.27,28 Therefore, it is important to raise awareness among these professionals as well about the vision concerns that these children are likely to exhibit.
The current study has few limitations. As CVI remains a diagnosis of exclusion, a firm diagnostic criteria have always been elusive. In our study, the diagnosis of CVI was made by the pediatric neurologist based on the MRI findings, medical history and general observation of visual behaviour. Comprehensive eye evaluation findings were only available in a small proportion of children (28.7%), among whom optic atrophy was noted to be high (66.6%), similar to other studies.29,30
In the current study, we used “within-the-characteristic” rating scale for assessing functional vision. Roman-Lantzy reports that the scores of the two rating scales can be similar but generally not identical.12 In a separate study carried out by our rehabilitation professionals, “across-the-characteristic” rating scale took approximately 40 minutes to 1 hour (unpublished results). Therefore, considering the time constraints, “within-the-characteristic” rating scale was used as a surrogate measure to categorize the children based on their functional vision. However, the authors agree that it would have been ideal to use both the rating scales and arrive at a final functional vision score. It is important to note that the scores obtained in this study were not used to plan rehabilitative strategies for children. Instead, all children who were recruited in the study were recommended a comprehensive rehabilitative assessment along with an eye examination. These results have not been discussed here, as they are beyond the scope of this paper.
The vision-related parameters of children with concerns of difficulty in face recognition and eye contact were significantly poorer (contrast sensitivity, p = 0.009 and functional vision, p = 0.02; grating acuity was tending towards significance, p = 0.06) when compared to those with other visual concerns; however, they were also significantly younger (p = 0.01). These findings indicate that these two visual concerns (i.e. face recognition and eye contact) are important to be asked to the parents/caregivers to help decide referral in addition to other referral parameters used by pediatric neurologists for children with CVI to undertake comprehensive eye evaluation, particularly in younger children in whom the parents may not have noticed any obvious visual limitation. Identifying these visual concerns early help in early diagnosis and referral. However, the current study has not looked into the specificity of these questions and it should be noted that children with other special educational needs, such as autism spectrum disorder, can also have concerns with eye contact.
Detailed structured questionnaires have been developed for children with CVI.31–33 These are primarily used in pediatric ophthalmology and vision rehabilitation centres and may be difficult to use in neurology clinics owing to time constraints. The most commonly reported concerns in this study included difficulty in recognizing faces and maintaining eye contact. These 2 concerns along with bumping into objects and eye deviation were also noted as the primary reasons by parents visiting a special needs vision clinic in a heterogeneous group of children with special needs.34 It would be useful to add these concerns as a part of the brief vision history that can be elicited in pediatric neurology clinics. Additionally, observing whether the child can fixate and follow light can form part of a quick assessment, as this was also reported to be the third most common concern in our study.
Conclusion
A basic vision-related history and quick assessment in the pediatric neurology clinic can result in early referrals to eye care and vision rehabilitation services. Particularly, children having a poor functional vision score may also have an associated reduction in grating acuity and contrast sensitivity. Appropriate refractive correction can improve the vision in these children to a certain extent, which could then have an associated improvement in the functional vision score and thereby positively impact the overall development of the child. This, however, needs further research.35
Acknowledgments
The authors thank the parents of children with CVI for consenting to study participation.
Funding
This work was funded by the Hyderabad Eye Research Foundation.
Disclosure
The authors report no conflicts of interest and have no proprietary interest in any of the materials mentioned in this article.
References
1. Leuck AH, Dutton GN. Vision and Brain: Understanding Cerebral Visual Impairment in Children.
2. Martin MB, Santos-Lozano A, Martin-Hernandez J, et al. Cerebral versus ocular visual impairment: the impact on developmental neuroplasticity. Front Psychol. 2016;7:1958. doi:10.3389/fpsyg.2016.01958
3. Pehere N, Chougule P, Dutton GN. Cerebral visual impairment in children: causes and associated ophthalmological problems. Indian J Ophthalmol. 2018;66(6):812–815. doi:10.4103/ijo.IJO_1274_17
4. Garbutt JM, Leege E, Sterkel R, Gentry S, Wallendorf M, Strunk RC. What are parents worried about? Health problems and health concerns for children. Clin Pediatr (Phila). 2012;51(9):840–847. doi:10.1177/0009922812455093
5. Duker LIS, Henwood BF, Bluthenthal RN, Juhlin E, Polido JC, Cermak SA. Parents’ perceptions of dental care challenges in male children with autism spectrum disorder: an initial qualitative exploration. Res Autism Spectr Disord. 2017;39:63–72. doi:10.1016/j.rasd.2017.03.002
6. Rannard A, Lyons C, Glenn S. Parent concerns and professional responses: the case of specific language impairment. Br J General Pract. 2005;55(518):710–714.
7. Wang BW. The pediatric neurological history (edited by: Muir K); 2011; Available from: https://learn.pediatrics.ubc.ca/body-systems/nervous-syste/the-pediatric-neurological-history/.
8. Glezer VD. Vision and Mind: Modeling Mental Functions. Mahwah, NJ: Lawrence Erlbaum Publishers; 1995.
9. Zeki S. A Vision of the Brain. Oxford: Blackwell Scientific Publications; 1993.
10. Gazzaniga MS, Ivry RB, Jangun GR. Cognitive Neuroscience, the Biology of the Mind. New York, NY: WW Norton & Co; 1998.
11. Parker S. The Eye and Seeing. New York, NY: Franklin Watts; 1989.
12. Roman-Lantzy C. Cortical Visual Impairment: An Approach to Assessment and Intervention.
13. Xiong YZ, Kwon M, Bittner AK, Virgili G, Giacomelli G, Legge GE. Relationship between acuity and contrast sensitivity: differences due to eye disease. Invest Ophthalmol Vis Sci. 2020;61(6):40. doi:10.1167/iovs.61.6.40
14. Matsuba CA, Jan JE. Long-term outcome of children with cortical visual impairment. Dev Med Child Neurol. 2006;48(6):508–512. doi:10.1017/S0012162206001071
15. van Genderen M, Dekker M, Pilon F, Bals I. Diagnosing cerebral visual impairment in children with good visual acuity. Strabismus. 2012;20(2):78–83. doi:10.3109/09273972.2012.680232
16. Cioni G, Fazzi B, Ipata AE, Canapicchi R, van Hof-van Duin J. Correlation between cerebral visual impairment and magnetic resonance imaging in children with neonatal encephalopathy. Dev Med Child Neurol. 1996;38(2):120–132. doi:10.1111/j.1469-8749.1996.tb12083.x
17. Chang M, Roman-Lantzy C, O’Neil SH, Reid MW, Borchert MS. Validity and reliability of CVI Range assessment for Clinical Research (CVI Range-CR): a longitudinal cohort study. BMJ Open Ophthalmol. 2022;7(1):e001144. doi:10.1136/bmjophth-2022-001144
18. Teller, DY, Dobson, V, Mayer, DL Reference and Instruction Manual: Teller acuity cards II (TAC II) (Stereo Optical Company). 2005 (revised) . Available from: https://eiiwebassets.s3.amazonaws.com/s/sterooptical/pdf/other-manuals/TAC_II_manual.pdf
19. Hopkins GR, Dougherty BE, Brown AM. The Ohio contrast cards: visual performance in a pediatric low-vision site. Optom Vis Sci. 2017;94(10):946–956. doi:10.1097/OPX.0000000000001119
20. Bauer CM, Manley CE, Ravenscroft J, Cabral H, Dilks DD, Bex PJ. Deficits in face recognition and consequent quality-of-life factors in individuals with cerebral visual impairment. Vision. 2023;7(1):9. doi:10.3390/vision7010009
21. Oliver H, Seccurro D, Dorich J, Rice M, Schwartz T, Harpster K. “Even though a lot of kids have it, not a lot of people have knowledge of it”: a qualitative study exploring the perspectives of parents of children with cerebral/cortical visual impairment. Res Dev Disabil. 2023;135:104443. doi:10.1016/j.ridd.2023.104443
22. Swaminathan M, Jayaraman D, Jacob N. Visual function assessment, ocular examination, and intervention in children with developmental delay: a systematic approach. Part 1. Indian J Ophthalmol. 2019;67(2):196–203. doi:10.4103/ijo.IJO_524_18
23. Bennett CR, Bex PJ, Bauer CM, Merabet LB. The assessment of visual function and functional vision. Semin Pediatr Neurol. 2019;31:30–40. doi:10.1016/j.spen.2019.05.006
24. Pilling RF. Make it easier: 3-word strategies to help children with cerebral visual impairment use their vision more effectively. Eye. 2023;37(2):285–289. doi:10.1038/s41433-021-01920-4
25. Ortibus E, Fazzi E, Dale N. Cerebral visual impairment and clinical assessment: the European perspective. Semin Pediatr Neurol. 2019;31:15–24. doi:10.1016/j.spen.2019.05.004
26. Chakram RS, Satgunam P, Subramanian A, et al. Does vision correlate with overall development in children with cerebral visual impairment? Invest Ophthalmol Vis Sci. 2022;63(7):3277 – A0329-3277–A0329.
27. Schenk-Rootlieb AJ, van Nieuwenhuizen O, van Waes PF, van der Graaf Y. Cerebral visual impairment in cerebral palsy: relation to structural abnormalities of the cerebrum. Neuropediatrics. 1994;25(2):68–72. doi:10.1055/s-2008-1071588
28. Uggetti C, Egitto MG, Fazzi E, et al. Cerebral visual impairment in periventricular leukomalacia: MR correlation. Am J Neuroradiol. 1996;17(5):979–985.
29. Pehere NK, Narasaiah A, Dutton GN. Cerebral visual impairment is a major cause of profound visual impairment in children aged less than 3 years: a study from tertiary eye care center in South India. Indian J Ophthalmol. 2019;67(10):1544–1547. doi:10.4103/ijo.IJO_1850_18
30. Bosch DGM, Boonstra FN, Willemsen MA, Cremers FP, de Vries BB. Low vision due to cerebral visual impairment: differentiating between acquired and genetic causes. BMC Ophthalmol. 2014;14(1). doi:10.1186/1471-2415-14-59
31. Tsirka A, Liasis A, Kuczynski A, et al. Clinical use of the Insight Inventory in cerebral visual impairment and the effectiveness of tailored habilitational strategies. Dev Med Child Neurol. 2020;62(11):1324–1330. doi:10.1111/dmcn.14650
32. Ben Itzhak N, Vancleef K, Franki I, Laenen A, Wagemans J, Ortibus E. Visuoperceptual profiles of children using the Flemish cerebral visual impairment questionnaire. Dev Med Child Neurol. 2020;62(8):969–976. doi:10.1111/dmcn.14448
33. Ortibus E, Laenen A, Verhoeven J, et al. Screening for cerebral visual impairment: value of a CVI questionnaire. Neuropediatrics. 2011;42(4):138–147. doi:10.1055/s-0031-1285908
34. Chakram RS, Satgunam P, Subramanian A, et al. Parents reported visual concerns in a population of children with special needs in India.
35. Bullaj R, Dyet L, Mitra S, et al. Effectiveness of early spectacle intervention on visual outcomes in babies at risk of cerebral visual impairment: a parallel group, open-label, randomised clinical feasibility trial protocol. BMJ Open. 2022;12(9):e059946. doi:10.1136/bmjopen-2021-059946
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.